Association versus causation epidemiology versus the law Part
- Slides: 14
Association versus causation: epidemiology versus the law? Part II – Logic or experience? Thursday 6 th February 2020 DWF London
‘The life of the law has not been logic, it has been experience. ’ - Oliver Wendell Holmes Jr ‘The Common Law’ 1881
Case example – Donna Von Trap (DVT) • Donna Von Trap – 30 years of age. Went to Bangkok for a mid-winter break. Flight duration 11 hours 30 minutes (direct). • Ms. Von Trap noticed pain in her right thigh a week after returning home. She attended A&E where she was diagnosed as having a DVT. • Ms. Von Trap was a healthy 30 -year-old. She had no known risk factors for a DVT.
• Ms. Von Trap seeks to claim under her personal accident insurance policy. • There is an exclusion within the policy for DVTs caused by long haul flights. • The question the court must answer is whether Ms. Von Trap’s DVT was caused by the flight.
• The association between air travel and deep vein thrombosis: Systematic review & meta-analysis Yaser Adi et al BMC Cardiovasc Disord. 2004; 4: 7. • Odds ratio for a risk of a DVT from a long-haul flight is 1. 70
“However, I do agree with Lord Rodger that doubling the risk is not an appropriate test of causation in cases to which the Fairchild exception does not apply. Risk is a forward looking concept – what are the chances that I will get a particular disease in the future? Causation usually looks backwards – what is the probable cause of the disease which I now have? …” Lady Hale, Sienkiewicz v. Greif (UK) Ltd [2011] UKSC 10.
Variation 1 • Same facts except that Ms. Von Trap has a known risk factor - a family history of venous thrombosis. • The Value of Family History as a Risk Indicator for Venous Thrombosis Irene D. Bezemer, MSc; Felix J. M. van der Meer, MD, Ph. D; Jeroen C. J. Eikenboom, MD, Ph. D; et al Arch Intern Med. 2009; 169(6): 610 -615 • A positive family history increased the risk of venous thrombosis more than 2 -fold (odds ratio [95% confidence interval], 2. 2 [1. 9 -2. 6]) and up to 4 -fold (3. 9 [2. 7 -5. 7]) when more than 1 relative was affected.
Questions: • Was the DVT caused or materially contributed to by the flight? • Do we know whether the risk factors are independent of each other? • Would your answer change on the basis that the family history consisted of only her mother who is overweight, a heavy smoker and had varicose veins? • Assuming that the flight and the family history are independent risk factors.
Variation 2 • Ms. Von Trap has just started taking the oral contraceptive pill. She is taking the 4 th generation of the specific pill. • Use of combined oral contraceptives and risk of venous thromboembolism: nested case-control studies using the QResearch and CPRD databases BMJ 2015; 350 doi: (Published 26 May 2015) • 5062 cases of venous thromboembolism from CPRD and 5500 from QResearch were analysed. Current exposure to any combined oral contraceptive was associated with an increased risk of venous thromboembolism (adjusted odds ratio 2. 97, 95% confidence interval 2. 78 to 3. 17) • Low risk – risk is low even though allows for increase in risk. • The number of extra cases of venous thromboembolism per year per 10 000 treated women was lowest for levonorgestrel (6, 95% confidence interval 5 to 7) and norgestimate (6, 5 to 8), and highest for desogestrel (14, 11 to 17) and cyproterone (14, 11 to 17).
"If it is a known fact that a particular type of act (or omission) is likely to have a particular effect, proof that the Defendant was responsible for such an act (or omission) and that the Claimant had what is the usual effect will be powerful evidence from which to infer causation, without necessarily requiring a detailed scientific explanation for the link. But inferring causation from proof of heightened risk is never an exercise to apply mechanistically. A doubled tiny risk will still be very small. " Lord Toulson, Williams v. Bermuda Hospitals Board [2016] UKPC 4.
Questions: • Assuming independent risk factors, would you find that the flight caused or materially contributed to the DVT? • If not, would you find that the contraceptive pill caused or materially contributed to the DVT?
Variation 3 • Varicose veins – Ms. Von Trapp has been suffering from varicose veins for several years. • Association of Varicose Veins With Incident Venous Thromboembolism and Peripheral Artery Disease Chang et al JAMA 2018 Feb 27; 319(8): 807 -817 • There were 212 84 patients in the varicose veins group (mean [SD] age, 54. 5 [16. 0] years; 69. 3% women) and 212 84 in the control group (mean [SD] age, 54. 3 [15. 6] years; 70. 3% women). The median follow-up duration was 7. 5 years for DVT, 7. 8 years for PE, and 7. 3 years for PAD for patients with varicose veins, and for the control group, followup duration was 7. 6 years for DVT, 7. 7 years for PE, and 7. 4 years for PAD. The varicose veins group had higher incidence rates than the control group for DVT (6. 55 vs 1. 23 per 1000 person-years [10 60 vs 1980 cases]; absolute risk difference [ARD], 5. 32 [95% CI, 5. 18 -5. 46]), for PE (0. 48 for the varicose veins group vs 0. 28 for the control group per 1000 person-years [793 vs 451 cases]; ARD, 0. 20 [95% CI, 0. 16 -0. 24]), and for PAD (10. 73 for the varicose veins group vs 6. 22 for the control group per 1000 person-years [16 15 vs 9709 cases]; ARD, 4. 51 [95% CI, 4. 31 -4. 71]). The hazard ratios for the varicose veins group compared with the control group were 5. 30 (95% CI, 5. 05 -5. 56) for DVT, 1. 73 (95% CI, 1. 54 -1. 94) for PE, and 1. 72 (95% CI, 1. 68 -1. 77) for PAD.
Questions: • Is the risk from varicose veins relevant to the assessment of causation? • DVT occurred within 1 week. Therefore the risk from varicose veins in the week is divisible by 52 as the data relates to ‘person-years’? • Absolute risk of someone with VV having a DVT over a 1 -week period is therefore 0. 01%? • Is this de minimis?
Concluding remarks
 Web causation of disease
Web causation of disease Proximate cause and ultimate cause
Proximate cause and ultimate cause Polygyny in animals
Polygyny in animals Rumus odds ratio
Rumus odds ratio Spurious association in epidemiology
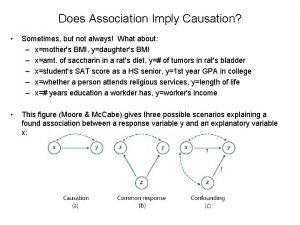
Spurious association in epidemiology Association and causation
Association and causation Association vs causality
Association vs causality Association and causation
Association and causation Causation in criminal law
Causation in criminal law Natural law versus positive law
Natural law versus positive law 8-6 practice the law of sines and law of cosines
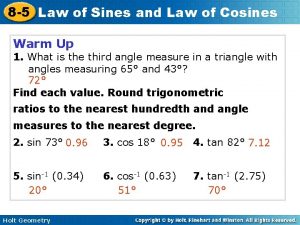
8-6 practice the law of sines and law of cosines Newton's first law and second law and third law
Newton's first law and second law and third law Newton's first law of motion
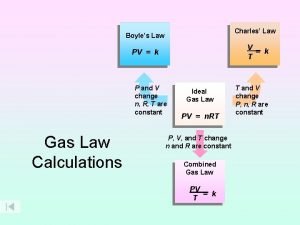
Newton's first law of motion Boyle's law charles law avogadro's law
Boyle's law charles law avogadro's law Avogadro's law constants
Avogadro's law constants