ASSESSMENT OF NEW SINGLE PATIENT USE CARDINAL HEALTH
- Slides: 1
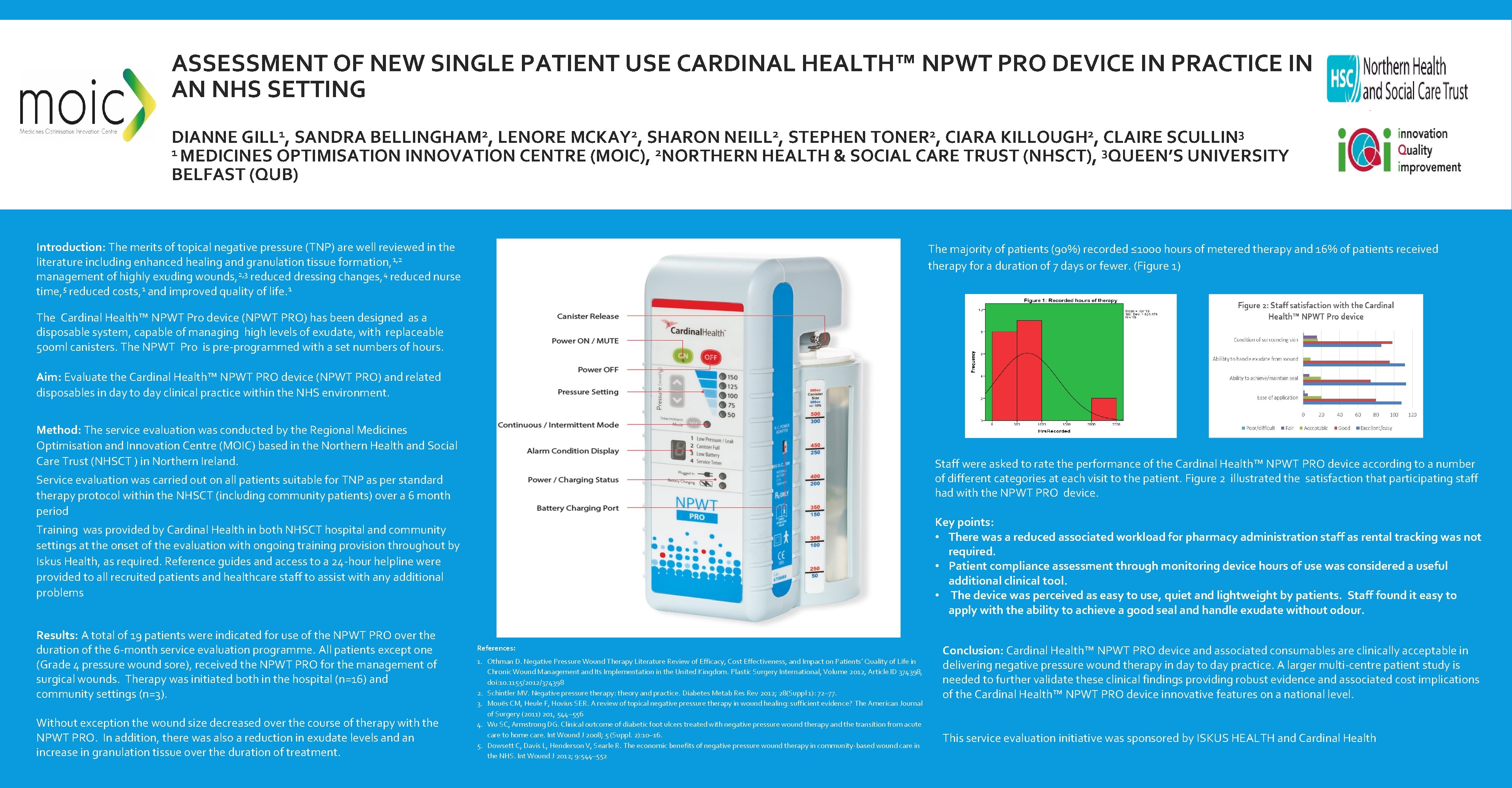
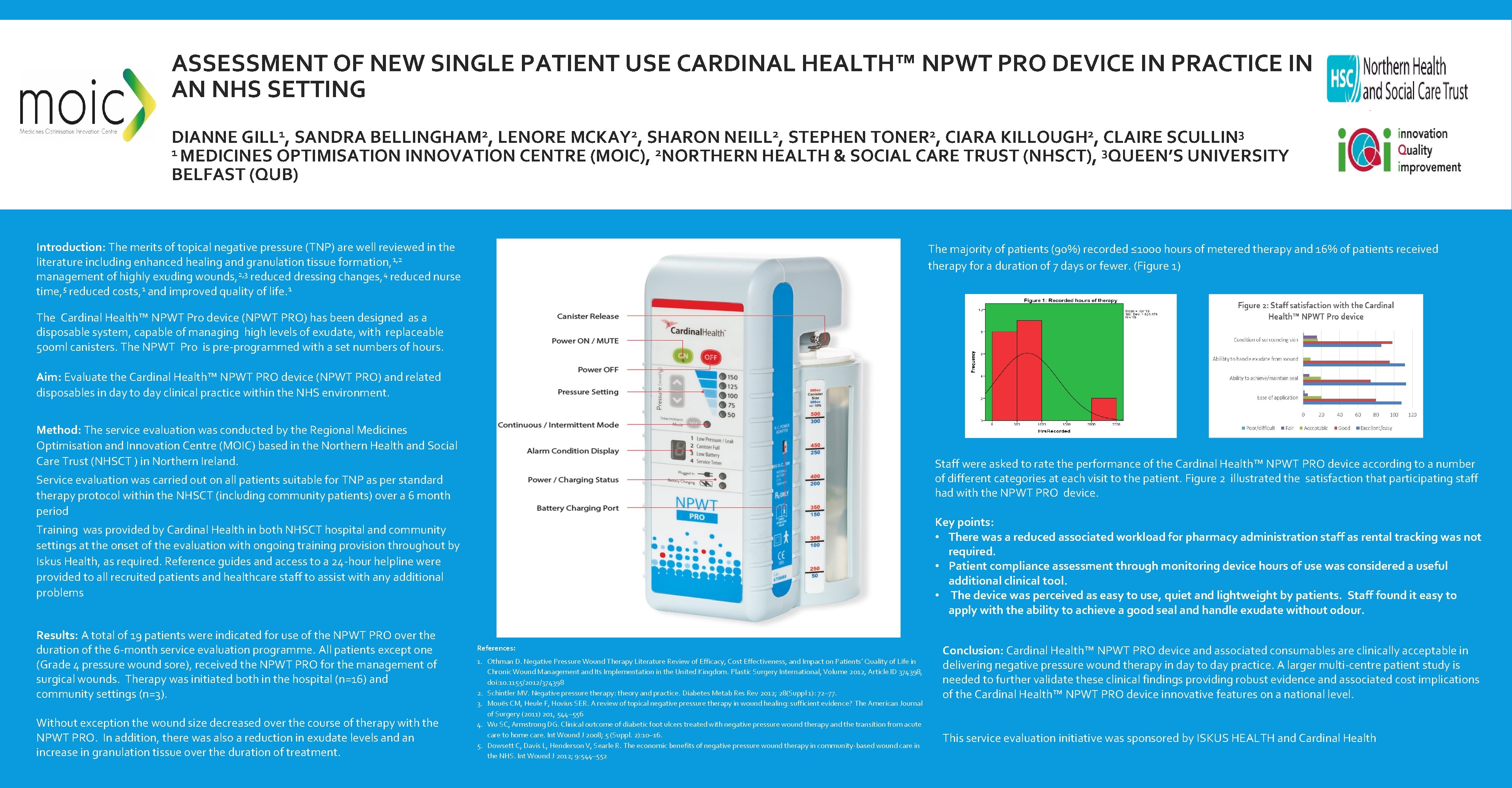
ASSESSMENT OF NEW SINGLE PATIENT USE CARDINAL HEALTH™ NPWT PRO DEVICE IN PRACTICE IN AN NHS SETTING DIANNE GILL 1, SANDRA BELLINGHAM 2, LENORE MCKAY 2, SHARON NEILL 2, STEPHEN TONER 2, CIARA KILLOUGH 2, CLAIRE SCULLIN 3 1 MEDICINES OPTIMISATION INNOVATION CENTRE (MOIC), 2 NORTHERN HEALTH & SOCIAL CARE TRUST (NHSCT), 3 QUEEN’S UNIVERSITY BELFAST (QUB) Introduction: The merits of topical negative pressure (TNP) are well reviewed in the literature including enhanced healing and granulation tissue formation, 1, 2 management of highly exuding wounds, 2, 3 reduced dressing changes, 4 reduced nurse time, 5 reduced costs, 1 and improved quality of life. 1 The majority of patients (90%) recorded ≤ 1000 hours of metered therapy and 16% of patients received therapy for a duration of 7 days or fewer. (Figure 1) The Cardinal Health™ NPWT Pro device (NPWT PRO) has been designed as a disposable system, capable of managing high levels of exudate, with replaceable 500 ml canisters. The NPWT Pro is pre-programmed with a set numbers of hours. Aim: Evaluate the Cardinal Health™ NPWT PRO device (NPWT PRO) and related disposables in day to day clinical practice within the NHS environment. Method: The service evaluation was conducted by the Regional Medicines Optimisation and Innovation Centre (MOIC) based in the Northern Health and Social Care Trust (NHSCT ) in Northern Ireland. Staff were asked to rate the performance of the Cardinal Health™ NPWT PRO device according to a number of different categories at each visit to the patient. Figure 2 illustrated the satisfaction that participating staff had with the NPWT PRO device. Service evaluation was carried out on all patients suitable for TNP as per standard therapy protocol within the NHSCT (including community patients) over a 6 month period Key points: • There was a reduced associated workload for pharmacy administration staff as rental tracking was not required. • Patient compliance assessment through monitoring device hours of use was considered a useful additional clinical tool. • The device was perceived as easy to use, quiet and lightweight by patients. Staff found it easy to apply with the ability to achieve a good seal and handle exudate without odour. Training was provided by Cardinal Health in both NHSCT hospital and community settings at the onset of the evaluation with ongoing training provision throughout by Iskus Health, as required. Reference guides and access to a 24 -hour helpline were provided to all recruited patients and healthcare staff to assist with any additional problems Results: A total of 19 patients were indicated for use of the NPWT PRO over the duration of the 6 -month service evaluation programme. All patients except one (Grade 4 pressure wound sore), received the NPWT PRO for the management of surgical wounds. Therapy was initiated both in the hospital (n=16) and community settings (n=3). Without exception the wound size decreased over the course of therapy with the NPWT PRO. In addition, there was also a reduction in exudate levels and an increase in granulation tissue over the duration of treatment. References: 1. Othman D. Negative Pressure Wound Therapy Literature Review of Efficacy, Cost Effectiveness, and Impact on Patients’ Quality of Life in Chronic Wound Management and Its Implementation in the United Kingdom. Plastic Surgery International, Volume 2012, Article ID 374398, doi: 10. 1155/2012/374398 2. Schintler MV. Negative pressure therapy: theory and practice. Diabetes Metab Res Rev 2012; 28(Suppl 1): 72– 77. 3. Mouës CM, Heule F, Hovius SER. A review of topical negative pressure therapy in wound healing: sufficient evidence? The American Journal of Surgery (2011) 201, 544– 556 4. Wu SC, Armstrong DG. Clinical outcome of diabetic foot ulcers treated with negative pressure wound therapy and the transition from acute care to home care. Int Wound J 2008; 5 (Suppl. 2): 10– 16. 5. Dowsett C, Davis L, Henderson V, Searle R. The economic benefits of negative pressure wound therapy in community-based wound care in the NHS. Int Wound J 2012; 9: 544– 552 Conclusion: Cardinal Health™ NPWT PRO device and associated consumables are clinically acceptable in delivering negative pressure wound therapy in day to day practice. A larger multi-centre patient study is needed to further validate these clinical findings providing robust evidence and associated cost implications of the Cardinal Health™ NPWT PRO device innovative features on a national level. This service evaluation initiative was sponsored by ISKUS HEALTH and Cardinal Health