Standardised Paediatric Parenteral Nutrition PN An opportunity to
- Slides: 1
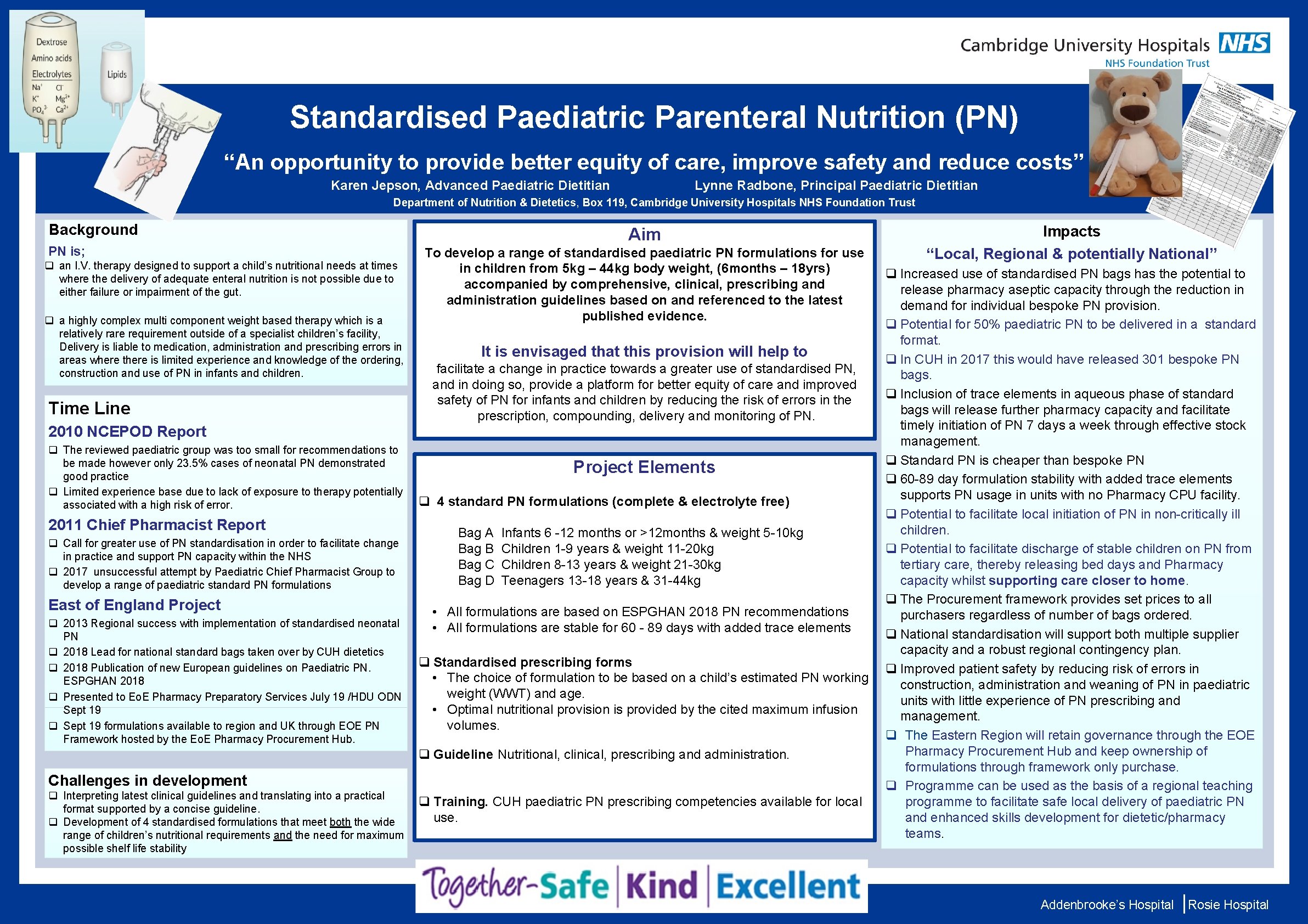
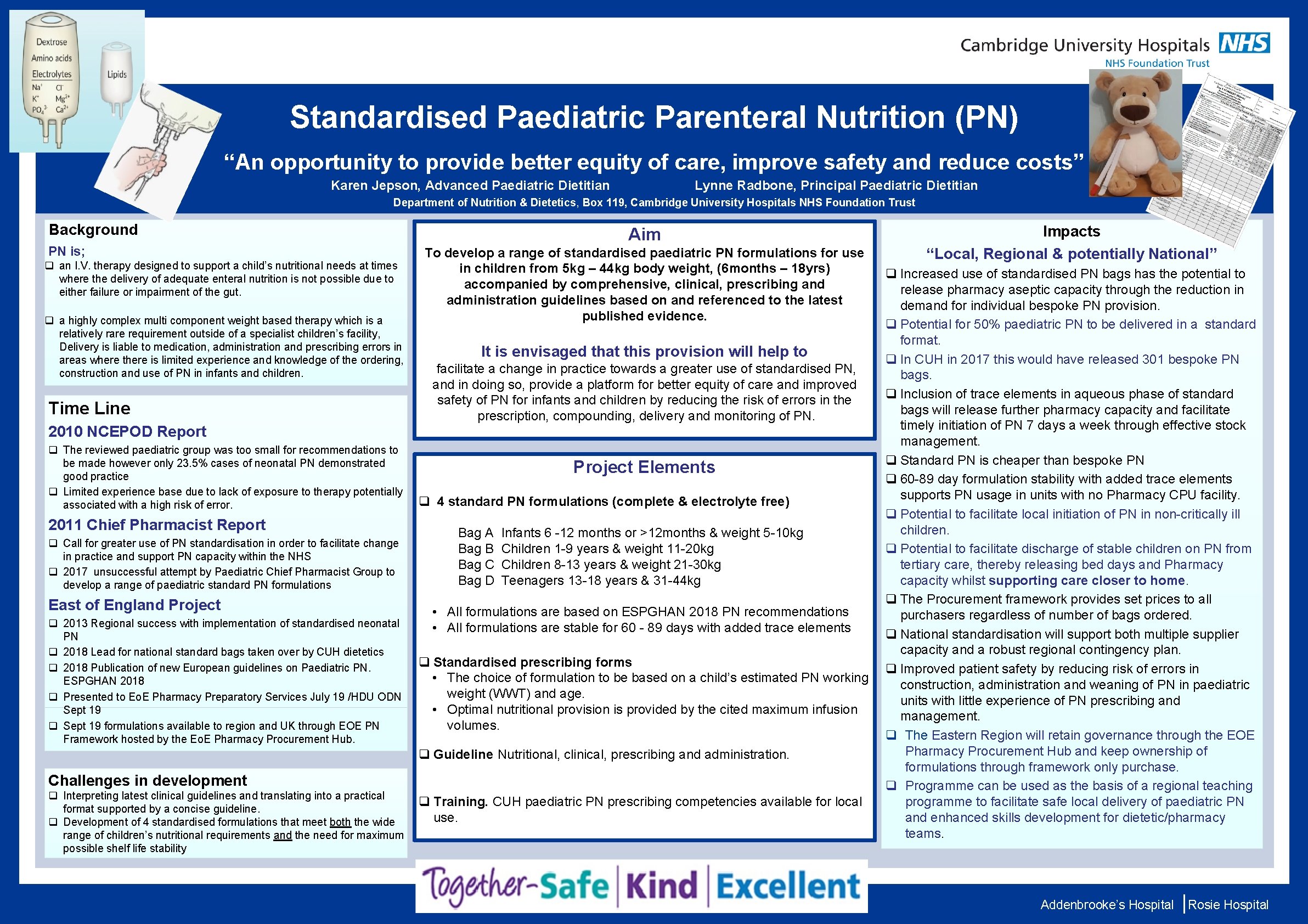
Standardised Paediatric Parenteral Nutrition (PN) “An opportunity to provide better equity of care, improve safety and reduce costs” Karen Jepson, Advanced Paediatric Dietitian Lynne Radbone, Principal Paediatric Dietitian Department of Nutrition & Dietetics, Box 119, Cambridge University Hospitals NHS Foundation Trust Background PN is; q an I. V. therapy designed to support a child’s nutritional needs at times where the delivery of adequate enteral nutrition is not possible due to either failure or impairment of the gut. Aim To develop a range of standardised paediatric PN formulations for use in children from 5 kg – 44 kg body weight, (6 months – 18 yrs) accompanied by comprehensive, clinical, prescribing and administration guidelines based on and referenced to the latest published evidence. Impacts “Local, Regional & potentially National” q Increased use of standardised PN bags has the potential to release pharmacy aseptic capacity through the reduction in demand for individual bespoke PN provision. q a highly complex multi component weight based therapy which is a q Potential for 50% paediatric PN to be delivered in a standard relatively rare requirement outside of a specialist children’s facility, format. Management: Delivery is liable to medication, administration and prescribing errors in It is envisaged that this provision will help to q In CUH in 2017 this would have released 301 bespoke PN areas where there is limited experience and knowledge of the ordering, • Intravenous Dextrose infusion with rates up to use 250 mls/hr of 20% Dextrose facilitate a change in practice towards a greater of standardised PN, construction and use of PN in infants and children. bags. and in doing so, provide a platform for better meals equity and of care and improved • Dietary intervention with frequent corn starch q Inclusion of trace elements in aqueous phase of standard safety of PN for infants and children by reducing the risk of errors in the bags will release further pharmacy capacity and facilitate Time Line • Diazoxide – intolerant leading todelivery hyponatraemia, oedema and nausea prescription, compounding, and monitoring of PN. timely initiation of PN 7 days a week through effective stock 2010 NCEPOD Report • Octreotide/glucagon intravenously – in order to replace counter-regulatory hormones management. q The reviewed paediatric group was too small for recommendations to q Standard PN is cheaper than bespoke PN 1 be made however only 23. 5% cases of neonatal PN demonstrated • Subcutaneous Octreotide hypoglycaemia worsened Project Elements good practice q 60 -89 day formulation stability with added trace elements q Limited experience base due to lack of exposure to therapy potentially • Prednisolone – developed fluid retention supports PN usage in units with no Pharmacy CPU facility. q 4 standard PN formulations (complete & electrolyte free) associated with a high risk of error. q Potential to facilitate initiation of PN in non-critically ill • Hepatic Arterial Embolisation (HAE) performed twice with initial improvement (post-procedure insulin 29 pmol/l), but relapsed after local 4 weeks. 2011 Chief Pharmacist Report children. Bag A Infants 6 -12 months or >12 months & weight 5 -10 kg q Call for greater use of PN standardisation in order to facilitate change q Potential to facilitate discharge of stable children on PN from Bag B Children 1 -9 years & weight 11 -20 kg in practice and support PN capacity within the NHS tertiary care, thereby releasing bed days and Pharmacy Bag C Children 8 -13 years & weight 21 -30 kg q 2017 unsuccessful attempt by Paediatric Chief Pharmacist Group to capacity whilst supporting care closer to home. Bag D Teenagers 13 -18 years & 31 -44 kg develop a range of paediatric standard PN formulations q The Procurement framework provides set prices to all East of England Project • All formulations are based on ESPGHAN 2018 PN recommendations purchasers regardless of number of bags ordered. q 2013 Regional success with implementation of standardised neonatal • All formulations are stable for 60 - 89 days with added trace elements q National standardisation will support both multiple supplier PN capacity and a robust regional contingency plan. q 2018 Lead for national standard bags taken over by CUH dietetics q Standardised prescribing forms q 2018 Publication of new European guidelines on Paediatric PN. q Improved patient safety by reducing risk of errors in • The choice of formulation to be based on a child’s estimated PN working ESPGHAN 2018 construction, administration and weaning of PN in paediatric weight (WWT) and age. q Presented to Eo. E Pharmacy Preparatory Services July 19 /HDU ODN units with little experience of PN prescribing and Sept 19 • Optimal nutritional provision is provided by the cited maximum infusion management. q Sept 19 formulations available to region and UK through EOE PN volumes. q The Eastern Region will retain governance through the EOE Framework hosted by the Eo. E Pharmacy Procurement Hub and keep ownership of q Guideline Nutritional, clinical, prescribing and administration. formulations through framework only purchase. Challenges in development q Programme can be used as the basis of a regional teaching q Interpreting latest clinical guidelines and translating into a practical programme to facilitate safe local delivery of paediatric PN q Training. CUH paediatric PN prescribing competencies available for local format supported by a concise guideline. and enhanced skills development for dietetic/pharmacy use. q Development of 4 standardised formulations that meet both the wide teams. range of children’s nutritional requirements and the need for maximum possible shelf life stability Addenbrooke’s Hospital Rosie Hospital