Monitoring Delirium in the Hospitalized Elderly Sonia Sandhaus
- Slides: 1
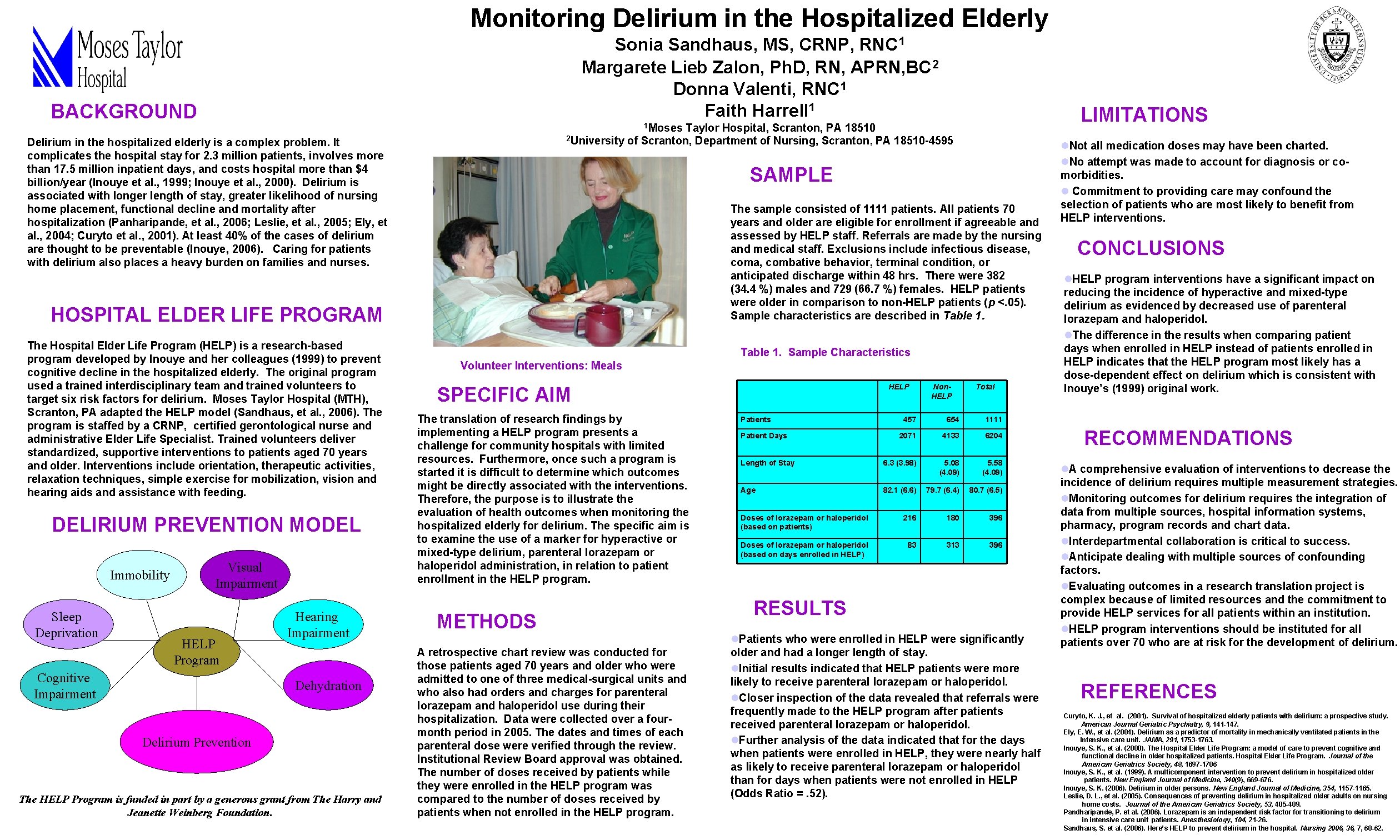
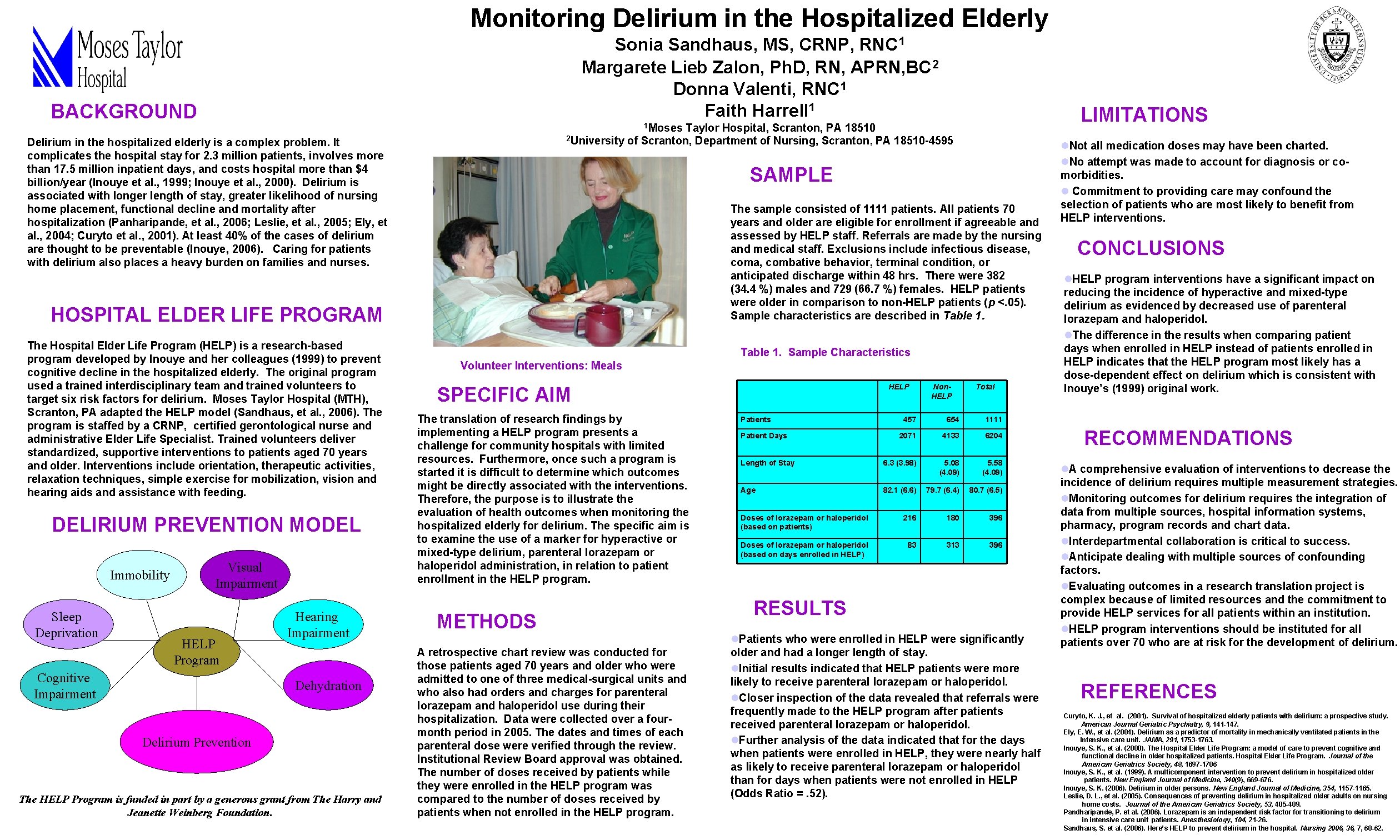
Monitoring Delirium in the Hospitalized Elderly Sonia Sandhaus, MS, CRNP, RNC 1 Margarete Lieb Zalon, Ph. D, RN, APRN, BC 2 Donna Valenti, RNC 1 Faith Harrell 1 BACKGROUND 2 University of Scranton, Department of Nursing, Scranton, Delirium in the hospitalized elderly is a complex problem. It complicates the hospital stay for 2. 3 million patients, involves more than 17. 5 million inpatient days, and costs hospital more than $4 billion/year (Inouye et al. , 1999; Inouye et al. , 2000). Delirium is associated with longer length of stay, greater likelihood of nursing home placement, functional decline and mortality after hospitalization (Panharipande, et al. , 2006; Leslie, et al. , 2005; Ely, et al. , 2004; Curyto et al. , 2001). At least 40% of the cases of delirium are thought to be preventable (Inouye, 2006). Caring for patients with delirium also places a heavy burden on families and nurses. The Hospital Elder Life Program (HELP) is a research-based program developed by Inouye and her colleagues (1999) to prevent cognitive decline in the hospitalized elderly. The original program used a trained interdisciplinary team and trained volunteers to target six risk factors for delirium. Moses Taylor Hospital (MTH), Scranton, PA adapted the HELP model (Sandhaus, et al. , 2006). The program is staffed by a CRNP, certified gerontological nurse and administrative Elder Life Specialist. Trained volunteers deliver standardized, supportive interventions to patients aged 70 years and older. Interventions include orientation, therapeutic activities, relaxation techniques, simple exercise for mobilization, vision and hearing aids and assistance with feeding. DELIRIUM PREVENTION MODEL Sleep Deprivation Visual Impairment HELP Program Cognitive Impairment Hearing Impairment Dehydration Delirium Prevention The HELP Program is funded in part by a generous grant from The Harry and Jeanette Weinberg Foundation. PA 18510 -4595 SAMPLE The sample consisted of 1111 patients. All patients 70 years and older are eligible for enrollment if agreeable and assessed by HELP staff. Referrals are made by the nursing and medical staff. Exclusions include infectious disease, coma, combative behavior, terminal condition, or anticipated discharge within 48 hrs. There were 382 (34. 4 %) males and 729 (66. 7 %) females. HELP patients were older in comparison to non-HELP patients (p <. 05). Sample characteristics are described in Table 1. HOSPITAL ELDER LIFE PROGRAM Immobility LIMITATIONS 1 Moses Taylor Hospital, Scranton, PA 18510 Table 1. Sample Characteristics Volunteer Interventions: Meals SPECIFIC AIM The translation of research findings by implementing a HELP program presents a challenge for community hospitals with limited resources. Furthermore, once such a program is started it is difficult to determine which outcomes might be directly associated with the interventions. Therefore, the purpose is to illustrate the evaluation of health outcomes when monitoring the hospitalized elderly for delirium. The specific aim is to examine the use of a marker for hyperactive or mixed-type delirium, parenteral lorazepam or haloperidol administration, in relation to patient enrollment in the HELP program. METHODS A retrospective chart review was conducted for those patients aged 70 years and older who were admitted to one of three medical-surgical units and who also had orders and charges for parenteral lorazepam and haloperidol use during their hospitalization. Data were collected over a fourmonth period in 2005. The dates and times of each parenteral dose were verified through the review. Institutional Review Board approval was obtained. The number of doses received by patients while they were enrolled in the HELP program was compared to the number of doses received by patients when not enrolled in the HELP program. HELP Patients Non. HELP Total 457 654 1111 2071 4133 6204 Length of Stay 6. 3 (3. 98) 5. 08 (4. 09) 5. 58 (4. 09) Age 82. 1 (6. 6) 79. 7 (6. 4) 80. 7 (6. 5) Doses of lorazepam or haloperidol (based on patients) 216 180 396 Doses of lorazepam or haloperidol (based on days enrolled in HELP) 83 313 396 Patient Days RESULTS l. Patients who were enrolled in HELP were significantly older and had a longer length of stay. l. Initial results indicated that HELP patients were more likely to receive parenteral lorazepam or haloperidol. l. Closer inspection of the data revealed that referrals were frequently made to the HELP program after patients received parenteral lorazepam or haloperidol. l. Further analysis of the data indicated that for the days when patients were enrolled in HELP, they were nearly half as likely to receive parenteral lorazepam or haloperidol than for days when patients were not enrolled in HELP (Odds Ratio =. 52). l. Not all medication doses may have been charted. l. No attempt was made to account for diagnosis or comorbidities. l Commitment to providing care may confound the selection of patients who are most likely to benefit from HELP interventions. CONCLUSIONS l. HELP program interventions have a significant impact on reducing the incidence of hyperactive and mixed-type delirium as evidenced by decreased use of parenteral lorazepam and haloperidol. l. The difference in the results when comparing patient days when enrolled in HELP instead of patients enrolled in HELP indicates that the HELP program most likely has a dose-dependent effect on delirium which is consistent with Inouye’s (1999) original work. RECOMMENDATIONS l. A comprehensive evaluation of interventions to decrease the incidence of delirium requires multiple measurement strategies. l. Monitoring outcomes for delirium requires the integration of data from multiple sources, hospital information systems, pharmacy, program records and chart data. l. Interdepartmental collaboration is critical to success. l. Anticipate dealing with multiple sources of confounding factors. l. Evaluating outcomes in a research translation project is complex because of limited resources and the commitment to provide HELP services for all patients within an institution. l. HELP program interventions should be instituted for all patients over 70 who are at risk for the development of delirium. REFERENCES Curyto, K. J. , et al. (2001). Survival of hospitalized elderly patients with delirium: a prospective study. American Journal Geriatric Psychiatry, 9, 141 -147. Ely, E. W. , et al. (2004). Delirium as a predictor of mortality in mechanically ventilated patients in the Intensive care unit. JAMA, 291, 1753 -1763. Inouye, S. K. , et al. (2000). The Hospital Elder Life Program: a model of care to prevent cognitive and functional decline in older hospitalized patients. Hospital Elder Life Program. Journal of the American Geriatrics Society, 48, 1697 -1706 Inouye, S. K. , et al. (1999). A multicomponent intervention to prevent delirium in hospitalized older patients. New England Journal of Medicine, 340(9), 669 -676. Inouye, S. K. (2006). Delirium in older persons. New England Journal of Medicine, 354, 1157 -1165. Leslie, D. L. , et al. (2005). Consequences of preventing delirium in hospitalized older adults on nursing home costs. Journal of the American Geriatrics Society, 53, 405 -409. Pandharipande, P. et al. (2006). Lorazepam is an independent risk factor for transitioning to delirium in intensive care unit patients. Anesthesiology, 104, 21 -26. Sandhaus, S. et al. (2006). Here’s HELP to prevent delirium in the hospital. Nursing 2006, 36, 7, 60 -62.