Child Care and Protection Act 3 of 2015

- Slides: 27
Child Care and Protection Act 3 of 2015 Chapter 18 Ministry of Gender Equality and Child Welfare Legal Assistance Centre
1. Overview • The Child Care and Protection Act applies the principle of child participation to medical interventions, surgical operations and HIV testing. • It sets criteria for determining when children are sufficiently mature to make independent or assisted decisions on medical issues. • It also sets special rules for consent to medical examinations of children who may have been abused or neglected.
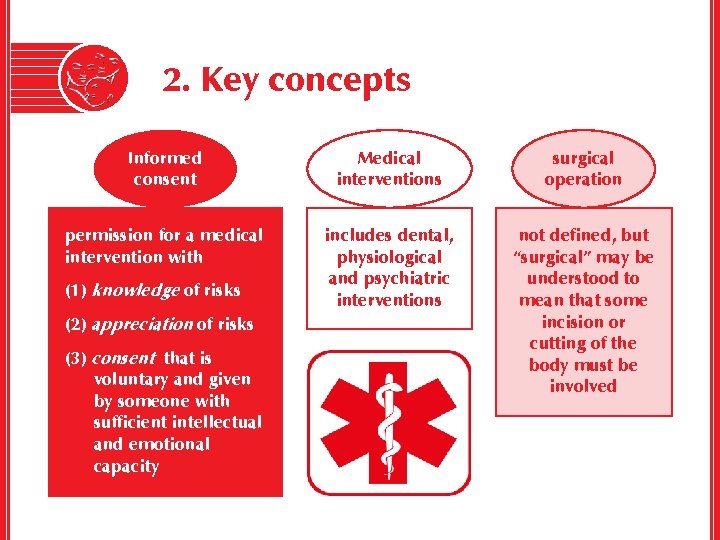
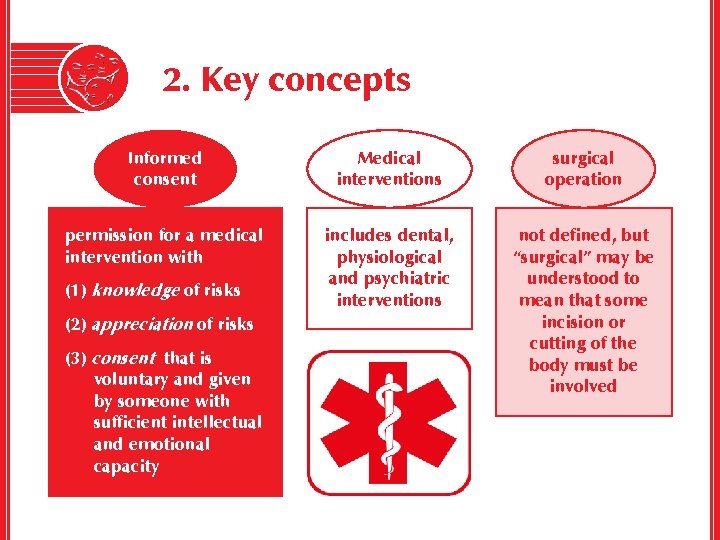
2. Key concepts Informed consent Medical interventions surgical operation permission for a medical intervention with includes dental, physiological and psychiatric interventions not defined, but “surgical” may be understood to mean that some incision or cutting of the body must be involved (1) knowledge of risks (2) appreciation of risks (3) consent that is voluntary and given by someone with sufficient intellectual and emotional capacity
3. International framework Convention on the Rights of the Child • Art 24(1): right of child to enjoyment of highest attainable standard of health and access to health care services • Art 12: child participation • decisions about health care should recognise children’s evolving capacity to take responsibility for their own health and development
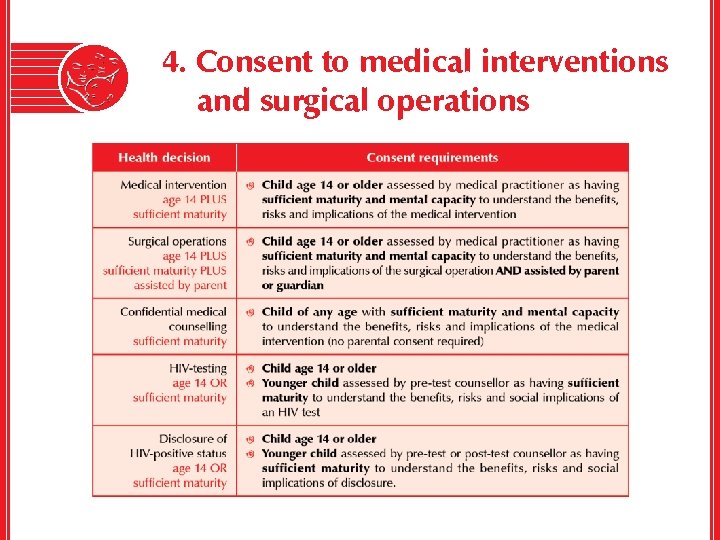
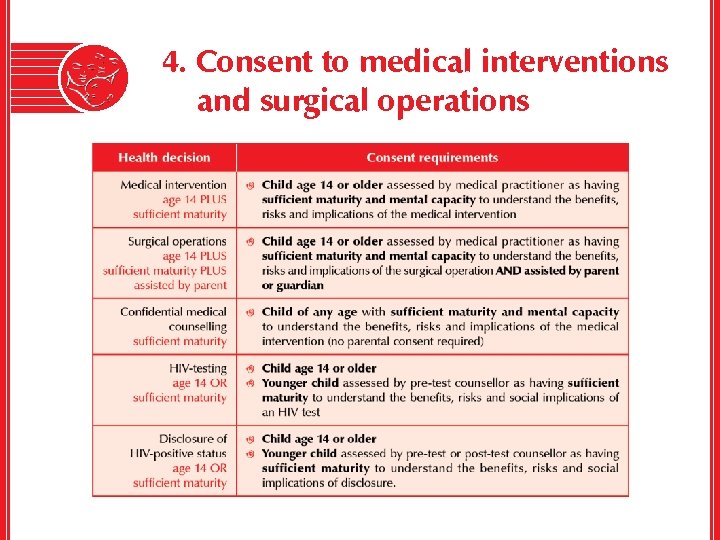
4. Consent to medical interventions and surgical operations
Who assesses a child’s decision-making capacity? The medical practitioner assesses the child’s capacity: l well-placed to assess the child’s understanding of the particular medical intervention l likely to be objective about the child’s decision-making capacity l avoids complicated procedures which might operate as barriers to a child’s health care.
Who decides when the child lacks decision-making capacity? If a child lacks capacity to give independent consent, the decision rests with the child’s parent or guardian. If a child has no parent or guardian, the child’s care-giver can give consent in their place. BUT the parent, guardian or care-giver must give due consideration to the views of the child is able to express an informed view.
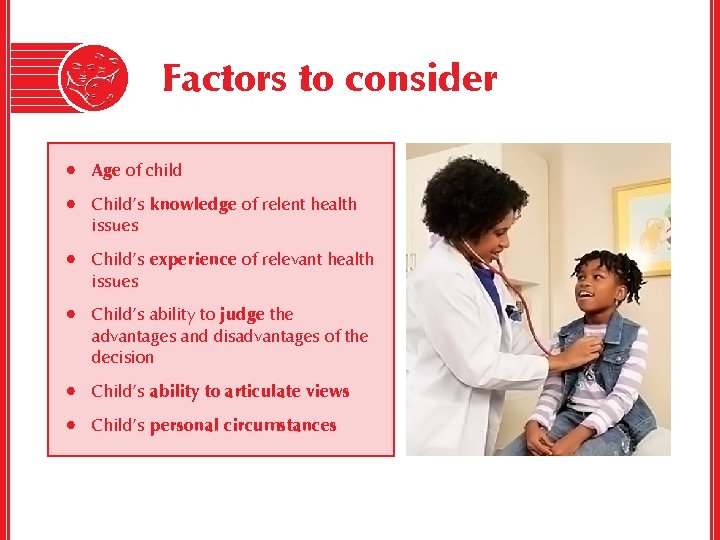
Factors to consider • Age of child • Child’s knowledge of relent health issues • Child’s experience of relevant health issues • Child’s ability to judge the advantages and disadvantages of the decision • Child’s ability to articulate views • Child’s personal circumstances
Access to contraceptives Not explicitly addressed, but some contraceptives = “medical intervention” National Policy on Sexual, Reproductive and Child Health (2013) “ 20. All persons who are sexually active, regardless of age or marital status, shall have the right to be fully informed about available family planning options and methods, and shall have the right to receive the family-planning method of their choice. 21. Adolescents [ages 10 -19] can access sexual and reproductive health services including family planning and STI services without parental consent after thorough counselling. ”
Substituted consent in non-emergency situations Lack of consent by parent, guardian or care-giver: (1) unreasonably refuses consent (2) incapable of giving consent (3) cannot readily be traced (4) deceased. Lack of consent by child: Child is competent but – (1) unreasonably refuses consent (2) is unable to give consent (eg unconscious). Any person with an interest in the child’s well-being can ask the Minister to give consent. If the Minister refuses, any person with an interest in the child’s wellbeing can apply to the children’s court for consent.
Refusing consent on the grounds of religious or other beliefs A parent, guardian or care-giver may NOT refuse consent to a medical intervention on a child on the grounds of religious or other beliefs UNLESS that parent, guardian or caregiver can show that there is a medically accepted alternative. A parent cannot impose his or her personal beliefs on a child in a way that is contrary to the child’s best interests, or in a way that might violate the child’s constitutional right to life.
Emergencies The Act does not use the term “emergency”, but this is a short way to describe a situation where: (1) a medical intervention or surgical operation is necessary to preserve the life of a child or to save a child from serious or lasting physical harm or disability AND (2) the situation is so urgent that the medical intervention or surgical operation should not be delayed in order to obtain the usual consent.
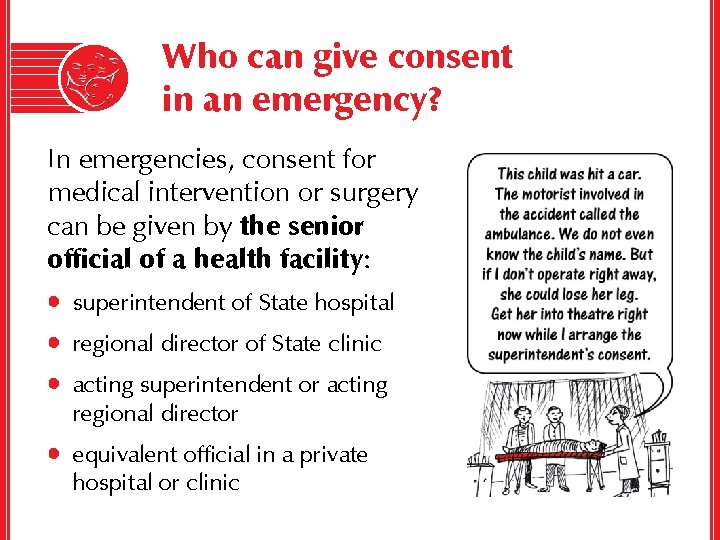
Who can give consent in an emergency? In emergencies, consent for medical intervention or surgery can be given by the senior official of a health facility: • superintendent of State hospital • regional director of State clinic • acting superintendent or acting regional director • equivalent official in a private hospital or clinic
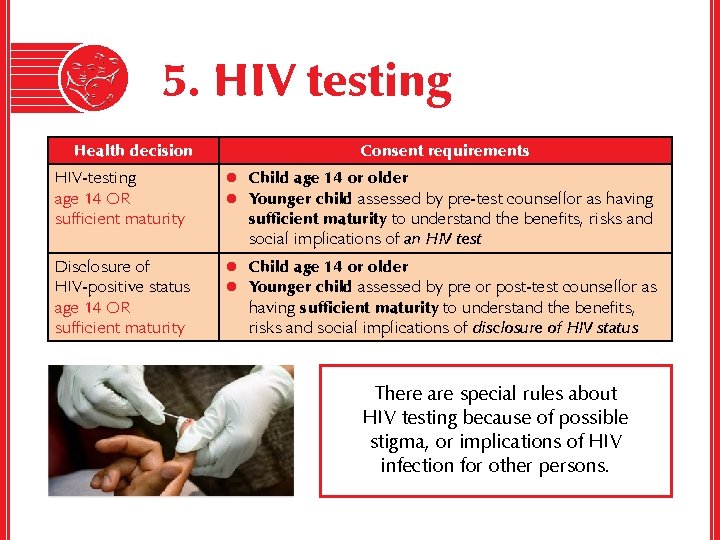
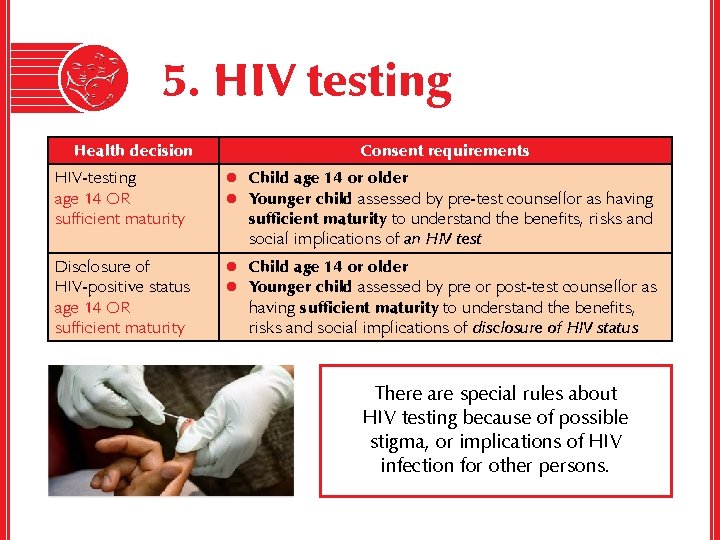
5. HIV testing Health decision Consent requirements HIV-testing age 14 OR sufficient maturity l Child age 14 or older l Younger child assessed by pre-test counsellor as having Disclosure of HIV-positive status age 14 OR sufficient maturity l Child age 14 or older l Younger child assessed by pre or post-test counsellor as sufficient maturity to understand the benefits, risks and social implications of an HIV test having sufficient maturity to understand the benefits, risks and social implications of disclosure of HIV status There are special rules about HIV testing because of possible stigma, or implications of HIV infection for other persons.
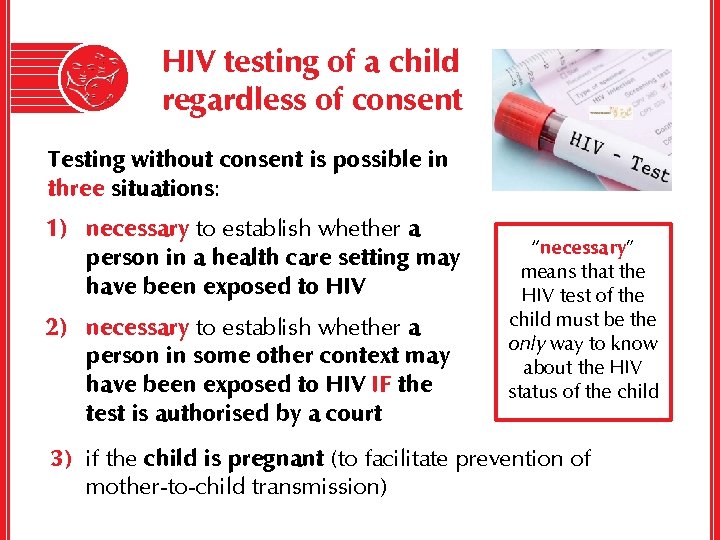
HIV testing of a child regardless of consent Testing without consent is possible in three situations: 1) necessary to establish whether a person in a health care setting may have been exposed to HIV 2) necessary to establish whether a person in some other context may have been exposed to HIV IF the test is authorised by a court “necessary” means that the HIV test of the child must be the only way to know about the HIV status of the child 3) if the child is pregnant (to facilitate prevention of mother-to-child transmission)
Pre- and post-test counselling No matter what circumstances lead to an HIV test: • the child must receive pre- and post-test counselling UNLESS child is too young to benefit • the child’s parent, guardian or care-giver must also receive pre- and post-test counselling where he or she has knowledge of the test o A parent, guardian or care-giver who is the decision-maker will obviously have this knowledge. o Where the child has the required age or capacity to be the decision-maker on testing and disclosure, the decision on whether to inform the parent or guardian of the test or its outcomes rests with the child.
Disclosure of HIV status l Why are there separate rules for consent to testing and consent to disclosure? It is because these issues do not always arise together. o For example, a child who was tested some time ago with parental consent might now want to disclose the test results to access HIV treatment independently, regardless of the parent’s views on this. l A child who is competent to give consent to an HIV test is almost certainly competent to consent to disclosure of his or her HIV status. A child who understands the implications of HIV testing will also understand the implications of disclosure of the test results.
Disclosure without consent 1) within the scope of powers and duties in terms of the Child Care and Protection Act or any other law 2) necessary to carry out the provisions of the Child Care and Protection Act 3) for the purpose of legal proceedings 4) in terms of a court order Example: adoption report prepared by social worker
General rules on HIV issues The general rules about consent to medical intervention also apply to HIV testing, treatment and disclosure. l If the child is not competent to make the decision, it lies with the child’s parent or guardian. l If there is no parent or guardian, then the care-giver can consent. l Minister can consent (a) if parent, guardian or care-giver unreasonably refuses to give consent, is incapable of giving consent, cannot readily be traced or is deceased (2) if child is competent to give consent but unreasonably refuses to do so, or is unable to do so. l If Minister refuses consent, children’s court can give consent.
Confidentiality & disclosure Unlawful disclosure of a child’s HIV-positive status is a crime punishable by a fine of up to N$20 000 or imprisonment for up to five years, or both.
6. Consent by child-parents A child-parent who is competent to consent in respect of himself or herself is also competent to consent in respect of his or her child. • If the child-parent does NOT have the required capacity for independent decision-making, then the child-parent’s parent or guardian would hold the decision-making power for the child of the child-parent • The rules on emergency situations and the rules on addressing lack of consent would apply in the usual way to decision-making in this situation.
7. Health care decision-making: powers of alternative care-givers The care-giver of a child placed in alternative care by a court order has certain health related duties: • to obtain basic medical intervention for child if needed • to ensure that the child obtains a surgical operation IF it is so urgent that deferring it to consult with the child’s parent would prejudice the child’s health or welfare.
8. Examination and treatment of abused or neglected child There is an exception to the general rules on consent if the parent or care-giver may be responsible for child abuse or neglect, or may want to protect some other person who was responsible
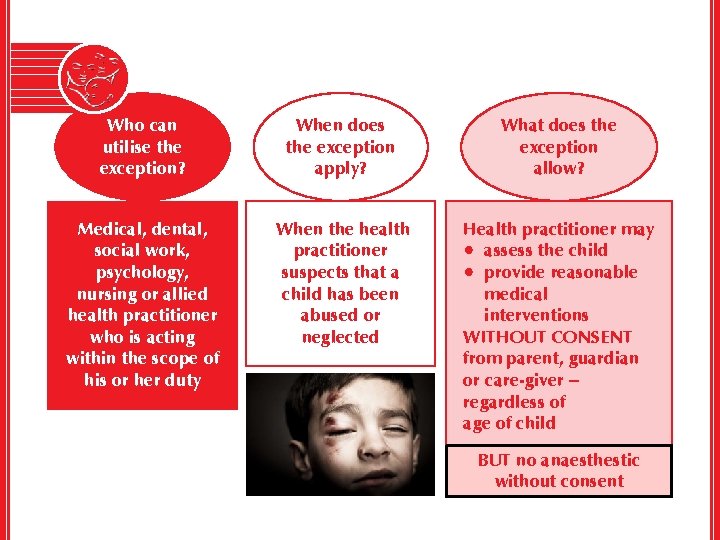
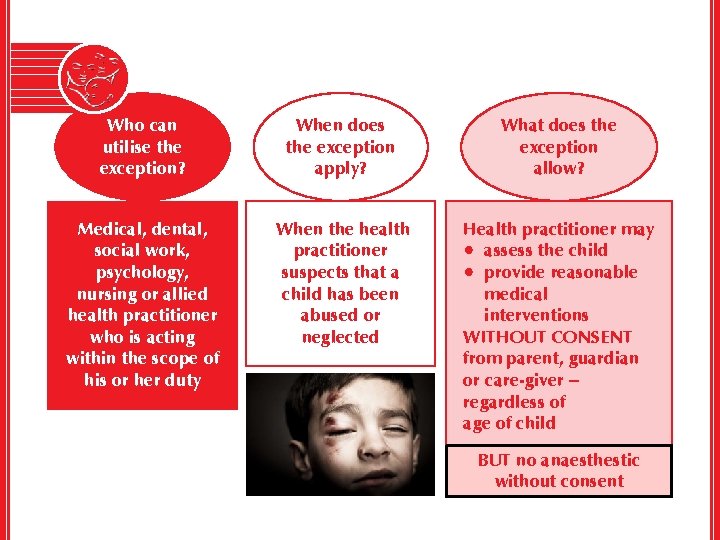
Who can utilise the exception? When does the exception apply? What does the exception allow? Medical, dental, social work, psychology, nursing or allied health practitioner who is acting within the scope of his or her duty When the health practitioner suspects that a child has been abused or neglected Health practitioner may • assess the child • provide reasonable medical interventions WITHOUT CONSENT from parent, guardian or care-giver – regardless of age of child BUT no anaesthestic without consent
Guidelines for the examination of an abused or neglected child ü ü ü ü address the child in a language which the child understands allow the child to be accompanied by a support person treat the child with empathy, care and understanding respect child’s right to privacy and confidentiality examine the child in a child-friendly environment conduct assessment or examination in private respect the child’s dignity
Mandatory reporting duty People who perform professional or official duties involving children are required to report any suspicion that a child is or may be in need of protective services. l must alert police or a State-employed social worker l failure to report is a crime punishable by a fine of up to N$20 000 or imprisonment for up to five years, or both

 Child care and protection act 3 of 2015
Child care and protection act 3 of 2015 Children rights and responsibilities
Children rights and responsibilities Child protection and toy safety act
Child protection and toy safety act Child protection reform amendment act 2017
Child protection reform amendment act 2017 Care and protection of children act
Care and protection of children act Handling information in care settings
Handling information in care settings Section 47 child care act
Section 47 child care act Safeguarding and child protection the essentials
Safeguarding and child protection the essentials Primary secondary tertiary medical care
Primary secondary tertiary medical care Courage child protection
Courage child protection Types of child protection
Types of child protection Types of child protection
Types of child protection Child protection case management tools
Child protection case management tools Types of child protection
Types of child protection Professional curiousity
Professional curiousity Community based child protection mechanisms
Community based child protection mechanisms Child protection training materials
Child protection training materials Child protection awareness training
Child protection awareness training Child protection minimum standards
Child protection minimum standards Child protection policy in schools example
Child protection policy in schools example Child protection policy
Child protection policy Act 1 act 2 act 3
Act 1 act 2 act 3 Domestic and family violence protection act 2012
Domestic and family violence protection act 2012 S68r family law act
S68r family law act 이진트리 복사 순회
이진트리 복사 순회 What is the children’s safety on motorcycles act of 2015?
What is the children’s safety on motorcycles act of 2015? Terrorist travel prevention act
Terrorist travel prevention act Companies act fiji
Companies act fiji