Spiritual Care Conference Can Spiritual Care Support Realistic





- Slides: 27

Spiritual Care Conference Can Spiritual Care Support Realistic Medicine in Practice? Often a patient’s distress is created by the situation they may find themselves in, rather than by the symptoms of the illness #spiritualcareconf 2/1/2022 1

Spiritual Care Conference Can Spiritual Care Support Realistic Medicine in Practice? Often a patient’s distress is created by the situation they may find themselves in, rather than by the symptoms of the illness
Spiritual Care? What do we mean we speak of ‘spirituality’? 2/1/2022 3
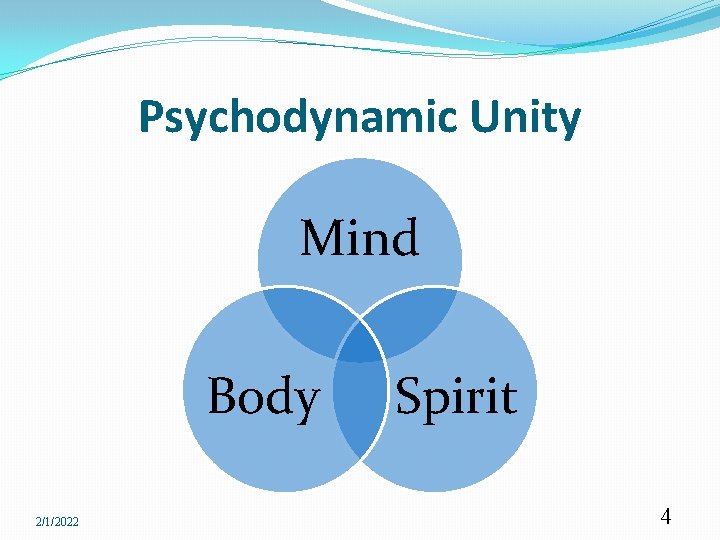
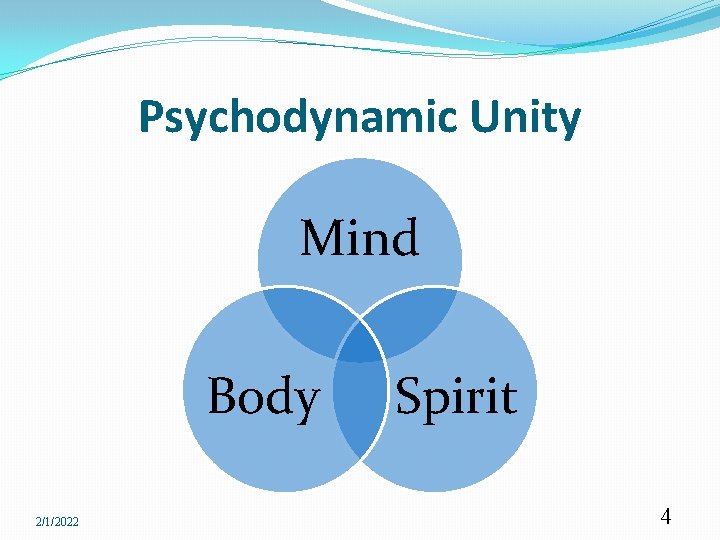
Psychodynamic Unity Mind Body 2/1/2022 Spirit 4
HDL (2002) 76 Spiritual Care in NHS Scotland Acknowledged spiritual and religious changes eg belief without Belonging Described relationship spiritual/religious Involving all staff not just chaplains A sensitive, non judgemental, person centred, culturally competent service Accepting WHO description which integrates spirituality as part of health 2/1/2022 5
Contemporary Spiritual Care It is widely recognised that the spiritual is a natural dimension of what it means to be human, which includes awareness of self, of relationships with others and with creation. Spiritual care is not necessarily religious. Religious care should always be spiritual 2/1/2022 6
Contemporary Spiritual Care is usually provided in a one to one relationship, is completely person centred and makes no assumptions about personal conviction or life orientation. Religious Care is provided in the context of shared religious beliefs, values, liturgies and lifestyle of a faith community. 2/1/2022 7
Among the basic spiritual needs that might be addressed within the normal, daily activity of healthcare are: The need to give and receive love The need to be understood The need to be valued as a human being The need forgiveness, hope and trust The need to explore beliefs and values The need to express feelings honestly The need to find meaning and purpose in life. 2/1/2022 8
Communication? Why is communication a barrier to realistic medicine? 2/1/2022 9
Background & context Scotland-wide survey, focus groups and interviews The majority of people in Scotland (70%) think that as a society we do not discuss death and dying enough (SPPC, 2003). This cultural resistance can contribute to poor communication when planning of end of life care (Scottish Government, 2008). 2/1/2022 10
Background & context cont: Living and Dying Well 2008 Short life Working Group 7 Report 2010 Stakeholder Group March 2011 CEL 2011 Shaping Bereavement Care Scottish Patient Safety Programme Fellowship 2012 “What matters to you”? IHI Conversation Ready 2015 Strategic Framework for Action on Palliative and End of Life Care 2016 2/1/2022 11
Background & context cont: Chief Medical Officer’s Reports 2016 – 2018 Realistic Medicine 2016 Realising Realistic Medicine 2017 Practising Realistic Medicine 2018 “Poor communication is the biggest source of complaints in the NHS, and she says there are too many examples of families being distraught at the overtreatment of loved ones at the end of life when they would have preferred less to be done”. (Catherine Calderwood, BMJ 2016; 355: i 5455 ) 2/1/2022 12
1998 Thesis: PALLIATIVE CARE : A THEOLOGICAL FOUNDATION “. . . a “good death” can be achieved when the dying person is relieved not only of their physical pain but also of their emotional pain and relief of emotional pain is somewhat achievable through good honest and open communication. . . ” George Beuken; Scottish Journal of Healthcare Chaplaincy Vol. . 6 No. 1 2003 2/1/2022 13
Vision Scotland should be a society in which dealing with death, dying, bereavement and loss in a healthy and constructive way is seen as part of ordinary life and where members of the public and health and social care professionals and volunteers have awareness of these issues and the many ways in which communities and individuals can support each other 2/1/2022 14

The Great Taboo Conversations around Death & Dying
Fear 2/1/2022 17
The Scale of the Problem Unnecessary harm is caused because people in Scotland are not open about death, dying and bereavement. For example: People who are dying or bereaved can experience isolation because people don't know what to say or how to act towards them People die without wills, leaving complicated situations for their families and friends. Health care professionals struggle to have conversations with their patients about what care or treatments they want as they approach death. This makes it hard to plan the care that a person really wants If the fact that someone is dying is not acknowledged then opportunities to resolve issues and say goodbye may be missed
2/1/2022 19
Breaking the Taboo How? 2/1/2022 20
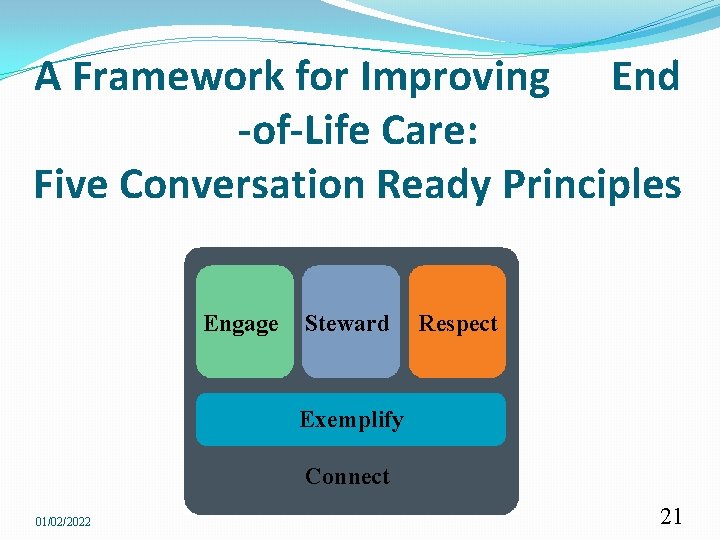
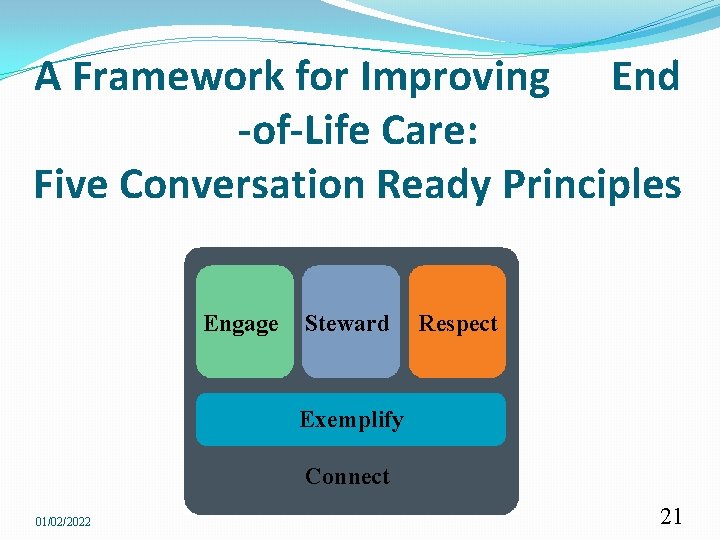
A Framework for Improving End -of-Life Care: Five Conversation Ready Principles Engage Steward Respect Exemplify Connect 01/02/2022 21
Exemplify this work in our own lives, so that we fully understand the benefits and challenges This principle embodies “walk the walk” and encourages all clinicians to “have the conversation” with their own families and loved ones about end-of-life care wishes. Through IHI’s work, we gained increased confidence that this is an important starting point with organizations involved in Conversation Ready work — not just a “nice to have” but, in many cases, essential to achieving their aims. 01/02/2022 22

I didn't want that Notice Wonder Realise 2/1/2022 24
Key Messages Being more open about death is a good thing Death is normal Thinking about death when you’re healthy means there is less to think about if you get sick We can all help each other with death, dying and bereavement Coming terms with your own mortality can help you to live life to the full There are things individuals and communities can actively do to help friends through difficult times relating to death, dying and bereavement Death is happening all around us, causing sadness and difficulties that people often don’t share Death can be upsetting, and people need to take the time to grieve
Useful Resources Good life, Good death, Good Grief http: //www. goodlifedeathgrief. org. uk/ Dying Matters http: //www. dyingmatters. org/overview/resources

 1 corinthians 2:9-13
1 corinthians 2:9-13 Golden rule
Golden rule What is spiritual care
What is spiritual care What is spiritual care
What is spiritual care Major support and minor support
Major support and minor support Health care levels primary secondary tertiary
Health care levels primary secondary tertiary Jigsaw classroom psychology definition
Jigsaw classroom psychology definition Realistic fiction definition
Realistic fiction definition Realistic fiction defintion
Realistic fiction defintion The hello goodbye window summary
The hello goodbye window summary Realistic conflict theory
Realistic conflict theory Realistic conflict theory
Realistic conflict theory Realistic conflict theory
Realistic conflict theory Characteristics of mystery flash fiction
Characteristics of mystery flash fiction Mystery
Mystery Semi realistic mannequin
Semi realistic mannequin Characteristics of realism in theatre
Characteristics of realism in theatre Magical realism vs fantasy
Magical realism vs fantasy Historical story
Historical story Performer audience director scenery aspects
Performer audience director scenery aspects Maddie lambert
Maddie lambert Realistic conflict theory
Realistic conflict theory George bernard shaw naturalism
George bernard shaw naturalism Realistic fiction story ideas for 7th grade
Realistic fiction story ideas for 7th grade Specific measurable attainable realistic timely
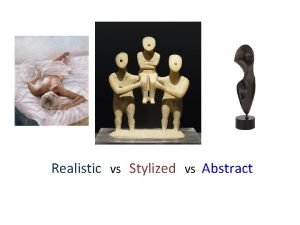
Specific measurable attainable realistic timely Stylized vs realistic
Stylized vs realistic Realistic constraints
Realistic constraints Monsters inc realistic
Monsters inc realistic