Making treatment systems more recoveryoriented John Marsden National


![How well are we doing? [1] • Two-thirds treated before. • Stable recovery after How well are we doing? [1] • Two-thirds treated before. • Stable recovery after](https://slidetodoc.com/presentation_image/d8cdd9e5e5dcc94b62d613f26747e497/image-8.jpg)
![How well are we doing? [2] • Average treatment pathway ~10 months. • ~70% How well are we doing? [2] • Average treatment pathway ~10 months. • ~70%](https://slidetodoc.com/presentation_image/d8cdd9e5e5dcc94b62d613f26747e497/image-9.jpg)
- Slides: 13
Making treatment systems more recovery-oriented. John Marsden National Addiction Centre, London EMCDDA conference Lisbon 7 th May 2009

UK treatment at crossroads • “The new abstentionists”. • Lamenting possible decline of residential treatments • Unhelpful polarised debate. • New philosophy? • Abstinence or maintenance – divide. • Need for rationale balance. • Need for re-integration efforts.

The treatments Somatic treatments • Medications to treat intoxication states. • Medications to treat withdrawal states. • Agonist maintenance therapies. • Relapse prevention therapies. • Medications to treat coexisting psychiatric disorders Psychosocial treatments • Cognitive-behavioural therapies. • Motivational enhancement therapies. • Behavioural therapies. • Psychodynamic and interpersonal therapies. • Family and couples therapies. • Self-help organisations and 12 -step oriented
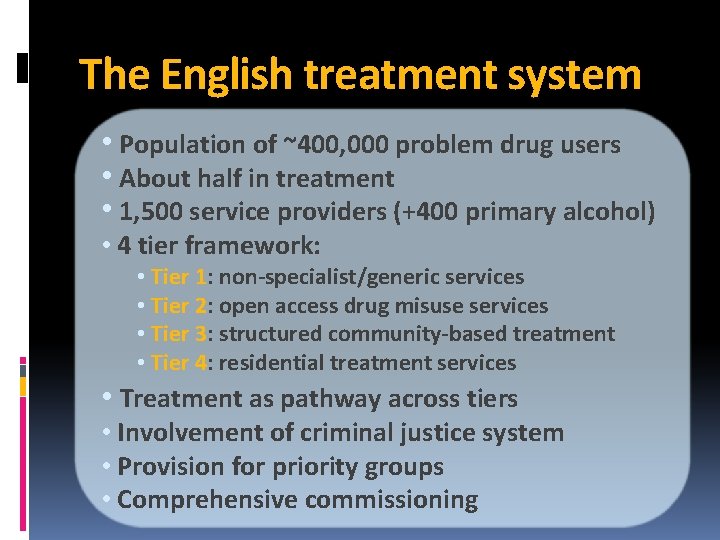
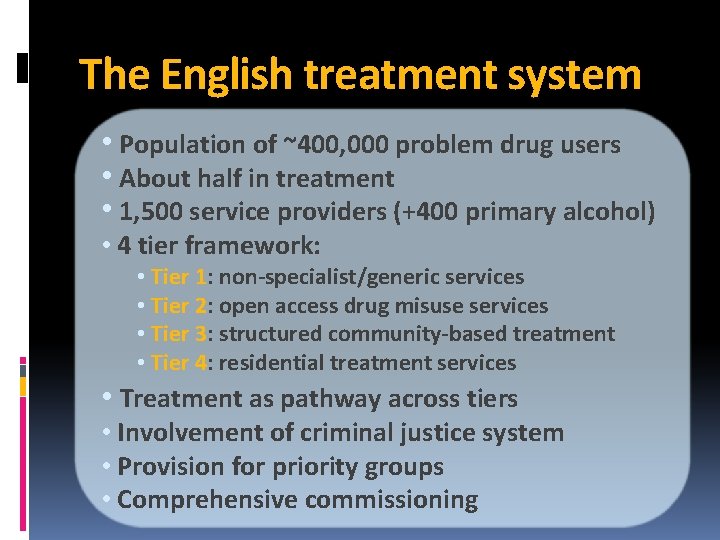
The English treatment system • Population of ~400, 000 problem drug users • About half in treatment • 1, 500 service providers (+400 primary alcohol) • 4 tier framework: • Tier 1: non-specialist/generic services • Tier 2: open access drug misuse services • Tier 3: structured community-based treatment • Tier 4: residential treatment services • Treatment as pathway across tiers • Involvement of criminal justice system • Provision for priority groups • Comprehensive commissioning
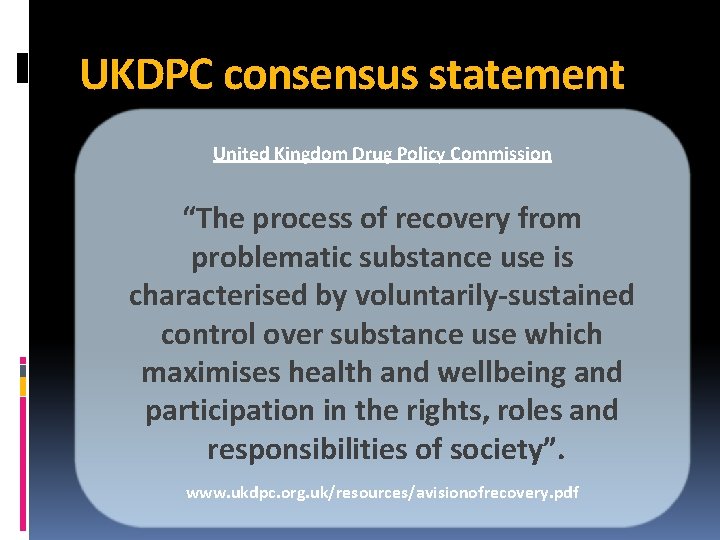
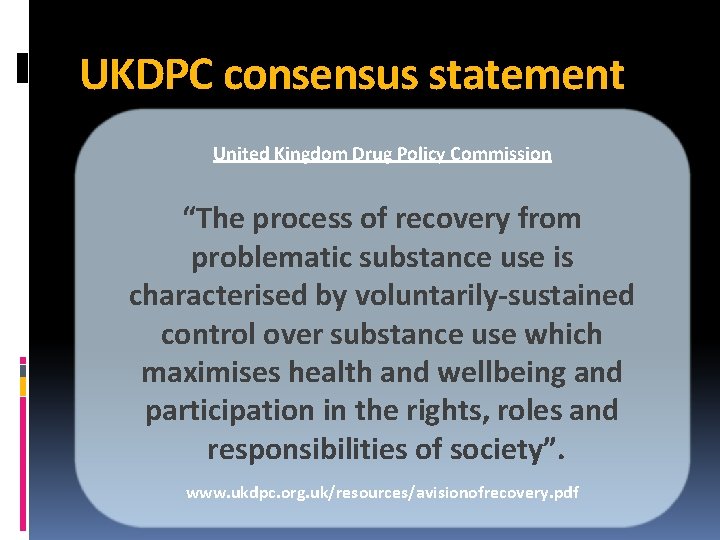
UKDPC consensus statement United Kingdom Drug Policy Commission “The process of recovery from problematic substance use is characterised by voluntarily-sustained control over substance use which maximises health and wellbeing and participation in the rights, roles and responsibilities of society”. www. ukdpc. org. uk/resources/avisionofrecovery. pdf
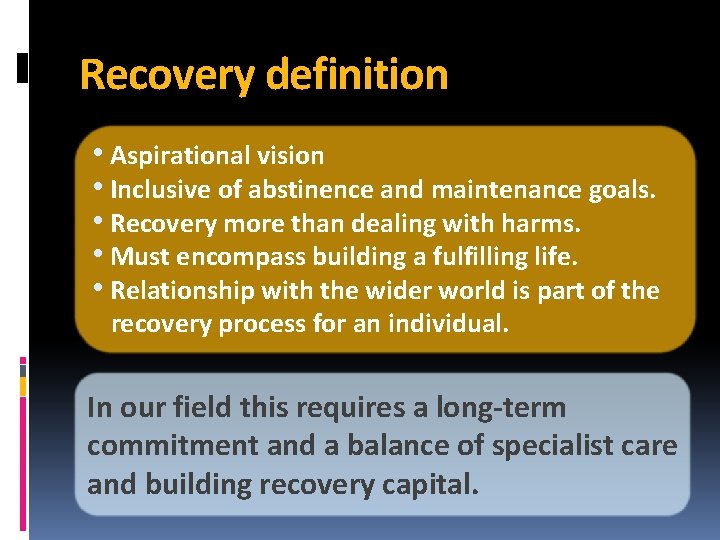
Recovery definition • Aspirational vision • Inclusive of abstinence and maintenance goals. • Recovery more than dealing with harms. • Must encompass building a fulfilling life. • Relationship with the wider world is part of the recovery process for an individual. In our field this requires a long-term commitment and a balance of specialist care and building recovery capital.
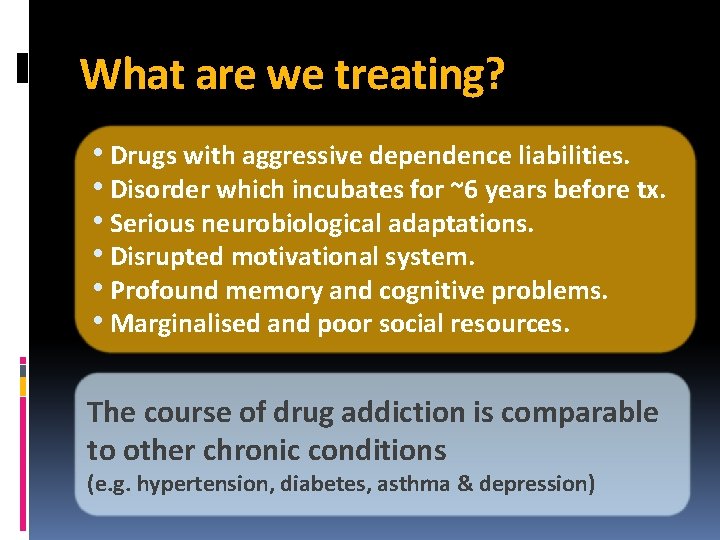
What are we treating? • Drugs with aggressive dependence liabilities. • Disorder which incubates for ~6 years before tx. • Serious neurobiological adaptations. • Disrupted motivational system. • Profound memory and cognitive problems. • Marginalised and poor social resources. The course of drug addiction is comparable to other chronic conditions (e. g. hypertension, diabetes, asthma & depression)
![How well are we doing 1 Twothirds treated before Stable recovery after How well are we doing? [1] • Two-thirds treated before. • Stable recovery after](https://slidetodoc.com/presentation_image/d8cdd9e5e5dcc94b62d613f26747e497/image-8.jpg)
How well are we doing? [1] • Two-thirds treated before. • Stable recovery after 3 -4 episodes of treatment. • Treatment: effects positive but delivery variable. • Arguably, many clients are ‘parked’ in OST. • Not enough focus on treating dependence. • Unplanned discharge rate too high. Trend towards shorter lengths of stay associated with increasing rates of continued drug use at discharge and readmission within the year. (Benyon, Bellis & Mc. Veigh 2006; BMC Public Health; 6: 205)
![How well are we doing 2 Average treatment pathway 10 months 70 How well are we doing? [2] • Average treatment pathway ~10 months. • ~70%](https://slidetodoc.com/presentation_image/d8cdd9e5e5dcc94b62d613f26747e497/image-9.jpg)
How well are we doing? [2] • Average treatment pathway ~10 months. • ~70% receive one treatment modality. • Some evidence of phased, linked interventions, but could be better. • Aftercare and follow-up Achilles' heel. • Many specialist agencies over worked and inward looking. Combination therapies way forward – OST platforms with protocol/manual guided psychosocial interventions (e. g. treatment incentives, CBT, interpersonal therapy, behavioural couples therapies.
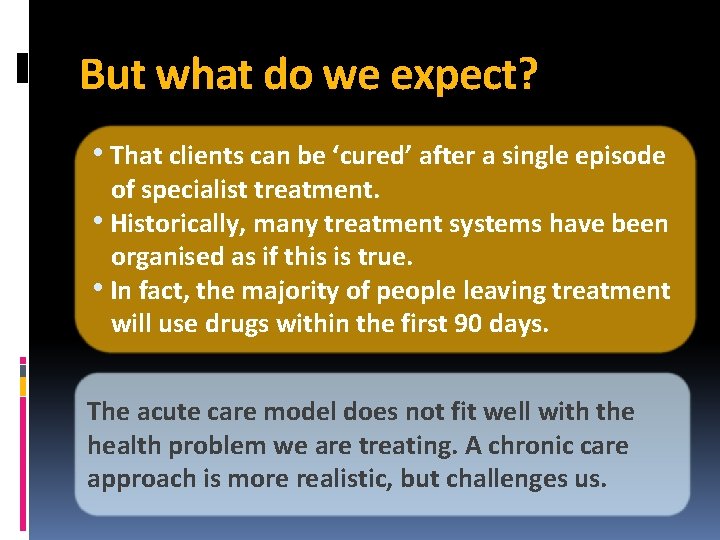
But what do we expect? • That clients can be ‘cured’ after a single episode of specialist treatment. • Historically, many treatment systems have been organised as if this is true. • In fact, the majority of people leaving treatment will use drugs within the first 90 days. The acute care model does not fit well with the health problem we are treating. A chronic care approach is more realistic, but challenges us.
What predicts recovery? • Resilience to social stressors. • Social supports. • Family life. • Identity shift to functional from dysfunctional. • Employment. • Stable housing.
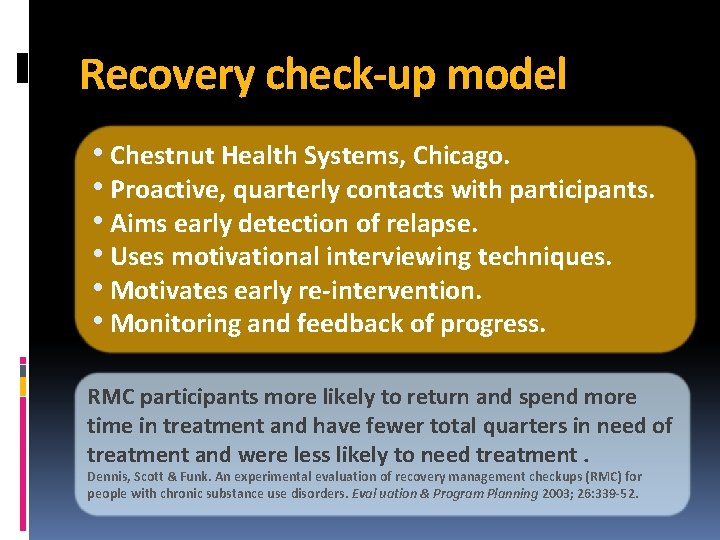
Recovery check-up model • Chestnut Health Systems, Chicago. • Proactive, quarterly contacts with participants. • Aims early detection of relapse. • Uses motivational interviewing techniques. • Motivates early re-intervention. • Monitoring and feedback of progress. RMC participants more likely to return and spend more time in treatment and have fewer total quarters in need of treatment and were less likely to need treatment. Dennis, Scott & Funk. An experimental evaluation of recovery management checkups (RMC) for people with chronic substance use disorders. Eval uation & Program Planning 2003; 26: 339 -52.
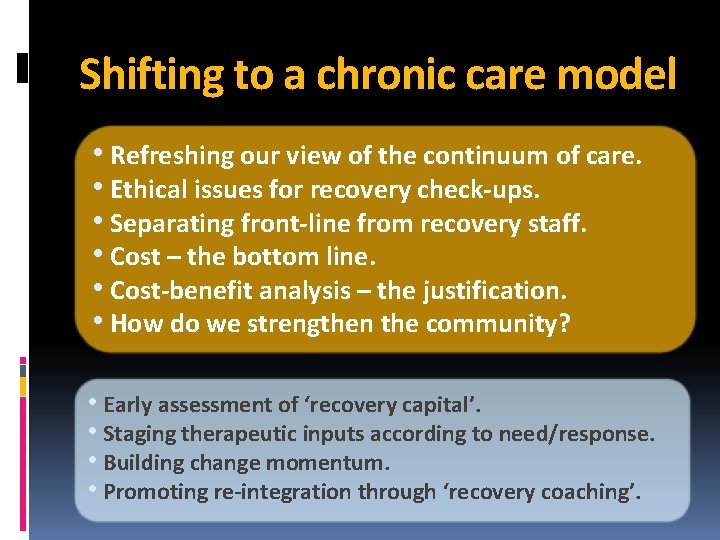
Shifting to a chronic care model • Refreshing our view of the continuum of care. • Ethical issues for recovery check-ups. • Separating front-line from recovery staff. • Cost – the bottom line. • Cost-benefit analysis – the justification. • How do we strengthen the community? • Early assessment of ‘recovery capital’. • Staging therapeutic inputs according to need/response. • Building change momentum. • Promoting re-integration through ‘recovery coaching’.
 Lirik lagu more more more we praise you
Lirik lagu more more more we praise you More more more i want more more more more we praise you
More more more i want more more more more we praise you John marsden addiction
John marsden addiction John marsden
John marsden Uzma moody
Uzma moody Vesper song of the reverend samuel marsden analysis
Vesper song of the reverend samuel marsden analysis Marsden
Marsden Marsden
Marsden Anticipatory care calendar
Anticipatory care calendar Great marsden
Great marsden Ed marsden
Ed marsden Greenstreet berman
Greenstreet berman John a. volpe national transportation systems center
John a. volpe national transportation systems center National treatment
National treatment