ANESTHESIA FOR ENDOSCOPIC PROCEDURES What goes in must







- Slides: 26

ANESTHESIA FOR ENDOSCOPIC PROCEDURES What goes in, must come out (or call a surgeon) © 2016 Mark S Weiss, MD Department of Anesthesiology and Critical Care
HUP GI w Sick, ASA III and IV, patients undergoing endoscopic GI procedures • Or ASA II patients with acute GI symptoms w “Minimally invasive, ” but room must be set up for full spectrum of emergencies/resuscitation/airway management • Set up the same as in any OR: – MSMAIDS! (machine, suction (flexible sucker), medications, airway, IV, special) – Double check supplemental O 2, emergency cardiac drugs – Remember help may be far away w Rapid turnover • Never fast, just efficient 2
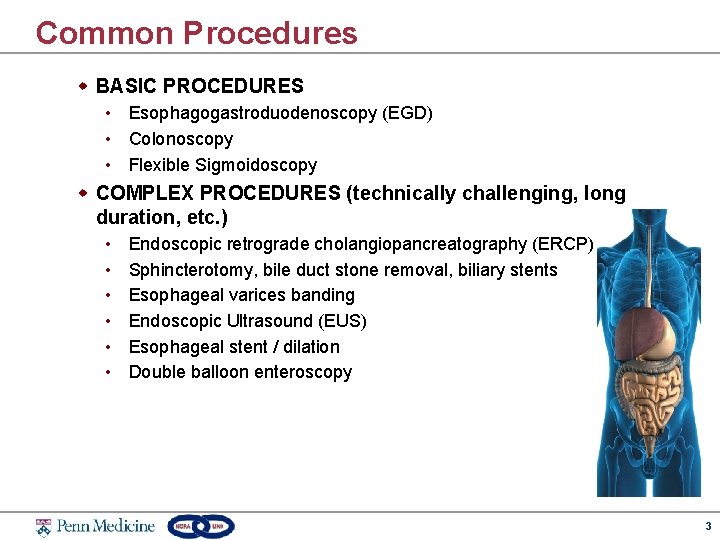
Common Procedures w BASIC PROCEDURES • Esophagogastroduodenoscopy (EGD) • Colonoscopy • Flexible Sigmoidoscopy w COMPLEX PROCEDURES (technically challenging, long duration, etc. ) • • • Endoscopic retrograde cholangiopancreatography (ERCP) Sphincterotomy, bile duct stone removal, biliary stents Esophageal varices banding Endoscopic Ultrasound (EUS) Esophageal stent / dilation Double balloon enteroscopy 3

EGD w Gastroscope (100 cm length, 8 -11 mm diameter) w Exam scope may go as far as duodenum w Quick procedure • 5 -30 min depending on diagnostic or therapeutic maneuvers 4
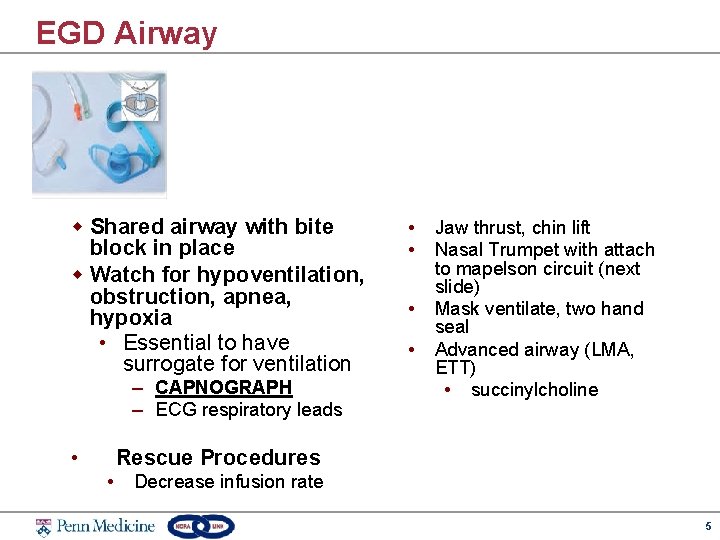
EGD Airway w Shared airway with bite block in place w Watch for hypoventilation, obstruction, apnea, hypoxia • Essential to have surrogate for ventilation – CAPNOGRAPH – ECG respiratory leads • • • Jaw thrust, chin lift Nasal Trumpet with attach to mapelson circuit (next slide) Mask ventilate, two hand seal Advanced airway (LMA, ETT) • succinylcholine Rescue Procedures • Decrease infusion rate 5
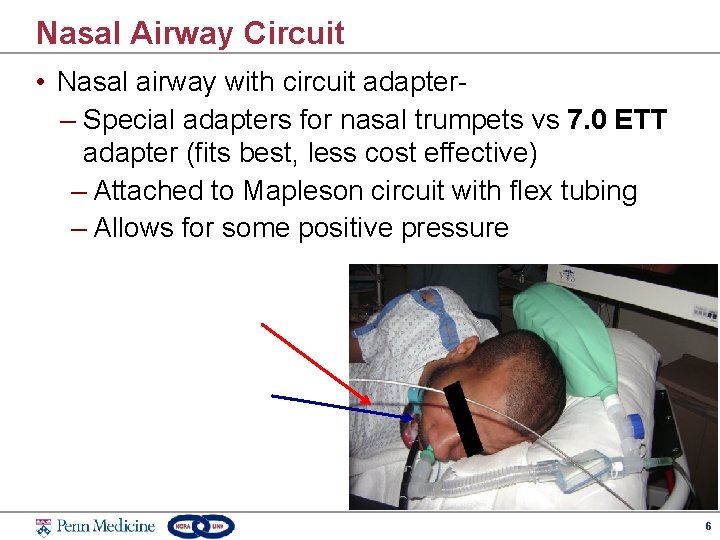
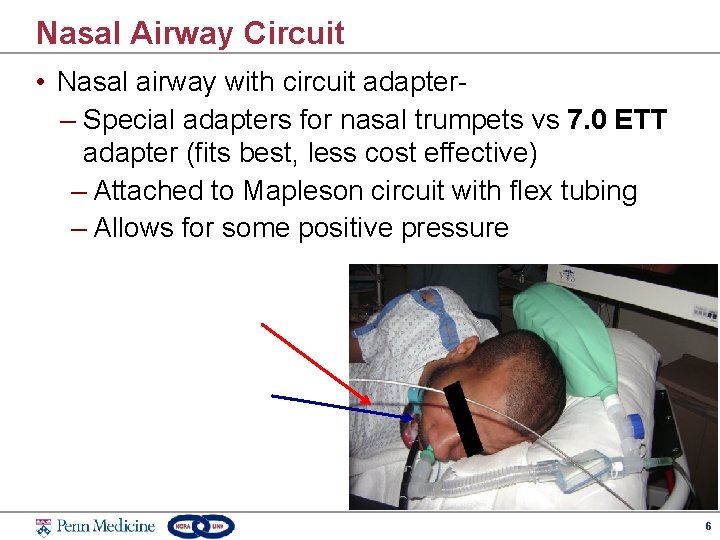
Nasal Airway Circuit • Nasal airway with circuit adapter– Special adapters for nasal trumpets vs 7. 0 ETT adapter (fits best, less cost effective) – Attached to Mapleson circuit with flex tubing – Allows for some positive pressure 6

EGD Stimulus w. Gag/pharyngeal reflex: • Afferent limb Glossopharyngeal (CN IX) • Efferent limb- Vagus nerve (CN X) 7
EGD Sedation Tips w Blunt gag reflex • Start with a safe and effective upfront bolus • Use Fentanyl as an adjunct to propofol w Keep patient immobile while in fragile areasesophagus/stomach • Stable maintenance propofol infusion • Depth of sedation influenced by procedure complexity (variceal ligation vs. routine diagnostic screen) • Potential for multiple scope passes (wider lumen scopes for EUS) 8
EGD Complications w. Perforation w. Bleeding w. Infection w. Rare (each 1: 1000) w. Variceal bleeding in liver disease 9
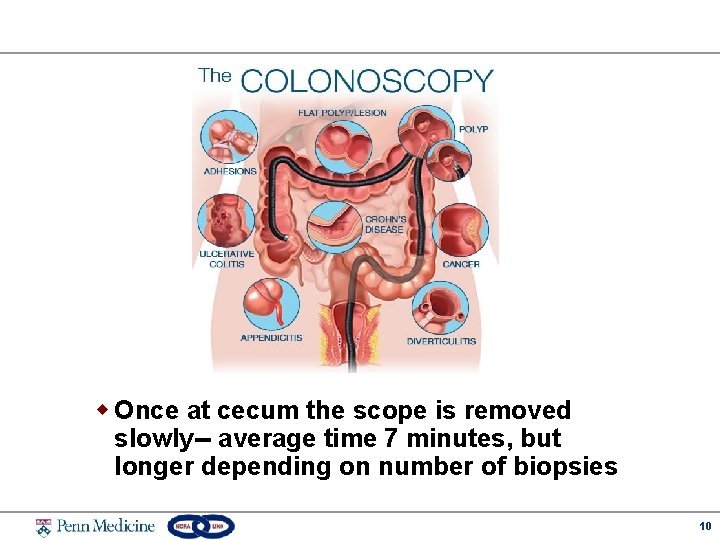
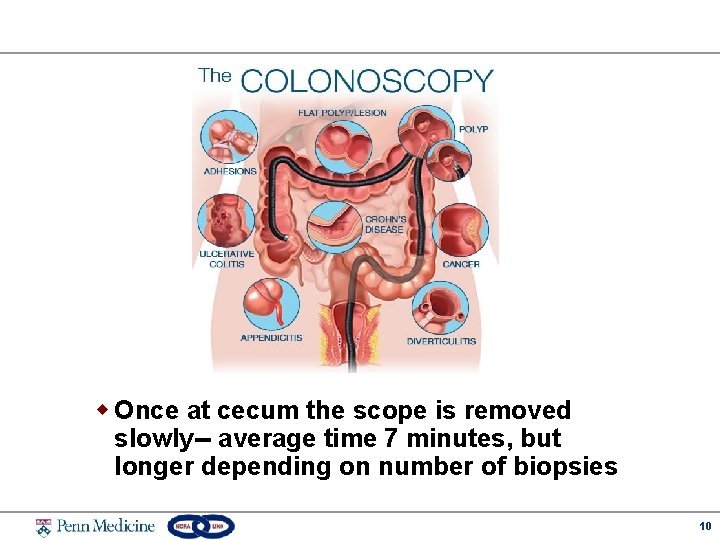
w Once at cecum the scope is removed slowly-- average time 7 minutes, but longer depending on number of biopsies 10

Colonoscopy Stimulus w Proceduralist technique greatly impacts the amount of pain stimulation • “Looping” the scope • Luminal distention through gas insufflation • External abdominal pressure to help direct scope • Retroflex at the sigmoid colon (end of the procedure) w Pain mechanism • Visceral pain, mechanoreceptors transmitted via rectal/pelvic spinal afferents, cell bodies in the lumbosacral region of the spinal cord • Autonomic vasovagal reactions 11
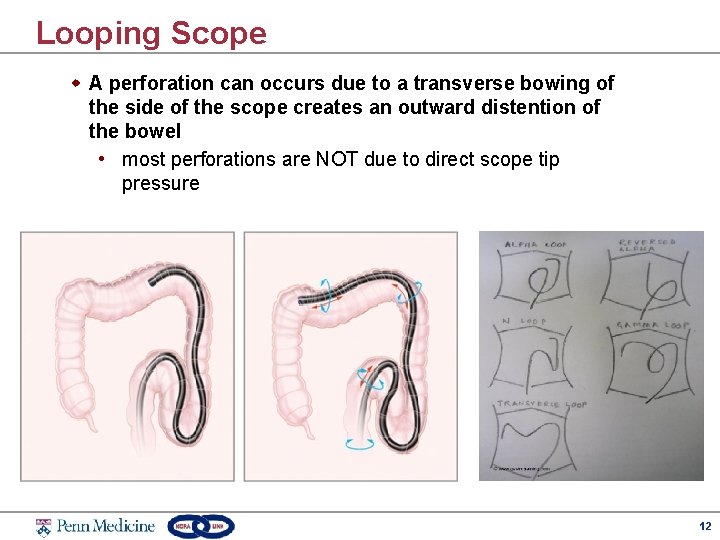
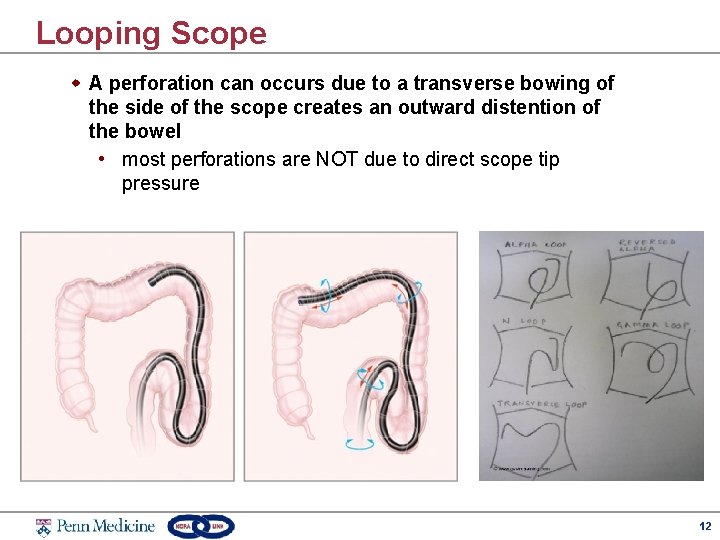
Looping Scope w A perforation can occurs due to a transverse bowing of the side of the scope creates an outward distention of the bowel • most perforations are NOT due to direct scope tip pressure 12
Colonoscopy Pain w Patient conditions can alter acute pain processing • • Inflammatory Bowel disease Irritable Bowel Syndrome Functional abdominal pain from chronic disease Cancer pain 13

Colonoscopy Sedation Tips w Scope insertion is not the most stimulating (unlike EGD) w Propofol (small bolus plus infusion) provides optimal procedural conditions in most patients w Pain stimulus is not predictable (i/e when the scope loops), but typically occurs in sigmoid and transverse colon • Fentanyl may be given if the patient moves w Propofol infusion can be discontinued while 20 -30 cm of scope remains w Retroflexion at rectum may arouse the patient, but do NOT give a reactionary bolus 14
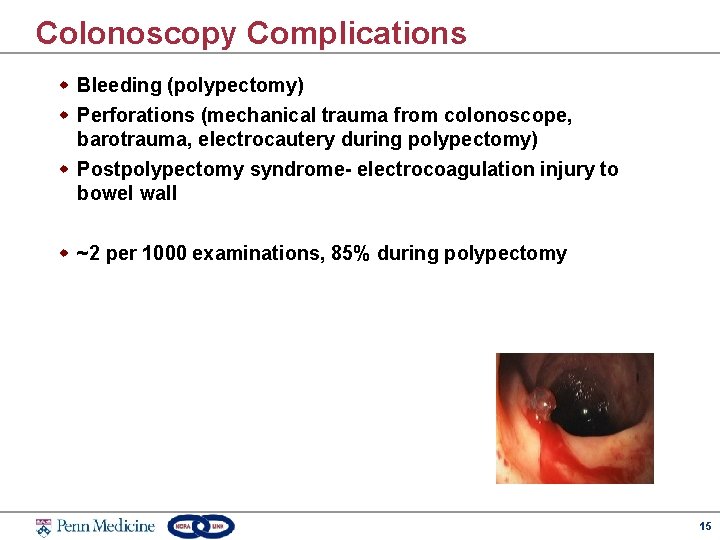
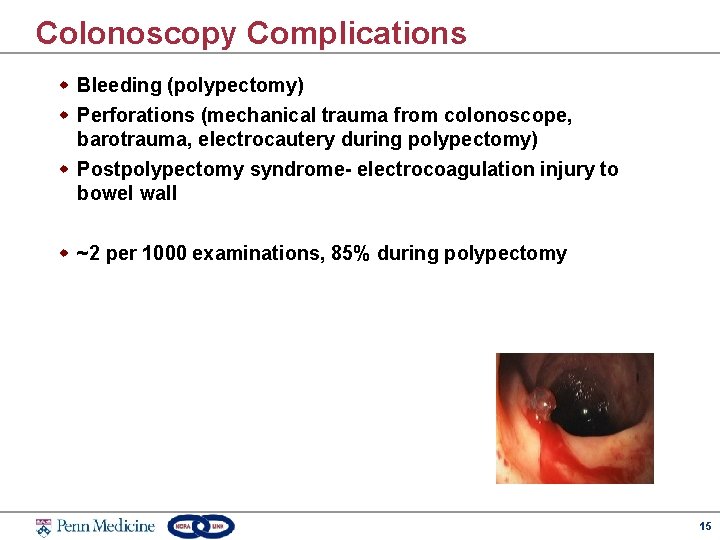
Colonoscopy Complications w Bleeding (polypectomy) w Perforations (mechanical trauma from colonoscope, barotrauma, electrocautery during polypectomy) w Postpolypectomy syndrome- electrocoagulation injury to bowel wall w ~2 per 1000 examinations, 85% during polypectomy 15
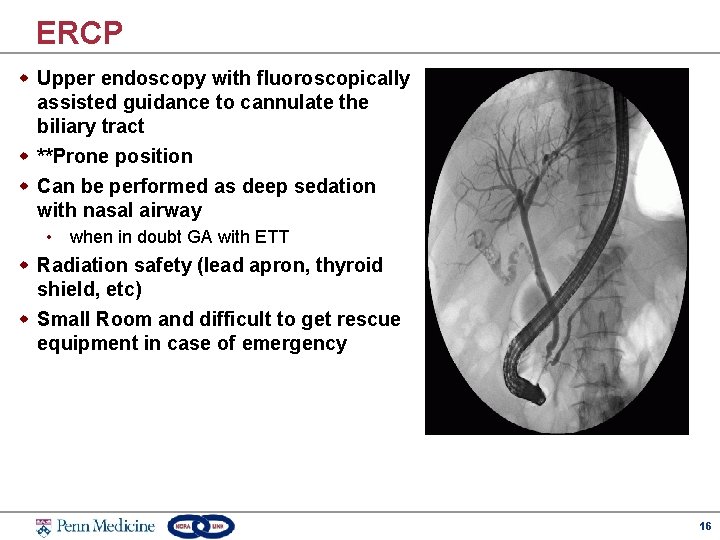
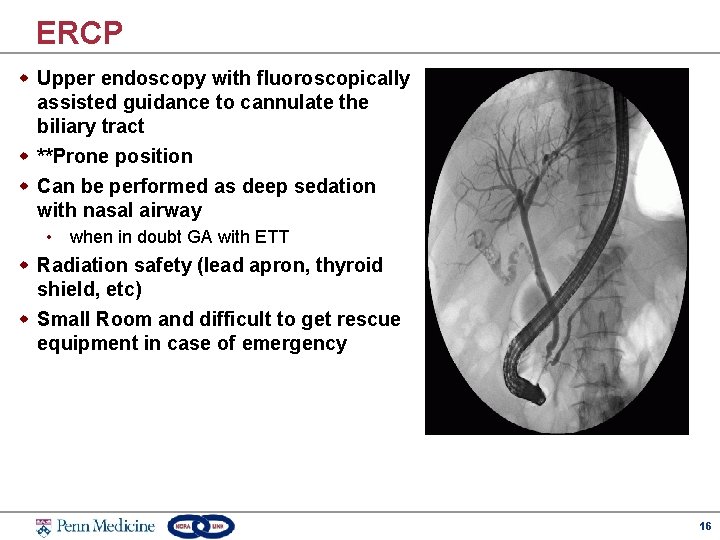
ERCP w Upper endoscopy with fluoroscopically assisted guidance to cannulate the biliary tract w **Prone position w Can be performed as deep sedation with nasal airway • when in doubt GA with ETT w Radiation safety (lead apron, thyroid shield, etc) w Small Room and difficult to get rescue equipment in case of emergency 16
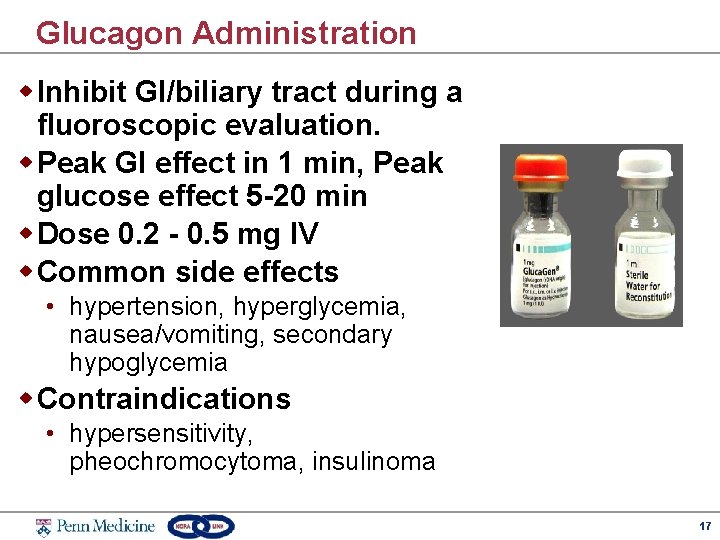
Glucagon Administration w Inhibit GI/biliary tract during a fluoroscopic evaluation. w Peak GI effect in 1 min, Peak glucose effect 5 -20 min w Dose 0. 2 - 0. 5 mg IV w Common side effects • hypertension, hyperglycemia, nausea/vomiting, secondary hypoglycemia w Contraindications • hypersensitivity, pheochromocytoma, insulinoma 17

Common Endoscopy Related Complications w. Attributed to sedation • Hypoxia, hypotension, consequences of hypercarbia, prolonged PACU stay • 50 -85% complications attributed to cardiopulmonary events in setting of sedation w. What is our value? • Safe administration of deep sedation during complex procedures • Reduction complications in low risk procedures • Rescue during sedation care 18
Hypotension w Sympathetic blunting of response to hypovolemia by anesthetics w Vasovagal reaction w Procedural complication w Rare: • • Decreased LV contractility (from anesthetics), Hypercapnia/hypoxia Increased PVR (decreased RV function) anaphylaxis 19
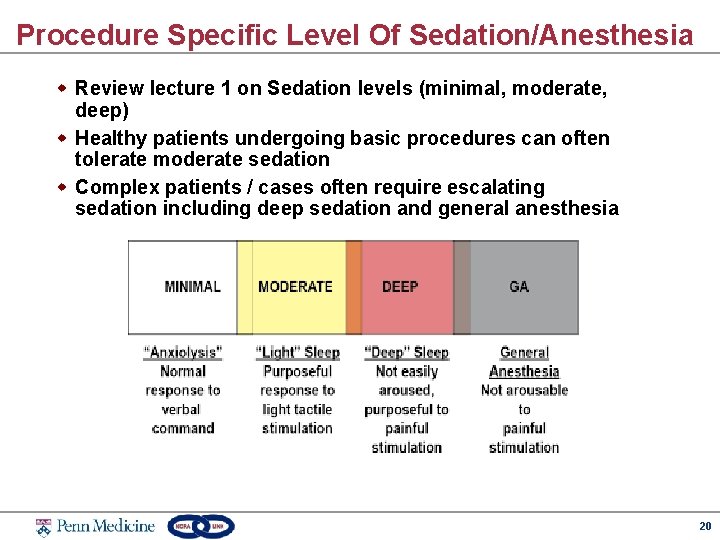
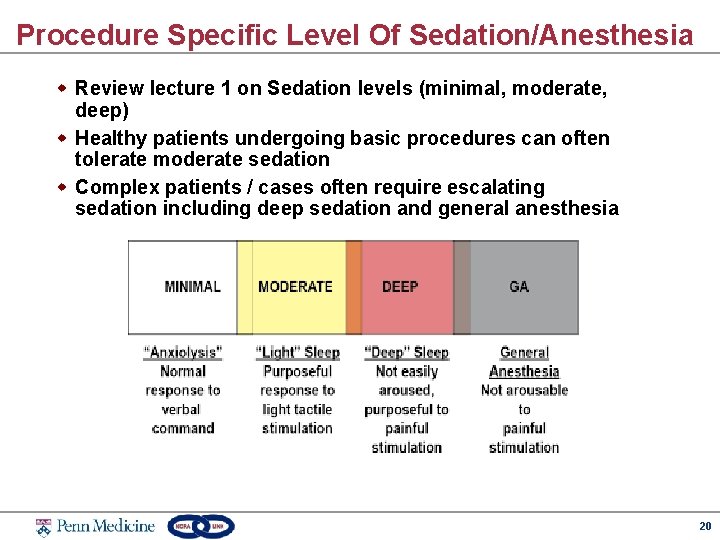
Procedure Specific Level Of Sedation/Anesthesia w Review lecture 1 on Sedation levels (minimal, moderate, deep) w Healthy patients undergoing basic procedures can often tolerate moderate sedation w Complex patients / cases often require escalating sedation including deep sedation and general anesthesia 20
Anesthesia Controversy w Is there a need for anesthesiologists caring for ASA I and II patients undergoing colonoscopies? • Not used routinely in Europe w IV conscious sedation (mild-moderate sedation) using midazolam fentanyl or MD (GI) directed deep sedation with propofol • Large data sets showing safe use 21
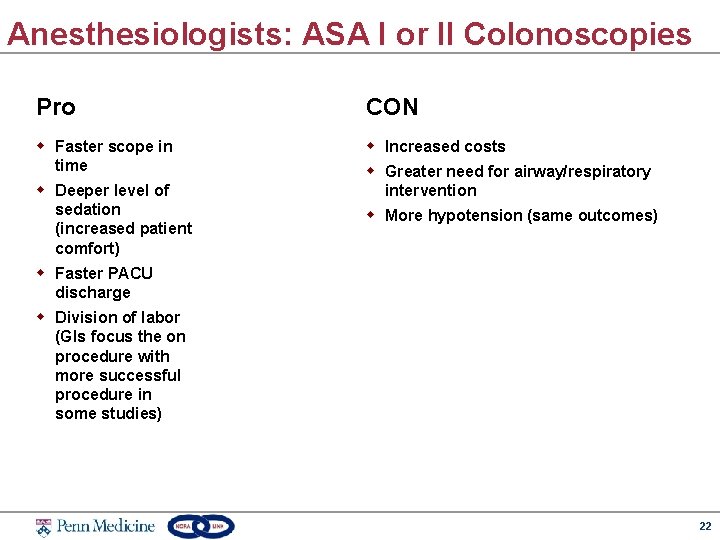
Anesthesiologists: ASA I or II Colonoscopies Pro CON w Faster scope in time w Increased costs w Deeper level of sedation (increased patient comfort) w Greater need for airway/respiratory intervention w More hypotension (same outcomes) w Faster PACU discharge w Division of labor (GIs focus the on procedure with more successful procedure in some studies) 22
Specific Issues Impacting Care w Colonoscopy bowel prep • Hypovolemia, electrolyte abnormalities, nausea/vomiting, patient discomfort w High volume, rapid turnover • Efficiency while keeping patient safety w Global NORA issues • less resources, remote proximity from anesthesia staff with identical OR standards 23
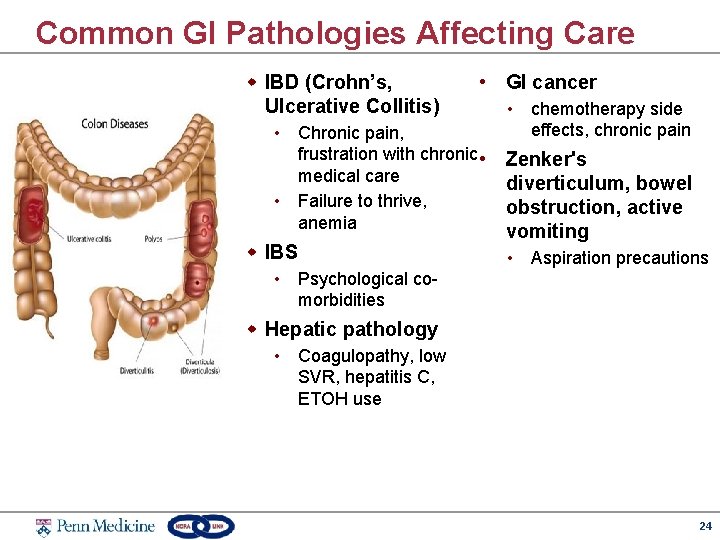
Common GI Pathologies Affecting Care w IBD (Crohn’s, Ulcerative Collitis) • GI cancer • Chronic pain, frustration with chronic • medical care • Failure to thrive, anemia w IBS • chemotherapy side effects, chronic pain Zenker's diverticulum, bowel obstruction, active vomiting • Aspiration precautions • Psychological comorbidities w Hepatic pathology • Coagulopathy, low SVR, hepatitis C, ETOH use 24

Co-Morbidity Specific Issues w Obstructive Sleep Apnea/ Heart Failure Obesity • Avoid hypercarbia/hypoxia • Sensitivity to anesthetics which increases PVR, ensure leading to decreased adequate SVR (so SVR is not oropharyngeal tone and upper < PVR) airway obstruction • Low Left Ventricular EF w High dose chronic opioid therapy • Avoid high doses of • Lower pain threshold, higher myocardial depressants anesthetic requirements, • Seizure disorder greater risk for post-op • Low - moderate doses may complications increase risk of severe myoclonus or (rare) seizure w Pulmonary Hypertension, Right 25
26