Islamic University of Gaza Faculty of Nursing Chapter

- Slides: 16
Islamic University of Gaza Faculty of Nursing Chapter (10) Assessment of musculo-skeletal system 1
*Subjective data: ask about: • Pain: at rest, with exercise, changes in shape or size of an extremity, changes in mobility to carry out activities of daily living, sports, and works. • Stiffness: time of day, relation to weight, " bearing or exercise". • Decreased or altered or absent sensations. • Redness or swelling of joints. • History of fractures and orthopedic surgery. • Occupational history. 2
• Assessment of musculo-skeletal system done firstly when the client walks, moves in bed or performs any type of physical activity. • Determine range of motion, muscle strength and tone, joint and muscle condition. • N. B: muscle problems commonly are manifestations of neurological disease, so you must do neurological assessment simultaneously. • Joints vary in their degree of mobility, range from freely movable e. g. knee, to slightly movable joints e. g. the spinal vertebra. 3
• During assessment of muscle groups: assess muscle weakness, or swelling, and size, then compare between sides. Joints should not be forced into painful positions. • Observe gait and posture as client walks into room. • Normally the client walks with arms swinging freely at sides and the head and the face leading the body. 4
• Loss of height is frequently the first clinical sign of osteoporosis. • Small amount of height loss expected with aging. • Ask client to put each joint through its full range of motion, if there is weakness, gently supporting & moving extremities through their range of motion, to assess abnormalities. • Normal joints are non tender, without swelling and move freely. **Elderly joints often become swollen & stiff, with reduced range of motion, resulting from cartilage erosion and fibrosis of synovial membranes. 5
Assessment of Neurological system • You can assess this system when doing physical examination e. g. cranial nerve function can be testing during the survey of the head and neck. • The neurological assessment consists of six parts: (mental status, cranial nerves, sensory functions, motor function, cerebellar function, reflexes). 6
*Subjective data: ask about: • Loss of consciousness, dizziness, and fainting. • Headache: precipitating factors and duration. • Numbness and tingling or paralysis or neuralgia. • Loss of memory, confusion, visual loss, blurring, and pain. • Facial pain, weakness, twitching, speech problems e. g. aphasia. • Swallowing problems and drooling. • Neck weakness or spasm. 7
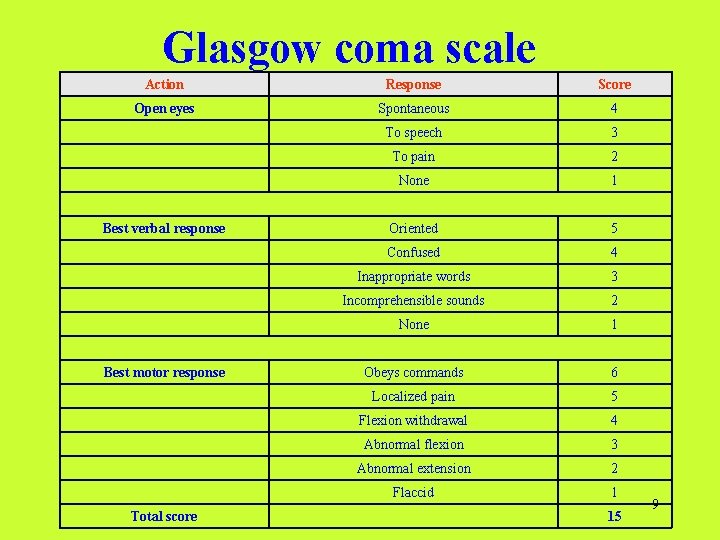
• Mental and emotional status is observed as the nursing history is collected, and by simply interacting with client, e. g. “Nursing care plan” • Level of consciousness, which ranges from full awakening, “alertness” to unresponsiveness to any form of external stimuli. • Alert client responds to questions spontaneously. • You can assess Level of consciousness by using Glasgow coma scale. 8
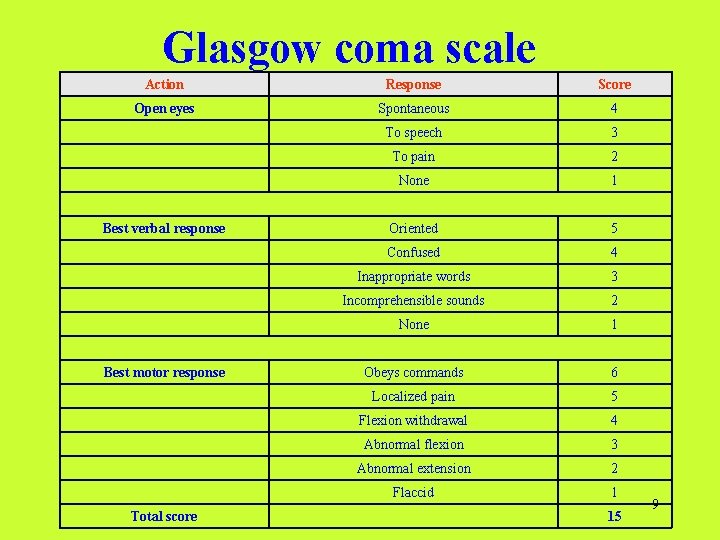
Glasgow coma scale Action Response Score Open eyes Spontaneous 4 To speech 3 To pain 2 None 1 Oriented 5 Confused 4 Inappropriate words 3 Incomprehensible sounds 2 None 1 Obeys commands 6 Localized pain 5 Flexion withdrawal 4 Abnormal flexion 3 Abnormal extension 2 Flaccid 1 Best verbal response Best motor response Total score 15 9
*Assessment of behavior and appearance • Behavior, mood, hygiene, grooming and choice of dress reveal pertinent information about client’s mental status. • Appearance reflects how a client feels about the self. • Personal hygiene such as unkempt hair, a dirty body, or broken, dirty fingernails should be noted. *Language: Assess ability of individual to understand spoken or written words & how he/she speaks or writes. 10
• Assess intellectual function, which includes: memory “recent, immediate, past”, knowledge, abstract thinking, association and judgment. * Assess for sensory function: - Assess sensitivity to light touch “cotton” - Assess sensitivity to pain “pinprick” - Assess sensitivity to vibrations “tuning fork” - Assess sensitivity to positions. **Don’t forget comparing both sides of body 11
Assessment of the breast Subjective data: ask about: • Tenderness, pain, swelling, or change in size of breasts. • Change in position of nipple or nipple discharge. • Presence of cysts, lumps, and lesions. • History of prior breast surgery. 12
*Female breast: *Inspection: • With the client sitting, arms relaxed at sides. Inspect Areola and nipples for position, pigmentation, inversion, discharge, crusting & masses. • Examine the breast tissue for size, shape, color, symmetry, surface, contour, skin characteristics. • Assess level of breasts, notes any retractions or dimpling of the skin. • Ask client to elevate her hands over head, repeat the observation. • Ask client to press her hands to her hips and repeat observation. 13
*Palpation: • Best done in recumbent position: -Raise the arm of client on the side of the breast being palpated above clients head. -Palpate the breast from less painful or less diseased area -Use on palpation palmer aspects of the fingers in a rotating motion, compressing the breast tissue against the chest wall, this is done quadrant by until the entire breast has been palpated. 14
-Note skin texture, moisture, temperature, or masses. -Gently squeeze the nipple and note any expressible discharge (Normally not present in non lactating women). -Repeat examination on the opposite breast & compare findings. **N. B: If mass is palpated, its location, size, shape, consistency, mobility and associated tenderness are reported. 15

*Male Breast: • Examination of male breast can be brief and should never be omitted. • Observe nipple & Palpate Areola for ulceration, nodules, swelling or discharge (Normally not present). *Genitourinary and reproductive assessment • You must focus your questions on the following: -Any bulges or pain when straining or lifting heavy objects. -Unusual drainage. -Pain with urination or incontinence. -Lower abdominal pain. 16
 Bil soruyu bas gaza
Bil soruyu bas gaza Paul wittek gazâ tezi
Paul wittek gazâ tezi Bil soruyu bas gaza
Bil soruyu bas gaza Gaza strip map
Gaza strip map Gaza strip map
Gaza strip map Mapa franja de gaza
Mapa franja de gaza Estado de israel palestina
Estado de israel palestina Gaza central desalination plant
Gaza central desalination plant Gáza
Gáza Oshbe
Oshbe Islamic university college
Islamic university college Faculty of medicine nursing and health sciences
Faculty of medicine nursing and health sciences Ulm nursing faculty
Ulm nursing faculty University of split faculty of maritime studies
University of split faculty of maritime studies University of bridgeport computer science
University of bridgeport computer science Bridgeport university computer science
Bridgeport university computer science Hubert kairuki memorial university faculty of medicine
Hubert kairuki memorial university faculty of medicine