Emergency airway management in Suspected PraderWilli syndrome Dr
- Slides: 1
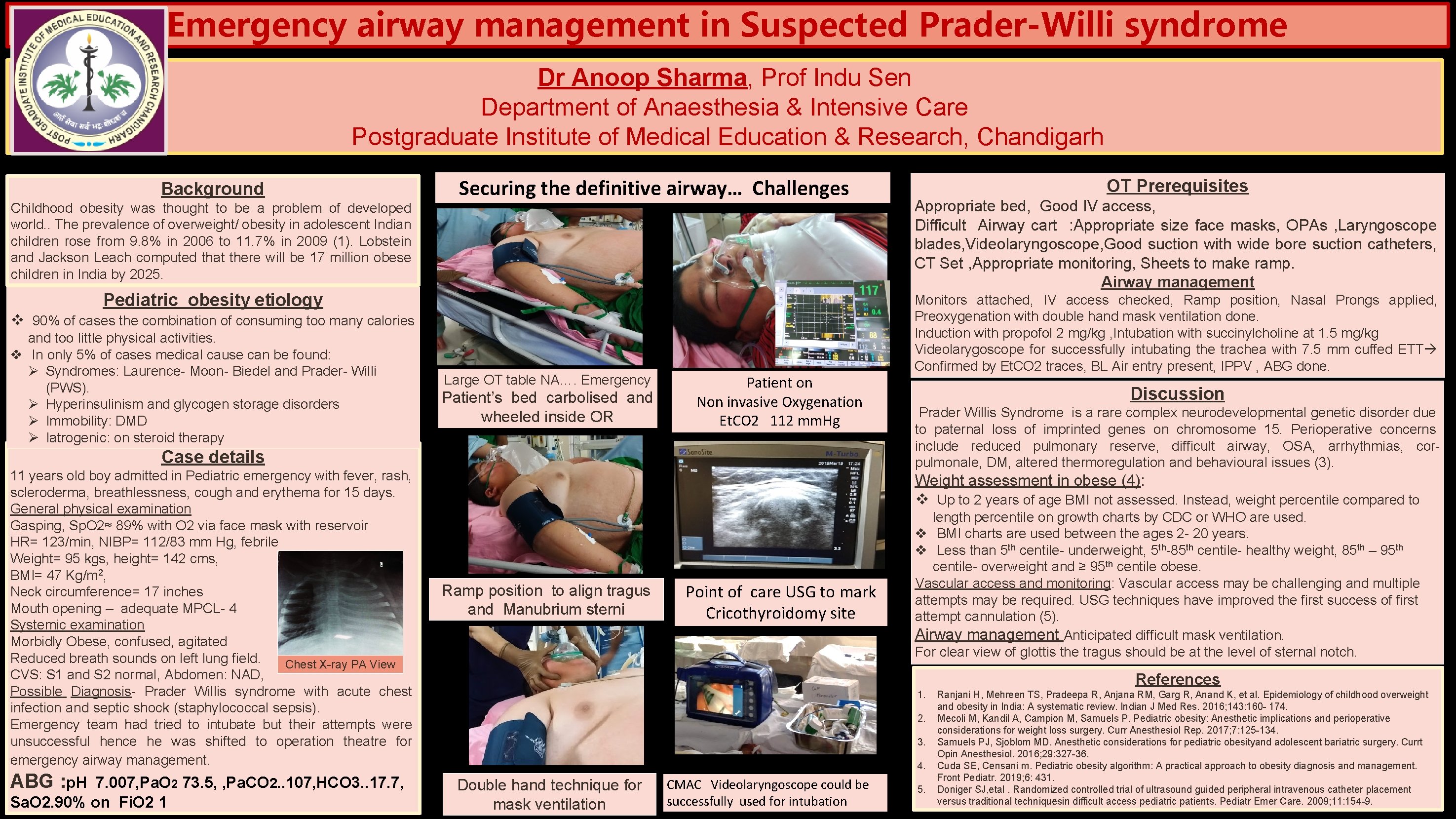
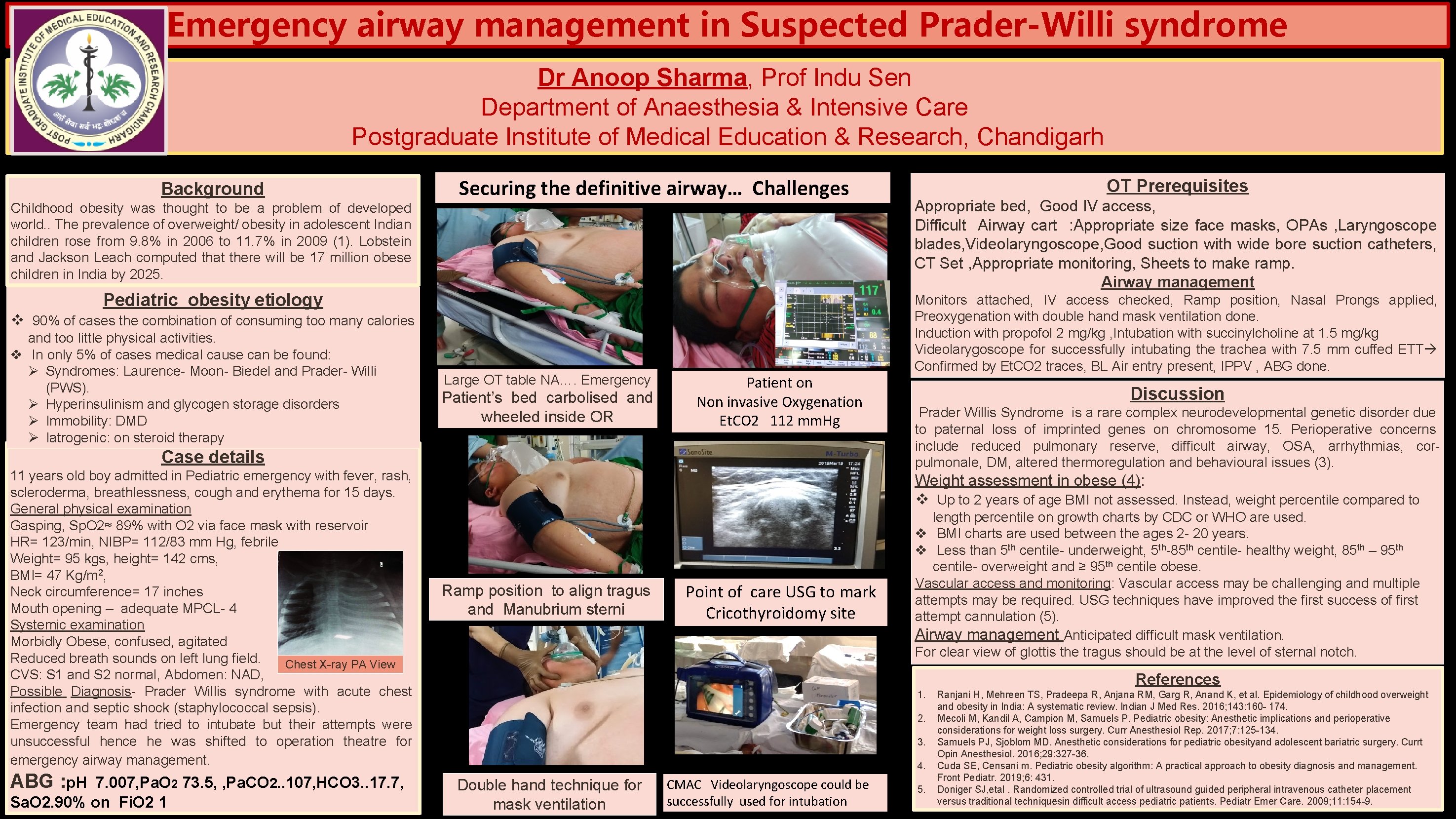
Emergency airway management in Suspected Prader-Willi syndrome Dr Anoop Sharma, Prof Indu Sen Department of Anaesthesia & Intensive Care Postgraduate Institute of Medical Education & Research, Chandigarh Background Childhood obesity was thought to be a problem of developed world. . The prevalence of overweight/ obesity in adolescent Indian children rose from 9. 8% in 2006 to 11. 7% in 2009 (1). Lobstein and Jackson Leach computed that there will be 17 million obese children in India by 2025. Securing the definitive airway… Challenges Pediatric obesity etiology v 90% of cases the combination of consuming too many calories and too little physical activities. v In only 5% of cases medical cause can be found: Ø Syndromes: Laurence- Moon- Biedel and Prader- Willi (PWS). Ø Hyperinsulinism and glycogen storage disorders Ø Immobility: DMD Ø Iatrogenic: on steroid therapy Large OT table NA…. Emergency Patient’s bed carbolised and wheeled inside OR Patient on Non invasive Oxygenation Et. CO 2 112 mm. Hg Case details 11 years old boy admitted in Pediatric emergency with fever, rash, scleroderma, breathlessness, cough and erythema for 15 days. General physical examination Gasping, Sp. O 2≈ 89% with O 2 via face mask with reservoir HR= 123/min, NIBP= 112/83 mm Hg, febrile Weight= 95 kgs, height= 142 cms, BMI= 47 Kg/m 2, Neck circumference= 17 inches Mouth opening – adequate MPCL- 4 Systemic examination Morbidly Obese, confused, agitated Reduced breath sounds on left lung field. Chest X-ray PA View CVS: S 1 and S 2 normal, Abdomen: NAD, Possible Diagnosis- Prader Willis syndrome with acute chest infection and septic shock (staphylococcal sepsis). Emergency team had tried to intubate but their attempts were unsuccessful hence he was shifted to operation theatre for emergency airway management. ABG : p. H 7. 007, Pa. O 2 73. 5, , Pa. CO 2. . 107, HCO 3. . 17. 7, Sa. O 2. 90% on Fi. O 2 1 OT Prerequisites Appropriate bed, Good IV access, Difficult Airway cart : Appropriate size face masks, OPAs , Laryngoscope blades, Videolaryngoscope, Good suction with wide bore suction catheters, CT Set , Appropriate monitoring, Sheets to make ramp. Airway management Monitors attached, IV access checked, Ramp position, Nasal Prongs applied, Preoxygenation with double hand mask ventilation done. Induction with propofol 2 mg/kg , Intubation with succinylcholine at 1. 5 mg/kg Videolarygoscope for successfully intubating the trachea with 7. 5 mm cuffed ETT Confirmed by Et. CO 2 traces, BL Air entry present, IPPV , ABG done. Discussion Prader Willis Syndrome is a rare complex neurodevelopmental genetic disorder due to paternal loss of imprinted genes on chromosome 15. Perioperative concerns include reduced pulmonary reserve, difficult airway, OSA, arrhythmias, corpulmonale, DM, altered thermoregulation and behavioural issues (3). Weight assessment in obese (4): v Up to 2 years of age BMI not assessed. Instead, weight percentile compared to Ramp position to align tragus and Manubrium sterni Point of care USG to mark Cricothyroidomy site length percentile on growth charts by CDC or WHO are used. v BMI charts are used between the ages 2 - 20 years. v Less than 5 th centile- underweight, 5 th-85 th centile- healthy weight, 85 th – 95 th centile- overweight and ≥ 95 th centile obese. Vascular access and monitoring: Vascular access may be challenging and multiple attempts may be required. USG techniques have improved the first success of first attempt cannulation (5). Airway management Anticipated difficult mask ventilation. For clear view of glottis the tragus should be at the level of sternal notch. References 1. 2. 3. 4. Double hand technique for mask ventilation CMAC Videolaryngoscope could be successfully used for intubation 5. Ranjani H, Mehreen TS, Pradeepa R, Anjana RM, Garg R, Anand K, et al. Epidemiology of childhood overweight and obesity in India: A systematic review. Indian J Med Res. 2016; 143: 160 - 174. Mecoli M, Kandil A, Campion M, Samuels P. Pediatric obesity: Anesthetic implications and perioperative considerations for weight loss surgery. Curr Anesthesiol Rep. 2017; 7: 125 -134. Samuels PJ, Sjoblom MD. Anesthetic considerations for pediatric obesityand adolescent bariatric surgery. Currt Opin Anesthesiol. 2016; 29: 327 -36. Cuda SE, Censani m. Pediatric obesity algorithm: A practical approach to obesity diagnosis and management. Front Pediatr. 2019; 6: 431. Doniger SJ, etal. Randomized controlled trial of ultrasound guided peripheral intravenous catheter placement versus traditional techniquesin difficult access pediatric patients. Pediatr Emer Care. 2009; 11: 154 -9.