An Overview of Anterior Cruciate Ligament Injuries PAS
- Slides: 19
An Overview of Anterior Cruciate Ligament Injuries PAS 646 March 30, 2006 Advisor: Samuel Powdrill, M. Phil, PA-C Kurt Kramer
Background • • • Anatomy of the knee Epidemiology Mechanism of injury Risk factors Presentation of injury Diagnosis Rehabilitation (“prehab” vs. “rehab”) Graft choices Surgical technique Prevention
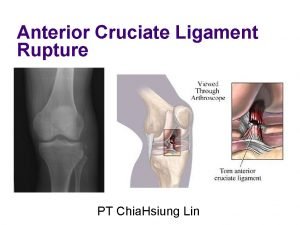
Discussion • Knee Anatomy – Anterior cruciate ligament (ACL) one of four stabilizing ligaments – Protects integrity of menisci and articular cartilage – ACL prevents excessive anterior translation of the tibia and internal or external rotation of the tibia on the femur
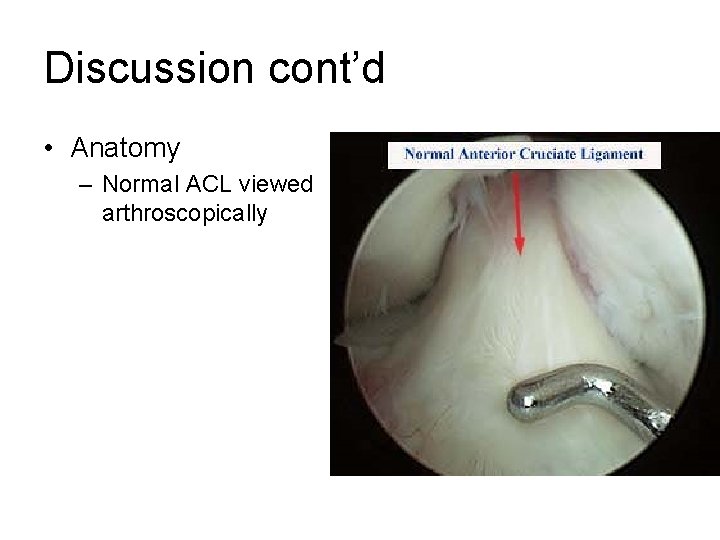
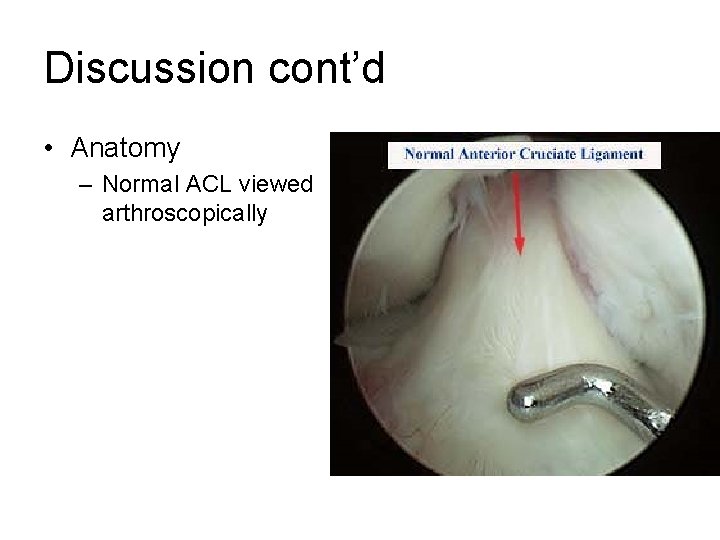
Discussion cont’d • Anatomy – Normal ACL viewed arthroscopically
Discussion cont’d • Epidemiology – Annual incidence of ~200, 000 ACL ruptures per year with an estimated 1 in 3, 000 – Females > Males – Incidence highest in population aged 15 -45 years old with 1 in 1750 persons (Brown, 2004) – Repair is now being indicated in older populations to prevent earlier onset of osteoarthritis – Average return to full activity is ~ 6 to 8 months
Discussion cont’d • Mechanism of Injury – Usually a hx of non-contact injury (70%) – Common is any physical activity that requires quick change in direction or a contact sport • Soccer, basketball, volleyball, football, and skiing – Mechanism usually involves sudden deceleration, hyperextension, and tibial torsion
Discussion cont’d • Risk Factors – Individuals participating in high risk sports – Playing surface • High shoe-surface friction that increase performance (artificial turf) – Neuromuscular deficits of the female sex • Increased incidence of female injury is NOT associated with sex specific hormones • Females tend to activate their quadriceps near full knee extension, thus landing with smaller angles of knee flexion than their male counterpart • Females show earlier neuromuscular fatigue
Discussion cont’d • ACL Injury Presentation – History is key! • Know the mechanism of ACL injuries! • Appropriate mechanism accompanied by what patient describes as a “pop” and excruciating pain – Excessive swelling with knee effusion – Decreased range of motion (ROM) – Inability to contract quadriceps • H-reflex
Discussion cont’d • Diagnosis – History and presentation – + Lachman’s or Anterior Drawer – Imaging • X-ray (avulsion) • MRI – Hemarthrosis (joint aspiration) – Appropriate referral
Discussion cont’d • Rehabilitation – Prehab (Gold-standard) • Implemented immediately after diagnosis • Decrease pain and swelling • Increase ROM, quad strength, and proprioception >90% of contralateral leg • Prehab allows for quicker post-operative return to ADLs and physical activity – Rehab • Progression varies depending on graft choice • Also focuses on decreasing pain and swelling, while increasing ROM, strength, and proprioception
Discussion cont’d • Graft choices (4 most commonly used) – Achilles tendon allograft • Used in pts. whom desire less painful recovery, improved cosmetic appearance, lead a less active lifestyle, and those with no other available graft choice • Cole et al. 2005 report that pts. had significantly less pain when compared to bone-patellar tendon-bone (BPTB) autograft (P<. 0001) • Increased risk of infection, immunologic response, and alteration of graft structural properties by sterilization, thus affecting long-term graft stability has deterred most surgeons from choosing this graft (Shelbourne 2002; Beynnon et al. 2005)
Discussion cont’d – Hamstring tendon autograft • Harvested from the semitendonosis or gracilis tendon from the ipsilateral leg • Some physicians prefer this graft due to pts. reporting patellofemoral pain with the BPTB autograft (Goldblatt 2005), while Svenson et al. report no significant difference in levels of pain b/w this graft and the BPTB autograft • Svenson et al. report increased laxity with hamstring autograft when compared to pts. that received a BPTB autograft • Freedman et al. report significantly lower graft failure (P<. 001), significantly better static knee stability (P<. 017), and higher patient satisfaction (P<. 001) with the use of BPTB autograft when compared to hamstring autografts
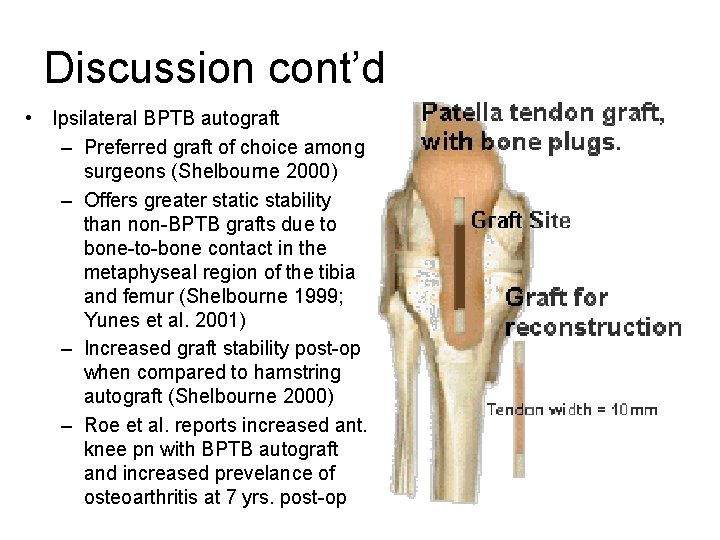
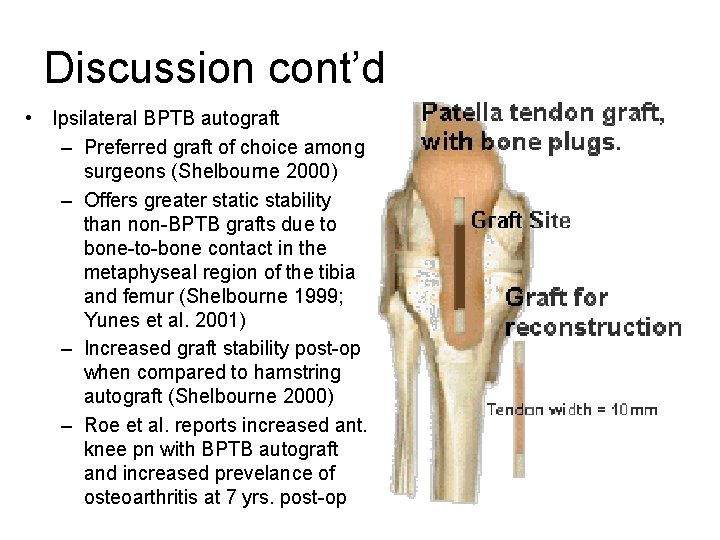
Discussion cont’d • Ipsilateral BPTB autograft – Preferred graft of choice among surgeons (Shelbourne 2000) – Offers greater static stability than non-BPTB grafts due to bone-to-bone contact in the metaphyseal region of the tibia and femur (Shelbourne 1999; Yunes et al. 2001) – Increased graft stability post-op when compared to hamstring autograft (Shelbourne 2000) – Roe et al. reports increased ant. knee pn with BPTB autograft and increased prevelance of osteoarthritis at 7 yrs. post-op
Discussion cont’d • Contralateral BPTB autograft – Many of same benefits and disadvantages as ipsilateral BPTB autograft – If combined with appropriate accelerated rehabilitation program may allow athlete to return to full activity 4 wks. post-op without an increased risk loss of stability or early graft tear (Shelbourne 2002) – Theory of contralateral BPTB autograft is that by dividing the trauma of surgery and rehab b/w both extremities, evidence shows course of rehab is easier, quicker, and more reliable (Shelbourne 2002) – Slightly longer operating time, increased patient education, and new approach to rehab for athletic trainers and PTs – Safe and predictable return without sacrificing strength, ROM, and stability – Used in patients in which return to sports is a priority
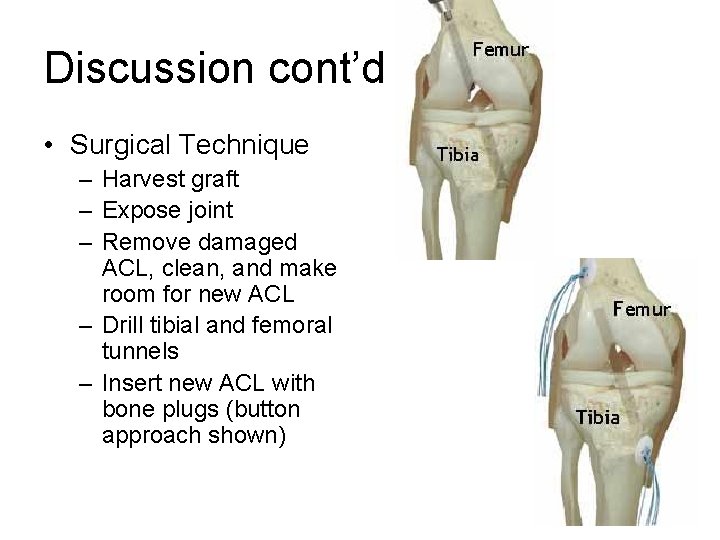
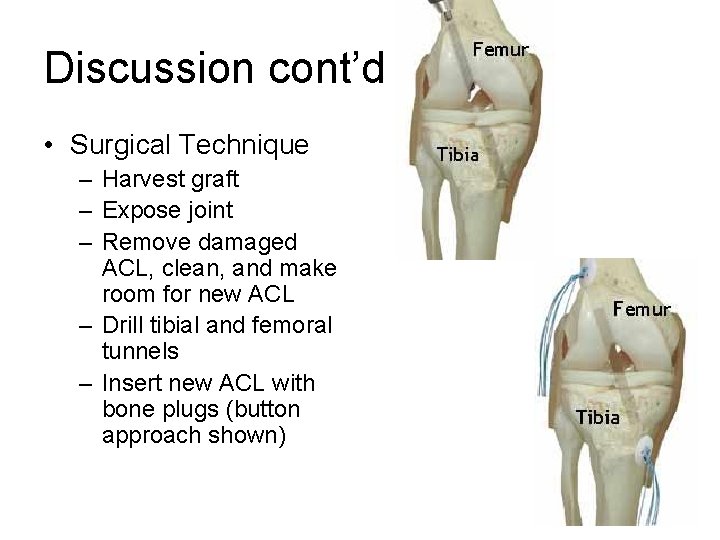
Discussion cont’d • Surgical Technique – Harvest graft – Expose joint – Remove damaged ACL, clean, and make room for new ACL – Drill tibial and femoral tunnels – Insert new ACL with bone plugs (button approach shown)
Discussion cont’d • Prevention – ACL injury prevention programs – Programs focus on modifying neuromuscular and biomechanical risk factors • Agility drills and plyometric exercises • Recognition of injury associated actions and positions • Educate athletes in proper jumping techniques, softer landings, instant recoil, and correct posture and alignment – Significantly decreased incidence of ACL injuries among female high school soccer, basketball, and volleyball athletes (Brown 2004); thus supporting theory that there are neuromuscular risk factors associated with the frequency of ACL tears
Conclusion • Important for PCP to have thorough understanding of anatomy, mx of injury, special testing, and appropriate tx or referral • Appropriate referral may be key to full return to activity and long-term patient satisfaction (everyone is different) • Be familiar with orthopedic surgeons in area and what protocols and grafting options they utilized • Pts. lead different lifestyles, thus one protocol and graft choice will likely be more appropriate treatment for one pt. than another • More research needed for long-term graft stability and pt. satisfaction for each graft • Swallow your pride and utilize local PTs and ATCs!
References • • • • • Beynnon BD, Johnson RJ, Abate JA, Fleming BC, Nichols CE. Treatment of anterior cruciate ligament injuries, Part 1. Am J Sports Med 2005; 33: 1579 -1602. Brown JR, Trojian TH. Anterior and posterior cruciate ligament injuries. Prim Care Clin Office Pract 2004; 31: 925 -56. Cole DW, et al. Cost comparison of anterior cruciate ligament reconstruction: autograft versus allograft. Arthroscopy 2005; 21: 786 -90. De. Carlo M, Shelbourne KD, Oneacre K. Rehabilitation program for both knees when the contralateral autogenous patellar tendon graft is used for primary anterior cruciate ligament reconstruction: a case study. J Orthop Sports Phys Ther 1999; 29: 144 -53. Freedman KB, D’Amato MJ, Nedeff DD, et al. Arthroscopic Anterior Cruciate Ligament Reconstruction: A meta-analysis comparing patellar tendon and hamstring tendon autografts. Am J Sports Med 2003; 31: 2 -11. Goldblatt JP, Fitzsimmons SE, Balk E, et al. Reconstruction of the anterior cruciate ligament: meta-analysis of patellar tendon versus hamstring tendon autograft. Arthroscopy 2005; 21: 791 -803. Jari S, Shelbourne KD. Simultaneous bilateral anterior cruciate ligament reconstruction. Am J Sports Med 2002; 30: 891 -4. Johnson DH, Maffulli N, King JB, et al. Anterior cruciate ligament reconstruction: A cynical view from the British Isles on the indications of surgery. Arthroscopy 2003; 19: 203 -9. Malinzak RA. Mechanisms of ACL injuries. Coach Kryzewski Human Performance Laboratory. K-Lab Symposium in Sports Performance Enhancement Workshop, Duke University Medical Center, Department of Sports Medicine-Orthopaedic Surgery, July 10 th, 1999. Mastrokalos DS, Springer J, Siebold R, et al. Donor site morbidity and return to the preinjury activity level after anterior cruciate ligament reconstruction using ipsilateral and contralateral patellar tendon autograft: a retrospective, nonrandomized study. Am J Sports Med 2005; 33: 85 -93. Poehling GG, Curl WW, Lee CA, et al. Analysis of outcomes of anterior cruciate ligament repair with 5 -year follow-up: allograft versus autograft. Roe J, Pinczewski LA, Russell VJ, et al. A 7 -year follow-up of patellar tendon and hamstring tendon grafts for arthroscopic anterior cruciate ligament reconstruction. Am J Sports Med 2005; 33: 1337 -45. Shelbourne KD, Rask BP. Controversies with anterior cruciate ligament surgery and rehabilitation. Am J of Knee Surgery 1998; 11: 136 -43. Shelbourne KD, Johnson BC. Effects of patellar tendon width and preoperative quadriceps strength on strength after anterior cruciate ligament reconstruction with ipsilateral bone-patellar tendon-bone autograft. Am J Sports Med 2004; 32: 1474 -8. Shelbourne KD, Davis TJ. Evaluation of knee stability before and after participation in a functional sports agility program during rehabilitation after anterior cruciate ligament reconstruction. Am J Sports Med 1999; 27: 156 -61. Shelbourne KD, Beaty JH. Graft selection for ACL reconstruction: Contralateral patellar tendon autograft (Instructional Course Lectures). Am Academy of Ortho Surg 2002; 51: 325 -328. Shelbourne KD, Urch SE. Primary anterior cruciate ligament reconstruction using the contralateral autogenous patellar tendon. Am J Sports Med 2000; 28: 651 -8. Wilk KE, Reinold MM, Hooks TR. Recent advances in the rehabilitation of isolated and combined anterior cruciate ligament injuries. Orthop Clin N Am 2003; 34: 107 -37. Yunes M, Richmond JC, Engels EA, et al. Patellar versus hamstring tendons in anterior cruciate ligament reconstruction: A meta-analysis. Zink EJ, Trumper RV, Smidt CR, et al. Gender comparison of knee strength recovery following ACL reconstruction with contralateral patellar tendon. Biomed Sci Instrum 2005; 41: 323 -8.
Questions?
 Woźny pas mu odwiązał pas słucki pas lity
Woźny pas mu odwiązał pas słucki pas lity Biomechanics of throwing a football
Biomechanics of throwing a football Trochanteric anastomosis
Trochanteric anastomosis Cruciate corolla
Cruciate corolla Cruciate anastomosis
Cruciate anastomosis Mid inguinal point
Mid inguinal point Schéma de la communication interpersonnelle
Schéma de la communication interpersonnelle Qui chante ne pleure pas devant ma tombe
Qui chante ne pleure pas devant ma tombe Lecture pas à pas
Lecture pas à pas Moteur pas à pas à aimant permanent
Moteur pas à pas à aimant permanent Uc davis web scheduler
Uc davis web scheduler Jsp 539
Jsp 539 Chapter 15 injuries to muscles and bones
Chapter 15 injuries to muscles and bones Chop saw injuries
Chop saw injuries Injury prevention safety and first aid
Injury prevention safety and first aid Chapter 4 basics of tissue injuries
Chapter 4 basics of tissue injuries Describe peeta's injuries
Describe peeta's injuries Chapter 11 injuries to the shoulder region
Chapter 11 injuries to the shoulder region Chapter 28 head and spine injuries
Chapter 28 head and spine injuries Common track and field injuries
Common track and field injuries