Molly Collins MD Palliative Medicine Fellow Sudha Natarajan
- Slides: 1
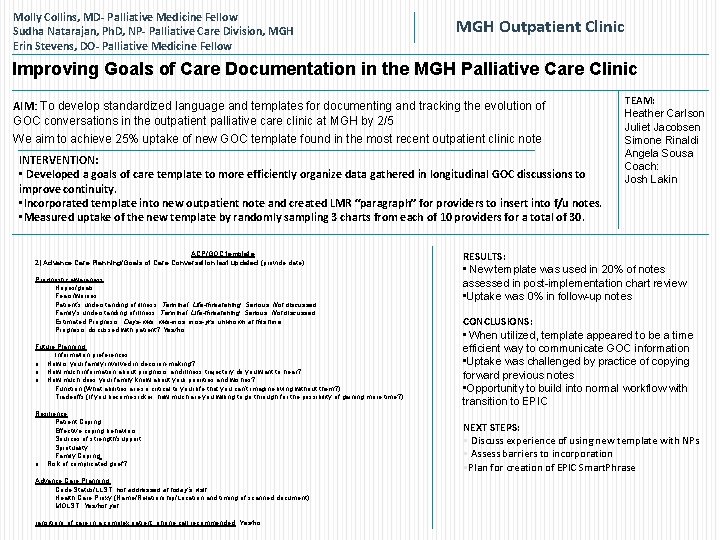
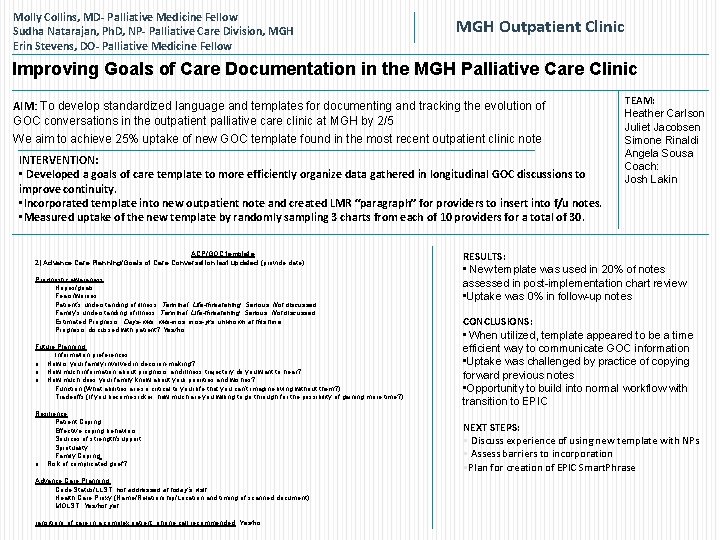
Molly Collins, MD- Palliative Medicine Fellow Sudha Natarajan, Ph. D, NP- Palliative Care Division, MGH Erin Stevens, DO- Palliative Medicine Fellow MGH Outpatient Clinic Improving Goals of Care Documentation in the MGH Palliative Care Clinic AIM: To develop standardized language and templates for documenting and tracking the evolution of GOC conversations in the outpatient palliative care clinic at MGH by 2/5 We aim to achieve 25% uptake of new GOC template found in the most recent outpatient clinic note INTERVENTION: • Developed a goals of care template to more efficiently organize data gathered in longitudinal GOC discussions to improve continuity. • Incorporated template into new outpatient note and created LMR “paragraph” for providers to insert into f/u notes. • Measured uptake of the new template by randomly sampling 3 charts from each of 10 providers for a total of 30. ACP/GOC template 2) Advance Care Planning/Goals of Care Conversation last updated (provide date): Prognostic awareness: · Hopes/goals: · Fears/worries: · Patient’s understanding of illness: Terminal, Life-threatening, Serious, Not discussed · Family’s understanding of illness: Terminal, Life-threatening, Serious, Not discussed · Estimated Prognosis: Days-wks, wks-mos, mos-yrs, unknown at this time · Prognosis discussed with patient? Yes/no Future Planning: · Information preferences: o How is your family involved in decision-making? o How much information about prognosis and illness trajectory do you want to hear? o How much does your family know about your priorities and wishes? · Function (What abilities are so critical to your life that you can’t imagine living without them? ): · Tradeoffs (If you become sicker, how much are you willing to go through for the possibility of gaining more time? ): Resilience: · Patient Coping: · Effective coping behaviors: · Sources of strength/support: · Spirituality: · Family Coping: o Risk of complicated grief? Advance Care Planning: · Code Status/LLST: not addressed at today’s visit · Health Care Proxy (Name/Relationship/Location and timing of scanned document): · MOLST: Yes/not yet ransitions of care in a complex patient, phone call recommended: Yes/no TEAM: Heather Carlson Juliet Jacobsen Simone Rinaldi Angela Sousa Coach: Josh Lakin RESULTS: • New template was used in 20% of notes assessed in post-implementation chart review • Uptake was 0% in follow-up notes CONCLUSIONS: • When utilized, template appeared to be a time efficient way to communicate GOC information • Uptake was challenged by practice of copying forward previous notes • Opportunity to build into normal workflow with transition to EPIC NEXT STEPS: § Discuss experience of using new template with NPs § Assess barriers to incorporation §Plan for creation of EPIC Smart. Phrase