Trauma Informed Care DeEscalation IRC IN ATL Escalation

- Slides: 10
Trauma Informed Care & De-Escalation IRC IN ATL
Escalation Example from this week/month of a client (without identifying details) who may have been emotionally triggered? Why? How many of us have dealt with an escalating client or community member? Safety for ourselves AND for our clients = de-escalation

Trauma as a Trigger Definition of Psychological Trauma: “The cluster of symptoms, adaptations, and reactions that interfere with the daily functioning of an individual who has experienced extreme suffering (including neglect and deprivation) secondary to severe physical abuse and injury, sexual abuse, witnessing or surviving severe community or domestic violence…” Trauma Informed Care: The commitment of a “trauma informed” system is to provide all services in a manner that is welcoming and appropriate to the special needs of trauma survivors. Being trauma informed is being sensitive to impacts on client’s ability to cope, reason, react, process, and respond due to the psychological and physiological triggers of past trauma and providing services in this knowledge.
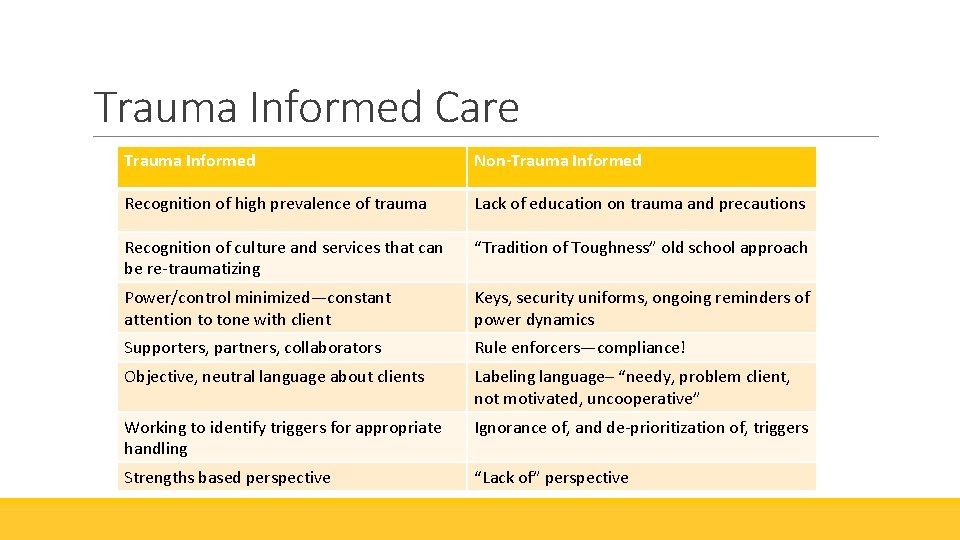
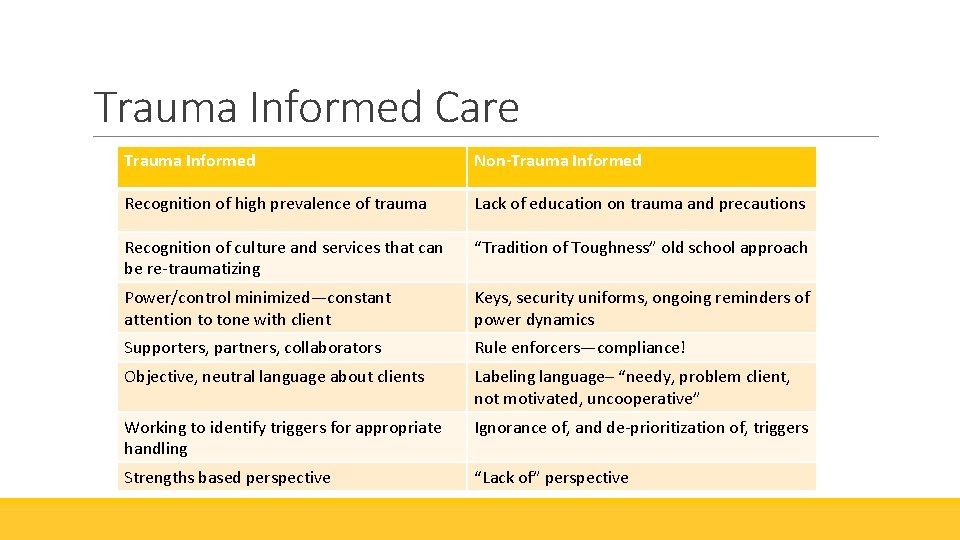
Trauma Informed Care Trauma Informed Non-Trauma Informed Recognition of high prevalence of trauma Lack of education on trauma and precautions Recognition of culture and services that can be re-traumatizing “Tradition of Toughness” old school approach Power/control minimized—constant attention to tone with client Keys, security uniforms, ongoing reminders of power dynamics Supporters, partners, collaborators Rule enforcers—compliance! Objective, neutral language about clients Labeling language– “needy, problem client, not motivated, uncooperative” Working to identify triggers for appropriate handling Ignorance of, and de-prioritization of, triggers Strengths based perspective “Lack of” perspective
Common service provision triggers for children: loud noises; hand or body gestures; confusion or chaos; transitions; change in routine; feelings of anger, sadness or fear that trigger similar feelings connected to past trauma; physical touch; emergency vehicles and police and fire personnel; and separation from caregivers. Potential triggers for adults may include: being misunderstood (linguistically and culturally); feelings of embarrassment and shame about challenges such as lack of housing; mental health or substance use issues; violence in the home; difficulties parenting; authority figures; not having choices or decision-making power; and practices that seem unfair or discriminatory.
Why is TIC Important for De-Escalation?
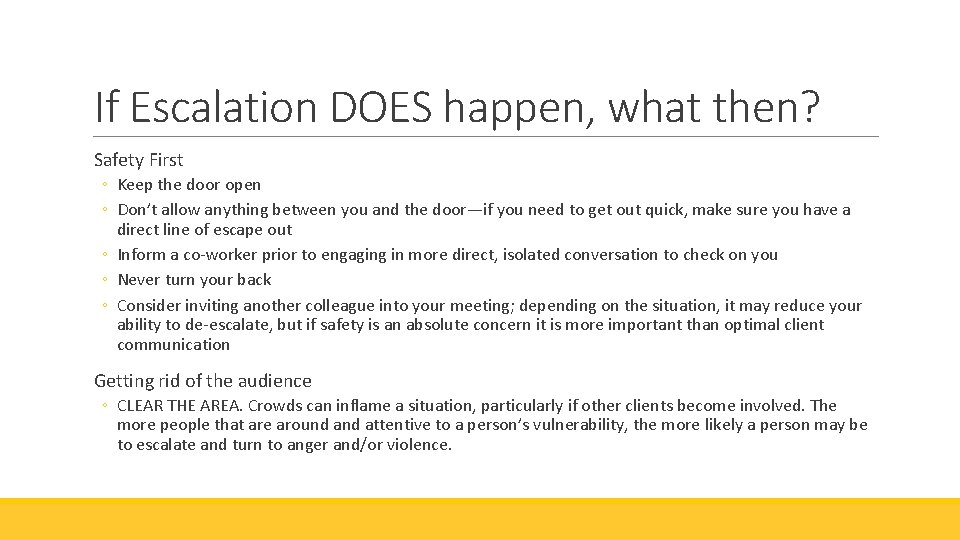
If Escalation DOES happen, what then? Safety First ◦ Keep the door open ◦ Don’t allow anything between you and the door—if you need to get out quick, make sure you have a direct line of escape out ◦ Inform a co-worker prior to engaging in more direct, isolated conversation to check on you ◦ Never turn your back ◦ Consider inviting another colleague into your meeting; depending on the situation, it may reduce your ability to de-escalate, but if safety is an absolute concern it is more important than optimal client communication Getting rid of the audience ◦ CLEAR THE AREA. Crowds can inflame a situation, particularly if other clients become involved. The more people that are around attentive to a person’s vulnerability, the more likely a person may be to escalate and turn to anger and/or violence.
If Escalation Happens Absolute Respect Our challenge is to maintain professionalism and to retain deep respect for the client throughout the intervention. We must treat clients with full dignity throughout their experience with us. Body Language Remember, de-escalation is abnormal. Your initial instincts are to flee or to take a defensive or offensive position. Remember to control your breathing to calm your natural ‘flight or fight’ instincts (as long as the situation is still safe!). ◦ Provide plenty of space to client ◦ Remain at same eye level as client—do not stand over client if they are seated. ◦ Position your body at an angle to the client—directly facing (chest to chest) can be interpreted subconsciously as aggressive, while an angled position diminishes this feeling and allows you a more direct escape if need be.
If Escalation Happens Listening ◦ It may be helpful to explain to the client that your goal is to listen to their feelings and concerns. Do not use this as an opportunity to ‘argue’ with a client about what you believe to have been true. Validation is key. If a client is escalating and talking too quickly, loudly, or impatiently (perhaps with an interpreter), you can say something along the lines of: ◦ “I really want to hear you, and I’m having trouble hearing what you’re saying when you’re talking this way. I am really here to listen, and I’m going to listen until you’re done talking.