FRI 0358 Usage of Creactive Protein Testing in
- Slides: 1
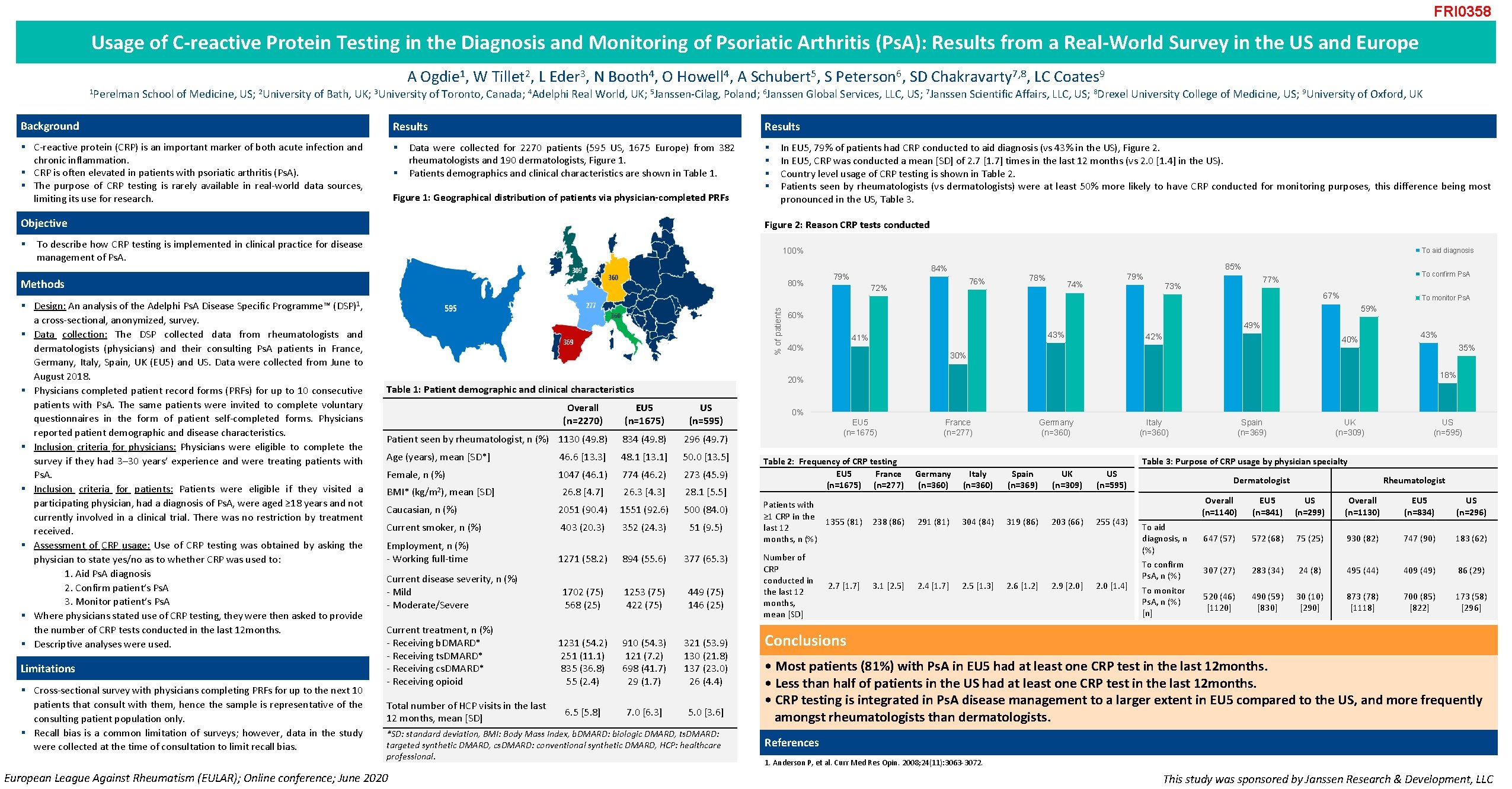
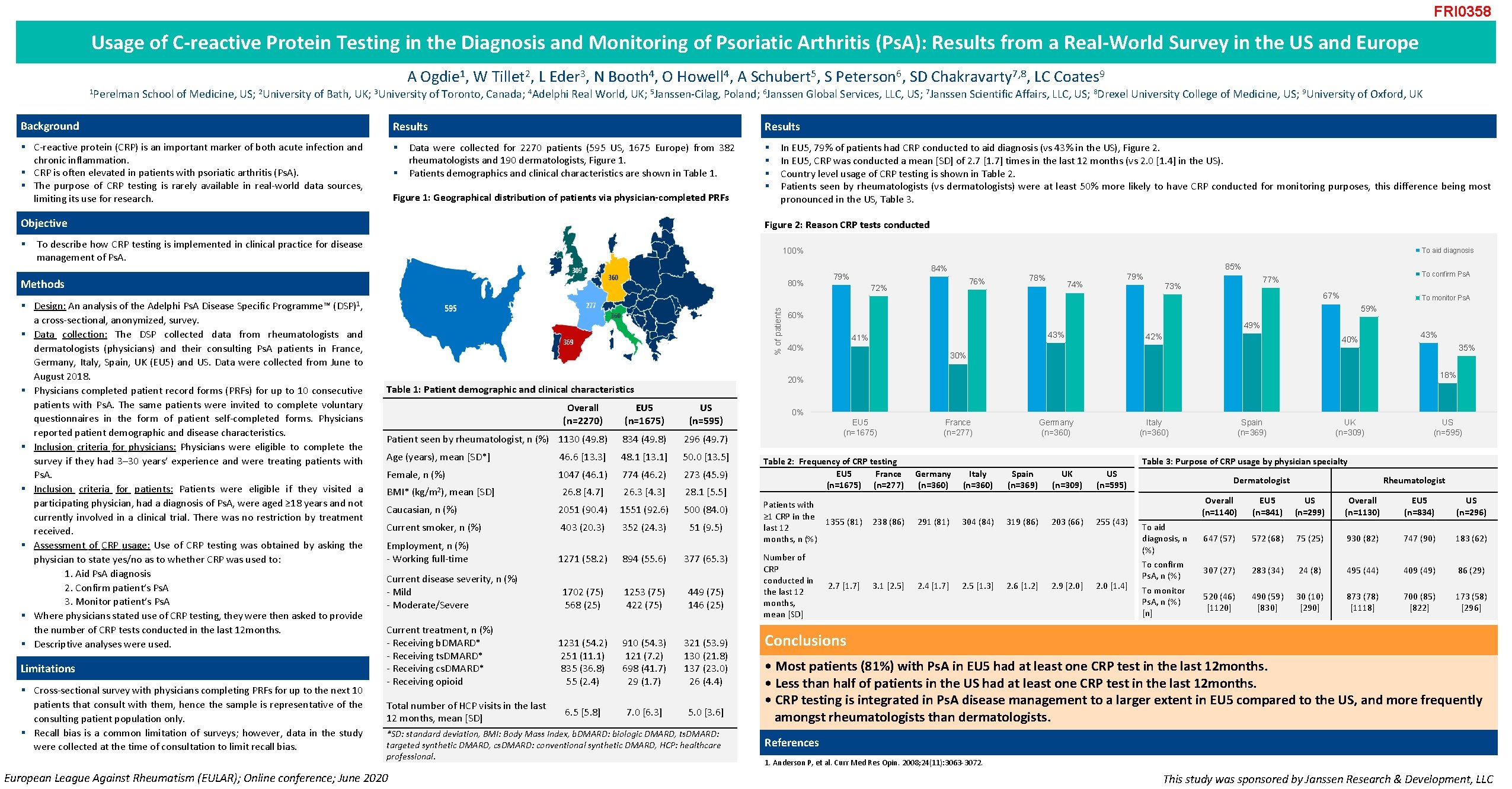
FRI 0358 Usage of C-reactive Protein Testing in the Diagnosis and Monitoring of Psoriatic Arthritis (Ps. A): Results from a Real-World Survey in the US and Europe 1 Perelman A Ogdie 1, W Tillet 2, L Eder 3, N Booth 4, O Howell 4, A Schubert 5, S Peterson 6, SD Chakravarty 7, 8, LC Coates 9 School of Medicine, US; 2 University of Bath, UK; 3 University of Toronto, Canada; 4 Adelphi Real World, UK; 5 Janssen-Cilag, Poland; 6 Janssen Global Services, LLC, US; 7 Janssen Scientific Affairs, LLC, US; 8 Drexel University College of Medicine, US; 9 University of Oxford, UK Background Results § C-reactive protein (CRP) is an important marker of both acute infection and chronic inflammation. § CRP is often elevated in patients with psoriatic arthritis (Ps. A). § The purpose of CRP testing is rarely available in real-world data sources, limiting its use for research. § § Results Data were collected for 2270 patients (595 US, 1675 Europe) from 382 rheumatologists and 190 dermatologists, Figure 1. Patients demographics and clinical characteristics are shown in Table 1. Figure 1: Geographical distribution of patients via physician-completed PRFs Objective § § § In EU 5, 79% of patients had CRP conducted to aid diagnosis (vs 43% in the US), Figure 2. In EU 5, CRP was conducted a mean [SD] of 2. 7 [1. 7] times in the last 12 months (vs 2. 0 [1. 4] in the US). Country level usage of CRP testing is shown in Table 2. Patients seen by rheumatologists (vs dermatologists) were at least 50% more likely to have CRP conducted for monitoring purposes, this difference being most pronounced in the US, Table 3. Figure 2: Reason CRP tests conducted To describe how CRP testing is implemented in clinical practice for disease management of Ps. A. 100% Methods 80% § Design: An analysis of the Adelphi Ps. A Disease Specific Programme™ a cross-sectional, anonymized, survey. § Data collection: The DSP collected data from rheumatologists and dermatologists (physicians) and their consulting Ps. A patients in France, Germany, Italy, Spain, UK (EU 5) and US. Data were collected from June to August 2018. § Physicians completed patient record forms (PRFs) for up to 10 consecutive patients with Ps. A. The same patients were invited to complete voluntary questionnaires in the form of patient self-completed forms. Physicians reported patient demographic and disease characteristics. § Inclusion criteria for physicians: Physicians were eligible to complete the survey if they had 3– 30 years’ experience and were treating patients with Ps. A. § Inclusion criteria for patients: Patients were eligible if they visited a participating physician, had a diagnosis of Ps. A, were aged ≥ 18 years and not currently involved in a clinical trial. There was no restriction by treatment received. § Assessment of CRP usage: Use of CRP testing was obtained by asking the physician to state yes/no as to whether CRP was used to: 1. Aid Ps. A diagnosis 2. Confirm patient’s Ps. A 3. Monitor patient’s Ps. A § Where physicians stated use of CRP testing, they were then asked to provide the number of CRP tests conducted in the last 12 months. § Descriptive analyses were used. Limitations § Cross-sectional survey with physicians completing PRFs for up to the next 10 patients that consult with them, hence the sample is representative of the consulting patient population only. § Recall bias is a common limitation of surveys; however, data in the study were collected at the time of consultation to limit recall bias. % of patients (DSP)1, EU 5 (n=1675) US (n=595) Patient seen by rheumatologist, n (%) 1130 (49. 8) 834 (49. 8) 296 (49. 7) Age (years), mean [SD*] 46. 6 [13. 3] 48. 1 [13. 1] 50. 0 [13. 5] Female, n (%) 1047 (46. 1) 774 (46. 2) 273 (45. 9) 26. 8 [4. 7] 26. 3 [4. 3] 28. 1 [5. 5] BMI* (kg/m 2), mean [SD] Caucasian, n (%) 2051 (90. 4) 1551 (92. 6) 500 (84. 0) Current smoker, n (%) 403 (20. 3) 352 (24. 3) 51 (9. 5) Employment, n (%) - Working full-time 1271 (58. 2) 894 (55. 6) 377 (65. 3) 1702 (75) 568 (25) 1253 (75) 422 (75) 449 (75) 146 (25) 1231 (54. 2) 251 (11. 1) 835 (36. 8) 55 (2. 4) 910 (54. 3) 121 (7. 2) 698 (41. 7) 29 (1. 7) 321 (53. 9) 130 (21. 8) 137 (23. 0) 26 (4. 4) 6. 5 [5. 8] 7. 0 [6. 3] 5. 0 [3. 6] Current disease severity, n (%) - Mild - Moderate/Severe Current treatment, n (%) - Receiving b. DMARD* - Receiving ts. DMARD* - Receiving cs. DMARD* - Receiving opioid Total number of HCP visits in the last 12 months, mean [SD] *SD: standard deviation, BMI: Body Mass Index, b. DMARD: biologic DMARD, ts. DMARD: targeted synthetic DMARD, cs. DMARD: conventional synthetic DMARD, HCP: healthcare professional. European League Against Rheumatism (EULAR); Online conference; June 2020 85% 84% 79% 76% 72% 78% 79% 74% To confirm Ps. A 77% 73% 67% To monitor Ps. A 59% 60% 49% 43% 41% 40% 42% 40% 43% 35% 30% 18% 20% Table 1: Patient demographic and clinical characteristics Overall (n=2270) To aid diagnosis 0% EU 5 (n=1675) Table 2: Frequency of CRP testing EU 5 France (n=1675) (n=277) Patients with ≥ 1 CRP in the 1355 (81) last 12 months, n (%) Number of CRP conducted in the last 12 months, mean [SD] 2. 7 [1. 7] 238 (86) 3. 1 [2. 5] France (n=277) Germany (n=360) Italy (n=360) Spain (n=369) UK (n=309) US (n=595) Table 3: Purpose of CRP usage by physician specialty Germany (n=360) 291 (81) 2. 4 [1. 7] Italy (n=360) 304 (84) 2. 5 [1. 3] Spain (n=369) 319 (86) 2. 6 [1. 2] UK (n=309) 203 (66) 2. 9 [2. 0] US (n=595) 255 (43) 2. 0 [1. 4] Dermatologist Rheumatologist Overall (n=1140) EU 5 (n=841) US (n=299) Overall (n=1130) EU 5 (n=834) US (n=296) To aid diagnosis, n (%) 647 (57) 572 (68) 75 (25) 930 (82) 747 (90) 183 (62) To confirm Ps. A, n (%) 307 (27) 283 (34) 24 (8) 495 (44) 409 (49) 86 (29) To monitor Ps. A, n (%) [n] 520 (46) [1120] 490 (59) [830] 30 (10) [290] 873 (78) [1118] 700 (85) [822] 173 (58) [296] Conclusions • Most patients (81%) with Ps. A in EU 5 had at least one CRP test in the last 12 months. • Less than half of patients in the US had at least one CRP test in the last 12 months. • CRP testing is integrated in Ps. A disease management to a larger extent in EU 5 compared to the US, and more frequently amongst rheumatologists than dermatologists. References 1. Anderson P, et al. Curr Med Res Opin. 2008; 24(11): 3063 -3072. This study was sponsored by Janssen Research & Development, LLC