PEDIATRIC ACUTE SCROTUM DIAGNOSTICS AND TREATMENT EVALUATION AT
- Slides: 1
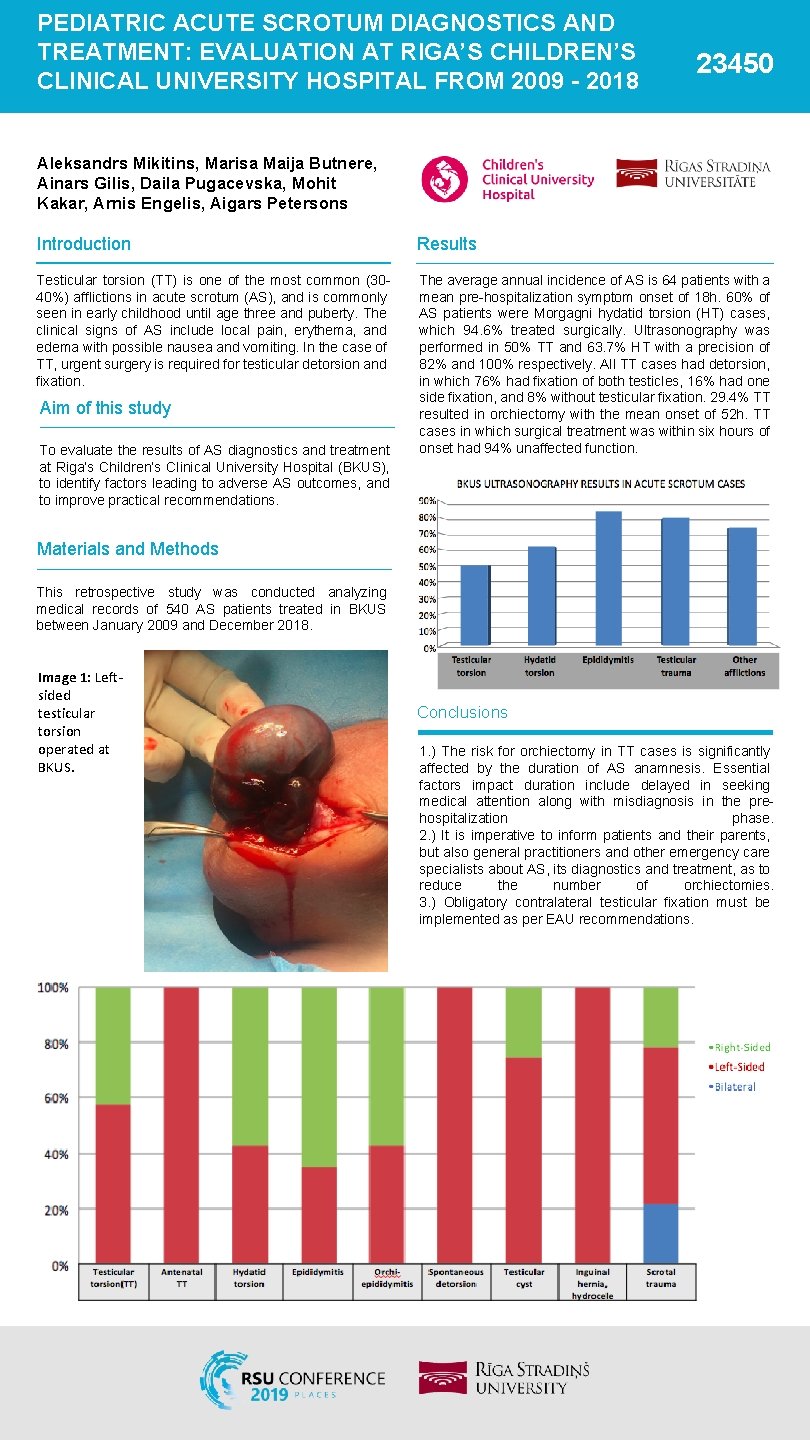
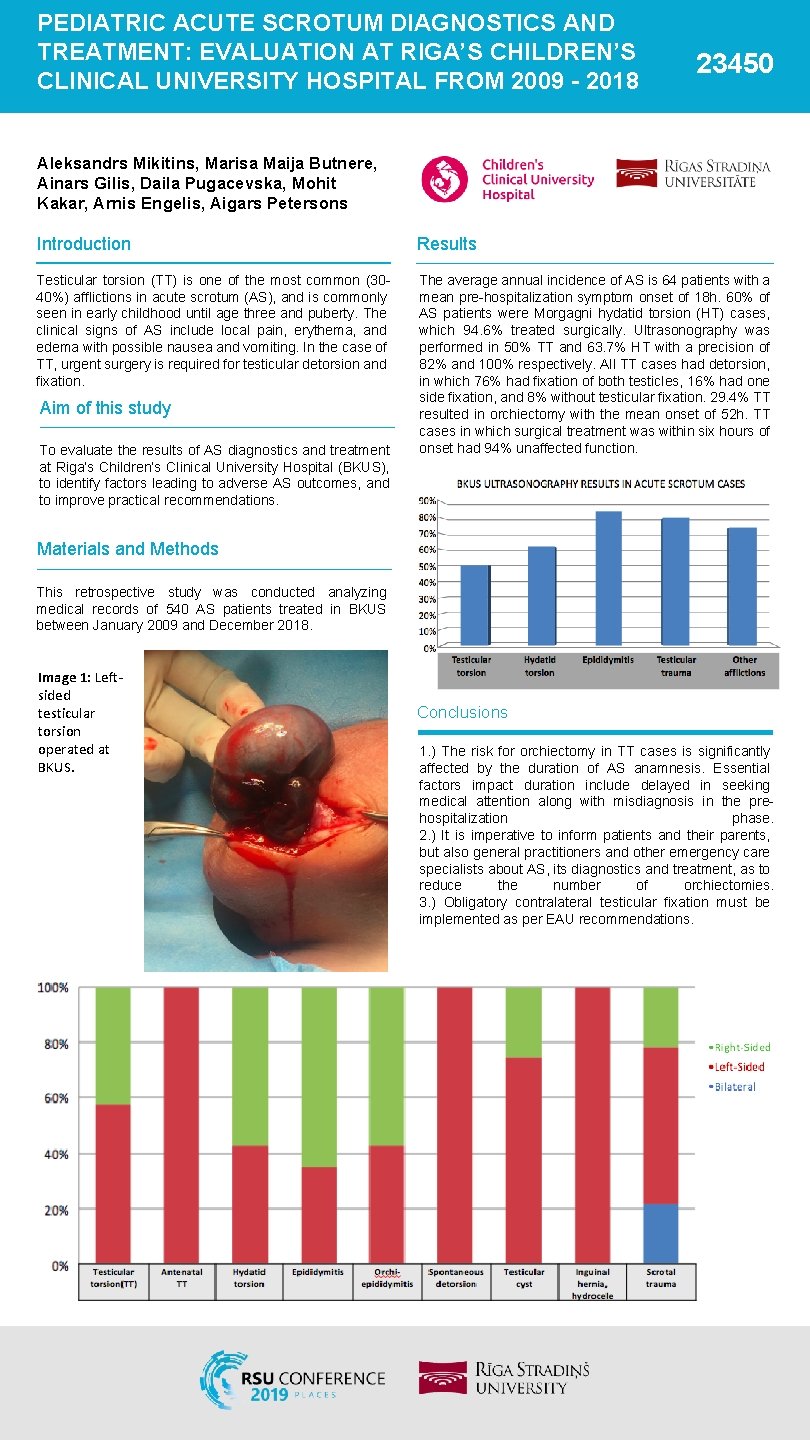
PEDIATRIC ACUTE SCROTUM DIAGNOSTICS AND TREATMENT: EVALUATION AT RIGA’S CHILDREN’S CLINICAL UNIVERSITY HOSPITAL FROM 2009 - 2018 23450 Aleksandrs Mikitins, Marisa Maija Butnere, Ainars Gilis, Daila Pugacevska, Mohit Kakar, Arnis Engelis, Aigars Petersons Introduction Results Testicular torsion (TT) is one of the most common (3040%) afflictions in acute scrotum (AS), and is commonly seen in early childhood until age three and puberty. The clinical signs of AS include local pain, erythema, and edema with possible nausea and vomiting. In the case of TT, urgent surgery is required for testicular detorsion and fixation. The average annual incidence of AS is 64 patients with a mean pre-hospitalization symptom onset of 18 h. 60% of AS patients were Morgagni hydatid torsion (HT) cases, which 94. 6% treated surgically. Ultrasonography was performed in 50% TT and 63. 7% HT with a precision of 82% and 100% respectively. All TT cases had detorsion, in which 76% had fixation of both testicles, 16% had one side fixation, and 8% without testicular fixation. 29. 4% TT resulted in orchiectomy with the mean onset of 52 h. TT cases in which surgical treatment was within six hours of onset had 94% unaffected function. Aim of this study To evaluate the results of AS diagnostics and treatment at Riga’s Children’s Clinical University Hospital (BKUS), to identify factors leading to adverse AS outcomes, and to improve practical recommendations. Materials and Methods This retrospective study was conducted analyzing medical records of 540 AS patients treated in BKUS between January 2009 and December 2018. Image 1: Leftsided testicular torsion operated at BKUS. Conclusions 1. ) The risk for orchiectomy in TT cases is significantly affected by the duration of AS anamnesis. Essential factors impact duration include delayed in seeking medical attention along with misdiagnosis in the prehospitalization phase. 2. ) It is imperative to inform patients and their parents, but also general practitioners and other emergency care specialists about AS, its diagnostics and treatment, as to reduce the number of orchiectomies. 3. ) Obligatory contralateral testicular fixation must be implemented as per EAU recommendations.