Chapter 3 Treatment guidelines for NSCLC that does
- Slides: 3
Chapter 3 Treatment guidelines for NSCLC that does not have targetable driver mutations
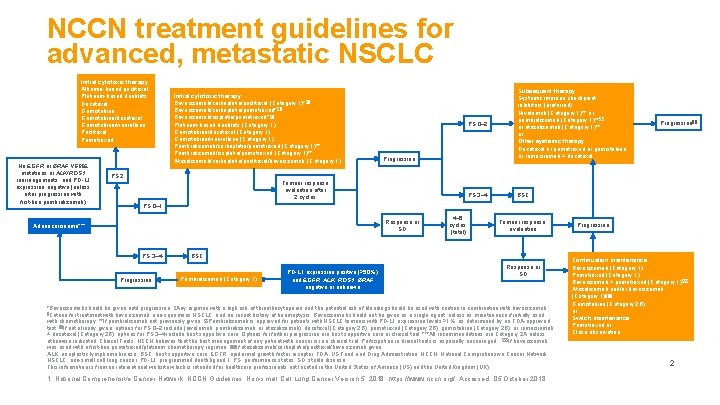
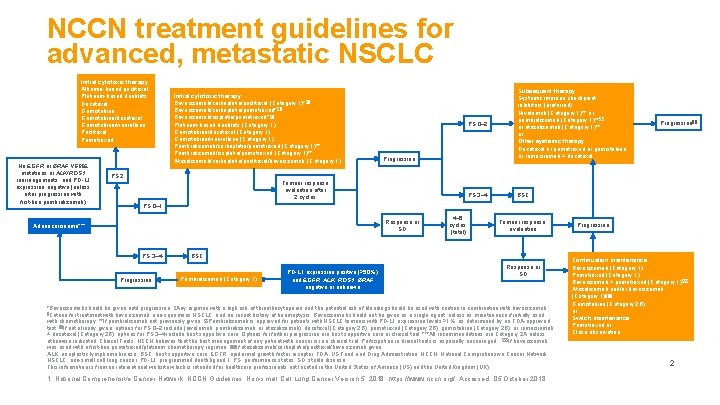
NCCN treatment guidelines for advanced, metastatic NSCLC Initial cytotoxic therapy: Albumin-bound paclitaxel Platinum-based doublets Docetaxel Gemcitabine/docetaxel Gemcitabine/vinorelbine Paclitaxel Pemetrexed No EGFR or BRAF V 600 E mutations or ALK/ROS 1 rearrangements, and PD-L 1 expression negative (unless after progression with first-line pembrolizumab) Initial cytotoxic therapy: Bevacizumab/carboplatin/paclitaxel (Category 1)*§¶ Bevacizumab/carboplatin/pemetrexed* §¶ Bevacizumab/cisplatin/pemetrexed* §¶ Platinum-based doublets (Category 1) Gemcitabine/docetaxel (Category 1) Gemcitabine/vinorelbine (Category 1) Pembrolizumab/carboplatin/pemetrexed (Category 1)** Pembrolizumab/cisplatin/pemetrexed (Category 1)** Atezolizumab/carboplatin/paclitaxel/bevacizumab (Category 1) PS 2 PS 0– 2 Subsequent therapy: Systemic immune checkpoint inhibitors (preferred) Nivolumab (Category 1)** or pembrolizumab (Category 1)**§§ or atezolizumab (Category 1)** or Other systemic therapy: Docetaxel or pemetrexed or gemcitabine or ramucirumab + docetaxel PS 3– 4 BSC Progression Tumour response evaluation after 2 cycles Progression ¶¶ PS 0– 1 Response or SD Adenocarcinoma*** PS 3– 4 Progression 4– 6 cycles (total) Tumour response evaluation BSC Pembrolizumab (Category 1) PD-L 1 expression positive (≥ 50%) and EGFR, ALK, ROS 1, BRAF negative or unknown Response or SD *Bevacizumab should be given until progression; §Any regimen with a high risk of thrombocytopenia and the potential risk of bleeding should be used with caution in combination with bevacizumab; ¶Criteria for treatment with bevacizumab: non-squamous NSCLC, and no recent history of haemoptysis. Bevacizumab should not be given as a single agent, unless as maintenance if initially used with chemotherapy; **If pembrolizumab not previously given; §§Pembrolizumab is approved for patients with NSCLC tumours with PD-L 1 expression levels ≥ 1%, as determined by an FDA-approved test; ¶¶If not already given, options for PS 0– 2 include (nivolumab, pembrolizumab, or atezolizumab), docetaxel (Category 2 B), pemetrexed (Category 2 B), gemcitabine (Category 2 B), or ramucirumab + docetaxel (Category 2 B); options for PS 3– 4 include best supportive care. Options for further progression are best supportive care or clinical trial; ***All recommendations are Category 2 A unless otherwise indicated. Clinical Trials: NCCN believes that the best management of any patient with cancer is in a clinical trial. Participation in clinical trials is especially encouraged; §§§If bevacizumab was used with a first-line pemetrexed/platinum chemotherapy regimen; ¶¶¶If atezolizumab/carboplatin/paclitaxel/bevacizumab given. ALK, anaplastic lymphoma kinase; BSC, best supportive care; EGFR, epidermal growth factor receptor; FDA, US Food and Drug Administration; NCCN, National Comprehensive Cancer Network; NSCLC, non-small cell lung cancer; PD-L 1, programmed death ligand 1; PS, performance status; SD, stable disease. This information is from an international website which is intended for healthcare professionals not located in the United States of America (US) and the United Kingdom (UK). 1. National Comprehensive Cancer Network. NCCN Guidelines: Non-small Cell Lung Cancer Version 5. 2018. https: //www. nccn. org/. Accessed: 05 October 2018. Progression Continuation maintenance: Bevacizumab (Category 1) Pemetrexed (Category 1) Bevacizumab + pemetrexed (Category 1)§§§ Atezolizumab and/or bevacizumab (Category 1)¶¶¶ Gemcitabine (Category 2 B) or Switch maintenance: Pemetrexed or Close observation 2
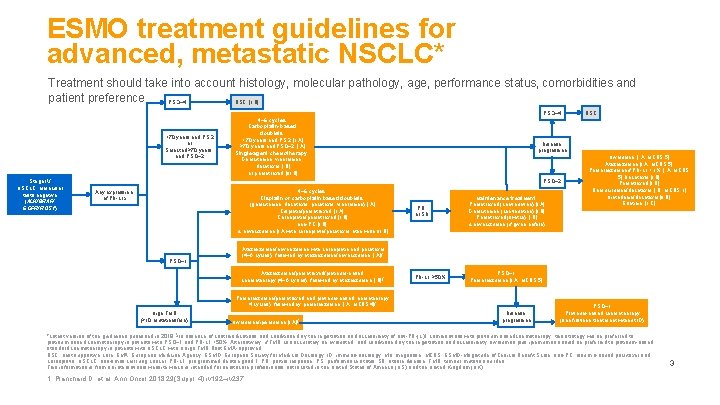
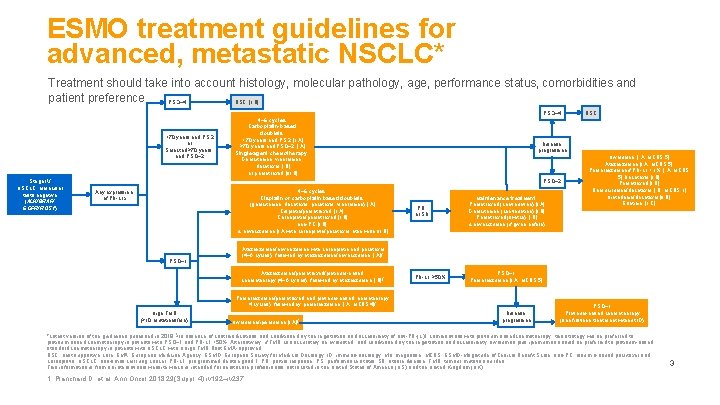
ESMO treatment guidelines for advanced, metastatic NSCLC* Treatment should take into account histology, molecular pathology, age, performance status, comorbidities and patient preference PS 3– 4 BSC [II, B] PS 3– 4 <70 years and PS 2 or Selected ≥ 70 years and PS 0– 2 Stage IV NSCLC: Molecular tests negative (ALK/BRAF/ EGFR/ROS 1) 4– 6 cycles: Carboplatin-based doublets: <70 years and PS 2 [II, A] ≥ 70 years and PS 0– 2 [I, A] Single-agent chemotherapy: Gemcitabine, vinorelbine, docetaxel [I, B] or pemetrexed [III, B] Disease progression PS 0– 2 4– 6 cycles: Cisplatin or carboplatin based doublets: (gemcitabine, docetaxel, paclitaxel, vinorelbine) [I, A] Cisplatin/pemetrexed [II, A] Carboplatin/pemetrexed [II, B] nab-PC [I, B] ± bevacizumab [I, A with carboplatin/paclitaxel, otherwise III, B] Any expression of PD-L 1§ PS 0– 1 PR or SD Maintenance treatment: Pemetrexed (continuation) [I, A] Gemcitabine (continuation) [I, B] Pemetrexed (switch) [I, B] ± bevacizumab (if given before) PD-L 1 ≥ 50% PS 0– 1 Pembrolizumab [I, A; MCBS 5] Nivolumab [I, A; MCBS 5] Atezolizumab [I, A; MCBS 5] Pembrolizumab if PD-L 1 >1% [I, A; MCBS 5] Docetaxel [I, B] Pemetrexed [I, B] Ramucirumab/docetaxel [I, B; MCBS 1] Nintedanib/docetaxel [II, B] Erlotinib [II, C] Atezolizumab/bevacizumab with carboplatin and paclitaxel (4– 6 cycles), followed by atezolizumab/bevacizumab [I, A]¶ Atezolizumab/pemetrexed/platinum-based chemotherapy (4– 6 cycles), followed by atezolizumab [I, B]¶ Pembrolizumab/pemetrexed and platinum-based hemotherapy 4 cycles), followed by pembrolizumab [I, A; MCBS 4]¶ High TMB (≥ 10 mutations/Mb) BSC Nivolumab/ipilimumab [I, A]¶ Disease progression PS 0– 1 Platinum-based chemotherapy (see first-line treatment without IO) *Latest version of the guidelines published in 2018; §In absence of contraindications and conditioned by the registration and accessibility of anti-PD-(L)1 combinations with platinum-based chemotherapy, this strategy will be preferred to platinum-based chemotherapy in patients with PS 0– 1 and PD-L 1 <50%. Alternatively, if TMB can accurately be evaluated, and conditioned by the registration and accessibility, nivolumab plus ipilimumab should be preferred to platinum-based standard chemotherapy in patients with NSCLC with a high TMB; ¶not EMA-approved. BSC, best supportive care; EMA, European Medicine Agency; ESMO, European Society for Medical Oncology; IO, immuno-oncology; Mb, megabase; MCBS, ESMO-Magnitude of Clinical Benefit Scale; nab-PC, albumin-bound paclitaxel and carboplatin; NSCLC, non-small cell lung cancer; PD-L 1, programmed death ligand 1; PR, partial response; PS, performance status; SD, stable disease, TMB, tumour mutation burden. This information is from an international website which is intended for healthcare professionals not located in the United States of America (US) and the United Kingdom (UK). 1. Planchard D, et al. Ann Oncol 2018; 29(Suppl. 4): iv 192–iv 237. 3