The Impact of Regional STElevation Myocardial Infarction Systems
- Slides: 1
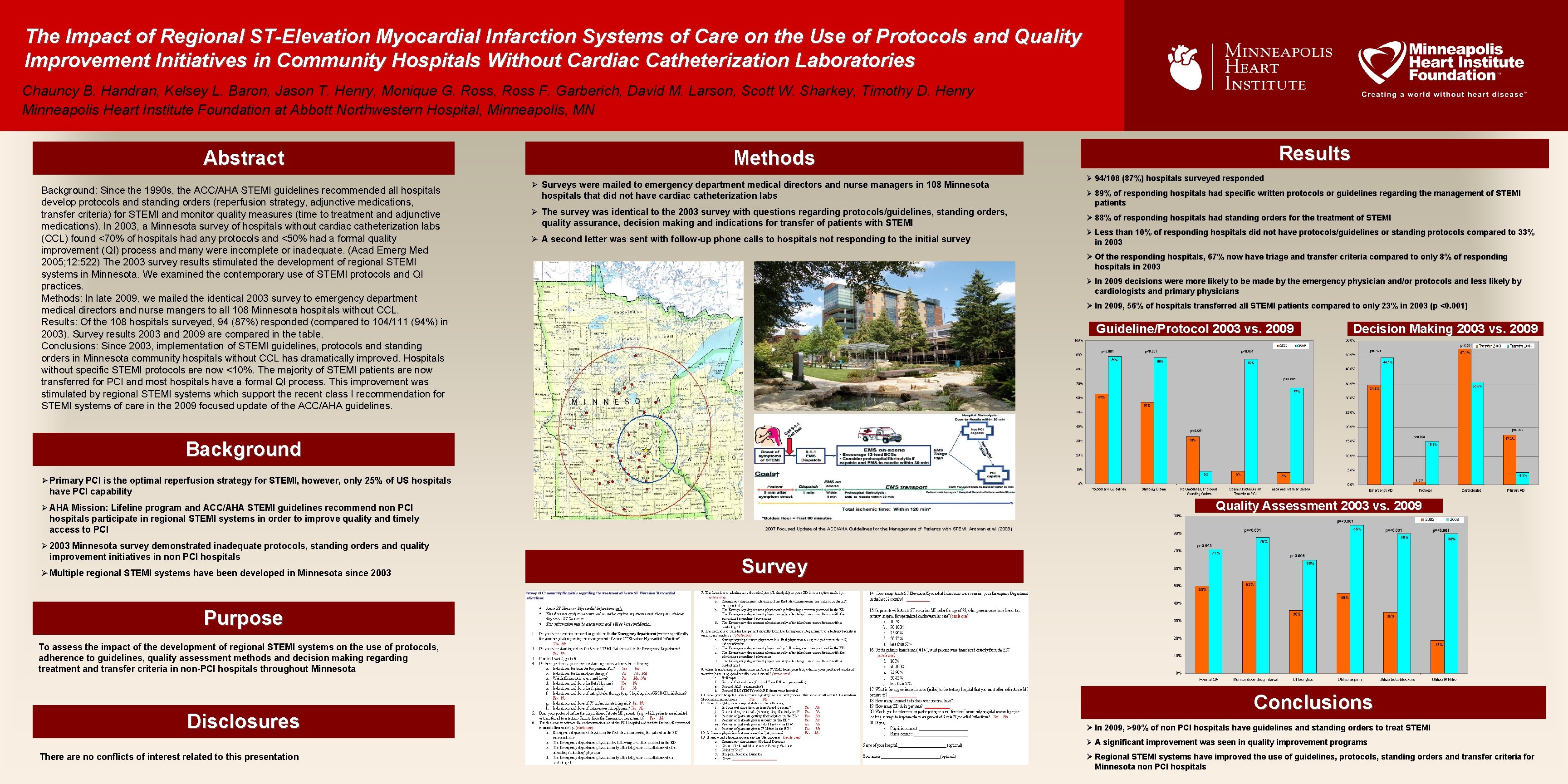
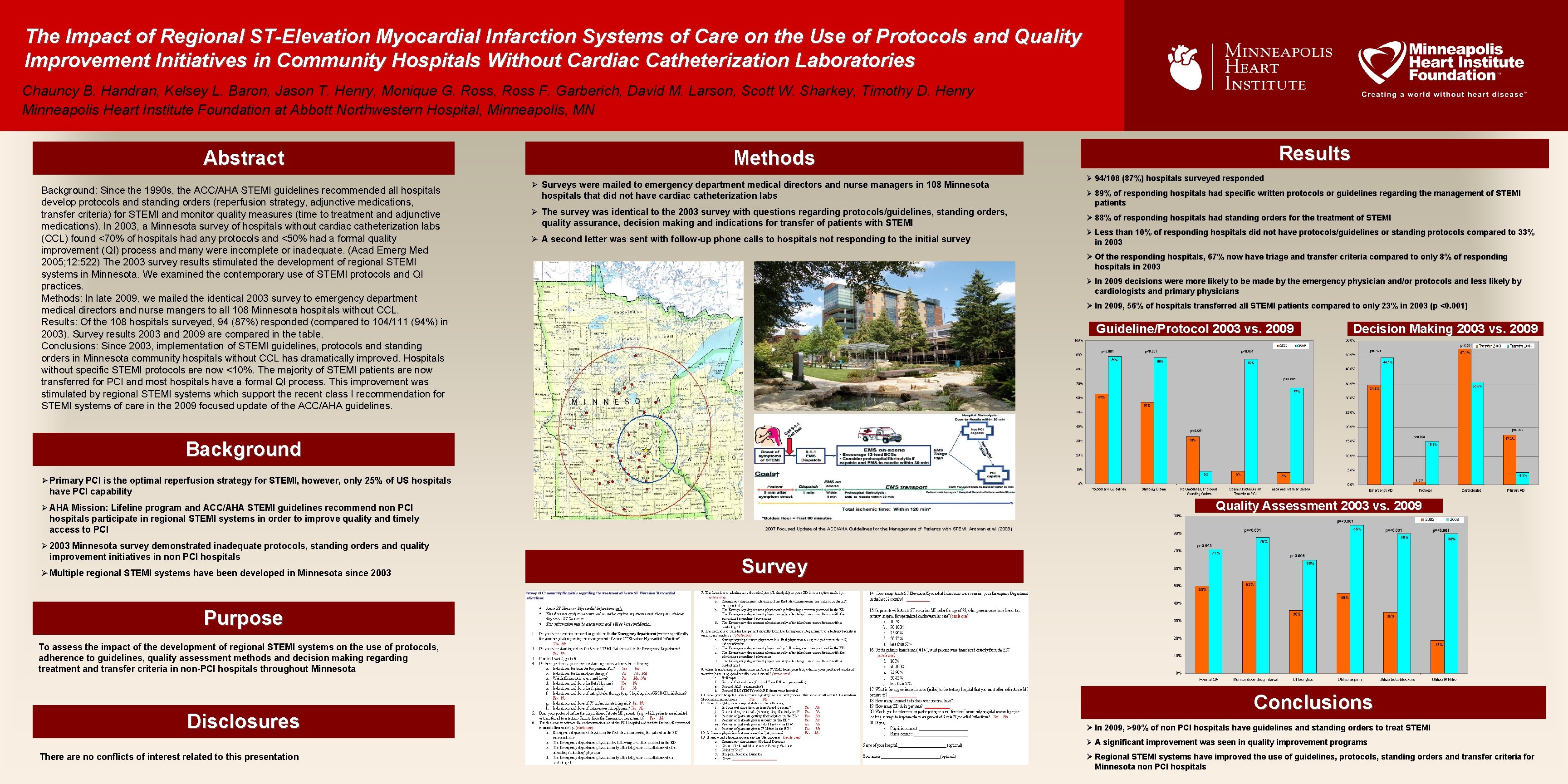
The Impact of Regional ST-Elevation Myocardial Infarction Systems of Care on the Use of Protocols and Quality Improvement Initiatives in Community Hospitals Without Cardiac Catheterization Laboratories Chauncy B. Handran, Kelsey L. Baron, Jason T. Henry, Monique G. Ross, Ross F. Garberich, David M. Larson, Scott W. Sharkey, Timothy D. Henry Minneapolis Heart Institute Foundation at Abbott Northwestern Hospital, Minneapolis, MN Abstract Background: Since the 1990 s, the ACC/AHA STEMI guidelines recommended all hospitals develop protocols and standing orders (reperfusion strategy, adjunctive medications, transfer criteria) for STEMI and monitor quality measures (time to treatment and adjunctive medications). In 2003, a Minnesota survey of hospitals without cardiac catheterization labs (CCL) found <70% of hospitals had any protocols and <50% had a formal quality improvement (QI) process and many were incomplete or inadequate. (Acad Emerg Med 2005; 12: 522) The 2003 survey results stimulated the development of regional STEMI systems in Minnesota. We examined the contemporary use of STEMI protocols and QI practices. Methods: In late 2009, we mailed the identical 2003 survey to emergency department medical directors and nurse mangers to all 108 Minnesota hospitals without CCL. Results: Of the 108 hospitals surveyed, 94 (87%) responded (compared to 104/111 (94%) in 2003). Survey results 2003 and 2009 are compared in the table. Conclusions: Since 2003, implementation of STEMI guidelines, protocols and standing orders in Minnesota community hospitals without CCL has dramatically improved. Hospitals without specific STEMI protocols are now <10%. The majority of STEMI patients are now transferred for PCI and most hospitals have a formal QI process. This improvement was stimulated by regional STEMI systems which support the recent class I recommendation for STEMI systems of care in the 2009 focused update of the ACC/AHA guidelines. Results Methods Ø Surveys were mailed to emergency department medical directors and nurse managers in 108 Minnesota hospitals that did not have cardiac catheterization labs Ø The survey was identical to the 2003 survey with questions regarding protocols/guidelines, standing orders, quality assurance, decision making and indications for transfer of patients with STEMI Ø A second letter was sent with follow-up phone calls to hospitals not responding to the initial survey Ø 94/108 (87%) hospitals surveyed responded Ø 89% of responding hospitals had specific written protocols or guidelines regarding the management of STEMI patients Ø 88% of responding hospitals had standing orders for the treatment of STEMI Ø Less than 10% of responding hospitals did not have protocols/guidelines or standing protocols compared to 33% in 2003 Ø Of the responding hospitals, 67% now have triage and transfer criteria compared to only 8% of responding hospitals in 2003 Ø In 2009 decisions were more likely to be made by the emergency physician and/or protocols and less likely by cardiologists and primary physicians Ø In 2009, 56% of hospitals transferred all STEMI patients compared to only 23% in 2003 (p <0. 001) 31 Community hospitals without PCI capability BLUE- Zone 1 (<90 minutes) Guideline/Protocol 2003 vs. 2009 RED- Zone 2 (90 -120 minutes) Decision Making 2003 vs. 2009 Background Ø Primary PCI is the optimal reperfusion strategy for STEMI, however, only 25% of US hospitals have PCI capability Ø AHA Mission: Lifeline program and ACC/AHA STEMI guidelines recommend non PCI hospitals participate in regional STEMI systems in order to improve quality and timely access to PCI Ø 2003 Minnesota survey demonstrated inadequate protocols, standing orders and quality improvement initiatives in non PCI hospitals Ø Multiple regional STEMI systems have been developed in Minnesota since 2003 Quality Assessment 2003 vs. 2009 2007 Focused Update of the ACC/AHA Guidelines for the Management of Patients with STEMI. Antman et al. (2008) Survey Purpose To assess the impact of the development of regional STEMI systems on the use of protocols, adherence to guidelines, quality assessment methods and decision making regarding treatment and transfer criteria in non-PCI hospitals throughout Minnesota Disclosures Conclusions Ø In 2009, >90% of non PCI hospitals have guidelines and standing orders to treat STEMI Ø A significant improvement was seen in quality improvement programs There are no conflicts of interest related to this presentation Ø Regional STEMI systems have improved the use of guidelines, protocols, standing orders and transfer criteria for Minnesota non PCI hospitals