Community Ophthalmology Service Wandsworth Merton LDU and Sutton

- Slides: 6
Community Ophthalmology Service Wandsworth & Merton LDU and Sutton CCG’s September 2018 Steven Nzekwue
Why do we need a Community Ophthalmology Service? • More than 2 million people have reduced vision in the UK and it is estimated that this figure will double by 2050 (RNi. B). • Ophthalmology is the second highest cause of outpatient appointments for any speciality with 7. 1 million attendances in 2014/15 and more than 450, 000 eye related A&E attendances nationally (HSCIC). • Hospital eye services (HES) are overwhelmed. Patients are losing sight because of delayed treatment due to postponed hospital eye service appointments, (Royal College of Ophthalmology). • People are living longer with multiple long term conditions, and the rise in prevalence of people with diabetes also presents an added risk. • There are inequalities in access to services. Our proposal is to deliver eye care services across the borough’s of Merton, Wandsworth and Sutton which is fair and easily accessible. • There is limited community eye care provision in Wandsworth and Merton. Patients are having to attend hospital for treatment which could have been more conveniently and appropriately managed locally in the community, therefore adding cost the system.
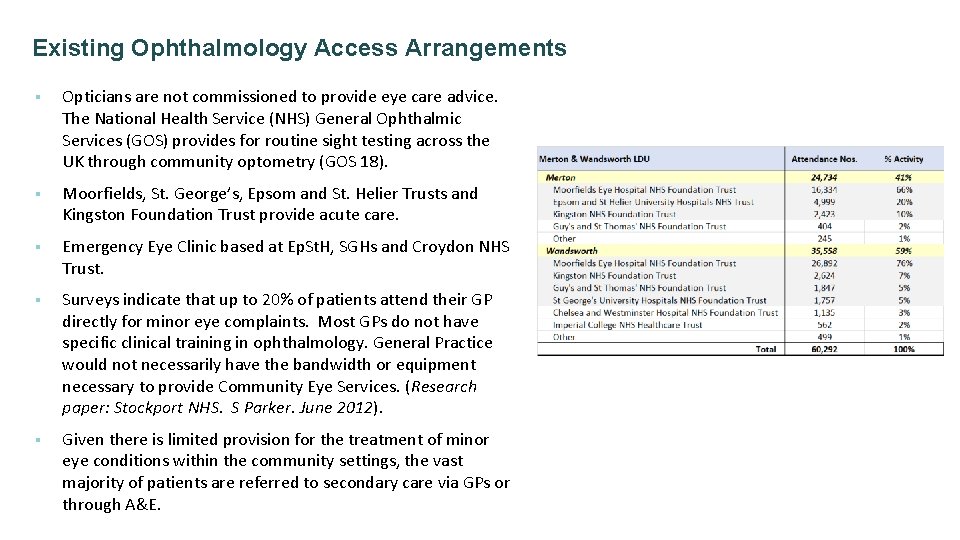
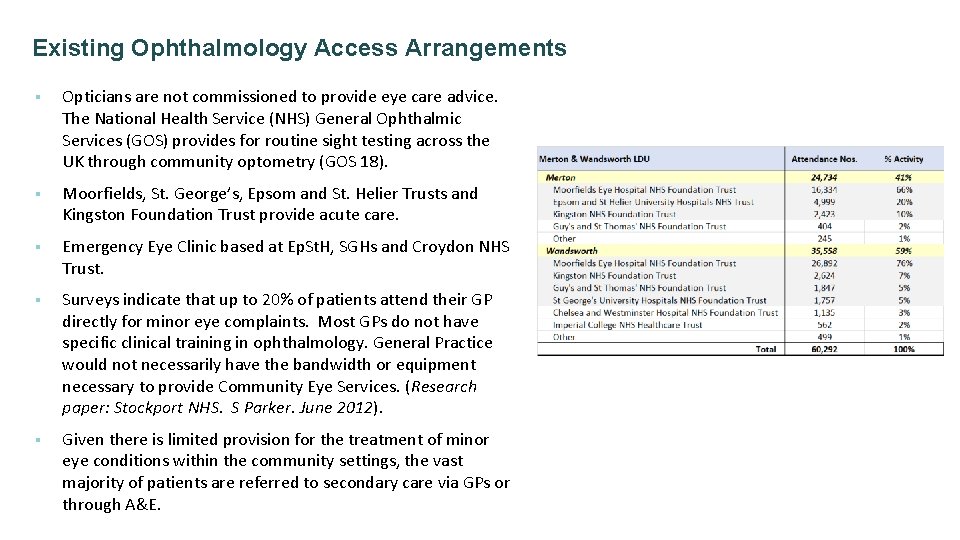
Existing Ophthalmology Access Arrangements § Opticians are not commissioned to provide eye care advice. The National Health Service (NHS) General Ophthalmic Services (GOS) provides for routine sight testing across the UK through community optometry (GOS 18). § Moorfields, St. George’s, Epsom and St. Helier Trusts and Kingston Foundation Trust provide acute care. § Emergency Eye Clinic based at Ep. St. H, SGHs and Croydon NHS Trust. § Surveys indicate that up to 20% of patients attend their GP directly for minor eye complaints. Most GPs do not have specific clinical training in ophthalmology. General Practice would not necessarily have the bandwidth or equipment necessary to provide Community Eye Services. (Research paper: Stockport NHS. S Parker. June 2012). § Given there is limited provision for the treatment of minor eye conditions within the community settings, the vast majority of patients are referred to secondary care via GPs or through A&E.

What is the proposed Community Ophthalmology Service? The scope of ophthalmology service includes the following elements: • • Minor Eye Conditions Service (MECS Cataract pathway to include direct referral from optometrists and provide pre-operative screening. Glaucoma - Intraocular Pressure (IOP) service. Single Point of Access (SPA). Services will be delivered from a easily accessible (potentially high street) sites across both CCGs. This model has worked elsewhere in other CCGs across the country. Locally, it has been particularly successful: • Lambeth, Southwark, Bromley. Minor Eye Services include: • Loss of vision including transient loss. • Ocular pain. • Flashes/floaters. • Systemic disease affecting the eye. • Foreign body removal. • Dry eye. • White eye. • Watery eye. • Differential diagnosis of the red eye. • In-growing eyelashes. • Lumps and bumps in the vicinity of the eye. • Double vision. • Retinal lesions. • Field defects.
Benefits? The new ophthalmology services will mean the following: • § § § • • • Reduced variation in care/post code lottery scenarios by providing easily accessible low level ophthalmology services in central locations across the three CCG geographies. Rapid access to local eye care services. More time for patients to discuss their needs and ask questions. Less travel time, time off work and related costs. Enhanced patient experience. Improved patient choice. Maximises the knowledge and skills of the provider(s) to manage and prioritise patients. Improve primary and community collaborative working; with the provider(s) offering advice and guidance to GPs to patients in their GP Practice. Ensures patients are seen in the most appropriate care setting.
Next Steps • • Canvas patient and public feedback on services. Finalise service model. Procurement proposed to initiate in November, and finalise early in New Year. Services start April. Questions & Feedback? • • Are there any gaps in the service proposals? How can we further engage with patients and members of the public on the services? What/where are the best ways to promote the services in the mobilisation phase? Are there any volunteers to be part of the procurement evaluation process?