Effect of Epinephrine on outcomes in OutofHospital Cardiac


- Slides: 4
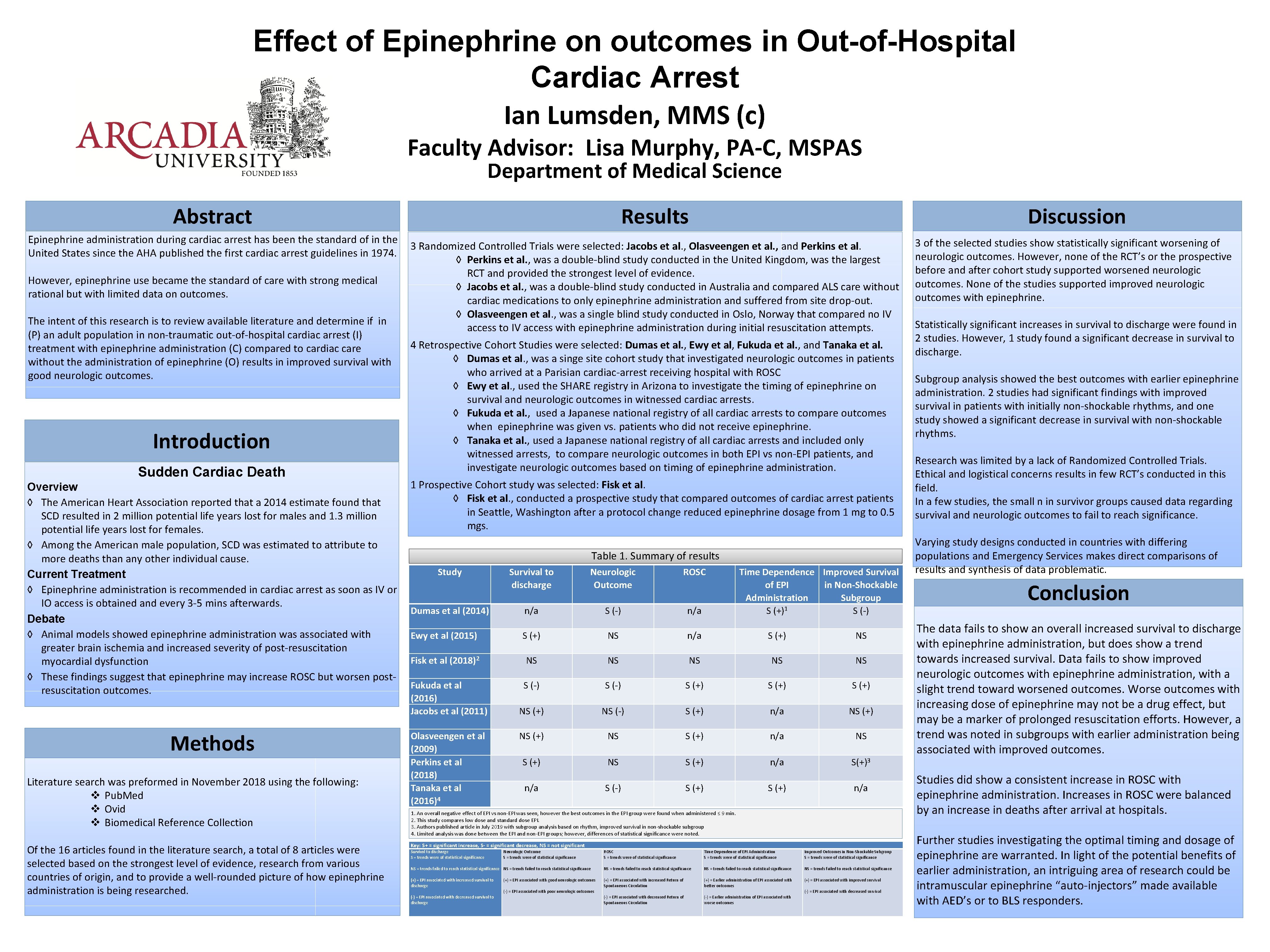
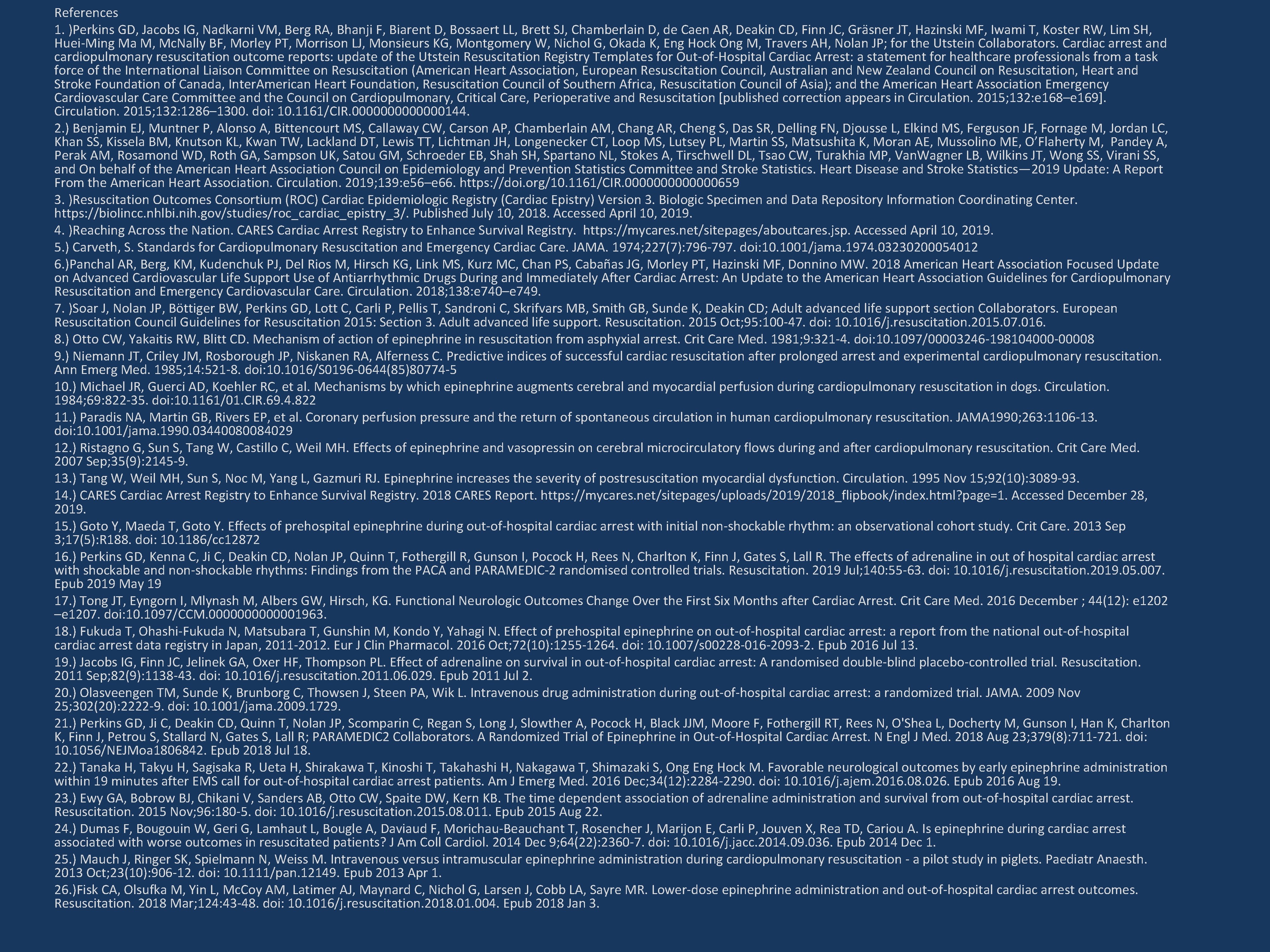
Effect of Epinephrine on outcomes in Out-of-Hospital Cardiac Arrest Ian Lumsden, MMS (c) Faculty Advisor: Lisa Murphy, PA-C, MSPAS Department of Medical Science Abstract Epinephrine administration during cardiac arrest has been the standard of in the United States since the AHA published the first cardiac arrest guidelines in 1974. However, epinephrine use became the standard of care with strong medical rational but with limited data on outcomes. The intent of this research is to review available literature and determine if in (P) an adult population in non-traumatic out-of-hospital cardiac arrest (I) treatment with epinephrine administration (C) compared to cardiac care without the administration of epinephrine (O) results in improved survival with good neurologic outcomes. Introduction Sudden Cardiac Death Overview ◊ The American Heart Association reported that a 2014 estimate found that SCD resulted in 2 million potential life years lost for males and 1. 3 million potential life years lost for females. ◊ Among the American male population, SCD was estimated to attribute to more deaths than any other individual cause. Current Treatment ◊ Epinephrine administration is recommended in cardiac arrest as soon as IV or IO access is obtained and every 3 -5 mins afterwards. Debate ◊ Animal models showed epinephrine administration was associated with greater brain ischemia and increased severity of post-resuscitation myocardial dysfunction ◊ These findings suggest that epinephrine may increase ROSC but worsen postresuscitation outcomes. Methods Literature search was preformed in November 2018 using the following: v Pub. Med v Ovid v Biomedical Reference Collection Of the 16 articles found in the literature search, a total of 8 articles were selected based on the strongest level of evidence, research from various countries of origin, and to provide a well-rounded picture of how epinephrine administration is being researched. Results Discussion 3 Randomized Controlled Trials were selected: Jacobs et al. , Olasveengen et al. , and Perkins et al. ◊ Perkins et al. , was a double-blind study conducted in the United Kingdom, was the largest RCT and provided the strongest level of evidence. ◊ Jacobs et al. , was a double-blind study conducted in Australia and compared ALS care without cardiac medications to only epinephrine administration and suffered from site drop-out. ◊ Olasveengen et al. , was a single blind study conducted in Oslo, Norway that compared no IV access to IV access with epinephrine administration during initial resuscitation attempts. 4 Retrospective Cohort Studies were selected: Dumas et al. , Ewy et al, Fukuda et al. , and Tanaka et al. ◊ Dumas et al. , was a singe site cohort study that investigated neurologic outcomes in patients who arrived at a Parisian cardiac-arrest receiving hospital with ROSC ◊ Ewy et al. , used the SHARE registry in Arizona to investigate the timing of epinephrine on survival and neurologic outcomes in witnessed cardiac arrests. ◊ Fukuda et al. , used a Japanese national registry of all cardiac arrests to compare outcomes when epinephrine was given vs. patients who did not receive epinephrine. ◊ Tanaka et al. , used a Japanese national registry of all cardiac arrests and included only witnessed arrests, to compare neurologic outcomes in both EPI vs non-EPI patients, and investigate neurologic outcomes based on timing of epinephrine administration. 1 Prospective Cohort study was selected: Fisk et al. ◊ Fisk et al. , conducted a prospective study that compared outcomes of cardiac arrest patients in Seattle, Washington after a protocol change reduced epinephrine dosage from 1 mg to 0. 5 mgs. Table 1. Summary of results Study Dumas et al (2014) Survival to discharge Neurologic Outcome ROSC n/a S (-) n/a Time Dependence Improved Survival of EPI in Non-Shockable Administration Subgroup S (+)1 S (-) Ewy et al (2015) S (+) NS n/a S (+) NS Fisk et al (2018)2 NS NS NS Fukuda et al (2016) Jacobs et al (2011) S (-) S (+) NS (-) S (+) n/a NS (+) NS S (+) n/a S(+)3 Olasveengen et al (2009) Perkins et al (2018) Tanaka et al (2016)4 n/a S (-) S (+) n/a 1. An overall negative effect of EPI vs non-EPI was seen, however the best outcomes in the EPI group were found when administered ≤ 9 min. 2. This study compares low dose and standard dose EPI. 3. Authors published article in July 2019 with subgroup analysis based on rhythm, improved survival in non-shockable subgroup 4. Limited analysis was done between the EPI and non-EPI groups; however, differences of statistical significance were noted. Key: S+ = significant increase, S- = significant decrease, NS = not significant Survival to discharge S = trends were of statistical significance Neurologic Outcome S = trends were of statistical significance ROSC S = trends were of statistical significance Time Dependence of EPI Administration S = trends were of statistical significance Improved Outcomes in Non-Shockable Subgroup S = trends were of statistical significance NS = trends failed to reach statistical significance NS = trends failed to reach statistical significance (+) = EPI associated with increased survival to discharge (+) = EPI associated with increased Return of Spontaneous Circulation (+) = Earlier administration of EPI associated with better outcomes (+) = EPI associated with improved survival (+) = EPI associated with good neurologic outcomes (-) = EPI associated with poor neurologic outcomes (-) = EPI associated with decreased survival to discharge (-) = EPI associated with decreased survival (-) = EPI associated with decreased Return of Spontaneous Circulation (-) = Earlier administration of EPI associated with worse outcomes 3 of the selected studies show statistically significant worsening of neurologic outcomes. However, none of the RCT’s or the prospective before and after cohort study supported worsened neurologic outcomes. None of the studies supported improved neurologic outcomes with epinephrine. Statistically significant increases in survival to discharge were found in 2 studies. However, 1 study found a significant decrease in survival to discharge. Subgroup analysis showed the best outcomes with earlier epinephrine administration. 2 studies had significant findings with improved survival in patients with initially non-shockable rhythms, and one study showed a significant decrease in survival with non-shockable rhythms. Research was limited by a lack of Randomized Controlled Trials. Ethical and logistical concerns results in few RCT’s conducted in this field. In a few studies, the small n in survivor groups caused data regarding survival and neurologic outcomes to fail to reach significance. Varying study designs conducted in countries with differing populations and Emergency Services makes direct comparisons of results and synthesis of data problematic. Conclusion The data fails to show an overall increased survival to discharge with epinephrine administration, but does show a trend towards increased survival. Data fails to show improved neurologic outcomes with epinephrine administration, with a slight trend toward worsened outcomes. Worse outcomes with increasing dose of epinephrine may not be a drug effect, but may be a marker of prolonged resuscitation efforts. However, a trend was noted in subgroups with earlier administration being associated with improved outcomes. Studies did show a consistent increase in ROSC with epinephrine administration. Increases in ROSC were balanced by an increase in deaths after arrival at hospitals. Further studies investigating the optimal timing and dosage of epinephrine are warranted. In light of the potential benefits of earlier administration, an intriguing area of research could be intramuscular epinephrine “auto-injectors” made available with AED’s or to BLS responders.


References 1. )Perkins GD, Jacobs IG, Nadkarni VM, Berg RA, Bhanji F, Biarent D, Bossaert LL, Brett SJ, Chamberlain D, de Caen AR, Deakin CD, Finn JC, Gräsner JT, Hazinski MF, Iwami T, Koster RW, Lim SH, Huei-Ming Ma M, Mc. Nally BF, Morley PT, Morrison LJ, Monsieurs KG, Montgomery W, Nichol G, Okada K, Eng Hock Ong M, Travers AH, Nolan JP; for the Utstein Collaborators. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein Resuscitation Registry Templates for Out-of-Hospital Cardiac Arrest: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, Inter. American Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation [published correction appears in Circulation. 2015; 132: e 168–e 169]. Circulation. 2015; 132: 1286– 1300. doi: 10. 1161/CIR. 0000000144. 2. ) Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Das SR, Delling FN, Djousse L, Elkind MS, Ferguson JF, Fornage M, Jordan LC, Khan SS, Kissela BM, Knutson KL, Kwan TW, Lackland DT, Lewis TT, Lichtman JH, Longenecker CT, Loop MS, Lutsey PL, Martin SS, Matsushita K, Moran AE, Mussolino ME, O’Flaherty M, Pandey A, Perak AM, Rosamond WD, Roth GA, Sampson UK, Satou GM, Schroeder EB, Shah SH, Spartano NL, Stokes A, Tirschwell DL, Tsao CW, Turakhia MP, Van. Wagner LB, Wilkins JT, Wong SS, Virani SS, and On behalf of the American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics. Heart Disease and Stroke Statistics— 2019 Update: A Report From the American Heart Association. Circulation. 2019; 139: e 56–e 66. https: //doi. org/10. 1161/CIR. 0000000659 3. )Resuscitation Outcomes Consortium (ROC) Cardiac Epidemiologic Registry (Cardiac Epistry) Version 3. Biologic Specimen and Data Repository Information Coordinating Center. https: //biolincc. nhlbi. nih. gov/studies/roc_cardiac_epistry_3/. Published July 10, 2018. Accessed April 10, 2019. 4. )Reaching Across the Nation. CARES Cardiac Arrest Registry to Enhance Survival Registry. https: //mycares. net/sitepages/aboutcares. jsp. Accessed April 10, 2019. 5. ) Carveth, S. Standards for Cardiopulmonary Resuscitation and Emergency Cardiac Care. JAMA. 1974; 227(7): 796 -797. doi: 10. 1001/jama. 1974. 03230200054012 6. )Panchal AR, Berg, KM, Kudenchuk PJ, Del Rios M, Hirsch KG, Link MS, Kurz MC, Chan PS, Cabañas JG, Morley PT, Hazinski MF, Donnino MW. 2018 American Heart Association Focused Update on Advanced Cardiovascular Life Support Use of Antiarrhythmic Drugs During and Immediately After Cardiac Arrest: An Update to the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2018; 138: e 740–e 749. 7. )Soar J, Nolan JP, Böttiger BW, Perkins GD, Lott C, Carli P, Pellis T, Sandroni C, Skrifvars MB, Smith GB, Sunde K, Deakin CD; Adult advanced life support section Collaborators. European Resuscitation Council Guidelines for Resuscitation 2015: Section 3. Adult advanced life support. Resuscitation. 2015 Oct; 95: 100 -47. doi: 10. 1016/j. resuscitation. 2015. 07. 016. 8. ) Otto CW, Yakaitis RW, Blitt CD. Mechanism of action of epinephrine in resuscitation from asphyxial arrest. Crit Care Med. 1981; 9: 321 -4. doi: 10. 1097/00003246 -198104000 -00008 9. ) Niemann JT, Criley JM, Rosborough JP, Niskanen RA, Alferness C. Predictive indices of successful cardiac resuscitation after prolonged arrest and experimental cardiopulmonary resuscitation. Ann Emerg Med. 1985; 14: 521 -8. doi: 10. 1016/S 0196 -0644(85)80774 -5 10. ) Michael JR, Guerci AD, Koehler RC, et al. Mechanisms by which epinephrine augments cerebral and myocardial perfusion during cardiopulmonary resuscitation in dogs. Circulation. 1984; 69: 822 -35. doi: 10. 1161/01. CIR. 69. 4. 822 11. ) Paradis NA, Martin GB, Rivers EP, et al. Coronary perfusion pressure and the return of spontaneous circulation in human cardiopulmonary resuscitation. JAMA 1990; 263: 1106 -13. doi: 10. 1001/jama. 1990. 03440080084029 12. ) Ristagno G, Sun S, Tang W, Castillo C, Weil MH. Effects of epinephrine and vasopressin on cerebral microcirculatory flows during and after cardiopulmonary resuscitation. Crit Care Med. 2007 Sep; 35(9): 2145 -9. 13. ) Tang W, Weil MH, Sun S, Noc M, Yang L, Gazmuri RJ. Epinephrine increases the severity of postresuscitation myocardial dysfunction. Circulation. 1995 Nov 15; 92(10): 3089 -93. 14. ) CARES Cardiac Arrest Registry to Enhance Survival Registry. 2018 CARES Report. https: //mycares. net/sitepages/uploads/2019/2018_flipbook/index. html? page=1. Accessed December 28, 2019. 15. ) Goto Y, Maeda T, Goto Y. Effects of prehospital epinephrine during out-of-hospital cardiac arrest with initial non-shockable rhythm: an observational cohort study. Crit Care. 2013 Sep 3; 17(5): R 188. doi: 10. 1186/cc 12872 16. ) Perkins GD, Kenna C, Ji C, Deakin CD, Nolan JP, Quinn T, Fothergill R, Gunson I, Pocock H, Rees N, Charlton K, Finn J, Gates S, Lall R. The effects of adrenaline in out of hospital cardiac arrest with shockable and non-shockable rhythms: Findings from the PACA and PARAMEDIC-2 randomised controlled trials. Resuscitation. 2019 Jul; 140: 55 -63. doi: 10. 1016/j. resuscitation. 2019. 05. 007. Epub 2019 May 19 17. ) Tong JT, Eyngorn I, Mlynash M, Albers GW, Hirsch, KG. Functional Neurologic Outcomes Change Over the First Six Months after Cardiac Arrest. Crit Care Med. 2016 December ; 44(12): e 1202 –e 1207. doi: 10. 1097/CCM. 0000001963. 18. ) Fukuda T, Ohashi-Fukuda N, Matsubara T, Gunshin M, Kondo Y, Yahagi N. Effect of prehospital epinephrine on out-of-hospital cardiac arrest: a report from the national out-of-hospital cardiac arrest data registry in Japan, 2011 -2012. Eur J Clin Pharmacol. 2016 Oct; 72(10): 1255 -1264. doi: 10. 1007/s 00228 -016 -2093 -2. Epub 2016 Jul 13. 19. ) Jacobs IG, Finn JC, Jelinek GA, Oxer HF, Thompson PL. Effect of adrenaline on survival in out-of-hospital cardiac arrest: A randomised double-blind placebo-controlled trial. Resuscitation. 2011 Sep; 82(9): 1138 -43. doi: 10. 1016/j. resuscitation. 2011. 06. 029. Epub 2011 Jul 2. 20. ) Olasveengen TM, Sunde K, Brunborg C, Thowsen J, Steen PA, Wik L. Intravenous drug administration during out-of-hospital cardiac arrest: a randomized trial. JAMA. 2009 Nov 25; 302(20): 2222 -9. doi: 10. 1001/jama. 2009. 1729. 21. ) Perkins GD, Ji C, Deakin CD, Quinn T, Nolan JP, Scomparin C, Regan S, Long J, Slowther A, Pocock H, Black JJM, Moore F, Fothergill RT, Rees N, O'Shea L, Docherty M, Gunson I, Han K, Charlton K, Finn J, Petrou S, Stallard N, Gates S, Lall R; PARAMEDIC 2 Collaborators. A Randomized Trial of Epinephrine in Out-of-Hospital Cardiac Arrest. N Engl J Med. 2018 Aug 23; 379(8): 711 -721. doi: 10. 1056/NEJMoa 1806842. Epub 2018 Jul 18. 22. ) Tanaka H, Takyu H, Sagisaka R, Ueta H, Shirakawa T, Kinoshi T, Takahashi H, Nakagawa T, Shimazaki S, Ong Eng Hock M. Favorable neurological outcomes by early epinephrine administration within 19 minutes after EMS call for out-of-hospital cardiac arrest patients. Am J Emerg Med. 2016 Dec; 34(12): 2284 -2290. doi: 10. 1016/j. ajem. 2016. 08. 026. Epub 2016 Aug 19. 23. ) Ewy GA, Bobrow BJ, Chikani V, Sanders AB, Otto CW, Spaite DW, Kern KB. The time dependent association of adrenaline administration and survival from out-of-hospital cardiac arrest. Resuscitation. 2015 Nov; 96: 180 -5. doi: 10. 1016/j. resuscitation. 2015. 08. 011. Epub 2015 Aug 22. 24. ) Dumas F, Bougouin W, Geri G, Lamhaut L, Bougle A, Daviaud F, Morichau-Beauchant T, Rosencher J, Marijon E, Carli P, Jouven X, Rea TD, Cariou A. Is epinephrine during cardiac arrest associated with worse outcomes in resuscitated patients? J Am Coll Cardiol. 2014 Dec 9; 64(22): 2360 -7. doi: 10. 1016/j. jacc. 2014. 09. 036. Epub 2014 Dec 1. 25. ) Mauch J, Ringer SK, Spielmann N, Weiss M. Intravenous versus intramuscular epinephrine administration during cardiopulmonary resuscitation - a pilot study in piglets. Paediatr Anaesth. 2013 Oct; 23(10): 906 -12. doi: 10. 1111/pan. 12149. Epub 2013 Apr 1. 26. )Fisk CA, Olsufka M, Yin L, Mc. Coy AM, Latimer AJ, Maynard C, Nichol G, Larsen J, Cobb LA, Sayre MR. Lower-dose epinephrine administration and out-of-hospital cardiac arrest outcomes. Resuscitation. 2018 Mar; 124: 43 -48. doi: 10. 1016/j. resuscitation. 2018. 01. 004. Epub 2018 Jan 3.