Policy Implications for Rural Healthcare Innovations in Rural



- Slides: 16

Policy Implications for Rural Healthcare Innovations in Rural Healthcare Environments Symposium Brock Slabach, MPH, FACHE Senior Vice President for Member Services National Rural Health Association

Improving the health of the 62 million who call rural America home. NRHA is non-profit and non-partisan.

Destination NRHA Plan now to attend these upcoming events. Annual Conference – May 10 -13, 2016 • Minneapolis, MN Rural Hospital Innovation Summit – May 10 -13, 2016 • Minneapolis, MN Quality Clinical Conference – Jul. 13 -15, 2016 • Oakland, CA RHC/CAH Conference – Sept. 20 -23, 2016 • Kansas City, MO Policy Institute—February 6 -9, 2017 • Washington, DC Visit Rural. Health. Web. org for details and discounts. 3
A History (short) of Rural Health • • • War on Poverty in the 60’s Community Health Centers, created in the War on Poverty Rural Health Clinics – 38 Years Old (1978), 4, 100 nationwide Result of PPS 1983: 440 hospital closures Policy Response 1992 -2003: – – – State Office of Rural Health (SORH Medicare Dependent Hospitals (MDH) Critical Access Hospital (CAH) 1997 Medicare Rural Flexibility Program (1997) Low-Volume Hospital (LVH) Adjustment (2003 and 2010) • Patient Protection and Affordable Care Act (ACA) 2010 • Medicare Access and Chip Reauthorization Act (MACRA) 2015
Rural Hospital Overview • Total Rural Hospitals: 1, 855 – 1, 333 Critical Access Hospitals (CAH) – 522 Prospective Payment System (PPS) Hospitals (less than 100 staffed beds) • CAH: Paid on Cost Based Reimbursement (CBR) • PPS: Paid on a Diagnosis Related Group (DRG), with a prospective rate
NRHA Analysis of Rural Hospitals Target solutions for three cohorts of rural hospitals: • At high-risk of closure (n=210) • At-risk of closure (n=463) • Stable with strategically sound fundamentals (n=974) • High-performers or first movers (n=208)
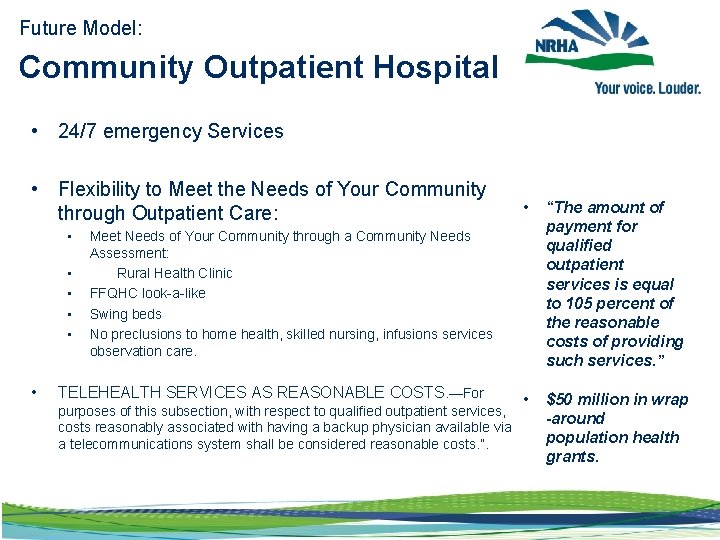
Future Model: Community Outpatient Hospital • 24/7 emergency Services • Flexibility to Meet the Needs of Your Community through Outpatient Care: • • “The amount of payment for qualified outpatient services is equal to 105 percent of the reasonable costs of providing such services. ” • $50 million in wrap -around population health grants. Meet Needs of Your Community through a Community Needs Assessment: Rural Health Clinic FFQHC look-a-like Swing beds No preclusions to home health, skilled nursing, infusions services observation care. TELEHEALTH SERVICES AS REASONABLE COSTS. —For purposes of this subsection, with respect to qualified outpatient services, costs reasonably associated with having a backup physician available via a telecommunications system shall be considered reasonable costs. ”.
Rural Innovation Volume to Results: A major leap
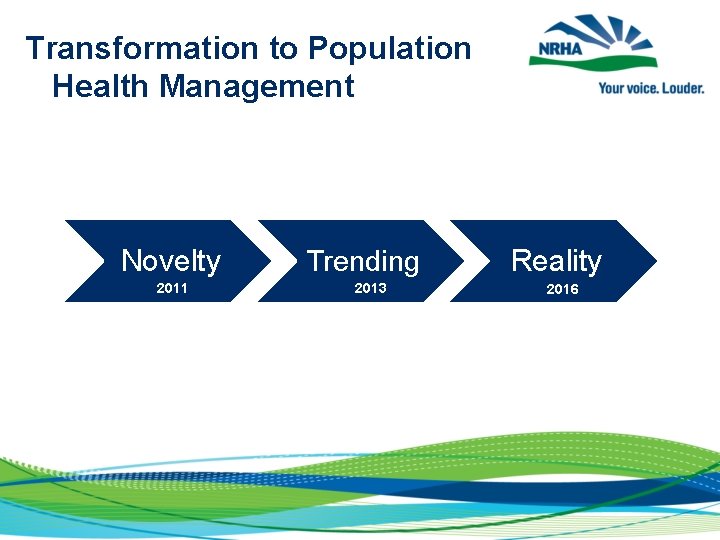
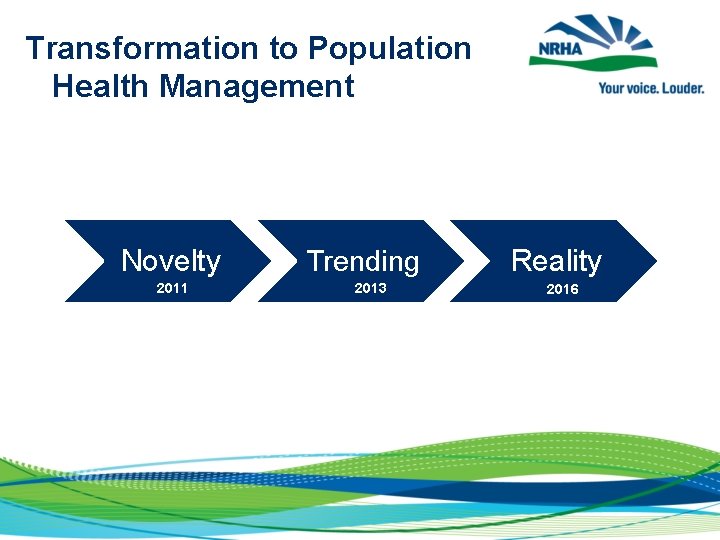
Transformation to Population Health Management Novelty 2011 Trending 2013 Reality 2016
Sec. Burwell’s Medicare Goals • 30% of Medicare provider payments in APMs by 2016 • 50% of Medicare provider payments in APMs by 2018 • 85% of Medicare fee-for-service payments to be tied to quality and value by 2016 • 90% of Medicare fee-for-service payments to be tied to quality and value by 2018
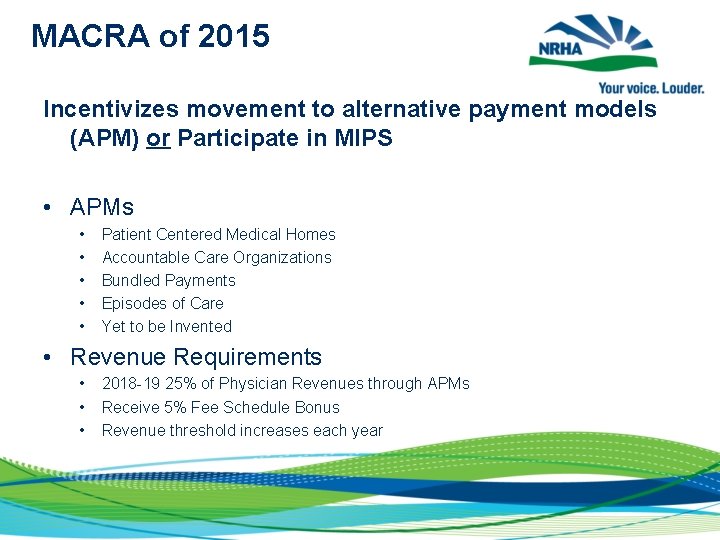
MACRA of 2015 Incentivizes movement to alternative payment models (APM) or Participate in MIPS • APMs • • • Patient Centered Medical Homes Accountable Care Organizations Bundled Payments Episodes of Care Yet to be Invented • Revenue Requirements • • • 2018 -19 25% of Physician Revenues through APMs Receive 5% Fee Schedule Bonus Revenue threshold increases each year
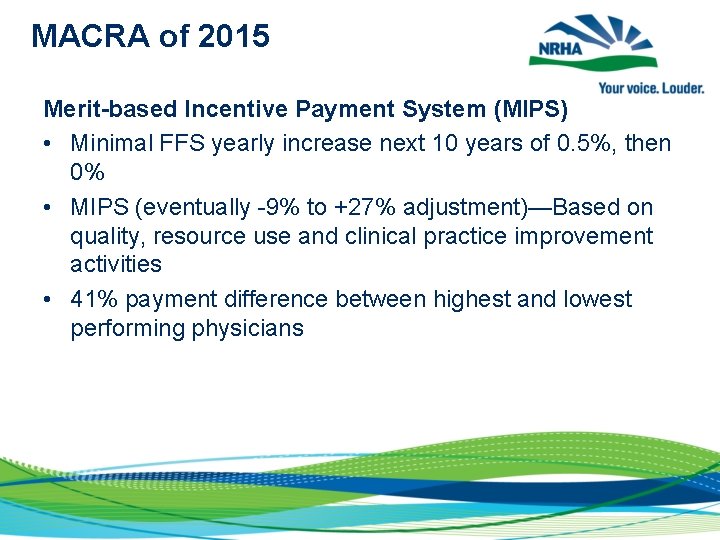
MACRA of 2015 Merit-based Incentive Payment System (MIPS) • Minimal FFS yearly increase next 10 years of 0. 5%, then 0% • MIPS (eventually -9% to +27% adjustment)—Based on quality, resource use and clinical practice improvement activities • 41% payment difference between highest and lowest performing physicians
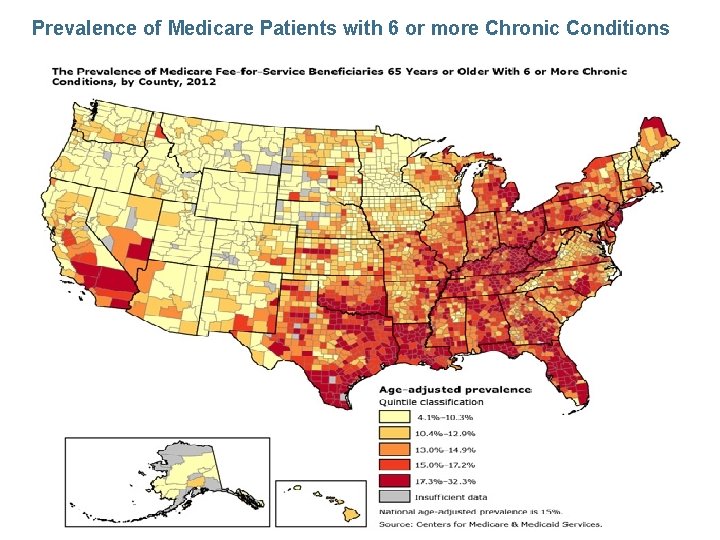
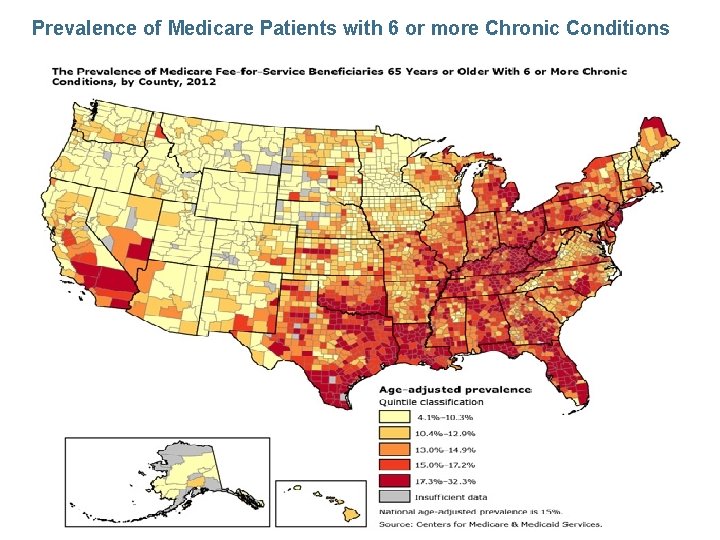
Prevalence of Medicare Patients with 6 or more Chronic Conditions
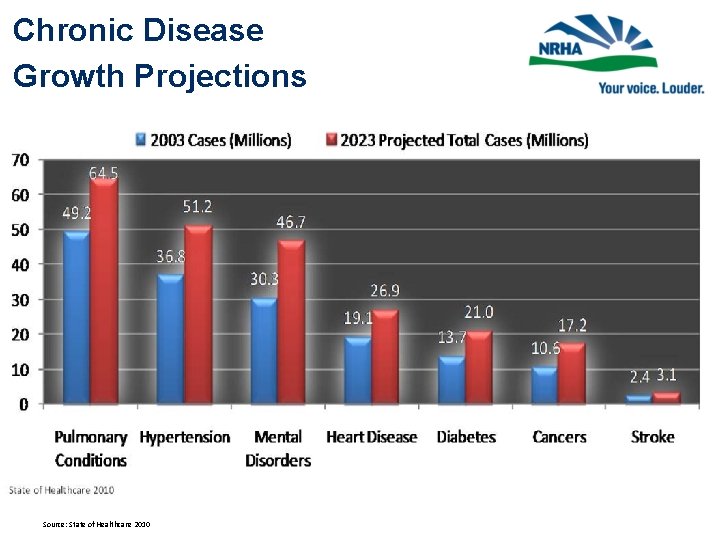
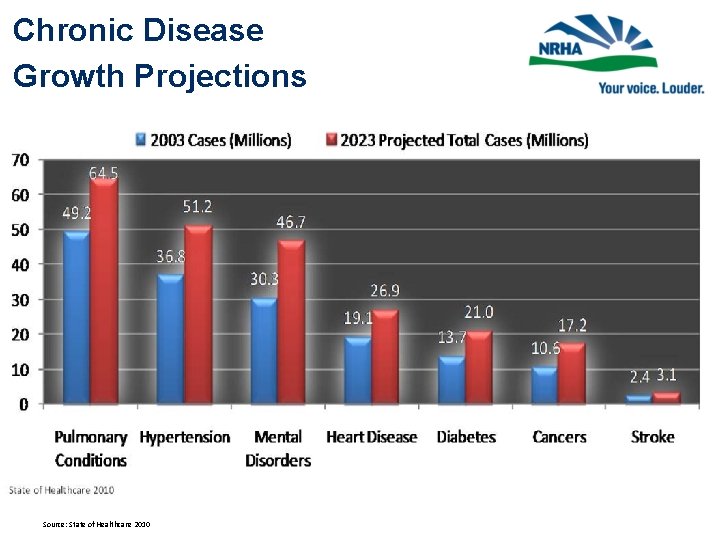
Chronic Disease Growth Projections Source: State of Healthcare 2010
What are the regulatory implications for rural healthcare design? • • • Aggressive review of bricks & mortar budgets Becoming “hospital without walls” Form follows finance: MACRA changes the finance Delivery System Reform (DSR) flows from APMs Increasing reliance on data analytics to improve health status • Telehealth strategies to intensify • Providers navigating the rapids of volume to value
THANK YOU Brock Slabach, MPH, FACHE Senior Vice President for Member Services National Rural Health Association bslabach@nrharural. org
 Sports medicine definition
Sports medicine definition Healthcare and the healthcare team chapter 2
Healthcare and the healthcare team chapter 2 Nursing informatics and healthcare policy
Nursing informatics and healthcare policy Discussion and implications
Discussion and implications Eng2d media unit
Eng2d media unit What are legal implications
What are legal implications Educational implications of learning curve
Educational implications of learning curve Legal implications in nursing practice
Legal implications in nursing practice Philosphy theories
Philosphy theories Ranexa nursing implications
Ranexa nursing implications Implication table method
Implication table method Implications of nativist theory
Implications of nativist theory Guided participation vygotsky examples
Guided participation vygotsky examples Marketing implications
Marketing implications Educational implications of existentialism
Educational implications of existentialism Implications of quantum entanglement
Implications of quantum entanglement Consumer behavior cengage
Consumer behavior cengage