Adolescent SelfHarm January 2019 Dr Cathy Wainhouse Consultant
- Slides: 21
Adolescent Self-Harm January 2019 Dr Cathy Wainhouse Consultant Child and Adolescent Psychiatrist Barnet Adolescent Service Honorary Teaching Fellow Imperial College London
CAMHS Nationally- the perfect storm ● Big increases in morbidity ● ● ● Locally referral increase 100% in 3 years Decrease in social care support earlier, in at risk families Divorce/family conflict Parental substance misuse/mental health Decrease in school supports/increase in school stressors ● bullying/social media ● Self-harm very common response to teen stress
CAMHS – the history ● Child Guidance - small service, therapy based, ended at 16 years unless still in school ● Early 2000’s time of plenty ● Increase in funding- mental health grant ● Recognition of helping children would help keep adults well ● Reduction in stigma/taboos, more outreach/older adolescents, now mostly up to 18 years ● Every Child Matters 2003 (Climbié) ● Children’s Act 2004
National policies ● Children’s NSF www. csip. org. uk ● Every Child Matters www. everychildmatters. gov. uk ● NICE guidance ● Comprehensive CAMHS Young Minds ● Developing comprehensive CAMHS, a guide, which aims to help service commissioners, PCTs and other children's mental health services bridge the gap between the aspirations of national service framework and the reality of developing services on the ground. ● Five year plan, focus on crisis, OOH services
CAMHS – The History ● Times of austerity ● ● Cinderella’s poor friend Social care cuts to a service not ‘theirs’ (60%) Lack of understanding in NHS commissioning 77% CCGs froze or cut CAMHS budget 2014/15 ● Commons Select Committee 2014 ● Consternation but no new money ● money finally released 2016 ● Tier 4 beds increase - 50 ● Green Paper
Tier model ● Tier 1 - Universal - Thrive - Coping ● Any non mental health specialist talking to children about their mental health, YOU! ● Tier 2 - Targeted - Getting help ● A mental health specialist working in a non mental health setting e. g. psychologist in GP practice ● Tier 3 - Specialist - Getting more help/Risk support ● Outpatient CAMHS - multidisciplinary ● Tier 4 - Highly Specialist ● Specialist/inpatient CAMHS- current crisis
Self-harm ● starts at 12 -14 years, with adolescent stressors ● 12 -20% (Whitlock 2012) ● Now 25% ● Number of children admitted to hospital with self-harm increased by 68% in 10 years ● Increasing prevalence or less private/stigma?
Why do adolescents self-harm? ● To release tension/overwhelming feelings ● emotional regulation ● risk of becoming their normal coping strategy-habit ● to feel less numb (abuse) ● to get a rush ● Manage anxiety/low moods ● peer assimilation
Risk factors ● Low self-esteem ● school/family higher expectations ● family neglect/abuse ● conflict in family/close relationships ● Loss/significant relationship ending ● exposure to trauma ● persistent bullying or peer rejection ● poor communication skills
Risk Factors ● Worries/pressures related to school work ● Contagion/links with peers who self-harm ● including social media contacts ● difficulty making friends ● Sexual problems - including sexual identity ● early starting conduct disorder ● Alcohol/drug misuse ● poor physical health
Adolescence ● Time of moving from parental control to self-control ● Increase in anxiety and low moods ● particularly post menarche ● Increasing risk taking behaviour ● ? less alcohol/drug misuse ● Decreasing sensitivity to social cues ● decreasing consequential thinking
Suicide ● Rare, though seems to be increasing ● Data from the Office for National Statistics shows in 2015 there were 168 males aged 10 to 19 and 63 females in the same age group who took their own lives. ● highest rate since 2001 (231 cf 240) ● international problem ● Blue Whale Challenge/13 Reasons Why
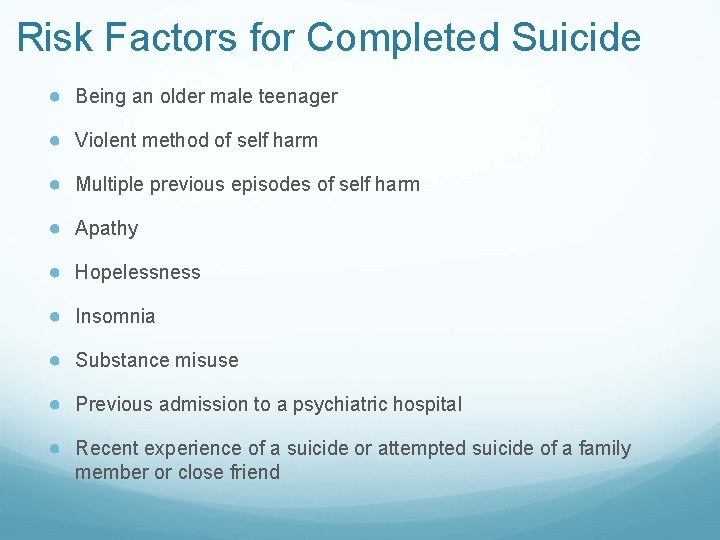
Risk Factors for Completed Suicide ● Being an older male teenager ● Violent method of self harm ● Multiple previous episodes of self harm ● Apathy ● Hopelessness ● Insomnia ● Substance misuse ● Previous admission to a psychiatric hospital ● Recent experience of a suicide or attempted suicide of a family member or close friend
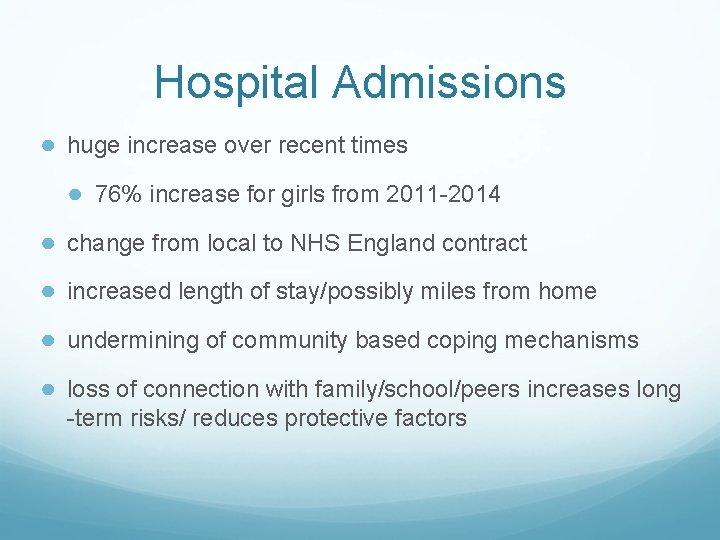
Hospital Admissions ● huge increase over recent times ● 76% increase for girls from 2011 -2014 ● change from local to NHS England contract ● increased length of stay/possibly miles from home ● undermining of community based coping mechanisms ● loss of connection with family/school/peers increases long -term risks/ reduces protective factors
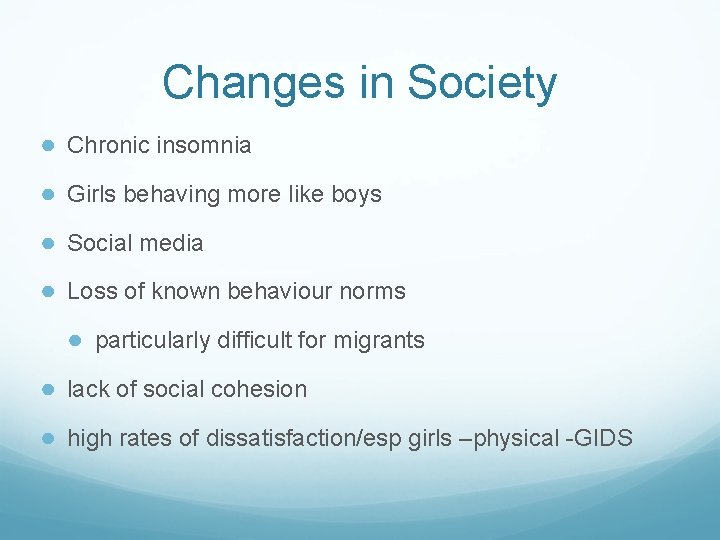
Changes in Society ● Chronic insomnia ● Girls behaving more like boys ● Social media ● Loss of known behaviour norms ● particularly difficult for migrants ● lack of social cohesion ● high rates of dissatisfaction/esp girls –physical -GIDS
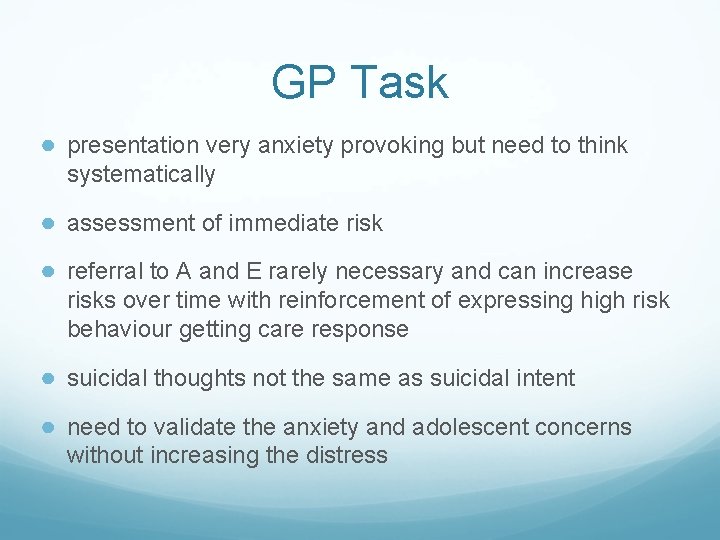
GP Task ● presentation very anxiety provoking but need to think systematically ● assessment of immediate risk ● referral to A and E rarely necessary and can increase risks over time with reinforcement of expressing high risk behaviour getting care response ● suicidal thoughts not the same as suicidal intent ● need to validate the anxiety and adolescent concerns without increasing the distress
Risk Assessment ● Dynamic, not box ticking ● hopelessness a concern ● adolescents work in absolutes, need to balance that ● PHQ-9 not a valid tool for adolescents ● distress vs depression ● Protective factors really important
GP tasks ● why asking for help now? ● has parent just found out? so their anxiety not the child’s? ● Need something to change in their life? ● situation become untenable? ● trying to communicate something else? (abuse) ● school requesting help?
Changing pathways to help ● not all adolescents who have self-harmed need to be seen in CAMHS ● school based problems best dealt with in school ● school counsellors and secondary project, HEWS ● Kooth project-online counselling ● other third sector supports (needs a lot more development) ● CAMHS for persistent long term self-harm and co-mormid mental health presentations
CAMHS ● BAS - Barnet Adolescent Service for longer term S-H ● contact to discuss if in doubt — 02087023444 ● standard referral form, case will be diverted ● based in Edgware but cover the whole borough
Longer Term Tasks ● Empowering parents to talk to their children and improve emotional literacy ● If parents don’t offer an emotional language, peers will and that is more likely to be maladaptive ● self-harm, eating restriction, conduct problems ● mismatch between intelligence and decreased consequential thinking
 Cathy wainhouse
Cathy wainhouse Selfharm definition
Selfharm definition Ib boundaries 2019
Ib boundaries 2019 Cathy abraham
Cathy abraham S. cathy sapp 7242582670
S. cathy sapp 7242582670 Gross anatomy of skeletal system
Gross anatomy of skeletal system Cathy jenner
Cathy jenner Cathy manduca
Cathy manduca Cathy blunt
Cathy blunt They say i say gerald graff summary
They say i say gerald graff summary Cathy landon
Cathy landon Cathy moore action mapping
Cathy moore action mapping Cathy has a nickel a dime
Cathy has a nickel a dime Cathy miller photography
Cathy miller photography Cathy legg
Cathy legg Cathy berkman
Cathy berkman East of eden trask family tree
East of eden trask family tree Kotter's 8 step model
Kotter's 8 step model Cathy curry ottawa
Cathy curry ottawa Cathy dunne
Cathy dunne Cathy alderman
Cathy alderman Cathy chuang
Cathy chuang