CASE 8 o yr old gentleman with PMH

- Slides: 19
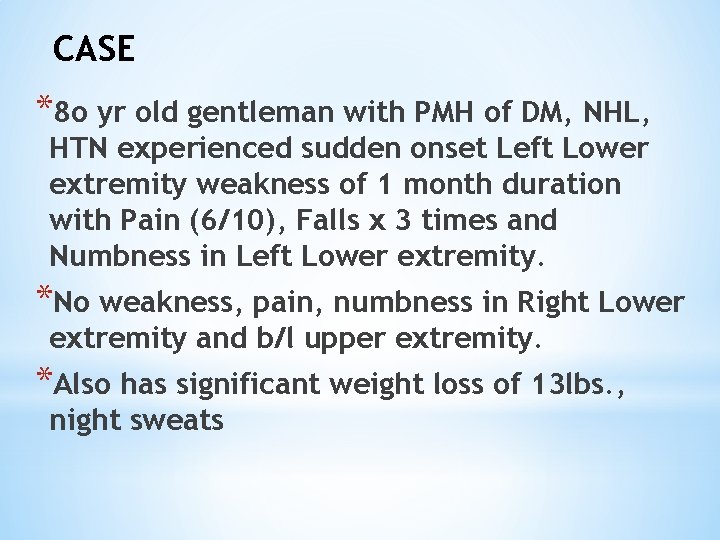
CASE *8 o yr old gentleman with PMH of DM, NHL, HTN experienced sudden onset Left Lower extremity weakness of 1 month duration with Pain (6/10), Falls x 3 times and Numbness in Left Lower extremity. *No weakness, pain, numbness in Right Lower extremity and b/l upper extremity. *Also has significant weight loss of 13 lbs. , night sweats
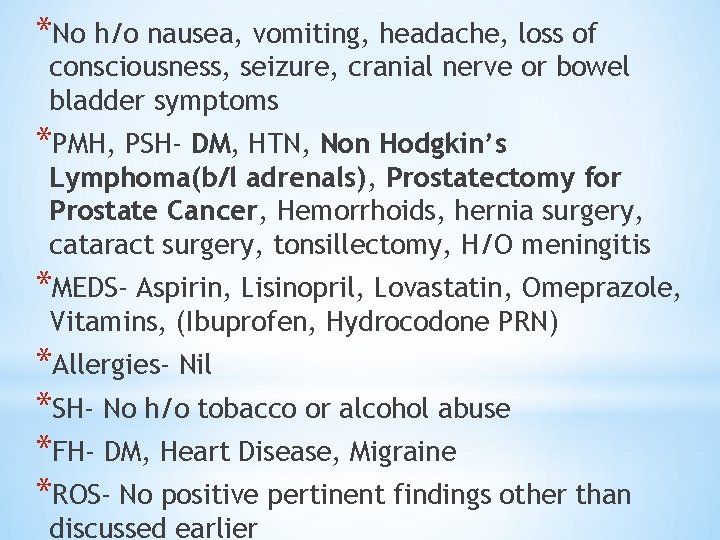
*No h/o nausea, vomiting, headache, loss of consciousness, seizure, cranial nerve or bowel bladder symptoms *PMH, PSH- DM, HTN, Non Hodgkin’s Lymphoma(b/l adrenals), Prostatectomy for Prostate Cancer, Hemorrhoids, hernia surgery, cataract surgery, tonsillectomy, H/O meningitis *MEDS- Aspirin, Lisinopril, Lovastatin, Omeprazole, Vitamins, (Ibuprofen, Hydrocodone PRN) *Allergies- Nil *SH- No h/o tobacco or alcohol abuse *FH- DM, Heart Disease, Migraine *ROS- No positive pertinent findings other than discussed earlier
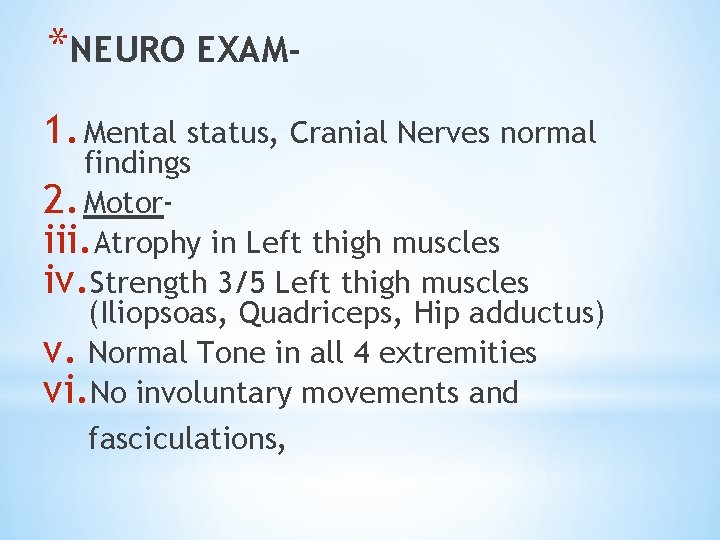
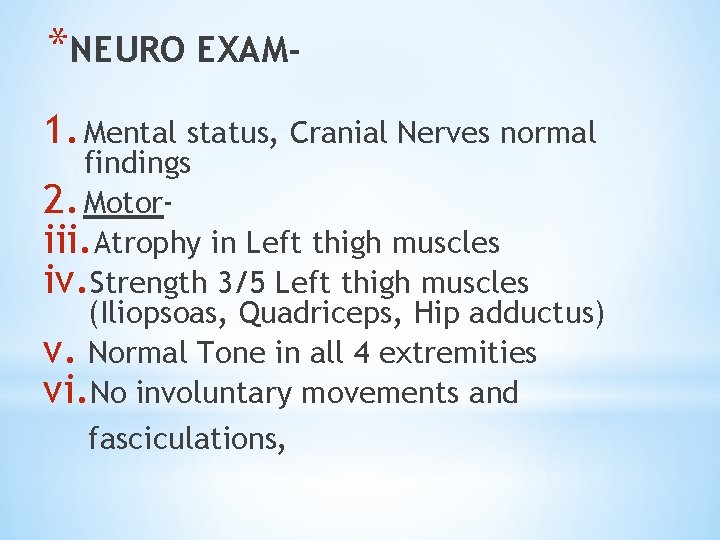
*NEURO EXAM 1. Mental status, Cranial Nerves normal findings 2. Motoriii. Atrophy in Left thigh muscles iv. Strength 3/5 Left thigh muscles (Iliopsoas, Quadriceps, Hip adductus) v. Normal Tone in all 4 extremities vi. No involuntary movements and fasciculations,
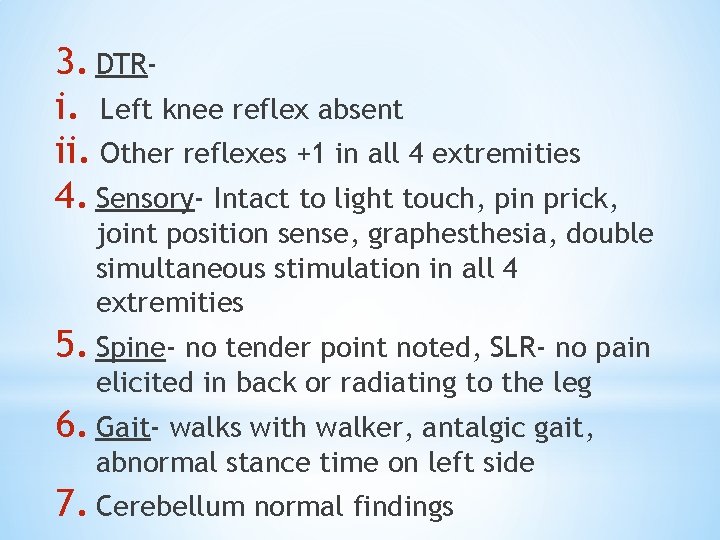
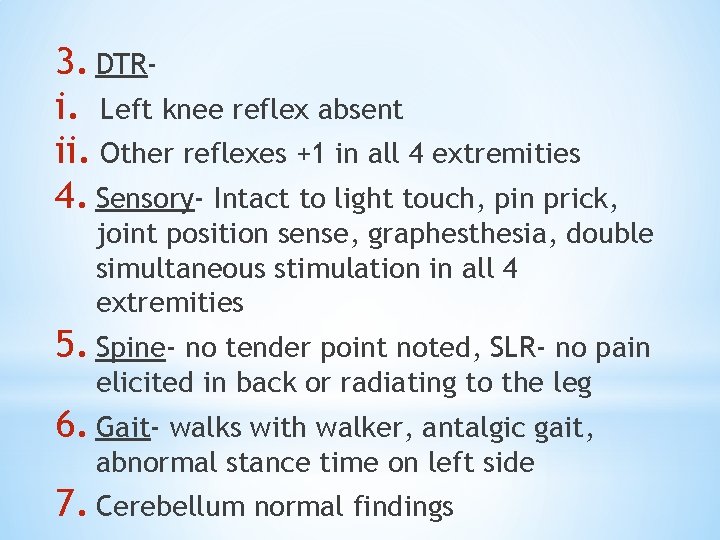
3. DTRi. Left knee reflex absent ii. Other reflexes +1 in all 4 extremities 4. Sensory- Intact to light touch, pin prick, joint position sense, graphesthesia, double simultaneous stimulation in all 4 extremities 5. Spine- no tender point noted, SLR- no pain elicited in back or radiating to the leg 6. Gait- walks with walker, antalgic gait, abnormal stance time on left side 7. Cerebellum normal findings
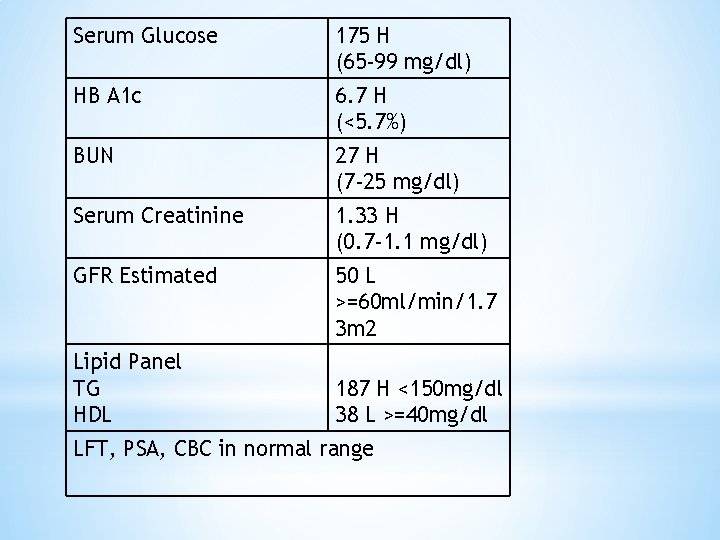
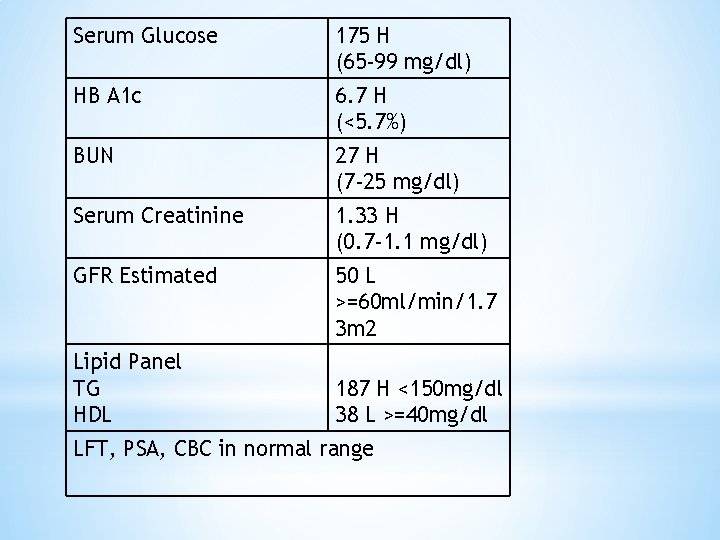
Serum Glucose 175 H (65 -99 mg/dl) HB A 1 c 6. 7 H (<5. 7%) BUN 27 H (7 -25 mg/dl) Serum Creatinine 1. 33 H (0. 7 -1. 1 mg/dl) GFR Estimated 50 L >=60 ml/min/1. 7 3 m 2 Lipid Panel TG HDL 187 H <150 mg/dl 38 L >=40 mg/dl LFT, PSA, CBC in normal range
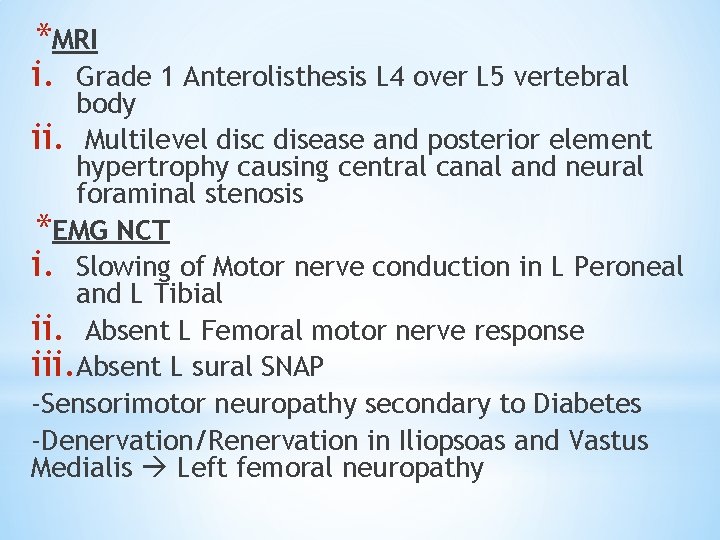
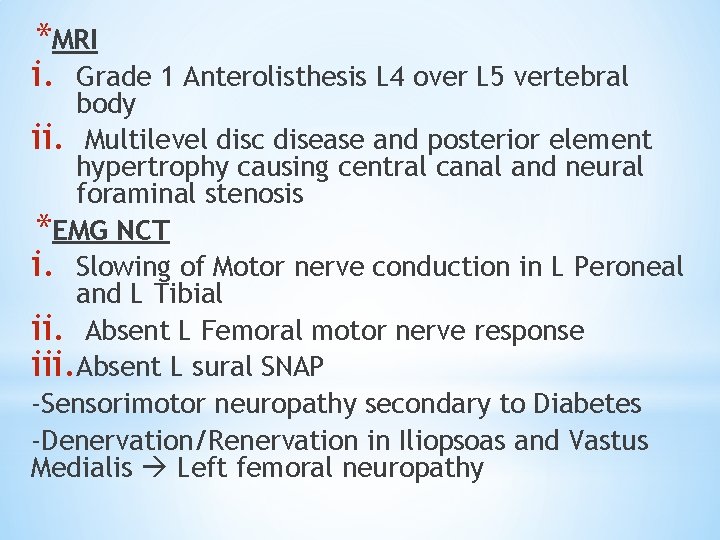
*MRI i. Grade 1 Anterolisthesis L 4 over L 5 vertebral body ii. Multilevel disc disease and posterior element hypertrophy causing central canal and neural foraminal stenosis *EMG NCT i. Slowing of Motor nerve conduction in L Peroneal and L Tibial ii. Absent L Femoral motor nerve response iii. Absent L sural SNAP -Sensorimotor neuropathy secondary to Diabetes -Denervation/Renervation in Iliopsoas and Vastus Medialis Left femoral neuropathy
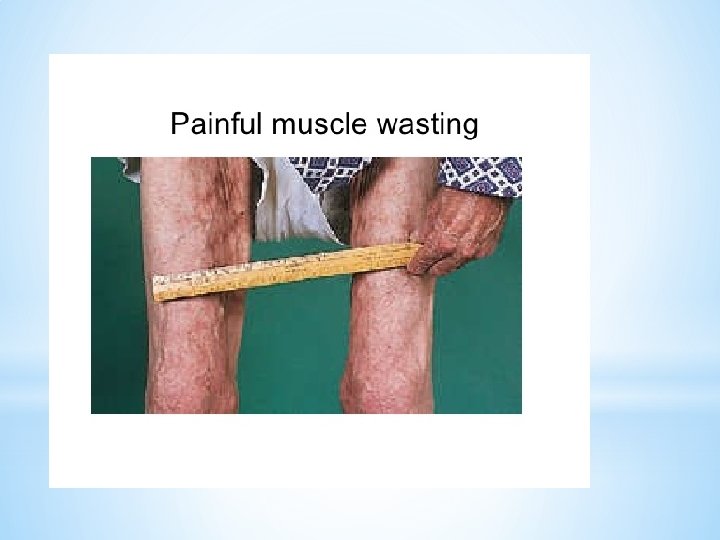
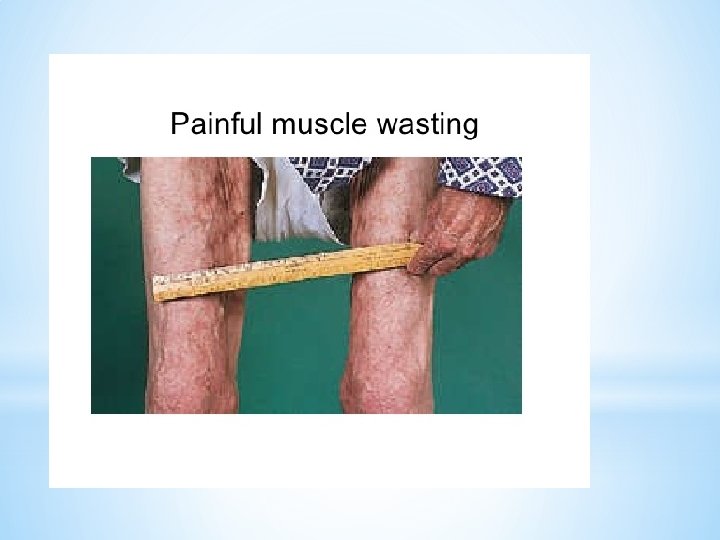
(DIABETIC AMYOTROPHY) weakness followed by wasting of pelvifemoral muscles, either unilaterally or bilaterally, with associated pain
*Diabetes Mellitus Type 2 then Type 1 *Acute sudden presentation over 2 to 3 weeks *Older male *The typical symptoms are fairly sudden onset and usually occur on one side of the body but may involve both sides
CLINICAL FEATURES *Proximal muscle weakness and atrophy in the quadriceps, hamstring, gluteal, hip adductors/abductors, and iliopsoas muscles. *Excruciating Pain *Falls *No sensory impairment, mild sensory loss may be observed in patients with coexisting chronic distal sensorimotor polyneuropathy. *The patellar tendon reflexes are typically diminished or absent, and the ankle reflexes usually normal *Weight loss
PATHOPHYSIOLOGY *Exact pathogenesis remains unknown. *Hyperglycemia may cause metabolic derangements in nerve conduction *Ischemic damage followed by axonal degeneration *Immune-mediated inflammatory processes. Microscopic vasculitis without vessel damage, Perivascular epineural inflammation *The site of the lesion remains controversial; it is theorized that diabetic amyotrophy may result from involvement of multiple sites, such as lumbosacral anterior horn cells, motor roots, plexus, or motor axons to the muscles of the proximal lower limbs
INVESTIGATIONS *Labs- Fasting plasma Glucose, complete blood count, comprehensive metabolic profile, A 1 C, erythrocyte sedimentation rate (ESR), creatine kinase, vitamin B 12, and thyroid-stimulating hormone levels *MRI or CT scan of the lumbosacral spine- To exclude mass lesions and structural disorders such as spinal stenosis and disc buldging
INVESTIGATIONS *EMG, NCT- Electromyography reveals findings consistent with denervation and axonal damage in the proximal muscles in both lower extremities *If clinically indicated, paraneoplastic panel to evaluate for occult malignancy, autoantibodies, cryoglobulins, cerebrospinal fluid analysis, porphyrin titers, and testing for heavy metals *Nerve biopsy- The sural and superficial peroneal nerves are preferred, significant fiber loss in an asymmetric fashion, focal ischemia
DIFFERENTIAL DIAGNOSIS *Anterior horn cell diseases (eg, poliomyelitis) *Polyradiculopathies due to porphyria, amyloid, heavy metal poisoning *Radiation, compression Plexopathy *Neoplasms, chronic inflammatory demyelinating polyneuropathy, Guillain-Barré syndrome, monoclonal gammopathy, inflammatory vasculitis, *Intervertebral disc disease, spinal stenosis *Myopathies, muscular dystrophies *Hypothyroidism, vitamin B 6 or B 12 deficiencies, syphilis, AIDS, Lyme disease * Diabetic neuropathic cachexia- presents with weight loss and lower limb diffuse pain, paresthesias, sensorimotor polyneuropathies but no weakness.
MANAGEMENT *Improves with time and the body may heal it itself. *Pain control Pregabalin, duloxetine, tricyclic antidepressants, antiepileptic drugs, and narcotic analgesics can be helpful. High doses of corticosteroids may lead to improvement of severe pain *Strict glycemic control * Physical therapy *Treatment with IV immunoglobulin or other immuno suppressive drugs is controversial, currently no evidence to support use of immunoglobulins to halt progression and improve symptoms.
PROGNOSIS *The course of diabetic amyo trophy is variable. There is often gradual but incomplete restoration in muscle strength in correlation with aggressive glycemic control and physical therapy. *The majority of patients have residual muscle weakness, absent patellar and/or ankle DTRs, exercise-related pain, stiffness, and difficulty walking or climbing stairs. Full recovery occurs in 10% to 20% of patients.
PROGNOSIS *The severe pain associated with diabetic amyotrophy begins to diminish several months after onset, but residual pain may persist for several years. *Neuropathic pain may be difficult to control in some patients with diabetic amyotrophy. 5
