Enhanced Killing of Methicillin Resistant Staphylococcus aureus MRSA

- Slides: 9
Enhanced Killing of Methicillin. Resistant Staphylococcus aureus (MRSA) Strains With Gatifloxacin and Benzalkonium Chloride Joseph M. Blondeau, Ph. D; Christine Hesje, BSc Royal University Hospital and the University of Saskatchewan, Saskatoon, Saskatchewan, Canada Financial Disclosures This study was supported by an unrestricted educational grant from Allergan, Inc. , Irvine, CA. Authors have no financial interest.
INTRODUCTION Gram-positive staphylococcal species are common bacteria cultured from normal ocular flora and patients with endophthalmitis, keratitis, and conjunctivitis. 1 Antibacterial resistance among staphylococci such as Staphylococcus aureus is on the rise. § Among ocular isolates of S aureus, resistance to methicillin has significantly increased over the last decade, from less than 5. 0% to over 15. 0%. 2, 3 § Methicillin-resistant S aureus (MRSA) strains are now prevalent in both the hospital and community settings. 4 Effective therapeutic strategies are, therefore, necessary to prevent and treat ocular infections that result from resistant strains of bacteria.
INTRODUCTION Gatifloxacin ophthalmic solution 0. 3% (Zymar®; Allergan, Inc. ; Irvine, CA) is a fourth-generation fluoroquinolone that is frequently used against ocular infections. 5 Conventionally, the efficacy of ophthalmic antibiotic preparations against ocular pathogens is evaluated by considering only the active antibacterial ingredient. 6, 7 Zymar, however, contains 0. 005% benzalkonium chloride (BAK) (50 μg/m. L) as a preservative agent. 5 Preservatives exert antibacterial activity against Grampositive bacteria and thus may augment the potency of the active antibacterial ingredient. 8 This study was designed to determine if killing of MRSA strains by gatifloxacin is enhanced by BAK.
METHODS Two MRSA isolates collected through the clinical microbiology laboratory at Royal University Hospital in Saskatoon, Saskatchewan, Canada, were used in this study. Bacteria were identified by using the reference procedures as 9 indicated in the Manual of Clinical Microbiology. MRSA isolates (105 colony-forming units) were incubated with various concentrations of BAK, gatifloxacin plus BAK, or Zymar. The percentage of killed bacteria was determined after o o 20 or 30 minutes incubation at 35 C to 37 C in ambient air. Each timepoint was tested in triplicate and the values averaged, as were the values for both strains.
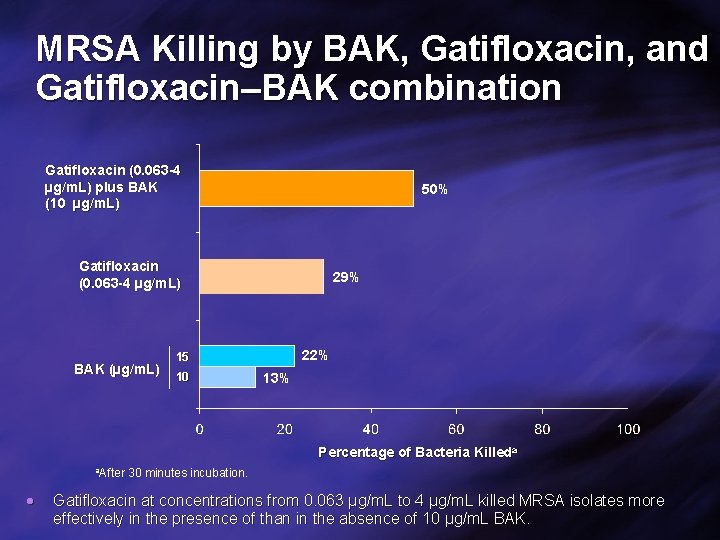
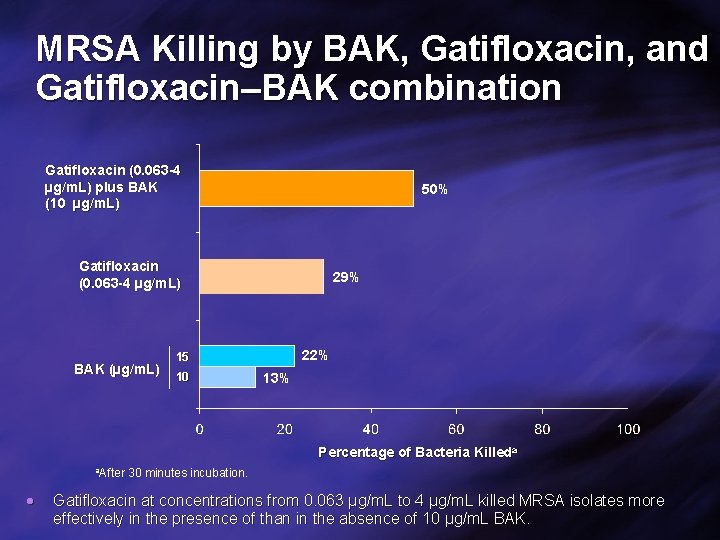
MRSA Killing by BAK, Gatifloxacin, and Gatifloxacin–BAK combination Gatifloxacin (0. 063 -4 µg/m. L) plus BAK (10 µg/m. L) 50% Gatifloxacin (0. 063 -4 µg/m. L) BAK (µg/m. L) 29% 22% 15 10 13% Percentage of Bacteria Killeda a. After 30 minutes incubation. Gatifloxacin at concentrations from 0. 063 µg/m. L to 4 µg/m. L killed MRSA isolates more effectively in the presence of than in the absence of 10 µg/m. L BAK.
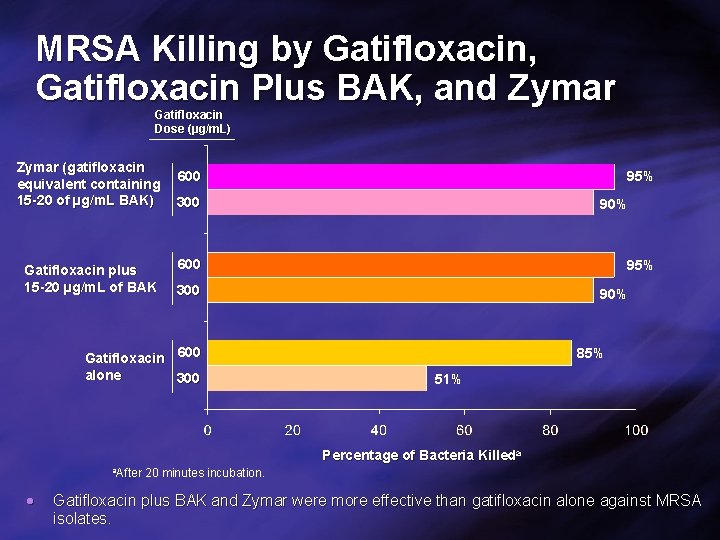
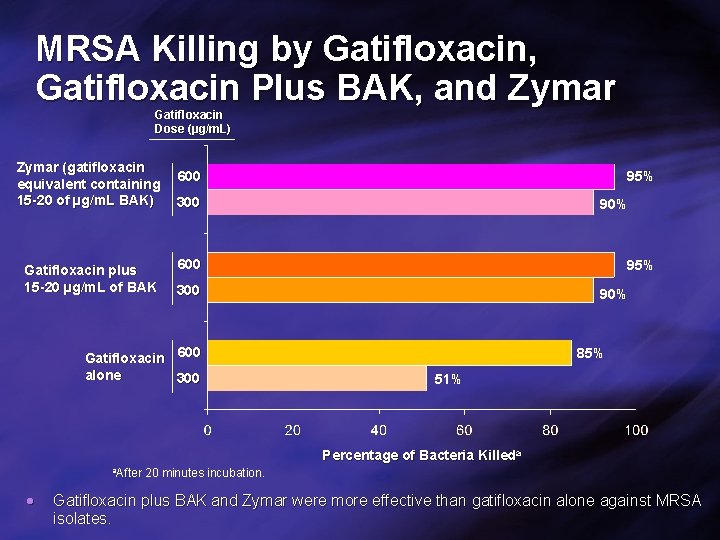
MRSA Killing by Gatifloxacin, Gatifloxacin Plus BAK, and Zymar Gatifloxacin Dose (µ (µg/m. L) Zymar (gatifloxacin equivalent containing 15 -20 of µg/m. L BAK) Gatifloxacin plus 15 -20 µg/m. L of BAK 600 95% 300 90% 600 95% 300 Gatifloxacin 600 alone 300 90% 85% 51% Percentage of Bacteria Killeda a. After 20 minutes incubation. Gatifloxacin plus BAK and Zymar were more effective than gatifloxacin alone against MRSA isolates.
DISCUSSION • Gatifloxacin plus BAK and Zymar were more effective than either gatifloxacin or BAK alone against MRSA. • Consistent with these findings, we recently demonstrated that the addition of BAK dramatically lowered the minimum inhibitory concentration of gatifloxacin against MRSA. 10 • These findings suggest that the presence of BAK in Zymar may serve to enhance antibacterial efficacy of gatifloxacin. • A recent study demonstrated that gatifloxacin plus BAK was significantly more effective than either gatifloxacin or BAK alone in killing gatifloxacin–resistant MRSA in vivo. 11 • The contribution of BAK may also explain the in vivo efficacy of Zymar against S aureus that were resistant to the gatifloxacin molecule in vitro. 12, 13 • These findings point out the importance of evaluating the efficacy of ocular antibiotics on the basis of their ophthalmic formulations rather than simply the active ingredients.
CONCLUSIONS • Gatifloxacin plus BAK killed more bacteria than gatifloxacin alone, indicating that BAK enhanced bactericidal activity of gatifloxacin. • These findings suggest that Zymar, which contains BAK, is effective against resistant pathogens.

References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. Kowalski RP, Dhaliwal DK. Expert Rev Anti Infect Ther. 2005; 3: 131 -139. Cavuoto K, Zutshi D, Karp CL, et al. Ophthalmology. 2008; 115: 51 -56. Freidlin J, Acharya N, Lietman TM, et al. Am J Ophthalmol. 2007; 144: 313 -315. Blomquist PH. Trans Am Ophthalmol Soc. 2006; 104: 322 -345. Zymar® [package insert]. Irvine, CA: Allergan, Inc. ; 2007. Callegan MC, Ramirez R, Kane ST, et al. Adv Ther. 2003; 20: 246 -252. Kowalski RP, Yates KA, Romanowski EG, et al. Ophthalmology. 2005; 112: 1987. e 1 -1987. e 6. Dantas PE, Uesugui E, Nishiwaki-Dantas MC, et al. Cornea. 2000; 19: 353 -354. Isenberg HD. Clinical Microbiology Procedures Handbook. Washington, D. C. : American Society for Microbiology; 1992. Blondeau JM, Borsos S, Hesje CK. J Chemother. 2007; 19: 146 -151. Romanowski EG, Mah FS, Kowalski RP, et al. J Ocul Pharmacol Ther. 2008; 24: 380 -384. Romanowski EG, Mah FS, Yates KA, et al. Am J Ophthalmol. 2005; 139: 867 -877. Tungsiripat T, Sarayba MA, Kaufman MB, et al. Am J Ophthalmol. 2003; 136: 76 -81.
 Staphylococcus aureus
Staphylococcus aureus Staphylococcus aureus
Staphylococcus aureus 4 domains of life
4 domains of life Portage staphylococcus aureus
Portage staphylococcus aureus Staphylococcus aureus bacteria structure
Staphylococcus aureus bacteria structure Staphylococcus gamma hemolysis
Staphylococcus gamma hemolysis Staphylococcus aureus bacteria structure
Staphylococcus aureus bacteria structure Selective and differential media
Selective and differential media Enzymes of staphylococcus aureus
Enzymes of staphylococcus aureus Staphylococcus aureus cocci or bacilli
Staphylococcus aureus cocci or bacilli