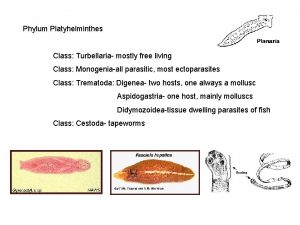
PARASITIC PLATYHELMINTHES FLAT WORMS Phylum Platyhelminthes flatworms characteristics


- Slides: 24

PARASITIC PLATYHELMINTHES “FLAT WORMS”
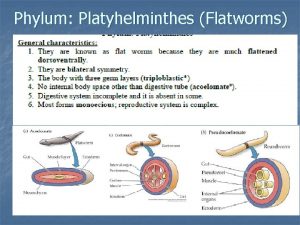
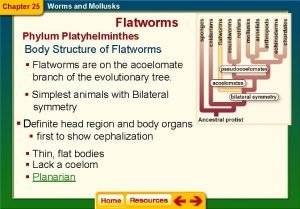
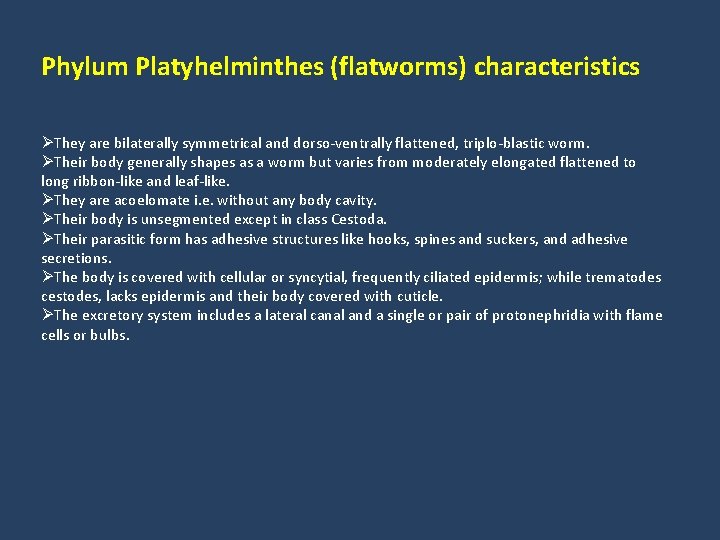
Phylum Platyhelminthes (flatworms) characteristics ØThey are bilaterally symmetrical and dorso-ventrally flattened, triplo-blastic worm. ØTheir body generally shapes as a worm but varies from moderately elongated flattened to long ribbon-like and leaf-like. ØThey are acoelomate i. e. without any body cavity. ØTheir body is unsegmented except in class Cestoda. ØTheir parasitic form has adhesive structures like hooks, spines and suckers, and adhesive secretions. ØThe body is covered with cellular or syncytial, frequently ciliated epidermis; while trematodes cestodes, lacks epidermis and their body covered with cuticle. ØThe excretory system includes a lateral canal and a single or pair of protonephridia with flame cells or bulbs.
The Pork Tape worm
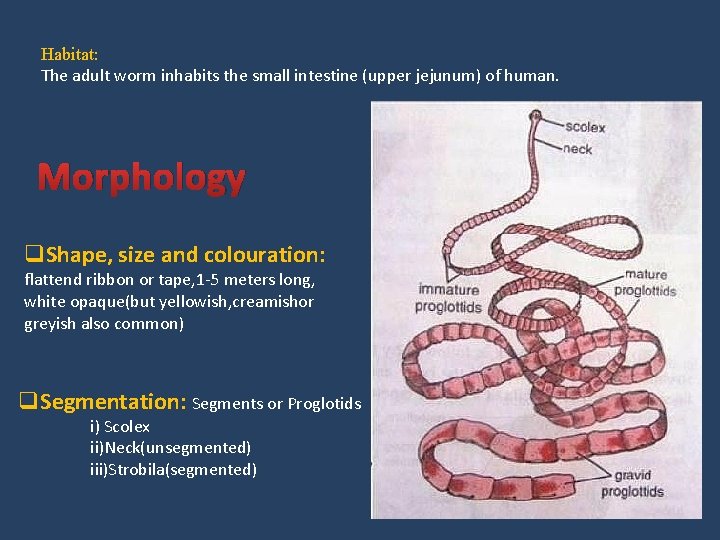
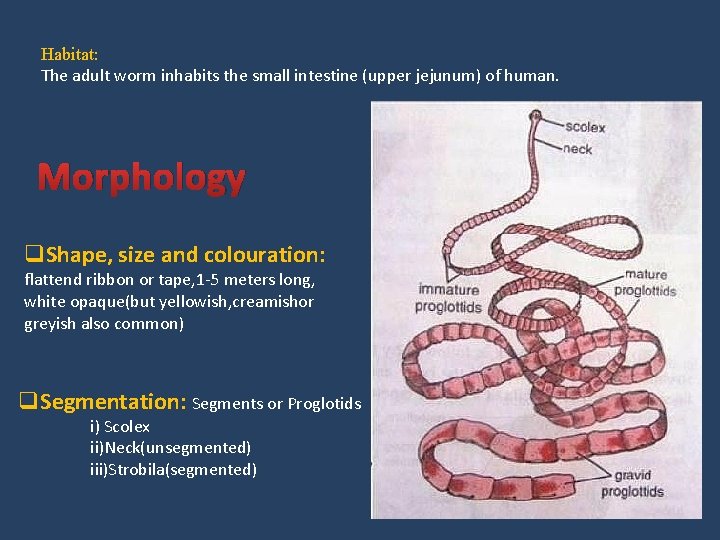
Habitat: The adult worm inhabits the small intestine (upper jejunum) of human. Morphology q. Shape, size and colouration: flattend ribbon or tape, 1 -5 meters long, white opaque(but yellowish, creamishor greyish also common) q. Segmentation: Segments or Proglotids i) Scolex ii)Neck(unsegmented) iii)Strobila(segmented)
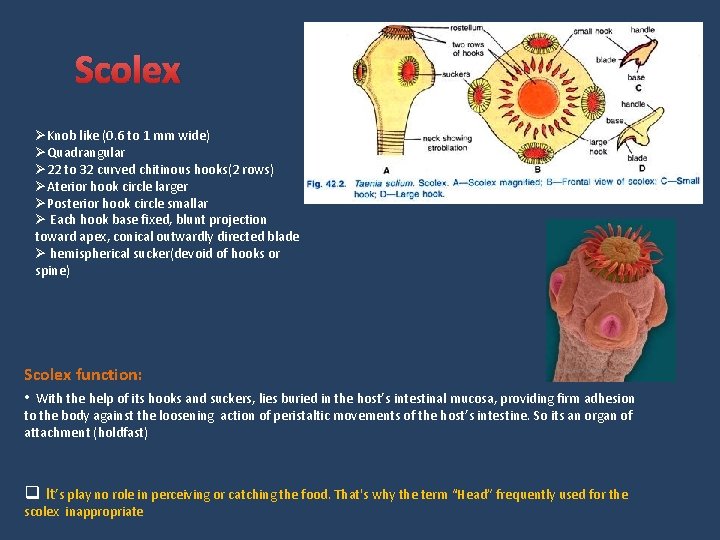
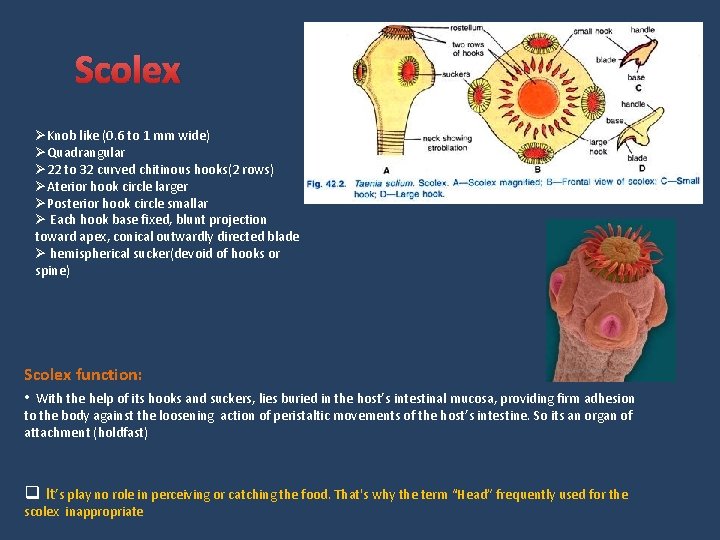
Scolex ØKnob like (0. 6 to 1 mm wide) ØQuadrangular Ø 22 to 32 curved chitinous hooks(2 rows) ØAterior hook circle larger ØPosterior hook circle smallar Ø Each hook base fixed, blunt projection toward apex, conical outwardly directed blade Ø hemispherical sucker(devoid of hooks or spine) Scolex function: • With the help of its hooks and suckers, lies buried in the host’s intestinal mucosa, providing firm adhesion to the body against the loosening action of peristaltic movements of the host’s intestine. So its an organ of attachment (holdfast) q It’s play no role in perceiving or catching the food. That's why the term “Head” frequently used for the scolex inappropriate
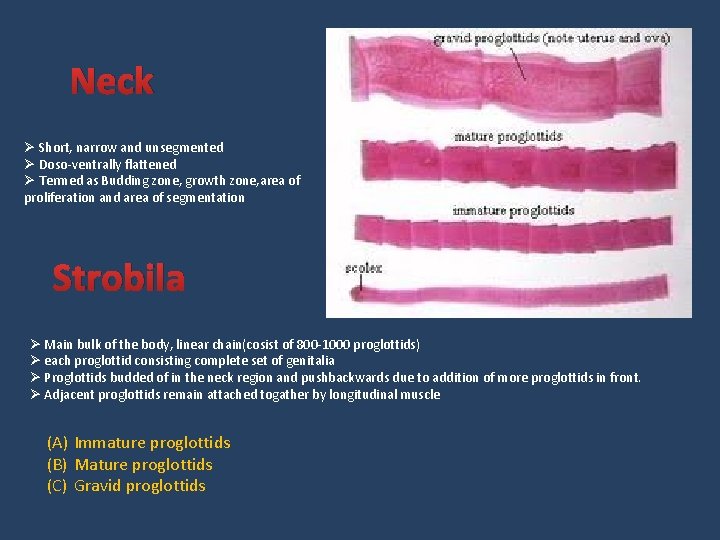
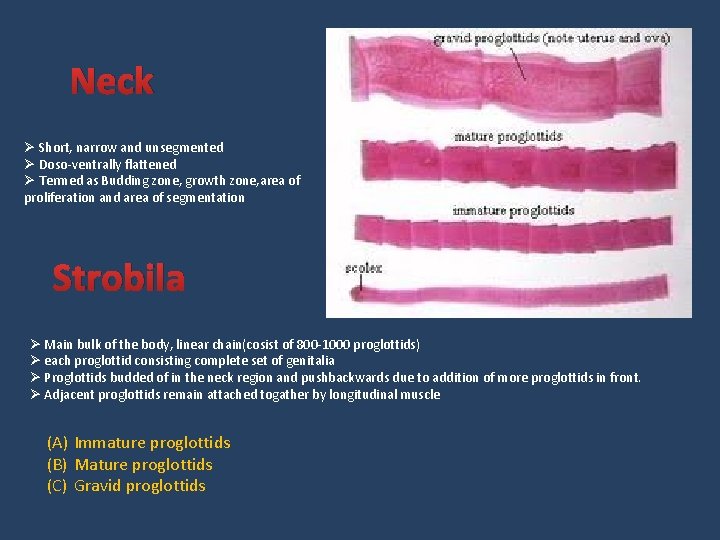
Neck Ø Short, narrow and unsegmented Ø Doso-ventrally flattened Ø Termed as Budding zone, growth zone, area of proliferation and area of segmentation Strobila Ø Main bulk of the body, linear chain(cosist of 800 -1000 proglottids) Ø each proglottid consisting complete set of genitalia Ø Proglottids budded of in the neck region and pushbackwards due to addition of more proglottids in front. Ø Adjacent proglottids remain attached togather by longitudinal muscle (A) Immature proglottids (B) Mature proglottids (C) Gravid proglottids
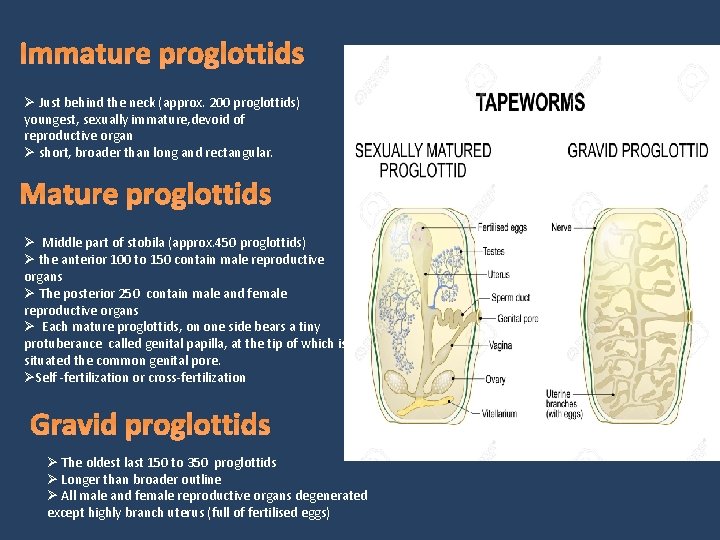
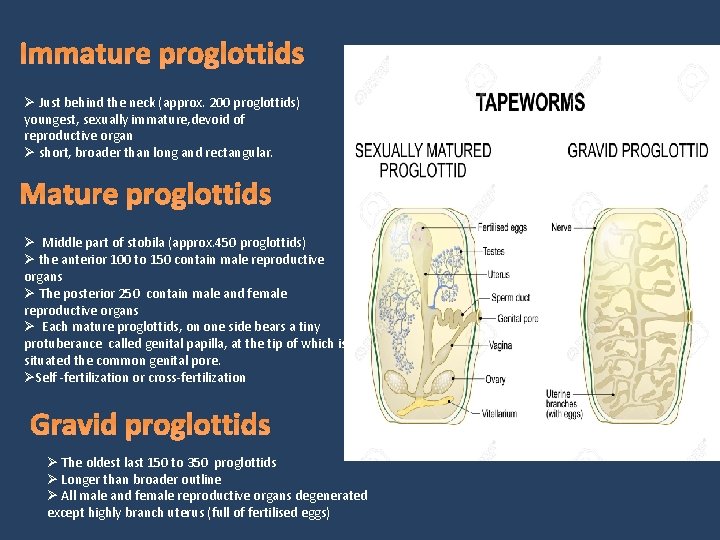
Immature proglottids Ø Just behind the neck (approx. 200 proglottids) youngest, sexually immature, devoid of reproductive organ Ø short, broader than long and rectangular. Mature proglottids Ø Middle part of stobila (approx. 450 proglottids) Ø the anterior 100 to 150 contain male reproductive organs Ø The posterior 250 contain male and female reproductive organs Ø Each mature proglottids, on one side bears a tiny protuberance called genital papilla, at the tip of which is situated the common genital pore. ØSelf -fertilization or cross-fertilization Gravid proglottids Ø The oldest last 150 to 350 proglottids Ø Longer than broader outline Ø All male and female reproductive organs degenerated except highly branch uterus (full of fertilised eggs)
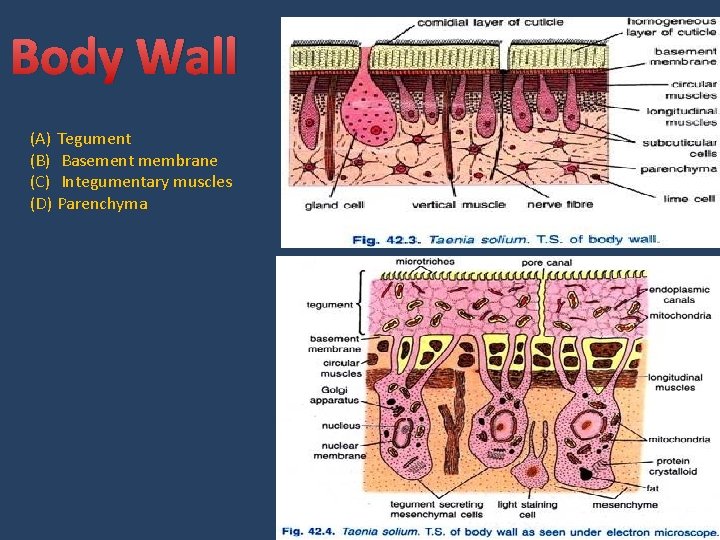
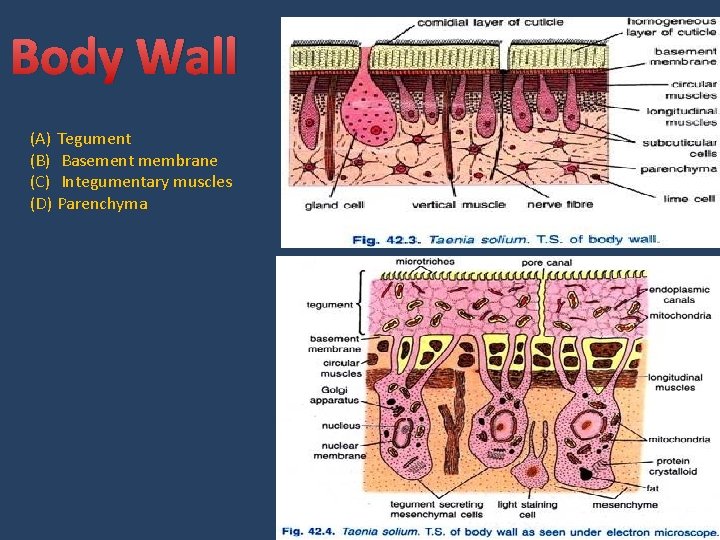
Body Wall (A) Tegument (B) Basement membrane (C) Integumentary muscles (D) Parenchyma
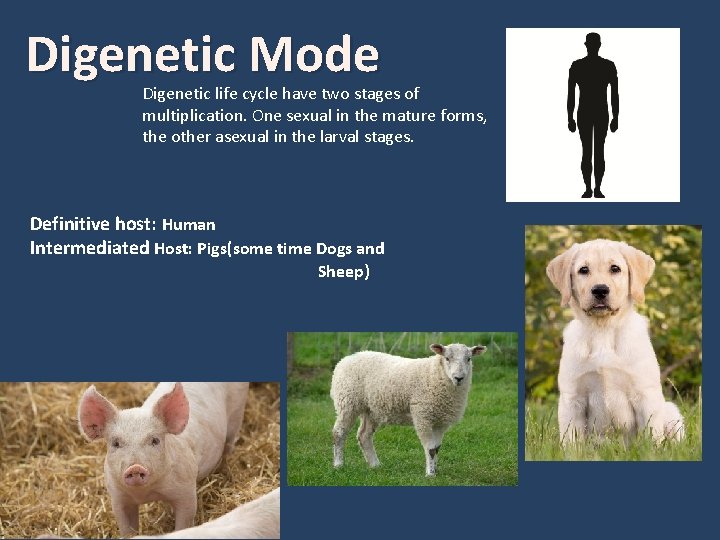
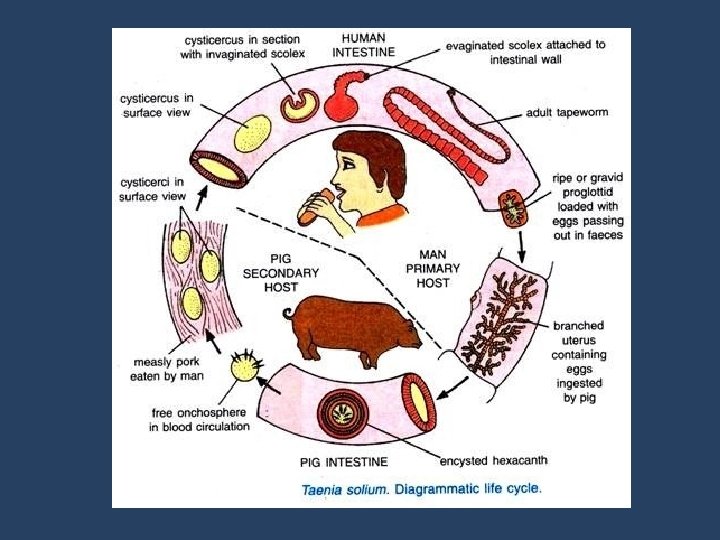
Digenetic Mode Digenetic life cycle have two stages of multiplication. One sexual in the mature forms, the other asexual in the larval stages. Definitive host: Human Intermediated Host: Pigs(some time Dogs and Sheep)
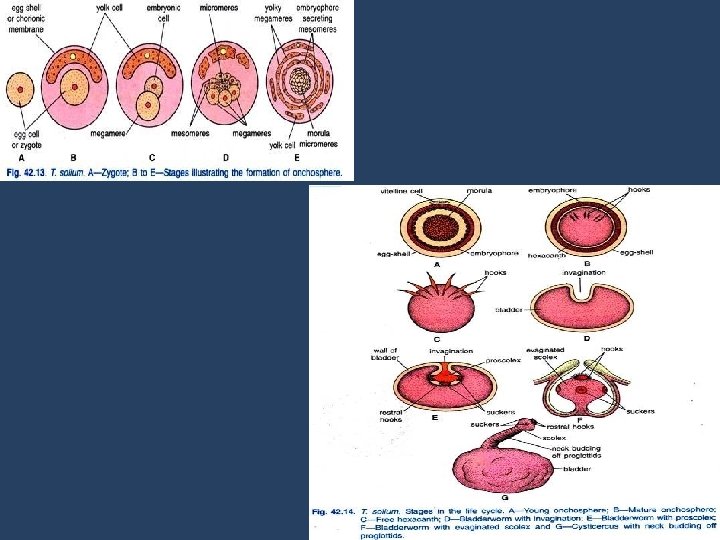
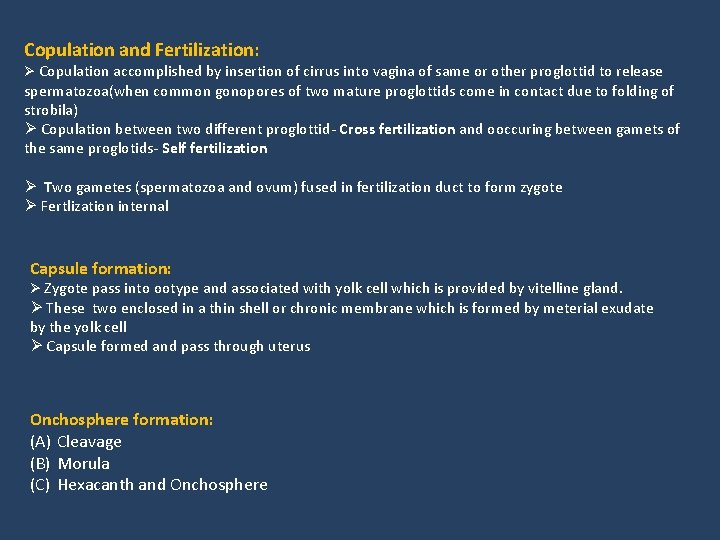
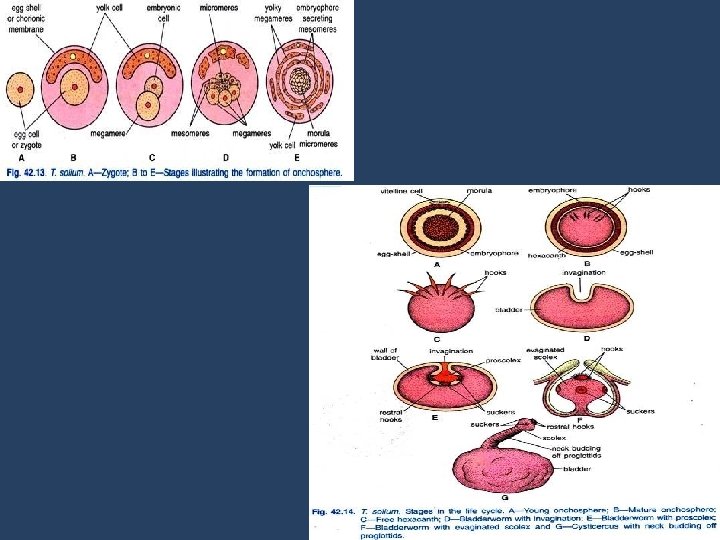
Copulation and Fertilization: Ø Copulation accomplished by insertion of cirrus into vagina of same or other proglottid to release spermatozoa(when common gonopores of two mature proglottids come in contact due to folding of strobila) Ø Copulation between two different proglottid- Cross fertilization and ooccuring between gamets of the same proglotids- Self fertilization Ø Two gametes (spermatozoa and ovum) fused in fertilization duct to form zygote Ø Fertlization internal Capsule formation: Ø Zygote pass into ootype and associated with yolk cell which is provided by vitelline gland. Ø These two enclosed in a thin shell or chronic membrane which is formed by meterial exudate by the yolk cell Ø Capsule formed and pass through uterus Onchosphere formation: (A) Cleavage (B) Morula (C) Hexacanth and Onchosphere
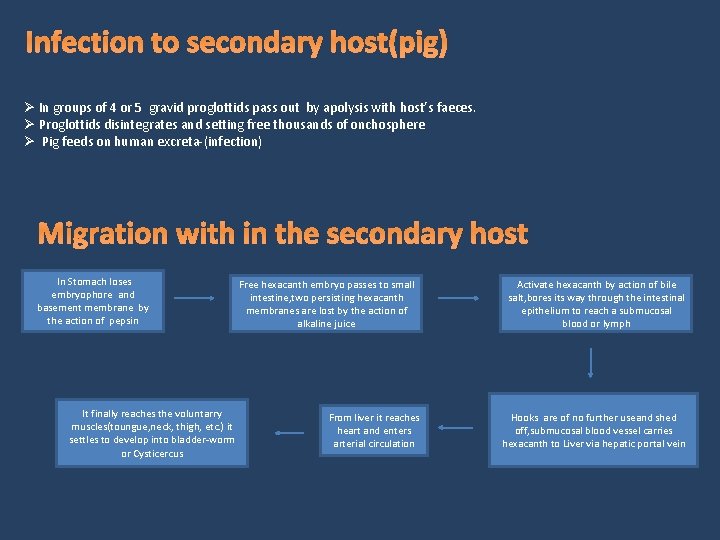
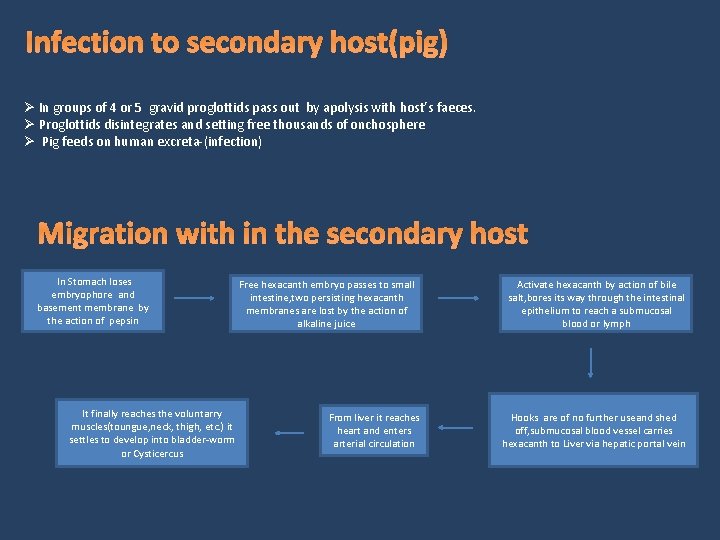
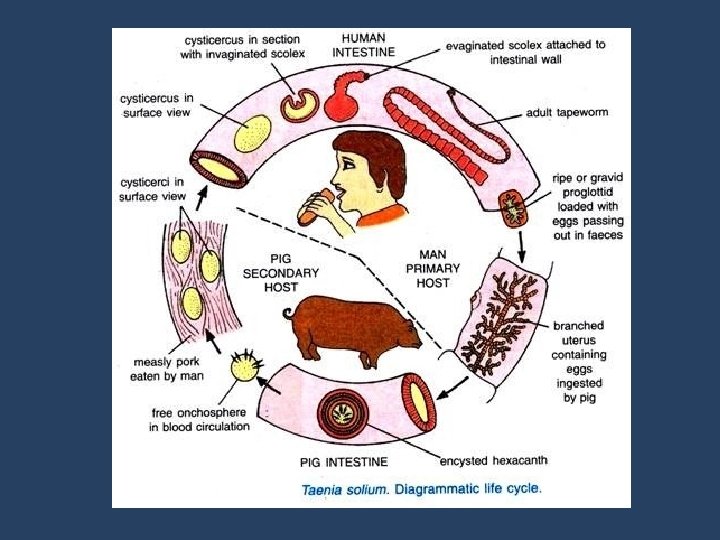
Infection to secondary host(pig) Ø In groups of 4 or 5 gravid proglottids pass out by apolysis with host’s faeces. Ø Proglottids disintegrates and setting free thousands of onchosphere Ø Pig feeds on human excreta-(infection) Migration with in the secondary host In Stomach loses embryophore and basement membrane by the action of pepsin It finally reaches the voluntarry muscles(toungue, neck, thigh, etc. ) it settles to develop into bladder-worm or Cysticercus Free hexacanth embryo passes to small intestine, two persisting hexacanth membranes are lost by the action of alkaline juice From liver it reaches heart and enters arterial circulation Activate hexacanth by action of bile salt, bores its way through the intestinal epithelium to reach a submucosal blood or lymph Hooks are of no further useand shed off, submucosal blood vessel carries hexacanth to Liver via hepatic portal vein
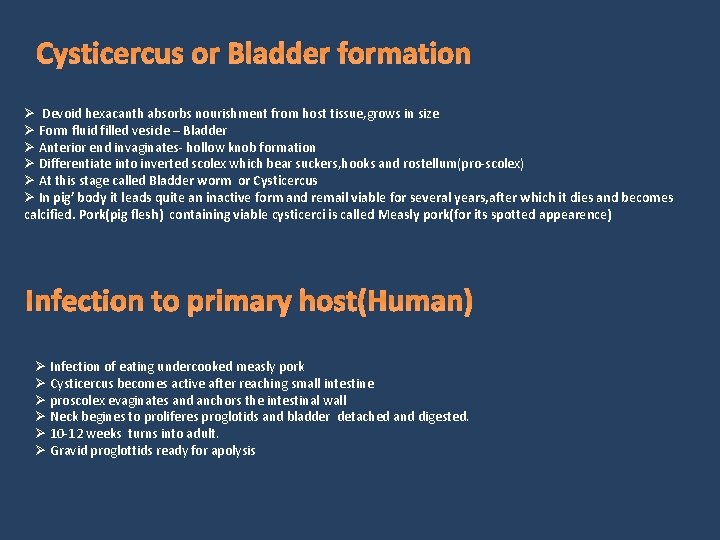
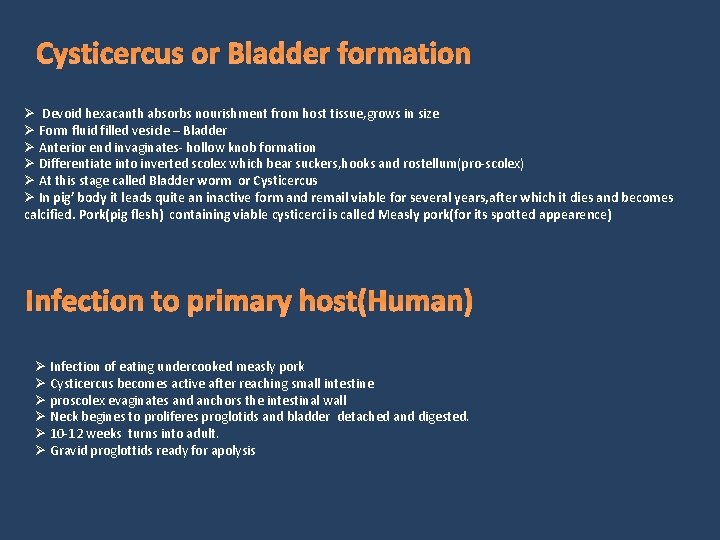
Cysticercus or Bladder formation Ø Devoid hexacanth absorbs nourishment from host tissue, grows in size Ø Form fluid filled vesicle – Bladder Ø Anterior end invaginates- hollow knob formation Ø Differentiate into inverted scolex which bear suckers, hooks and rostellum(pro-scolex) Ø At this stage called Bladder worm or Cysticercus Ø In pig’ body it leads quite an inactive form and remail viable for several years, after which it dies and becomes calcified. Pork(pig flesh) containing viable cysticerci is called Measly pork(for its spotted appearence) Infection to primary host(Human) Ø Infection of eating undercooked measly pork Ø Cysticercus becomes active after reaching small intestine Ø proscolex evaginates and anchors the intestinal wall Ø Neck begines to proliferes proglotids and bladder detached and digested. Ø 10 -12 weeks turns into adult. Ø Gravid proglottids ready for apolysis
Mode of Transmission ØIngestion of uncooked pork infected with tape worm ØIngestion of food and water contaminated by the eggs present in the infective faeces of a Taenia carrier. ØEndogenous auto infection: Anus-hand-mouth transfer of eggs by contaminated hands of person with poor personal hygiene. ØAutoinfection: Reverse peristalsis in which eggs produced by T. solium are thrown back to the duodenum, where they hatch and cause tissue infection
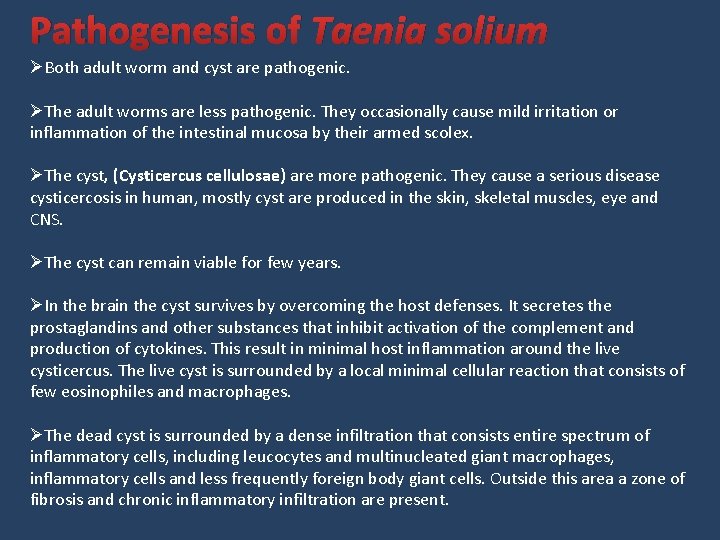
Pathogenesis of Taenia solium ØBoth adult worm and cyst are pathogenic. ØThe adult worms are less pathogenic. They occasionally cause mild irritation or inflammation of the intestinal mucosa by their armed scolex. ØThe cyst, (Cysticercus cellulosae) are more pathogenic. They cause a serious disease cysticercosis in human, mostly cyst are produced in the skin, skeletal muscles, eye and CNS. ØThe cyst can remain viable for few years. ØIn the brain the cyst survives by overcoming the host defenses. It secretes the prostaglandins and other substances that inhibit activation of the complement and production of cytokines. This result in minimal host inflammation around the live cysticercus. The live cyst is surrounded by a local minimal cellular reaction that consists of few eosinophiles and macrophages. ØThe dead cyst is surrounded by a dense infiltration that consists entire spectrum of inflammatory cells, including leucocytes and multinucleated giant macrophages, inflammatory cells and less frequently foreign body giant cells. Outside this area a zone of fibrosis and chronic inflammatory infiltration are present.
Clinical Diseases 1. Intestinal Taeniasis: ØMostly the infection is asymptomatic. ØIn symptomatic cases, the clinical symptoms are nonspecific and mild and includes- nausea, abdominal discomfort, hunger pain, loss of weight, chronic indigestion etc. ØLess frequently nausea, vomiting, headache and diarrhea are present in few cases. 2. Cysticercosis: ØCysticercosis is the infection with the larval stage of the parasite. ØHuman beings acquire infection through fecal oral contamination with T. solium eggs from tapeworm carriers or by auto infection. ØClinical manifestation depend on the affected organ; neurocysticercosis and ophthalmic cysticercosis are associated with substantial morbidity. (A) Extraneural cysticercosis: ØSubcutaneous cysticercosis present as small, movable, painless nodules that are commonly noticed in the arms or chest. ØAfter a few months or even years, the nodules become swollen, tender and inflamed and then they gradually disappears. ØMuscular cysticercosis is a causal finding, appearing as dot shaped or ellipsoidal calcifications. ØIn rare cases, very massive parasite burdens enlarge the patient’s limbs (muscular pseudohypertrophy). ØThe heart is another occasional location, infected in about 5% of patient’s cardiac cysticercosis is asymptomatic.
(B) Ophthalmic cysticercosis: ØThis condition is present in 20% of cases. ØMost cysts are found in the vitreous, subretinal space and conjunctiva. ØThe condition may present as iritis, and conjunctivitis. ØThe cyst in subconjunctival or subretinal sites may present as slowly growing nodules confusing with tumors. ØOccasionally, subretinal eye cyst may lead to blindness due to detachment of retina. (C) Neurocysticercosis: ØThe parasite commonly infects the CNS, causing neurocysticercosis as a clinical disorder. ØAfter entering the CNS, cysticerci are visible and elicit few inflammatory changes in the surrounding tissue. ØCysticerci cause symptoms because of mass effect or by blocking the circulation of cerebrospinal fluid, most symptoms are the direct result of the inflammatory process that accompanies cyst degeneration. ØSymptoms and signs are varied and nonspecific. ØEpileptic seizures are the commonest presentation and generally represent the primary or sole manifestation of the disease. ØSeizures occur in 50 -80% of cases with parenchyma brain cysts or calcifications. ØThe disease also present with intracranial hypertension, hydrocephalus or both in 20 -30% of cases. ØThe syndrome is related to the location of parasites in the cerebral ventricles or basal cisterns blocking circulation of CSF and is caused by several different mechanisms- the presence of the parasite itself, ependymal inflammation or residual fibrosis. ØOccasionally a cyst grows larger than the usual and acts in the same way as a tumor mass (giant cyst). ØThese giant cysts compress adjacent cerebral structures, causing localized deficits and intracranial hypertension. Motor deficits can also arise because of oedema secondary to cyst degeneration or as a result of stroke complicating the infection. ØIn children and teenagers, an acute encephalitic presentation can happen, more likely in female than male. Massive non encephalitic forms also occur. ØCompromise of the spine occurs in adult 1% cases, presenting with compressive manifestation.
Diagnosis Specimen: Faeces, muscle tissue, blood, CSF 1. Macroscopic examination: ØA naked examination of the specimen can be made for segment or proglottids. ØThe whitish segment can easily be recognized against the dark yellow mass of the faeces. 2. Stool Microscopy: Demonstration of eggs and less frequently proglottids and scolex in faeces is used as tool for diagnosis. Eggs: ØEggs are demonstrated by a thick faecal smear examination. ØThe eggs shed irregularly, so 2 -3 stool sample should be collected. ØEggs can be seen in perianal area and can be detected by cellophane swab. ØSince eggs of T. soluim and T. saginata are similar, species diagnosis can be made by Acid-fast staining. Eggs of T. soluim are non-acid fast whereas T. saginata is acid fast. Proglottids: The gravid proglottids are found in faeces or recovered from the under clothings. They are washed in clean water and placed between two sides. The sides are held by adhesive tape at each end are examined by hand less for lateral branches. Observation: Taenia soluim: 7 -12 lateral branches on each side of utetine stem Scolex: T. soluim – bears a row of hooks
3. Antigen detection: ØThis is a very useful for screening the cases of intestinal taeniasis. ØAntigens capture ELISA polyclonal antisera raised against Taenia is employed to detect antigen in faeces. Ø 4. Serodiagnosis: ØDetection of antigens in serum or CSF indicates recent or viable infection. 5. Histopathological diagnosis ØDiagnosis of Neurocycticercosis (NCC) is made by demonstrating cysticerci in the biopsy tissue obtained from brain during post mortem. ØSkeletal cysticercosis can be diagnosed by histological examination of biopsy. 6. Imaging method: ØX-ray of the soft tissue in arm and thigh, chest and neck may show dead, calcified or elongated cysts. ØX-ray of the skull may reveal cerebral calcification and intracranial lesions in the neurocysticercosis. ØCT scan is best method for detecting dead, calcified and multiple cysts is pathognomonic of neurocysticercosis. ØMRI shows a mural nodule within the cyst which is pathognomonic for NCC.

Treatment i. Praziquantel– drug of choice. ØDose- oral. Ø 50 mg/kg body weight Ø 3 divided doses for 15 days. ii. Niclosamide: ØDose of 2 g for and Adult ØMinor side effects iii. Albendazole: ØA dose of 400 mg twice daily for 30 days. iv. Surgery: ØFor cysticercosis of ocular, ventricular and spinal cord.
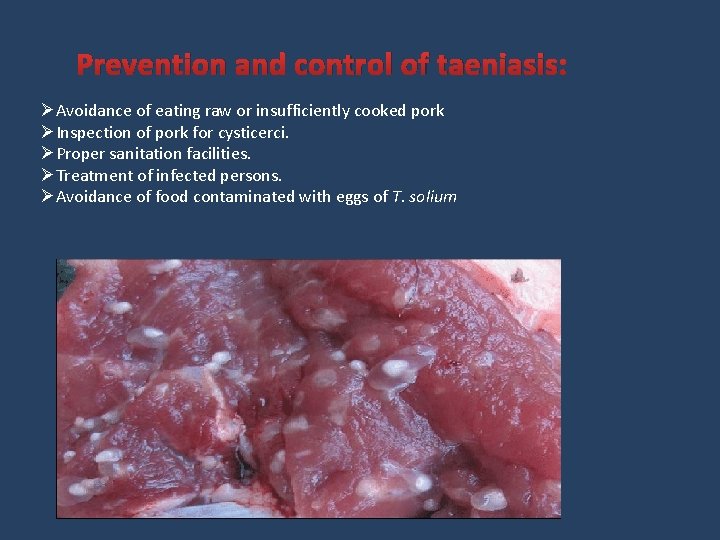
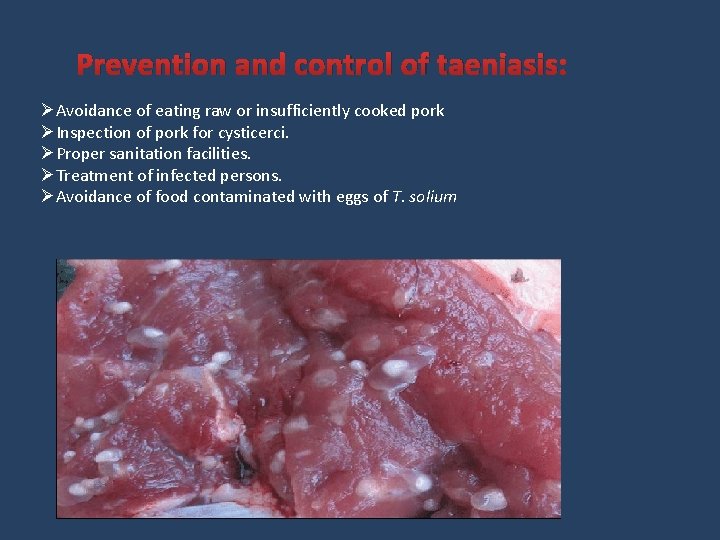
Prevention and control of taeniasis: ØAvoidance of eating raw or insufficiently cooked pork ØInspection of pork for cysticerci. ØProper sanitation facilities. ØTreatment of infected persons. ØAvoidance of food contaminated with eggs of T. solium
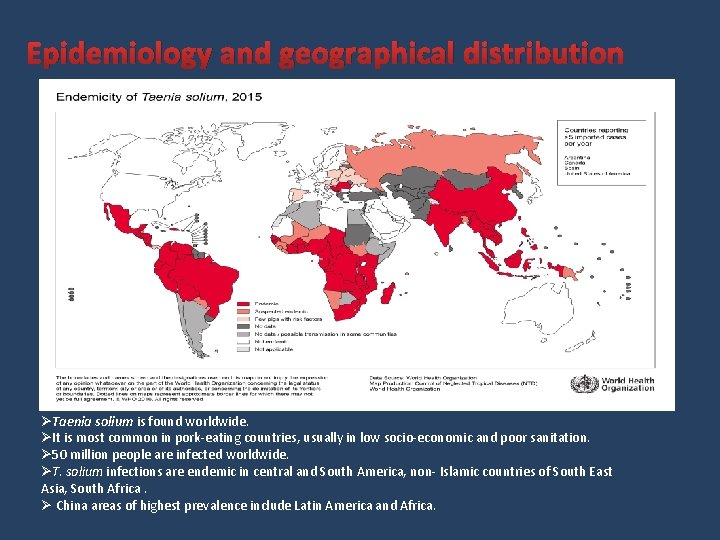
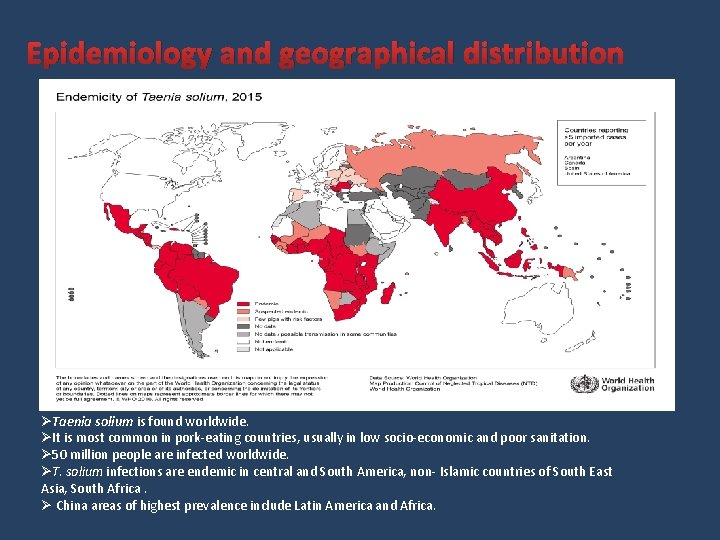
Epidemiology and geographical distribution ØTaenia solium is found worldwide. ØIt is most common in pork-eating countries, usually in low socio-economic and poor sanitation. Ø 50 million people are infected worldwide. ØT. solium infections are endemic in central and South America, non- Islamic countries of South East Asia, South Africa. Ø China areas of highest prevalence include Latin America and Africa.
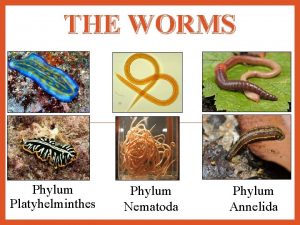
 Flatworms roundworms and segmented worms
Flatworms roundworms and segmented worms Are worms mollusks
Are worms mollusks Characteristics of platyhelminthes
Characteristics of platyhelminthes Triploblastik aselomata
Triploblastik aselomata Eumetazoa phylum
Eumetazoa phylum Phylum platyhelminthes characteristics
Phylum platyhelminthes characteristics Phylum platyhelminthes characteristics
Phylum platyhelminthes characteristics Platyhelminthes- characteristics
Platyhelminthes- characteristics Triploblastica
Triploblastica Flatworms examples
Flatworms examples Platyhelminthes examples
Platyhelminthes examples Unsegmented phylum
Unsegmented phylum Characteristics of segmented worms
Characteristics of segmented worms Segmented worms features
Segmented worms features Cestodes
Cestodes Flatworm bilateral symmetry
Flatworm bilateral symmetry Plat ee
Plat ee Platyhelminthes
Platyhelminthes Invertebrate phylogeny
Invertebrate phylogeny Raccoon symbiotic relationships
Raccoon symbiotic relationships Parasitic arthropods
Parasitic arthropods Faciola
Faciola Parasitic cone
Parasitic cone Parasitic cone
Parasitic cone Parasitic computing
Parasitic computing