Analysis of Weight Gain Delivery Outcomes in Asians
- Slides: 1
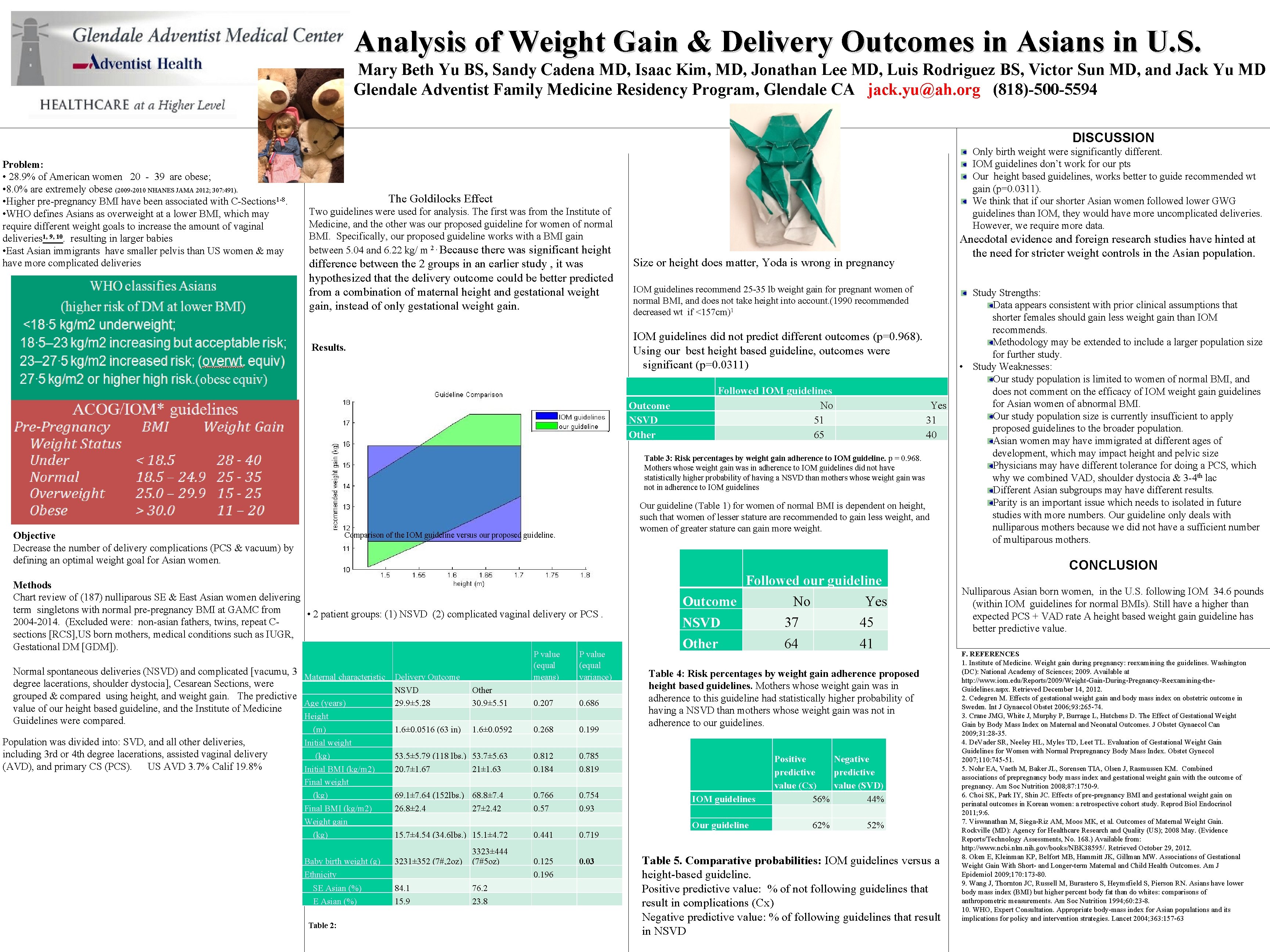
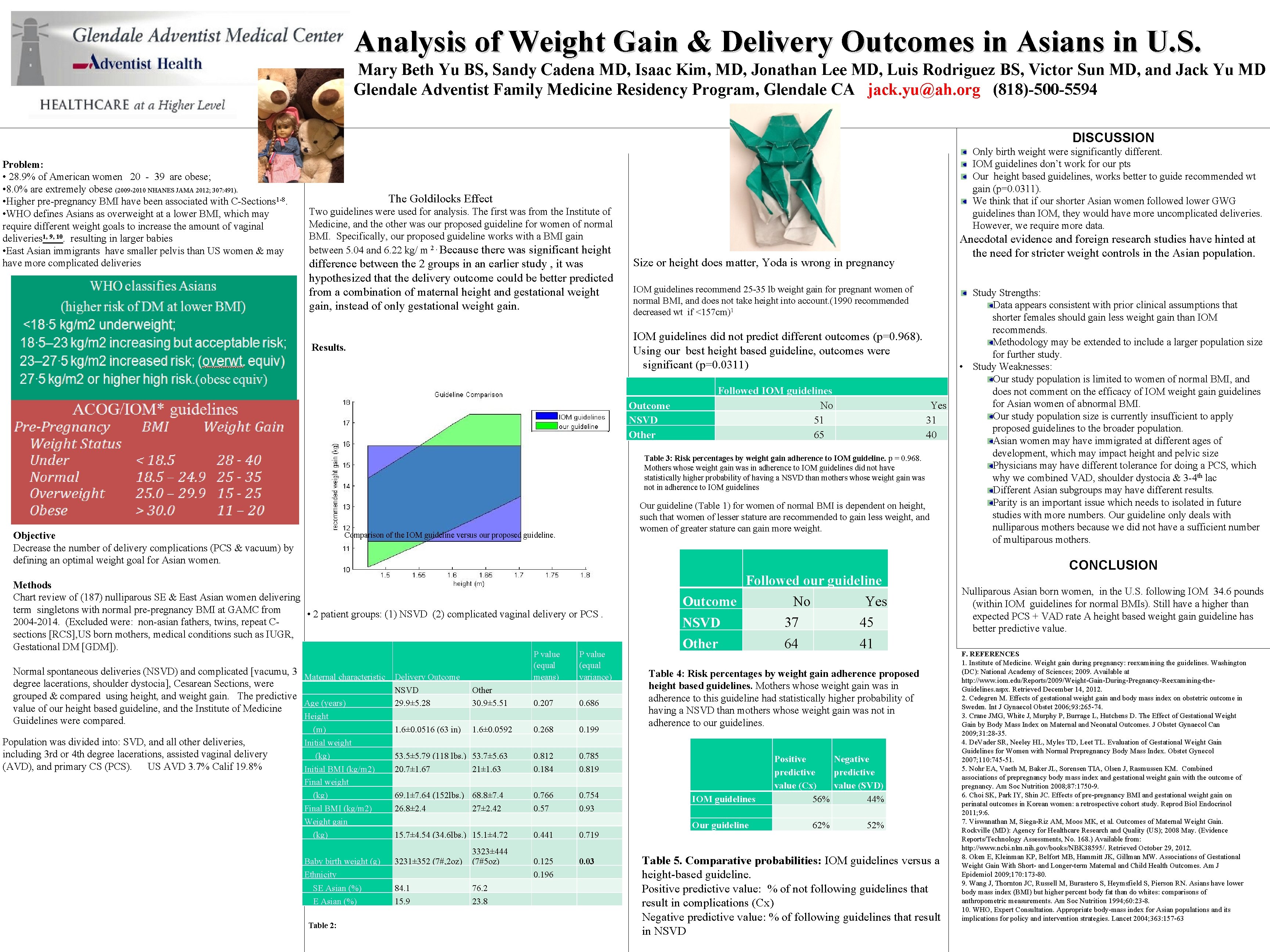
Analysis of Weight Gain & Delivery Outcomes in Asians in U. S. Mary Beth Yu BS, Sandy Cadena MD, Isaac Kim, MD, Jonathan Lee MD, Luis Rodriguez BS, Victor Sun MD, and Jack Yu MD Glendale Adventist Family Medicine Residency Program, Glendale CA jack. yu@ah. org (818)-500 -5594 DISCUSSION Problem: • 28. 9% of American women 20 - 39 are obese; • 8. 0% are extremely obese (2009 -2010 NHANES JAMA 2012; 307: 491). • Higher pre-pregnancy BMI have been associated with C-Sections 1 -8. • WHO defines Asians as overweight at a lower BMI, which may require different weight goals to increase the amount of vaginal deliveries 1, 9, 10. resulting in larger babies • East Asian immigrants have smaller pelvis than US women & may have more complicated deliveries Only birth weight were significantly different. IOM guidelines don’t work for our pts Our height based guidelines, works better to guide recommended wt gain (p=0. 0311). We think that if our shorter Asian women followed lower GWG guidelines than IOM, they would have more uncomplicated deliveries. However, we require more data. The Goldilocks Effect Two guidelines were used for analysis. The first was from the Institute of Medicine, and the other was our proposed guideline for women of normal BMI. Specifically, our proposed guideline works with a BMI gain between 5. 04 and 6. 22 kg/ m 2. Because there was significant height difference between the 2 groups in an earlier study , it was hypothesized that the delivery outcome could be better predicted from a combination of maternal height and gestational weight gain, instead of only gestational weight gain. Size or height does matter, Yoda is wrong in pregnancy IOM guidelines recommend 25 -35 lb weight gain for pregnant women of normal BMI, and does not take height into account. (1990 recommended decreased wt if <157 cm)1 IOM guidelines did not predict different outcomes (p=0. 968). Using our best height based guideline, outcomes were significant (p=0. 0311) Results. Outcome NSVD Other TABLE 1: Proposed guidelines. Based on height differences in Asian women. Objective Decrease the number of delivery complications (PCS & vacuum) by defining an optimal weight goal for Asian women. Comparison of the IOM guideline versus our proposed guideline. Yes 31 40 Table 3: Risk percentages by weight gain adherence to IOM guideline. p = 0. 968. Mothers whose weight gain was in adherence to IOM guidelines did not have statistically higher probability of having a NSVD than mothers whose weight gain was not in adherence to IOM guidelines Study Strengths: Data appears consistent with prior clinical assumptions that shorter females should gain less weight gain than IOM recommends. Methodology may be extended to include a larger population size for further study. • Study Weaknesses: Our study population is limited to women of normal BMI, and does not comment on the efficacy of IOM weight gain guidelines for Asian women of abnormal BMI. Our study population size is currently insufficient to apply proposed guidelines to the broader population. Asian women may have immigrated at different ages of development, which may impact height and pelvic size Physicians may have different tolerance for doing a PCS, which why we combined VAD, shoulder dystocia & 3 -4 th lac Different Asian subgroups may have different results. Parity is an important issue which needs to isolated in future studies with more numbers. Our guideline only deals with nulliparous mothers because we did not have a sufficient number of multiparous mothers. CONCLUSION P value (equal means) P value (equal variance) Other 30. 9± 5. 51 0. 207 0. 686 1. 6± 0. 0592 0. 268 0. 199 53. 5± 5. 79 (118 lbs. ) 53. 7± 5. 63 20. 7± 1. 67 21± 1. 63 0. 812 0. 184 0. 785 0. 819 69. 1± 7. 64 (152 lbs. ) 68. 8± 7. 4 26. 8± 2. 4 27± 2. 42 0. 766 0. 57 0. 754 0. 93 Normal spontaneous deliveries (NSVD) and complicated [vacumu, 3 Maternal characteristic Delivery Outcome degree lacerations, shoulder dystocia], Cesarean Sections, were NSVD grouped & compared using height, and weight gain. The predictive Age (years) 29. 9± 5. 28 value of our height based guideline, and the Institute of Medicine Height Guidelines were compared. (lb) Followed IOM guidelines No 51 65 Our guideline (Table 1) for women of normal BMI is dependent on height, such that women of lesser stature are recommended to gain less weight, and women of greater stature can gain more weight. Methods Chart review of (187) nulliparous SE & East Asian women delivering term singletons with normal pre-pregnancy BMI at GAMC from • 2 patient groups: (1) NSVD (2) complicated vaginal delivery or PCS. 2004 -2014. (Excluded were: non-asian fathers, twins, repeat Csections [RCS], US born mothers, medical conditions such as IUGR, Gestational DM [GDM]). Population was divided into: SVD, and all other deliveries, including 3 rd or 4 th degree lacerations, assisted vaginal delivery (AVD), and primary CS (PCS). US AVD 3. 7% Calif 19. 8% Anecdotal evidence and foreign research studies have hinted at the need for stricter weight controls in the Asian population. (m) Initial weight (kg) Initial BMI (kg/m 2) Final weight (kg) Final BMI (kg/m 2) Weight gain (kg) Baby birth weight (g) Ethnicity SE Asian (%) Table 2: 1. 6± 0. 0516 (63 in) 15. 7± 4. 54 (34. 6 lbs. ) 15. 1± 4. 72 3231± 352 (7#, 2 oz) 3323± 444 (7#5 oz) 84. 1 15. 9 76. 2 23. 8 0. 441 0. 719 0. 125 0. 196 0. 03 Followed our guideline Outcome NSVD Other No 37 Yes 45 64 41 Table 4: Risk percentages by weight gain adherence proposed height based guidelines. Mothers whose weight gain was in adherence to this guideline had statistically higher probability of having a NSVD than mothers whose weight gain was not in adherence to our guidelines. IOM guidelines Our guideline Positive Negative predictive value (Cx) value (SVD) 56% 44% 62% 52% Table 5. Comparative probabilities: IOM guidelines versus a height-based guideline. Positive predictive value: % of not following guidelines that result in complications (Cx) Negative predictive value: % of following guidelines that result in NSVD Nulliparous Asian born women, in the U. S. following IOM 34. 6 pounds (within IOM guidelines for normal BMIs). Still have a higher than expected PCS + VAD rate A height based weight gain guideline has better predictive value. F. REFERENCES 1. Institute of Medicine. Weight gain during pregnancy: reexamining the guidelines. Washington (DC): National Academy of Sciences; 2009. Available at http: //www. iom. edu/Reports/2009/Weight-Gain-During-Pregnancy-Reexamining-the. Guidelines. aspx. Retrieved December 14, 2012. 2. Cedegren M. Effects of gestational weight gain and body mass index on obstetric outcome in Sweden. Int J Gynaecol Obstet 2006; 93: 265 -74. 3. Crane JMG, White J, Murphy P, Burrage L, Hutchens D. The Effect of Gestational Weight Gain by Body Mass Index on Maternal and Neonatal Outcomes. J Obstet Gynaecol Can 2009; 31: 28 -35. 4. De. Vader SR, Neeley HL, Myles TD, Leet TL. Evaluation of Gestational Weight Gain Guidelines for Women with Normal Prepregnancy Body Mass Index. Obstet Gynecol 2007; 110: 745 -51. 5. Nohr EA, Vaeth M, Baker JL, Sorensen TIA, Olsen J, Rasmussen KM. Combined associations of prepregnancy body mass index and gestational weight gain with the outcome of pregnancy. Am Soc Nutrition 2008; 87: 1750 -9. 6. Choi SK, Park IY, Shin JC. Effects of pre-pregnancy BMI and gestational weight gain on perinatal outcomes in Korean women: a retrospective cohort study. Reprod Biol Endocrinol 2011; 9: 6. 7. Viswanathan M, Siega-Riz AM, Moos MK, et al. Outcomes of Maternal Weight Gain. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008 May. (Evidence Reports/Technology Assessments, No. 168. ) Available from: http: //www. ncbi. nlm. nih. gov/books/NBK 38595/. Retrieved October 29, 2012. 8. Oken E, Kleinman KP, Belfort MB, Hammitt JK, Gillman MW. Associations of Gestational Weight Gain With Short- and Longer-term Maternal and Child Health Outcomes. Am J Epidemiol 2009; 170: 173 -80. 9. Wang J, Thornton JC, Russell M, Burastero S, Heymsfield S, Pierson RN. Asians have lower body mass index (BMI) but higher percent body fat than do whites: comparisons of anthropometric measurements. Am Soc Nutrition 1994; 60: 23 -8. 10. WHO, Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004; 363: 157 -63