GOLD STANDARD FRAMEWORK GSF END OF LIFE CARE
- Slides: 7
GOLD STANDARD FRAMEWORK (GSF) END OF LIFE CARE AT PARK MEDICAL PRACTICE Amelia Randle, Somerset GP and SWAG Cancer Alliance Lead (GP Practice actual approaches to GSF may slightly vary)
PATIENT IDENTIFICATION AND TRACKING The GP End of Life Practice Lead and Secretary are notified of all patients identified as at the beginning of the end of life via: Hospital letters Patient contact. Patients are tracked and prioritised using three categories: Active treatment Prognosis months (flagged as amber) Prognosis weeks/days (flagged as red).
Each patient is assigned a Lead GP and a second GP to provide balance of continuity and accessible support The Lead GP is responsible for providing a regular review of ongoing care needs, and ensuring that all practicalities are in place – including the checklist in the following slides A GSF meeting is held on a monthly basis with District Nurses and Dorothy House Community Nurses when all Amber and Red patients are discussed All vulnerable patients, including those at end of life, are discussed at a weekly meeting of clinical staff The practice is in the process of establishing a shared record with Dorothy House staff to enable them to raise prescription requests and enter notes into patient records.
END OF LIFE CHECKLIST 1) Seek consent for patient to be added to register. Add patient to GSF folder in population manger. This is important as it will let GSF team know to discuss at monthly GSF meeting held with District Nurses and Dorothy House at 3 pm on first Monday of the month. 2) Ask patient their preferred place of care and enter code on EMIS (choices appear if you type ‘preferred place of care’) 3) DNAR form – leave copy in home. If completing in surgery, give original to reception staff. Or you can leave with MAR chart at pharmacy for collection along with Just In Case (JIC) meds. 4) Prescribe JIC medications. Fill out FP 10 and give to pharmacy or relatives. Ensure sufficient supplies to cover out of hospital period.
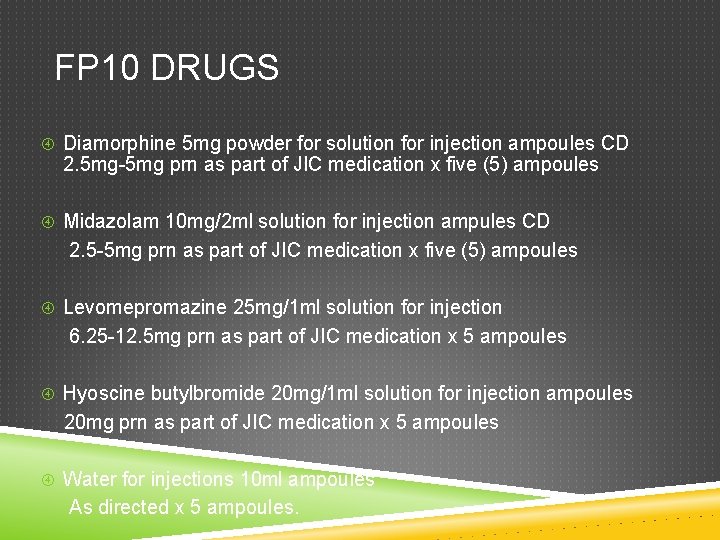
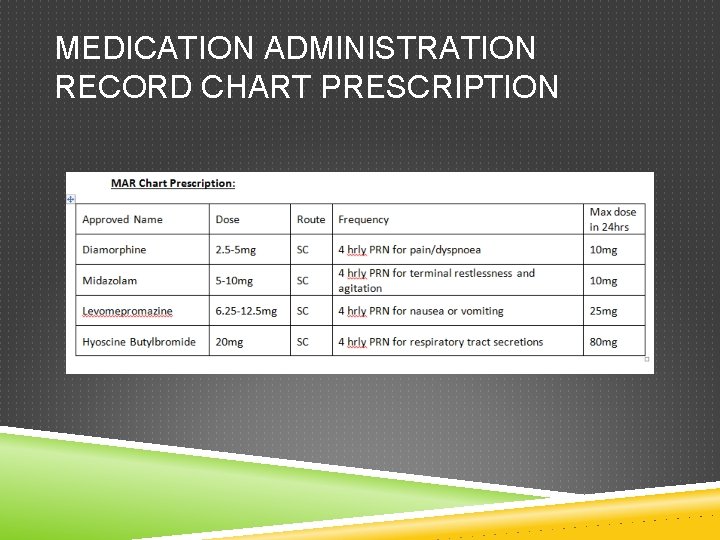
FP 10 DRUGS Diamorphine 5 mg powder for solution for injection ampoules CD 2. 5 mg-5 mg prn as part of JIC medication x five (5) ampoules Midazolam 10 mg/2 ml solution for injection ampules CD 2. 5 -5 mg prn as part of JIC medication x five (5) ampoules Levomepromazine 25 mg/1 ml solution for injection 6. 25 -12. 5 mg prn as part of JIC medication x 5 ampoules Hyoscine butylbromide 20 mg/1 ml solution for injection ampoules 20 mg prn as part of JIC medication x 5 ampoules Water for injections 10 ml ampoules As directed x 5 ampoules.
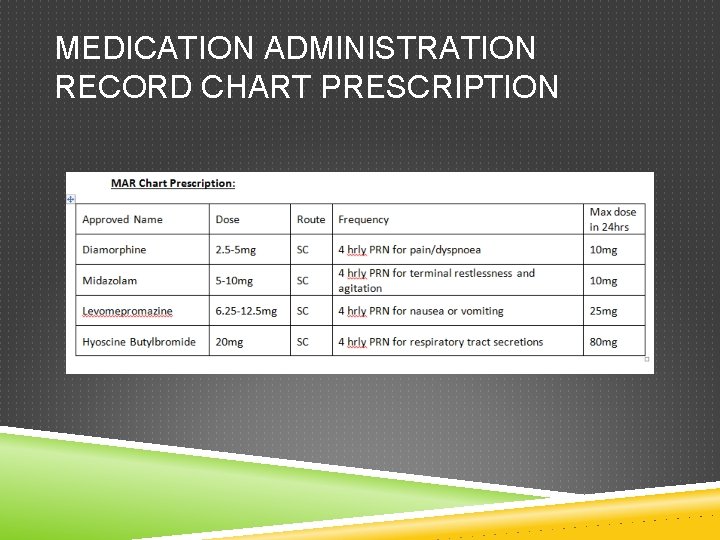
MEDICATION ADMINISTRATION RECORD CHART PRESCRIPTION
CHECKLIST CONTINUED Inform District Nurses of prescription of just in case medications and addition to GSF register – they will add to their caseload Complete Expected Death Form if the patient is in a nursing or residential home, if it would be appropriate for a qualified nurse to perform certification of death Complete special patient note on Adastra Electronic Patient Management Register.