Aetna Medicaid Overview Long Term Services and Supports


- Slides: 14
Aetna Medicaid Overview Long Term Services and Supports August 2013 Aetna Medicaid
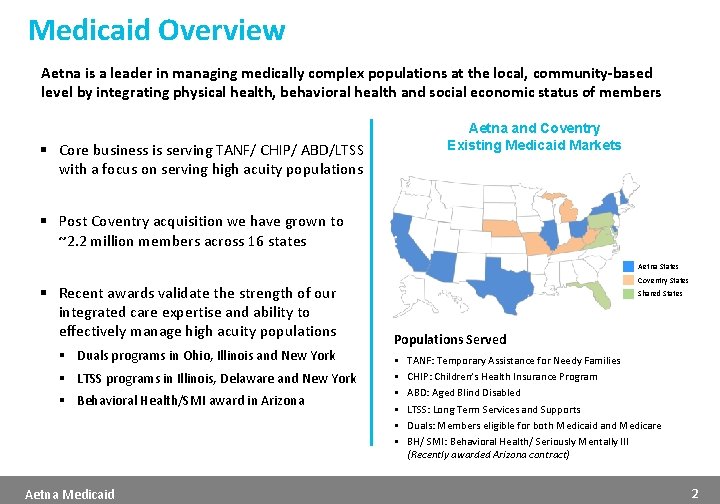
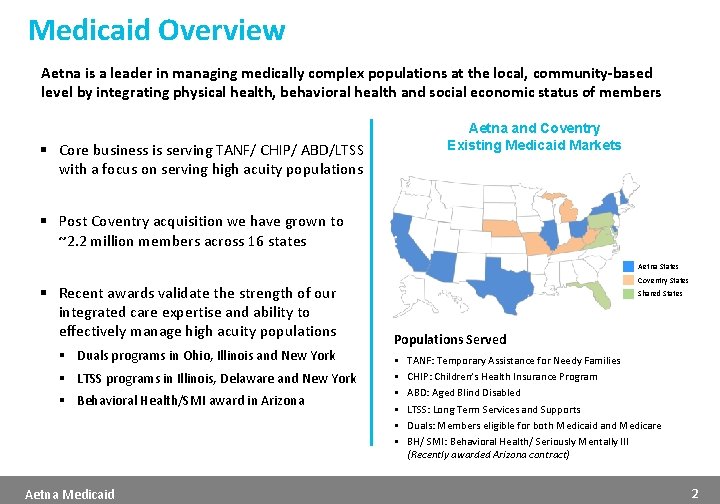
Medicaid Overview Aetna is a leader in managing medically complex populations at the local, community-based level by integrating physical health, behavioral health and social economic status of members Aetna and Coventry Existing Medicaid Markets § Core business is serving TANF/ CHIP/ ABD/LTSS with a focus on serving high acuity populations § Post Coventry acquisition we have grown to ~2. 2 million members across 16 states Aetna States § Recent awards validate the strength of our integrated care expertise and ability to effectively manage high acuity populations § Duals programs in Ohio, Illinois and New York § LTSS programs in Illinois, Delaware and New York § Behavioral Health/SMI award in Arizona Aetna Medicaid Coventry States Shared States Populations Served § § § TANF: Temporary Assistance for Needy Families CHIP: Children’s Health Insurance Program ABD: Aged Blind Disabled LTSS: Long Term Services and Supports Duals: Members eligible for both Medicaid and Medicare BH/ SMI: Behavioral Health/ Seriously Mentally Ill (Recently awarded Arizona contract) 2
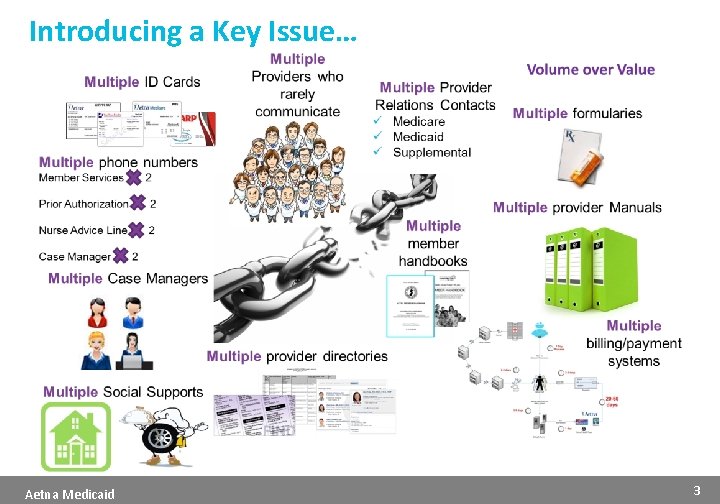
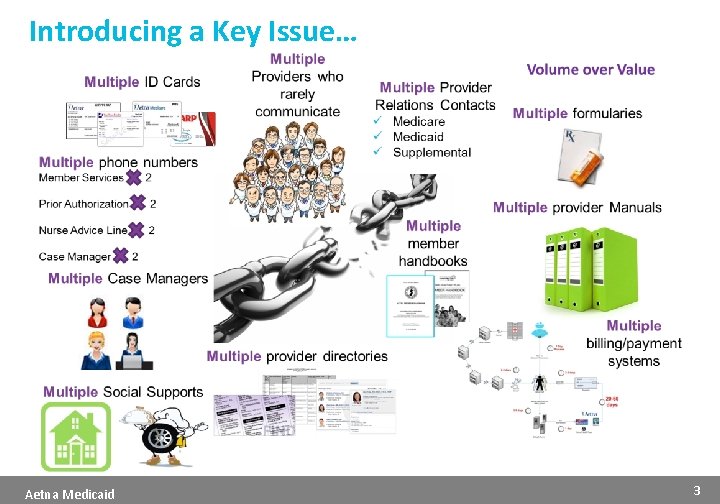
Introducing a Key Issue… Aetna Medicaid 3
Aetna Medicaid Model of Care and Capabilities Aetna Medicaid 4
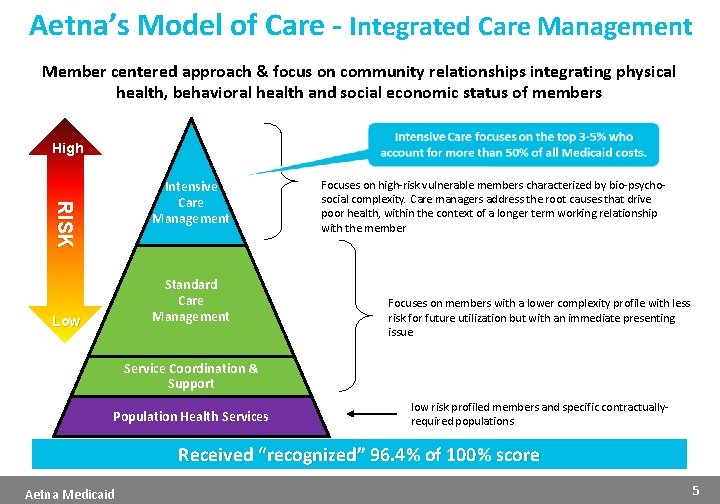
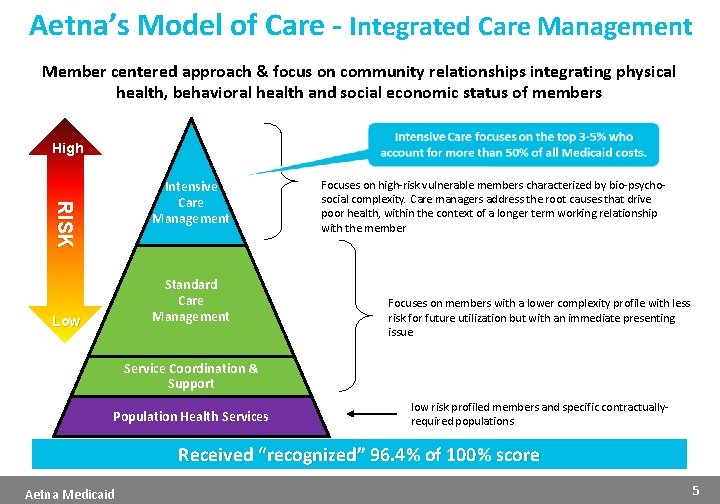
Aetna’s Model of Care - Integrated Care Management Member centered approach & focus on community relationships integrating physical health, behavioral health and social economic status of members High RISK Intensive Care Management Standard Care Management Low Focuses on high-risk vulnerable members characterized by bio-psychosocial complexity. Care managers address the root causes that drive poor health, within the context of a longer term working relationship with the member Focuses on members with a lower complexity profile with less risk for future utilization but with an immediate presenting issue Service Coordination & Support Population Health Services low risk profiled members and specific contractuallyrequired populations Received “recognized” 96. 4% of 100% score Aetna Medicaid 5
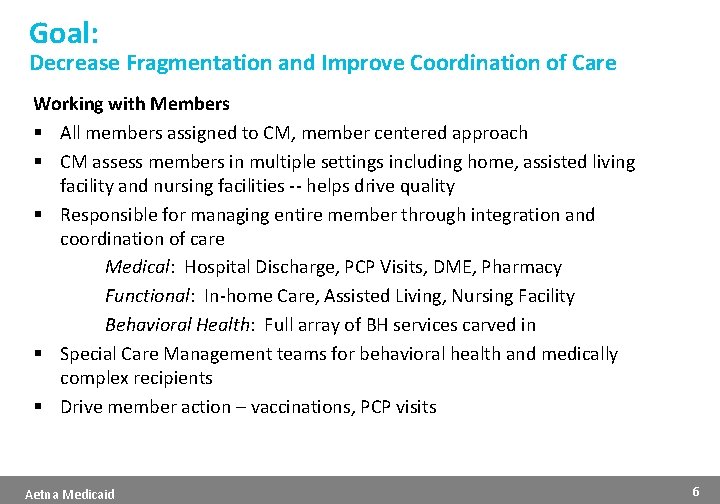
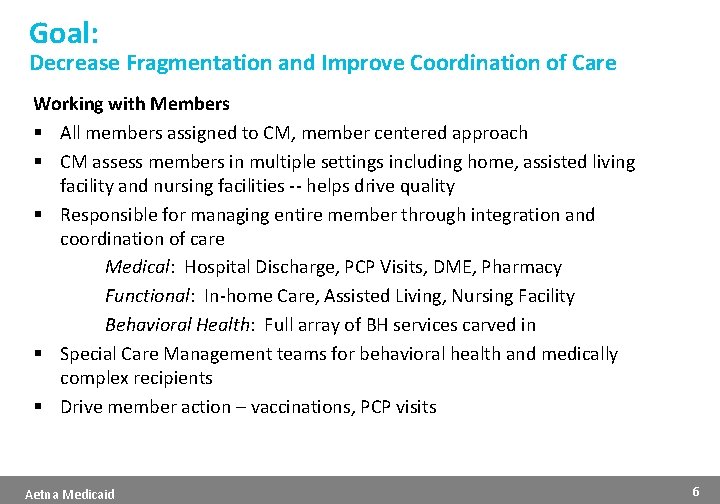
Goal: Decrease Fragmentation and Improve Coordination of Care Working with Members § All members assigned to CM, member centered approach § CM assess members in multiple settings including home, assisted living facility and nursing facilities -- helps drive quality § Responsible for managing entire member through integration and coordination of care Medical: Hospital Discharge, PCP Visits, DME, Pharmacy Functional: In-home Care, Assisted Living, Nursing Facility Behavioral Health: Full array of BH services carved in § Special Care Management teams for behavioral health and medically complex recipients § Drive member action – vaccinations, PCP visits Aetna Medicaid 6
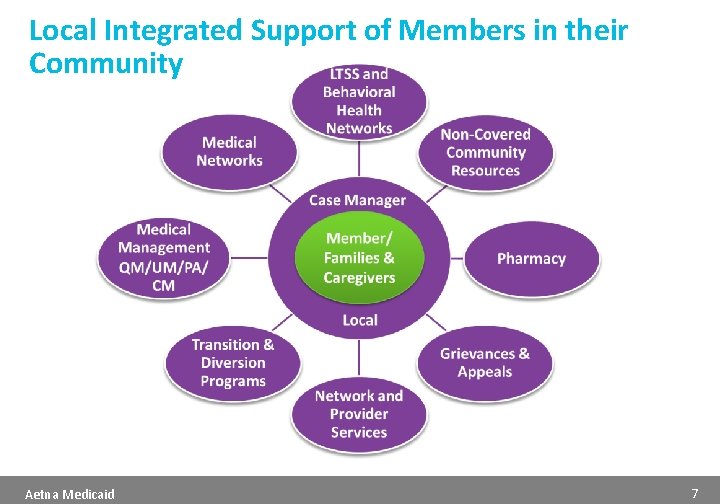
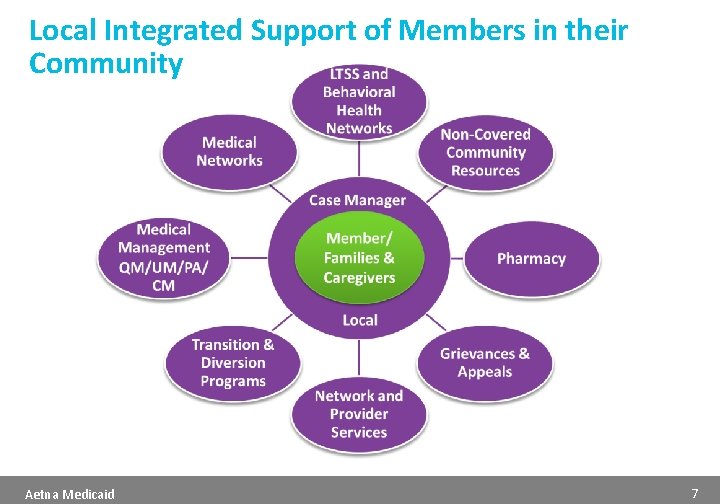
Local Integrated Support of Members in their Community Aetna Medicaid 7
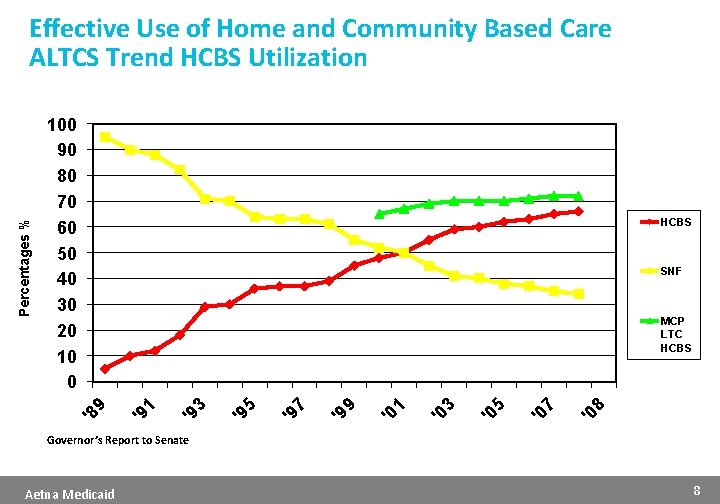
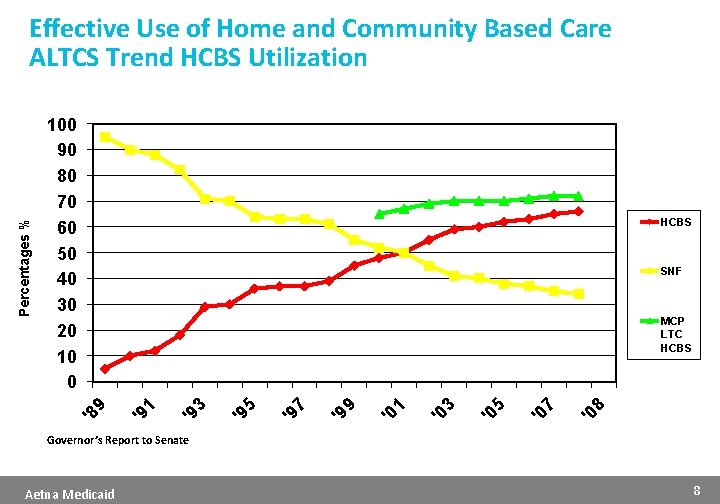
100 90 80 70 60 50 40 30 20 10 0 HCBS SNF 8 '0 7 '0 5 '0 3 '0 1 '0 9 '9 7 '9 5 '9 3 '9 '9 '8 1 MCP LTC HCBS 9 Percentages % Effective Use of Home and Community Based Care ALTCS Trend HCBS Utilization Governor’s Report to Senate Aetna Medicaid 8
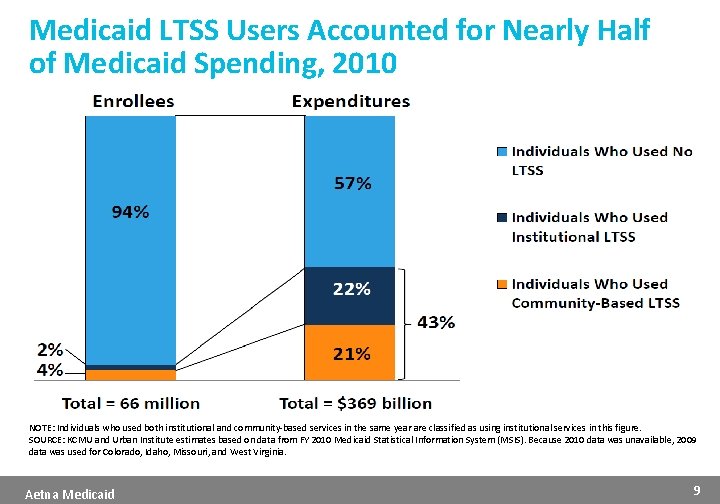
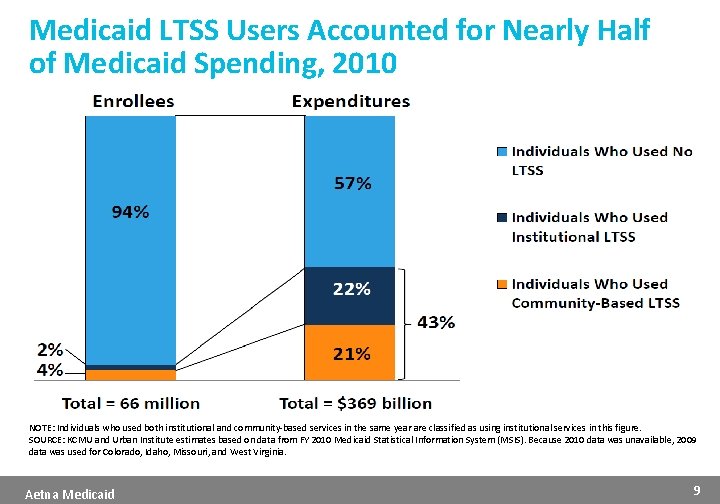
Medicaid LTSS Users Accounted for Nearly Half of Medicaid Spending, 2010 NOTE: Individuals who used both institutional and community-based services in the same year are classified as using institutional services in this figure. SOURCE: KCMU and Urban Institute estimates based on data from FY 2010 Medicaid Statistical Information System (MSIS). Because 2010 data was unavailable, 2009 data was used for Colorado, Idaho, Missouri, and West Virginia. Aetna Medicaid 9
Capitated Medicaid Managed LTSS: An Emerging Trend CMS reports that more than half the states are expected to be operating capitated Medicaid managed LTSS programs by January 2014, including: § Expansion of current Medicaid capitated managed LTSS programs under § 1115 or § 1915(b)/(c) ü 19 states with waivers implemented or approved as of 2012 (AZ, CA, DE, FL, HI, KS, MA, MI, MN, NH, NJ, NM, NY, NC, PA, TN, TX, WA, and WI) § Establishment of new Medicaid capitated managed LTSS programs under § 1115 or § 1915(b)/(c) ü 3 states with proposals pending (CA, IL, and NV) § Implementation of Medicare/Medicaid financial alignment demonstrations for dual eligible beneficiaries under § 1115 A combined with § 1115 or § 1915(b)/(c) ü 5 states with capitated proposals approved (CA, IL, MA, OH, and VA); 10 states with capitated proposals pending (HI, ID, MI, NY, OK, RI, SC, TX, VT, and WA) SOURCES: P. Saucier, J. Kasten, B. Burwell, and L. Gold, The Growth of Managed Long-Term Services and Supports (MLTSS) Programs: A 2012 Update, July 2012, available at: http: //www. medicaid. gov/Medicaid-CHIP-Program-Information/By-Topics/Delivery-Systems/Downloads/MLTSSP_White_paper_combined. pdf; M. Musumeci, Financial Alignment Demonstrations for Dual Eligible Beneficiaries Compared: California, Illinois, Massachusetts, Ohio, and Washington, The Henry J. Kaiser Family Foundation’s Commission on Medicaid and the Uninsured, May 2013, available at http: //www. kff. org/medicaid/issue-brief/illinois-massachusettsohio-and-washington-financial-alignment-demonstrations-for-dual-eligible-beneficiaries-compared/. Aetna Medicaid 10

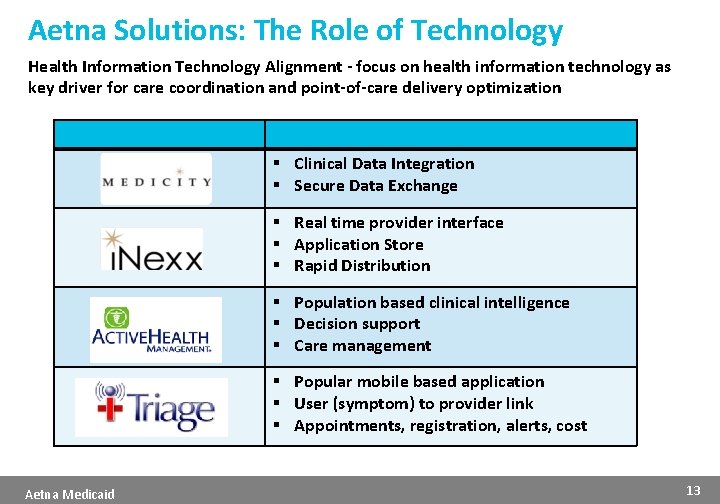
The New Health Care Landscape is Emerging… New and Innovative Relationships § Increased focus on innovative care management models for high-risk populations across the community care continuum Value-Based Payment Models § Demand for value-based purchasing arrangements focused on achieving quality outcomes: pay for performance, shared savings, bundled payments, alignment of quality incentives Health Information Technology Alignment § Intense focus on health information technology as key driver for care coordination and point-of-care delivery optimization Aetna Medicaid 11
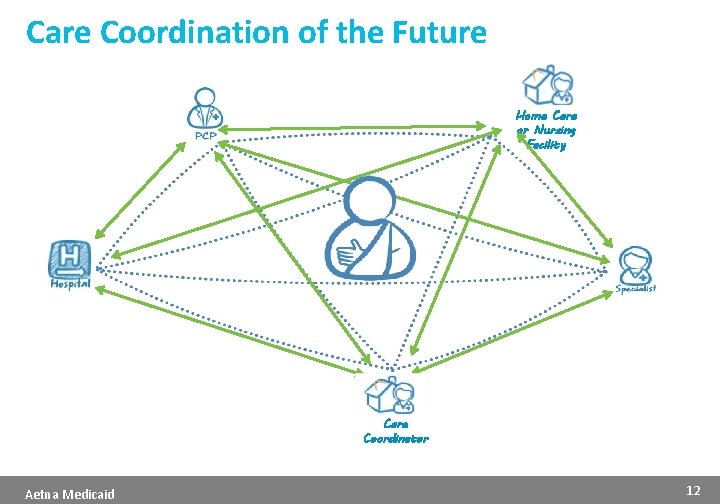
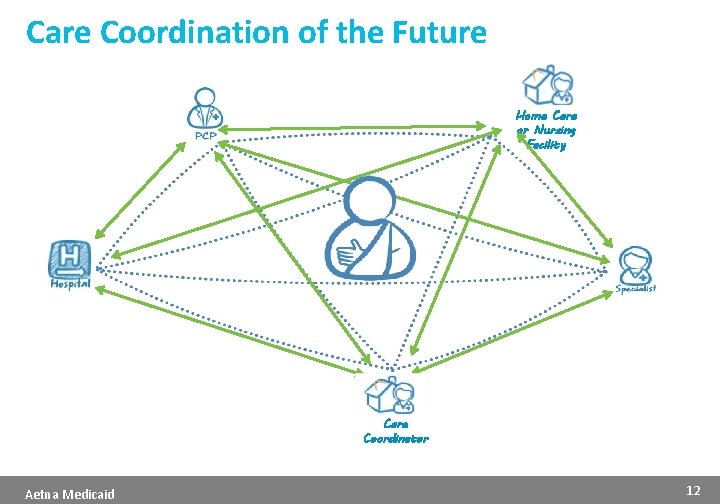
Care Coordination of the Future Home Care or Nursing Facility Care Coordinator Aetna Medicaid 12
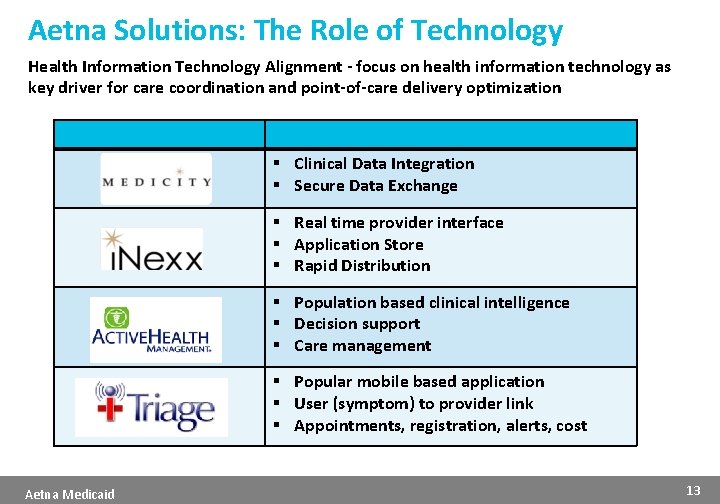
Aetna Solutions: The Role of Technology Health Information Technology Alignment - focus on health information technology as key driver for care coordination and point-of-care delivery optimization § Clinical Data Integration § Secure Data Exchange § Real time provider interface § Application Store § Rapid Distribution § Population based clinical intelligence § Decision support § Care management § Popular mobile based application § User (symptom) to provider link § Appointments, registration, alerts, cost Aetna Medicaid 13

A Partnership for the Future… Ø An Integrated System Ø The Right Experience Ø The Right Perspective Ø The Right Technology Ø The Right Results üHigh Quality üHigh Satisfaction üAligned Stakeholders üFuture Focused üCost Savings Thank You! Aetna Medicaid 14
 Long medium and short term planning in primary schools
Long medium and short term planning in primary schools Short term human resources
Short term human resources Difference between long term and short term liabilities
Difference between long term and short term liabilities Long term liabilities
Long term liabilities Long term goals
Long term goals Research paper on financial planning and forecasting
Research paper on financial planning and forecasting Long term memory vs short term memory
Long term memory vs short term memory Short short short long long long short short short
Short short short long long long short short short Once upon a time there lived a fox
Once upon a time there lived a fox Pinecrest supports and services center
Pinecrest supports and services center Aetna group number on card
Aetna group number on card Aetna cova health aware
Aetna cova health aware Aetna international log in
Aetna international log in Molina medicaid wv
Molina medicaid wv Rx bin number aetna
Rx bin number aetna