Sedation Selection Minimizing the Occurrence of Patient Complications
- Slides: 1
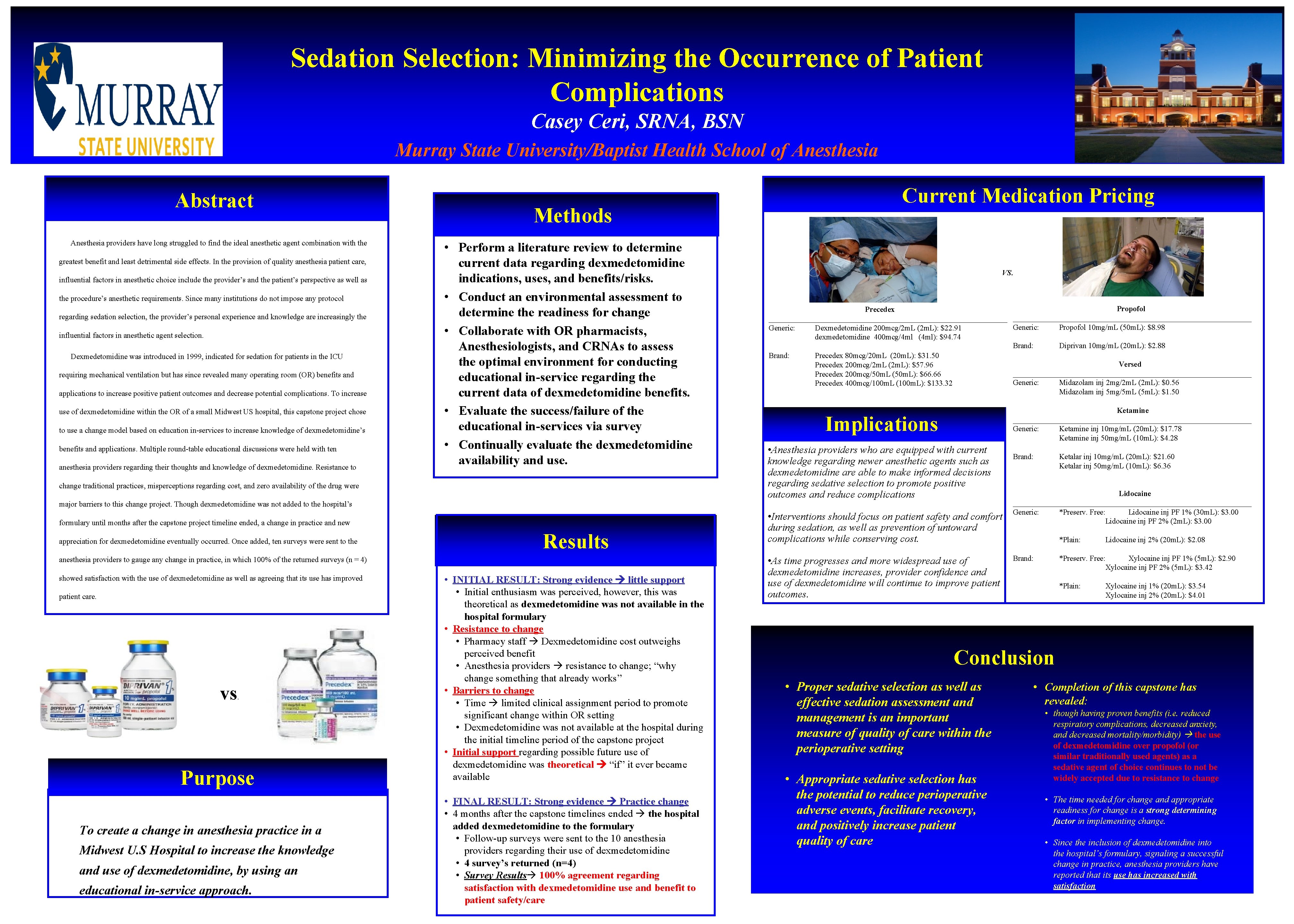
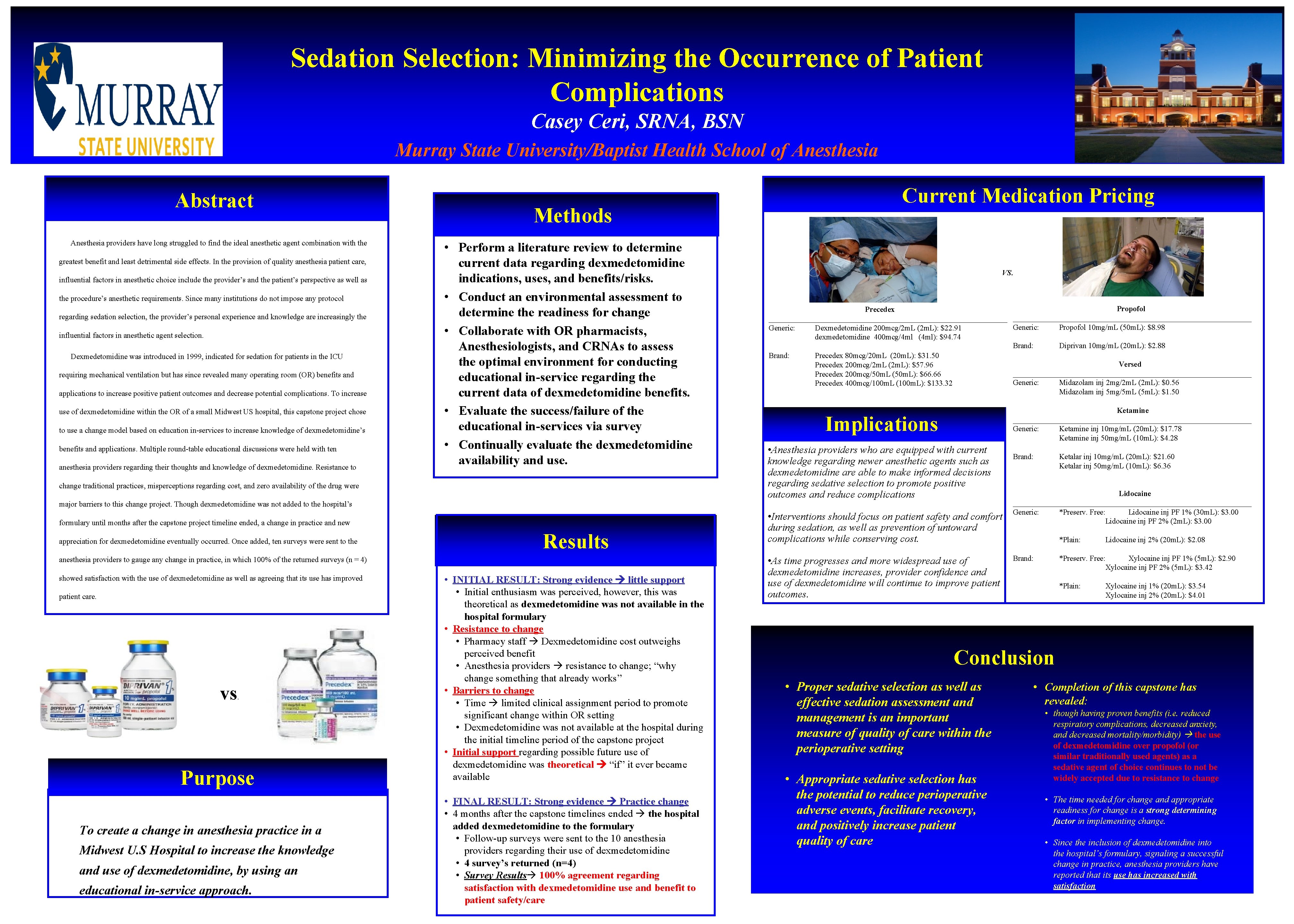
Sedation Selection: Minimizing the Occurrence of Patient Complications Casey Ceri, SRNA, BSN Murray State University/Baptist Health School of Anesthesia Abstract Anesthesia providers have long struggled to find the ideal anesthetic agent combination with the greatest benefit and least detrimental side effects. In the provision of quality anesthesia patient care, influential factors in anesthetic choice include the provider’s and the patient’s perspective as well as the procedure’s anesthetic requirements. Since many institutions do not impose any protocol regarding sedation selection, the provider’s personal experience and knowledge are increasingly the influential factors in anesthetic agent selection. Dexmedetomidine was introduced in 1999, indicated for sedation for patients in the ICU requiring mechanical ventilation but has since revealed many operating room (OR) benefits and applications to increase positive patient outcomes and decrease potential complications. To increase use of dexmedetomidine within the OR of a small Midwest US hospital, this capstone project chose to use a change model based on education in-services to increase knowledge of dexmedetomidine’s benefits and applications. Multiple round-table educational discussions were held with ten anesthesia providers regarding their thoughts and knowledge of dexmedetomidine. Resistance to Methods • Perform a literature review to determine current data regarding dexmedetomidine indications, uses, and benefits/risks. • Conduct an environmental assessment to determine the readiness for change • Collaborate with OR pharmacists, Anesthesiologists, and CRNAs to assess the optimal environment for conducting educational in-service regarding the current data of dexmedetomidine benefits. • Evaluate the success/failure of the educational in-services via survey • Continually evaluate the dexmedetomidine availability and use. change traditional practices, misperceptions regarding cost, and zero availability of the drug were Current Medication Pricing VS. Propofol Precedex ______________________________________________________________ Generic: Propofol 10 mg/m. L (50 m. L): $8. 98 Generic: Dexmedetomidine 200 mcg/2 m. L (2 m. L): $22. 91 dexmedetomidine 400 mcg/4 ml (4 ml): $94. 74 Brand: Diprivan 10 mg/m. L (20 m. L): $2. 88 Brand: Precedex 80 mcg/20 m. L (20 m. L): $31. 50 Versed Precedex 200 mcg/2 m. L (2 m. L): $57. 96 _______________________________ Precedex 200 mcg/50 m. L (50 m. L): $66. 66 Generic: Midazolam inj 2 mg/2 m. L (2 m. L): $0. 56 Precedex 400 mcg/100 m. L (100 m. L): $133. 32 Midazolam inj 5 mg/5 m. L (5 m. L): $1. 50 Ketamine _______________________________ Generic: Ketamine inj 10 mg/m. L (20 m. L): $17. 78 Ketamine inj 50 mg/m. L (10 m. L): $4. 28 Implications • Anesthesia providers who are equipped with current knowledge regarding newer anesthetic agents such as dexmedetomidine are able to make informed decisions regarding sedative selection to promote positive outcomes and reduce complications major barriers to this change project. Though dexmedetomidine was not added to the hospital’s formulary until months after the capstone project timeline ended, a change in practice and new appreciation for dexmedetomidine eventually occurred. Once added, ten surveys were sent to the Results anesthesia providers to gauge any change in practice, in which 100% of the returned surveys (n = 4) showed satisfaction with the use of dexmedetomidine as well as agreeing that its use has improved patient care. vs . Purpose To create a change in anesthesia practice in a Midwest U. S Hospital to increase the knowledge and use of dexmedetomidine, by using an educational in-service approach. • INITIAL RESULT: Strong evidence little support • Initial enthusiasm was perceived, however, this was theoretical as dexmedetomidine was not available in the hospital formulary • Resistance to change • Pharmacy staff Dexmedetomidine cost outweighs perceived benefit • Anesthesia providers resistance to change; “why change something that already works” • Barriers to change • Time limited clinical assignment period to promote significant change within OR setting • Dexmedetomidine was not available at the hospital during the initial timeline period of the capstone project • Initial support regarding possible future use of dexmedetomidine was theoretical “if” it ever became available • FINAL RESULT: Strong evidence Practice change • 4 months after the capstone timelines ended the hospital added dexmedetomidine to the formulary • Follow-up surveys were sent to the 10 anesthesia providers regarding their use of dexmedetomidine • 4 survey’s returned (n=4) • Survey Results 100% agreement regarding satisfaction with dexmedetomidine use and benefit to patient safety/care • Interventions should focus on patient safety and comfort during sedation, as well as prevention of untoward complications while conserving cost. • As time progresses and more widespread use of dexmedetomidine increases, provider confidence and use of dexmedetomidine will continue to improve patient outcomes. Brand: Ketalar inj 10 mg/m. L (20 m. L): $21. 60 Ketalar inj 50 mg/m. L (10 m. L): $6. 36 Lidocaine _______________________________ Generic: *Preserv. Free: Lidocaine inj PF 1% (30 m. L): $3. 00 Lidocaine inj PF 2% (2 m. L): $3. 00 *Plain: Brand: Lidocaine inj 2% (20 m. L): $2. 08 *Preserv. Free: Xylocaine inj PF 1% (5 m. L): $2. 90 Xylocaine inj PF 2% (5 m. L): $3. 42 *Plain: Xylocaine inj 1% (20 m. L): $3. 54 Xylocaine inj 2% (20 m. L): $4. 01 Conclusion • Proper sedative selection as well as effective sedation assessment and management is an important measure of quality of care within the perioperative setting • Appropriate sedative selection has the potential to reduce perioperative adverse events, facilitate recovery, and positively increase patient quality of care • Completion of this capstone has revealed: • though having proven benefits (i. e. reduced respiratory complications, decreased anxiety, and decreased mortality/morbidity) the use of dexmedetomidine over propofol (or similar traditionally used agents) as a sedative agent of choice continues to not be widely accepted due to resistance to change • The time needed for change and appropriate readiness for change is a strong determining factor in implementing change. • Since the inclusion of dexmedetomidine into the hospital’s formulary, signaling a successful change in practice, anesthesia providers have reported that its use has increased with satisfaction