AHRQ Safety Program for Longterm Care HAIsCAUTI CatheterAssociated
- Slides: 21
AHRQ Safety Program for Long-term Care: HAIs/CAUTI Catheter-Associated Urinary Tract Infection (CAUTI) Definitions and Reporting Onboarding #2 for All Long-Term Care Staff 1
Learning Objectives Upon completion of this session, long-term care staff will be able to: • define an indwelling catheter and catheter-associated urinary tract infection (CAUTI); • list the signs and symptoms for a CAUTI; and • understand the importance of their role in CAUTI identification. 2
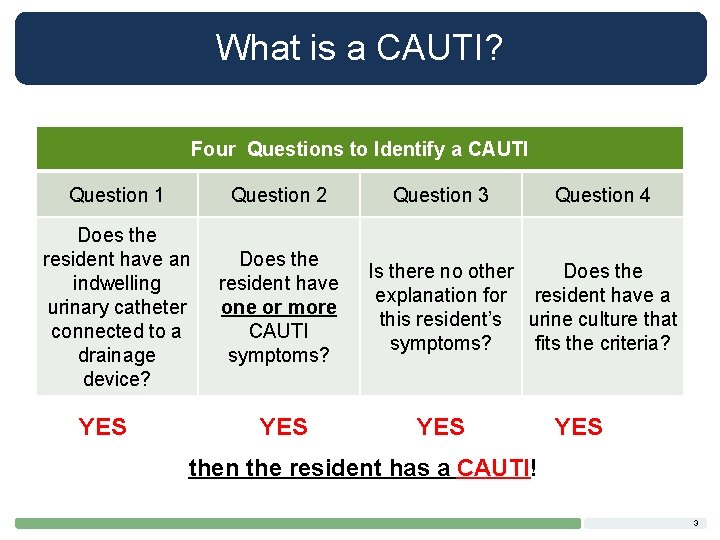
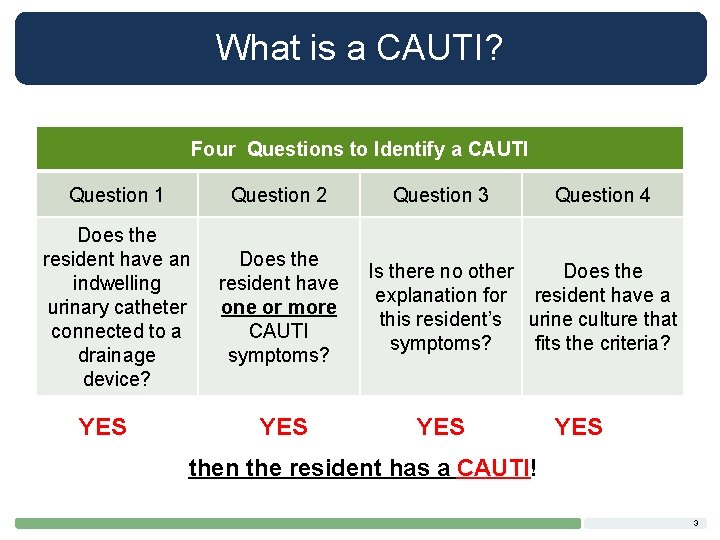
What is a CAUTI? Four Questions to Identify a CAUTI Question 1 Question 2 Does the resident have an indwelling urinary catheter connected to a drainage device? Does the resident have one or more CAUTI symptoms? YES Question 3 Question 4 Is there no other Does the explanation for resident have a this resident’s urine culture that symptoms? fits the criteria? YES then the resident has a CAUTI! 3
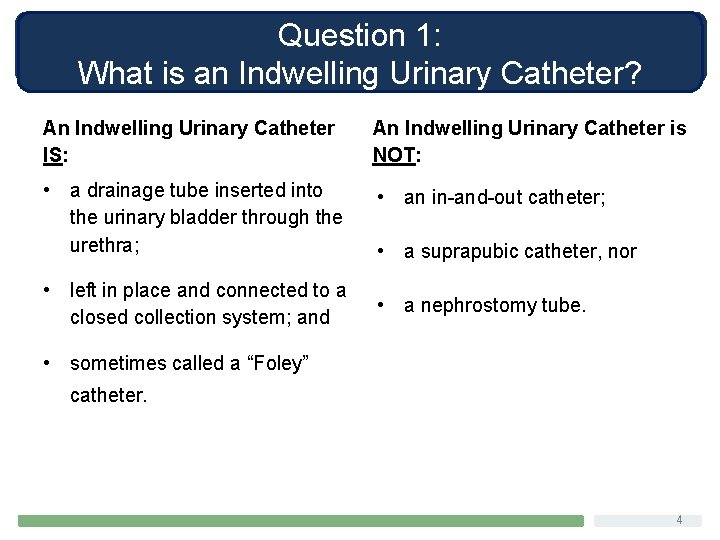
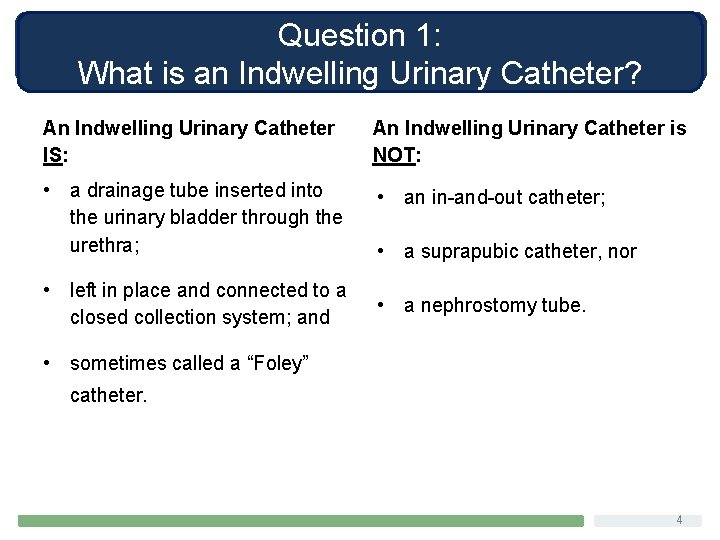
Question 1: What is an Indwelling Urinary Catheter? An Indwelling Urinary Catheter IS: An Indwelling Urinary Catheter is NOT: • a drainage tube inserted into the urinary bladder through the urethra; • an in-and-out catheter; • left in place and connected to a closed collection system; and • a suprapubic catheter, nor • a nephrostomy tube. • sometimes called a “Foley” catheter. 4
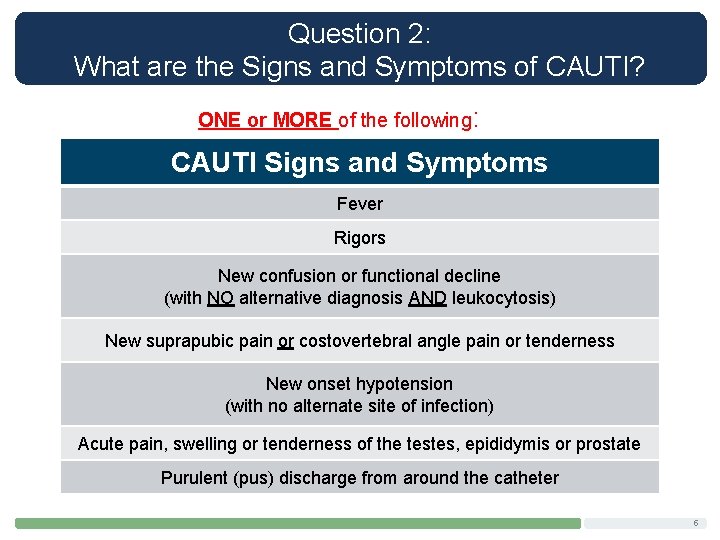
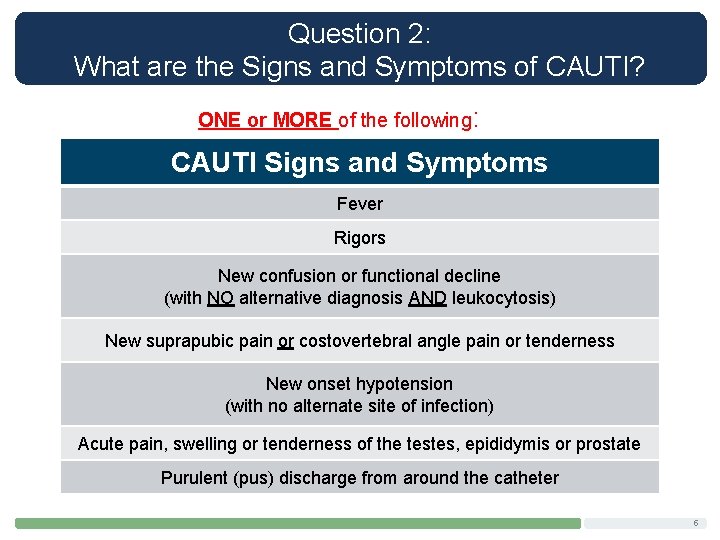
Question 2: What are the Signs and Symptoms of CAUTI? ONE or MORE of the following: CAUTI Signs and Symptoms Fever Rigors New confusion or functional decline (with NO alternative diagnosis AND leukocytosis) New suprapubic pain or costovertebral angle pain or tenderness New onset hypotension (with no alternate site of infection) Acute pain, swelling or tenderness of the testes, epididymis or prostate Purulent (pus) discharge from around the catheter 5
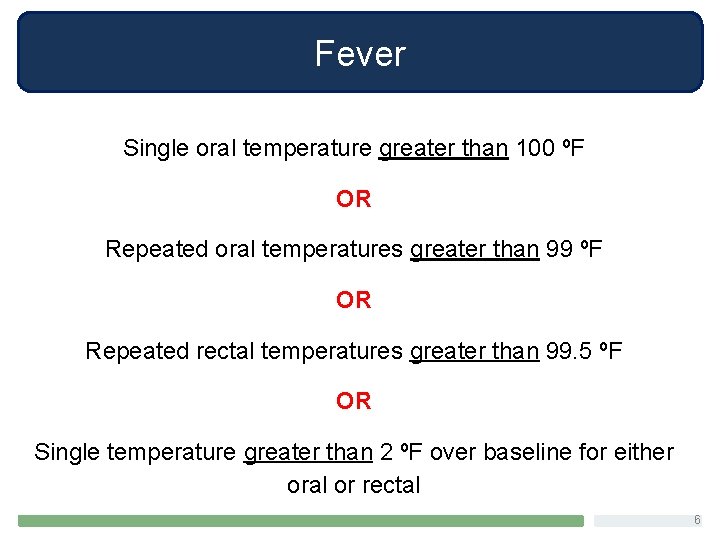
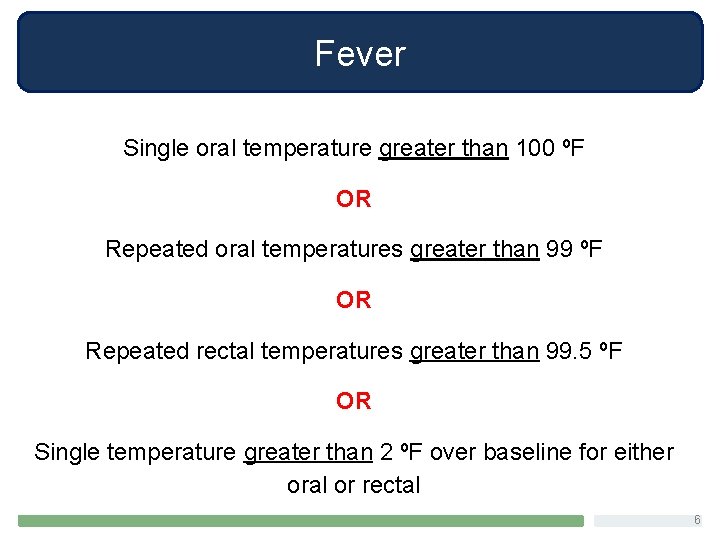
Fever Single oral temperature greater than 100 ºF OR Repeated oral temperatures greater than 99 ºF OR Repeated rectal temperatures greater than 99. 5 ºF OR Single temperature greater than 2 ºF over baseline for either oral or rectal 6
Rigors • Sudden, paroxysmal chill with high temperature. • Followed by a sense of heat and profuse perspiration. • Commonly called “fever and chills. ” 7
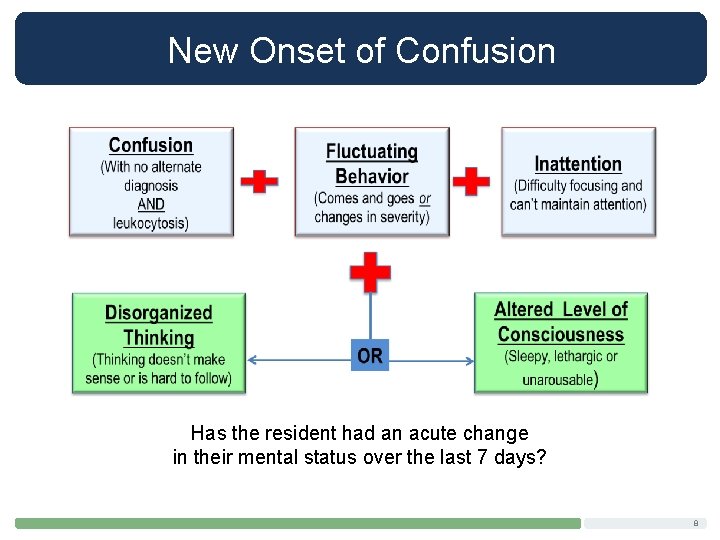
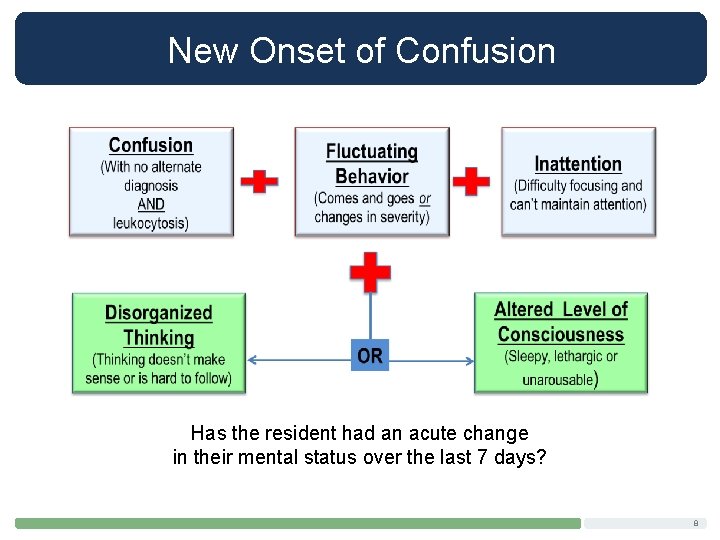
New Onset of Confusion Has the resident had an acute change in their mental status over the last 7 days? 8
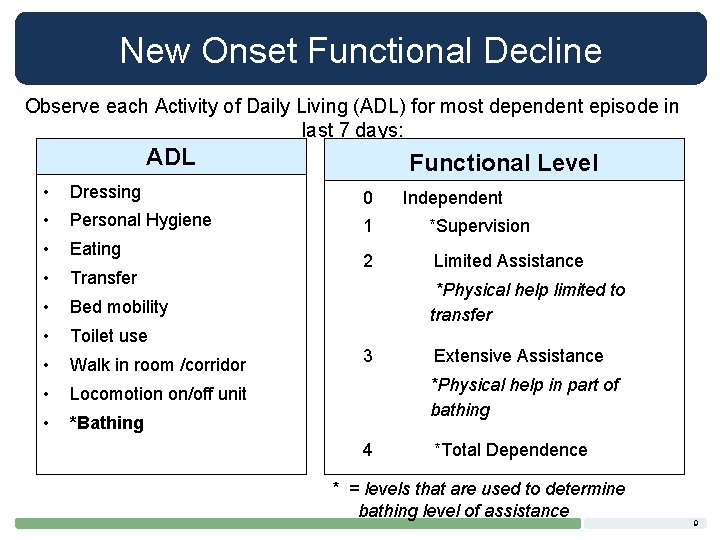
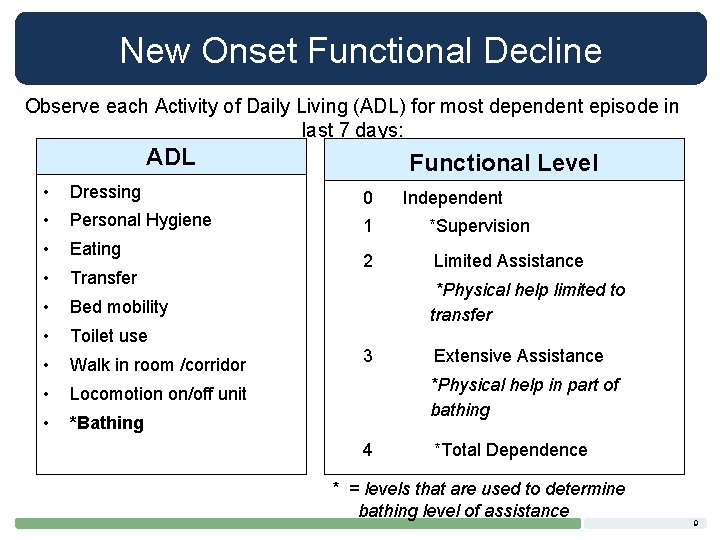
New Onset Functional Decline Observe each Activity of Daily Living (ADL) for most dependent episode in last 7 days: ADL Functional Level • Dressing 0 • Personal Hygiene 1 *Supervision • Eating • Transfer 2 Limited Assistance • Bed mobility • Toilet use • Walk in room /corridor • Locomotion on/off unit • *Bathing Independent *Physical help limited to transfer 3 Extensive Assistance *Physical help in part of bathing 4 *Total Dependence * = levels that are used to determine bathing level of assistance 9
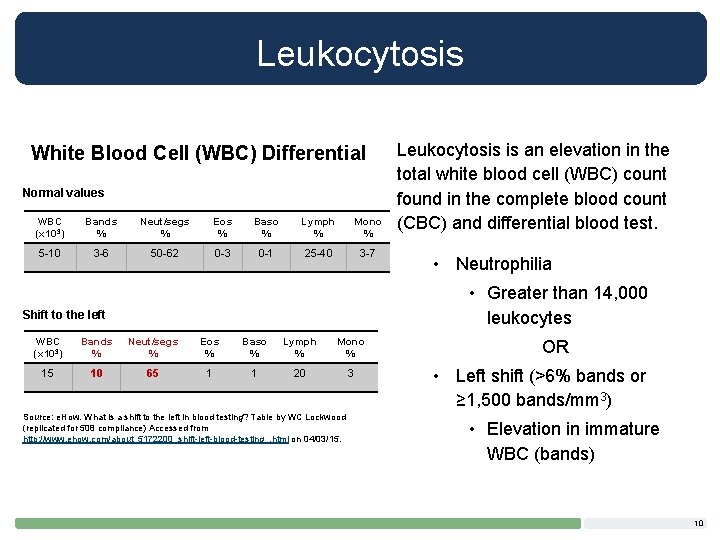
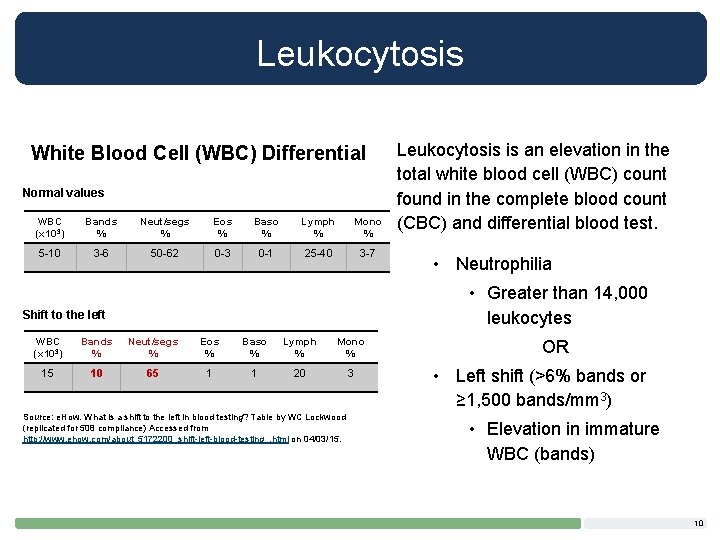
Leukocytosis White Blood Cell (WBC) Differential Normal values WBC (x 103) Bands % Neut/segs % Eos % Baso % Lymph % Mono % 5 -10 3 -6 50 -62 0 -3 0 -1 25 -40 3 -7 Leukocytosis is an elevation in the total white blood cell (WBC) count found in the complete blood count (CBC) and differential blood test. • Neutrophilia • Greater than 14, 000 leukocytes Shift to the left WBC (x 103) Bands % Neut/segs % Eos % Baso % Lymph % Mono % 15 10 65 1 1 20 3 Source: e. How. What is a shift to the left in blood testing? Table by WC Lockwood (replicated for 508 compliance) Accessed from http: //www. ehow. com/about_5172200_shift-left-blood-testing_. html on 04/03/15. OR • Left shift (>6% bands or ≥ 1, 500 bands/mm 3) • Elevation in immature WBC (bands) 10
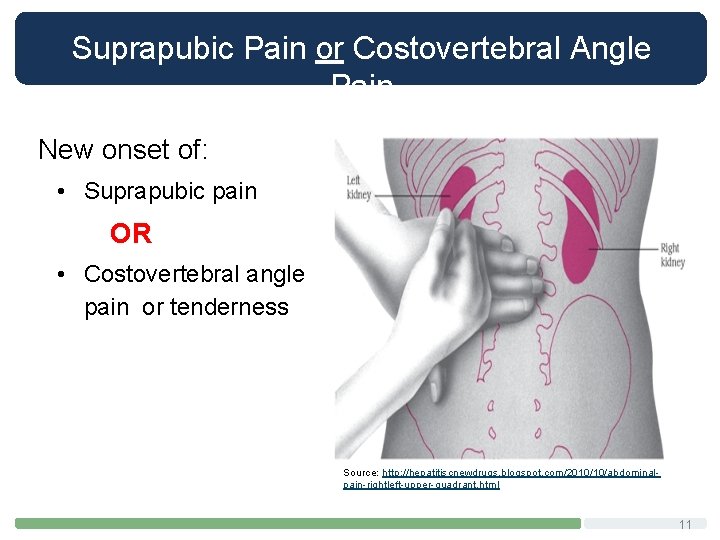
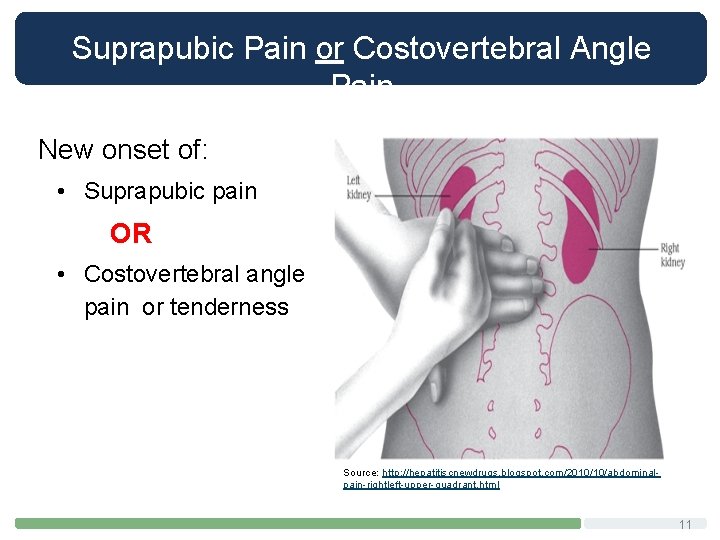
Suprapubic Pain or Costovertebral Angle Pain New onset of: • Suprapubic pain OR • Costovertebral angle pain or tenderness Source: http: //hepatitiscnewdrugs. blogspot. com/2010/10/abdominalpain-rightleft-upper-quadrant. html 11
Questions 3: Could Something Else Cause These Signs and Symptoms? The signs and symptoms just described are only indicative of a CAUTI if there are no other explanations for the signs and symptoms. 12
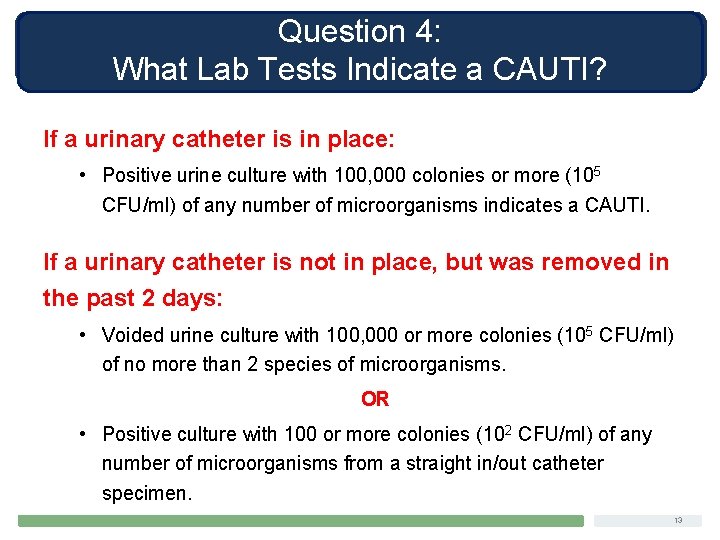
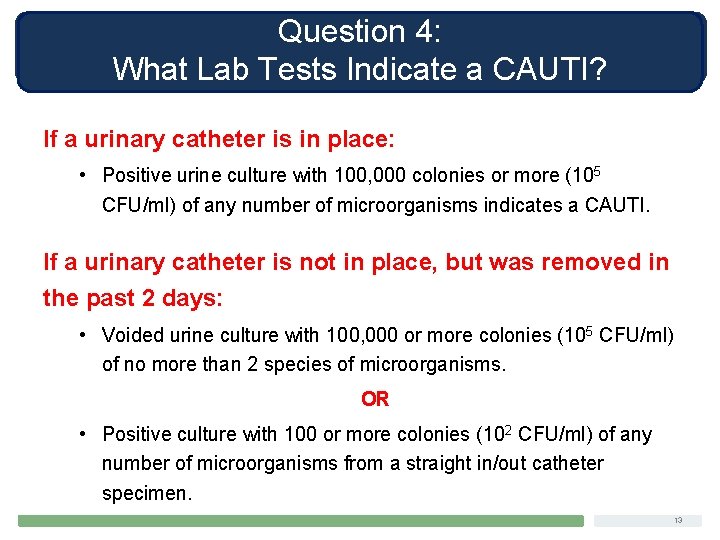
Question 4: What Lab Tests Indicate a CAUTI? If a urinary catheter is in place: • Positive urine culture with 100, 000 colonies or more (105 CFU/ml) of any number of microorganisms indicates a CAUTI. If a urinary catheter is not in place, but was removed in the past 2 days: • Voided urine culture with 100, 000 or more colonies (105 CFU/ml) of no more than 2 species of microorganisms. OR • Positive culture with 100 or more colonies (102 CFU/ml) of any number of microorganisms from a straight in/out catheter specimen. 13
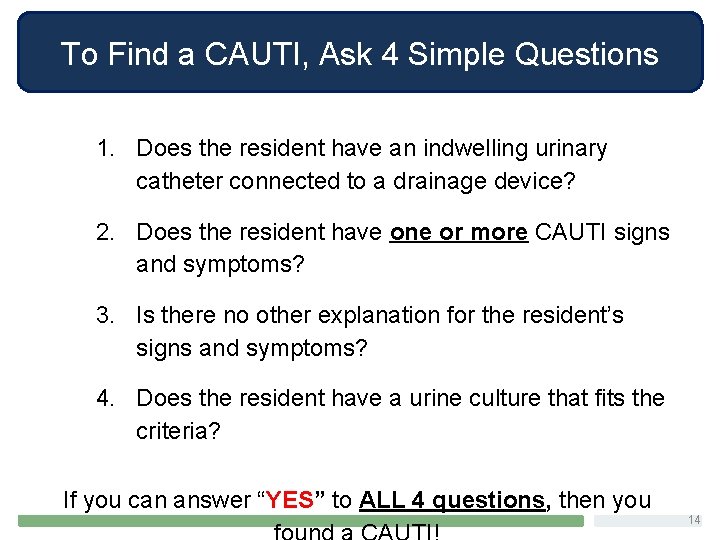
To Find a CAUTI, Ask 4 Simple Questions 1. Does the resident have an indwelling urinary catheter connected to a drainage device? 2. Does the resident have one or more CAUTI signs and symptoms? 3. Is there no other explanation for the resident’s signs and symptoms? 4. Does the resident have a urine culture that fits the criteria? If you can answer “YES” to ALL 4 questions, then you 14
Stay Updated with Useful Resources AHRQ Safety Program for Long-term Care: HAIs/CAUTI Project Website Login information Username: ltcsafety Password: ltcsafety Team. STEPPS® for Long-term Care CAUTI Criteria NHSN Definitions Pocket Cards LTC CAUTI Surveillance Worksheet 15
References National Healthcare Safety Network (NHSN). Urinary Tract Infection (UTI) Event for Long-term Care Facilities. [online] http: //www. cdc. gov/nhsn/LTC/uti/. Stone ND, Ashraf MS, Calder J. Surveillance Definitions of Infections in Long. Term Care Facilities: Revisiting the Mc. Geer Criteria. Infect Control Hosp Epidemiol 2012; 33(10): 965 -977. Centers for Medicare and Medicaid. MDS 3. 0 RAI Manual v 1. 12. October 1, 2014. [online] http: //www. cms. gov/Medicare/Quality-Initiatives-Patient. Assessment. Instruments/Nursing. Home. Quality. Inits/MDS 30 RAIManual. html. George-Gay B, Katherine Parker K. Understanding the Complete Blood Count With Differential. Journal of Peri. Anesthesia Nursing, Vol 18, No 2 (April), 2003: pp 96 -117. 16
Case Study, Skills Questions ENGAGEMENT ACTIVITIES 17
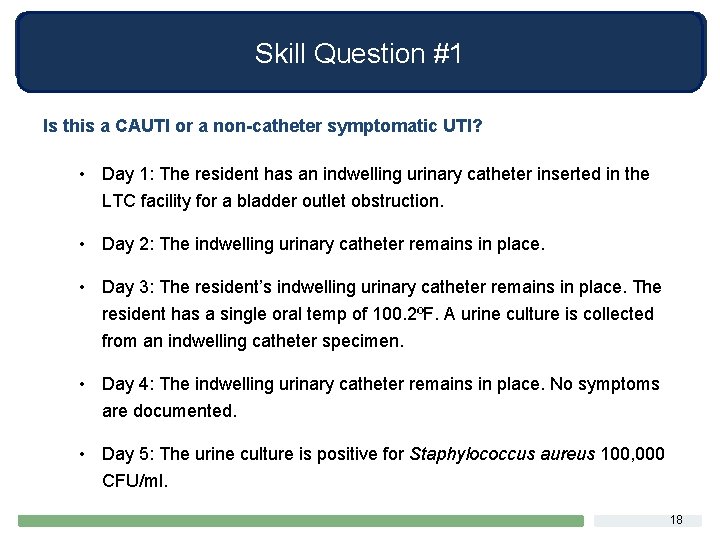
Skill Question #1 Is this a CAUTI or a non-catheter symptomatic UTI? • Day 1: The resident has an indwelling urinary catheter inserted in the LTC facility for a bladder outlet obstruction. • Day 2: The indwelling urinary catheter remains in place. • Day 3: The resident’s indwelling urinary catheter remains in place. The resident has a single oral temp of 100. 2ºF. A urine culture is collected from an indwelling catheter specimen. • Day 4: The indwelling urinary catheter remains in place. No symptoms are documented. • Day 5: The urine culture is positive for Staphylococcus aureus 100, 000 CFU/ml. 18
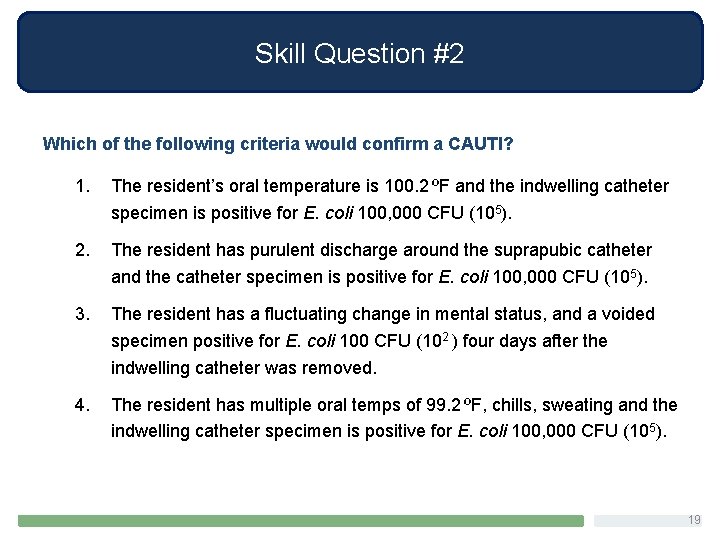
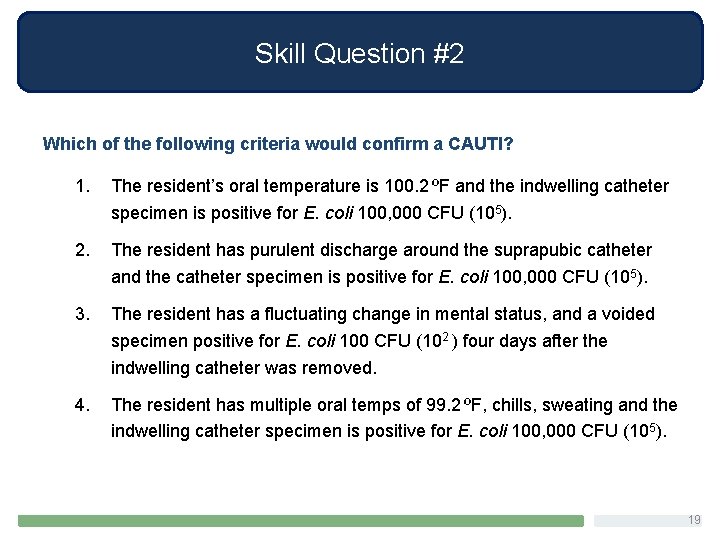
Skill Question #2 Which of the following criteria would confirm a CAUTI? 1. The resident’s oral temperature is 100. 2 ºF and the indwelling catheter specimen is positive for E. coli 100, 000 CFU (105). 2. The resident has purulent discharge around the suprapubic catheter and the catheter specimen is positive for E. coli 100, 000 CFU (105). 3. The resident has a fluctuating change in mental status, and a voided specimen positive for E. coli 100 CFU (102 ) four days after the indwelling catheter was removed. 4. The resident has multiple oral temps of 99. 2 ºF, chills, sweating and the indwelling catheter specimen is positive for E. coli 100, 000 CFU (105). 19
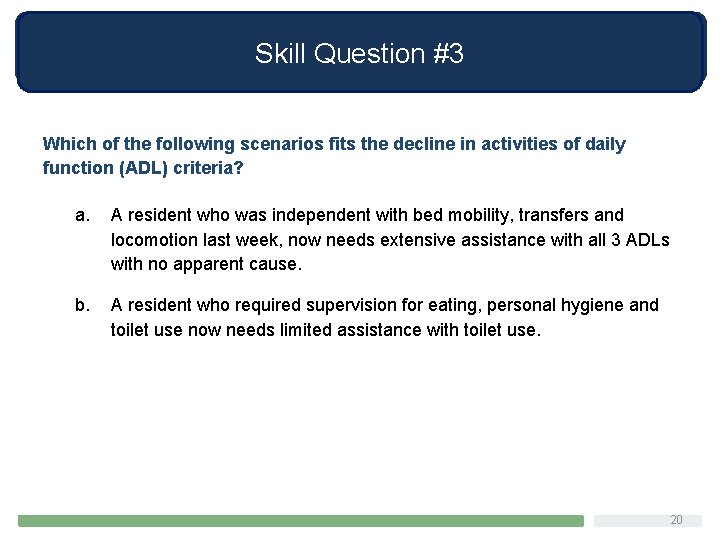
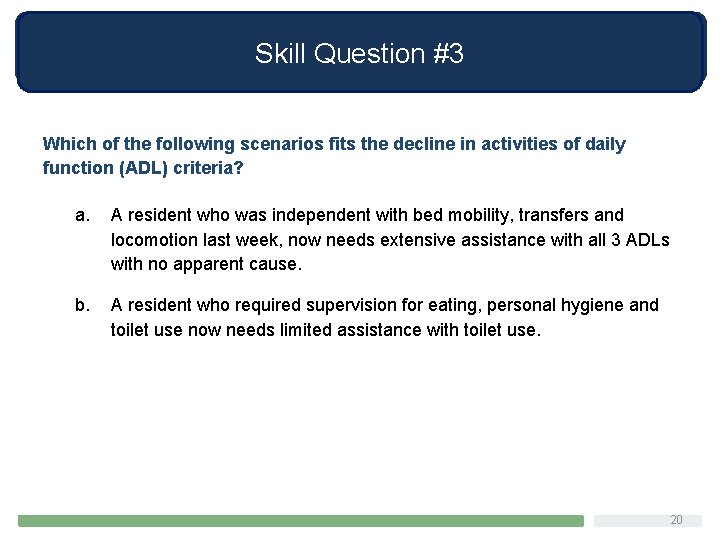
Skill Question #3 Which of the following scenarios fits the decline in activities of daily function (ADL) criteria? a. A resident who was independent with bed mobility, transfers and locomotion last week, now needs extensive assistance with all 3 ADLs with no apparent cause. b. A resident who required supervision for eating, personal hygiene and toilet use now needs limited assistance with toilet use. 20
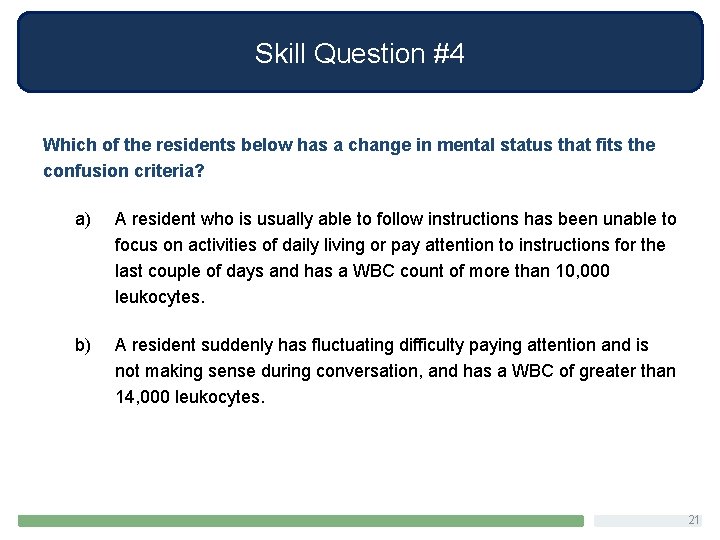
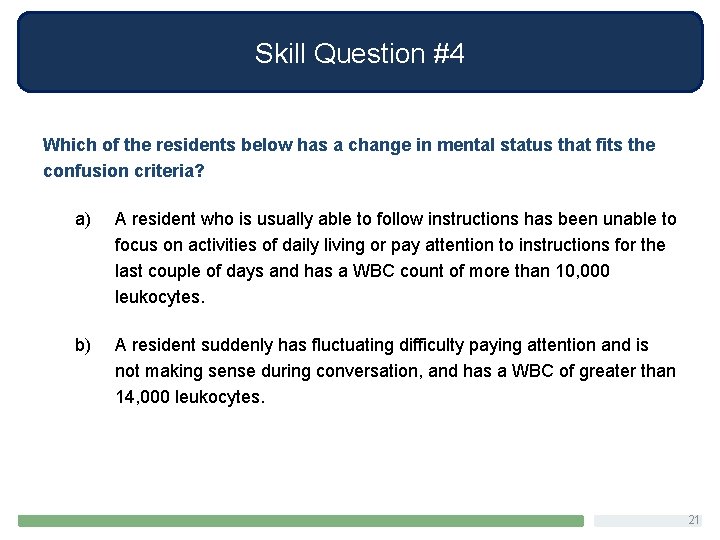
Skill Question #4 Which of the residents below has a change in mental status that fits the confusion criteria? a) A resident who is usually able to follow instructions has been unable to focus on activities of daily living or pay attention to instructions for the last couple of days and has a WBC count of more than 10, 000 leukocytes. b) A resident suddenly has fluctuating difficulty paying attention and is not making sense during conversation, and has a WBC of greater than 14, 000 leukocytes. 21
 Ahrq antibiotic stewardship
Ahrq antibiotic stewardship Ahrq safety culture survey
Ahrq safety culture survey Ahrq patient safety survey
Ahrq patient safety survey Lts stable
Lts stable Thomas silverstein
Thomas silverstein Ahrq quality indicators
Ahrq quality indicators Ahrq bedside shift report
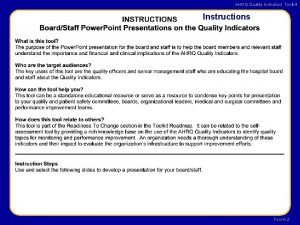
Ahrq bedside shift report Ahrq quality indicators toolkit
Ahrq quality indicators toolkit Ahrq qi
Ahrq qi Safety care certification
Safety care certification Primary secondary tertiary care definition
Primary secondary tertiary care definition Kontinuitetshantering
Kontinuitetshantering Typiska novell drag
Typiska novell drag Tack för att ni lyssnade bild
Tack för att ni lyssnade bild Ekologiskt fotavtryck
Ekologiskt fotavtryck Varför kallas perioden 1918-1939 för mellankrigstiden
Varför kallas perioden 1918-1939 för mellankrigstiden En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Kassaregister ideell förening
Kassaregister ideell förening Tidbok yrkesförare
Tidbok yrkesförare A gastrica
A gastrica Densitet vatten
Densitet vatten Datorkunskap för nybörjare
Datorkunskap för nybörjare