YOUTH DEPRESSION AND SUICIDE HEATHER DISTIN PCCS LORAIN




- Slides: 24
YOUTH DEPRESSION AND SUICIDE HEATHER DISTIN PCC-S

LORAIN COUNTY From July 2014 - July 2015 Number of Youth assessed by the county Mental Health Crisis Hotline Nord ESS: 889 Number of Youth assessed at Juvenile Court: 78 Number of Youth assessed at School: 53
WHAT IS DEPRESSION? • Mental Health Disorder Classified in the Diagnostic and Statistical Manual of Mental Disorders • Caused by “combination of genetic, biological, environmental, and psychological factors. ”
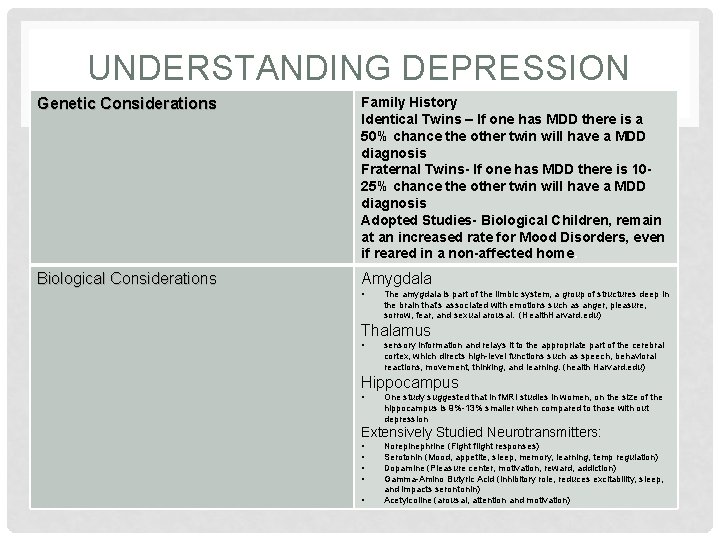
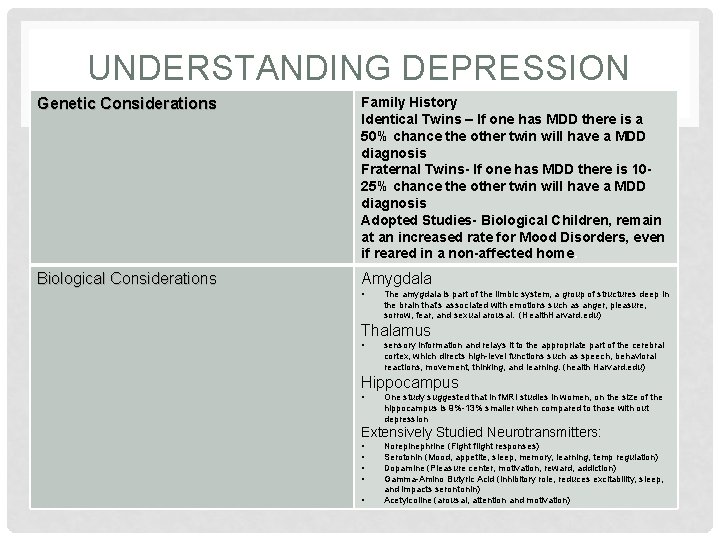
UNDERSTANDING DEPRESSION Genetic Considerations Family History Identical Twins – If one has MDD there is a 50% chance the other twin will have a MDD diagnosis Fraternal Twins- If one has MDD there is 1025% chance the other twin will have a MDD diagnosis Adopted Studies- Biological Children, remain at an increased rate for Mood Disorders, even if reared in a non-affected home. Biological Considerations Amygdala • The amygdala is part of the limbic system, a group of structures deep in the brain that’s associated with emotions such as anger, pleasure, sorrow, fear, and sexual arousal. (Health. Harvard. edu) Thalamus • sensory information and relays it to the appropriate part of the cerebral cortex, which directs high-level functions such as speech, behavioral reactions, movement, thinking, and learning. (health Harvard. edu) Hippocampus • One study suggested that in f. MRI studies in women, on the size of the hippocampus is 9%-13% smaller when compared to those with out depression Extensively Studied Neurotransmitters: • • • Norepinephrine (Fight flight responses) Serotonin (Mood, appetite, sleep, memory, learning, temp regulation) Dopamine (Pleasure center, motivation, reward, addiction) Gamma-Amino Butyric Acid (inhibitory role, reduces excitability, sleep, and impacts serontonin) Acetylcoline (arousal, attention and motivation)
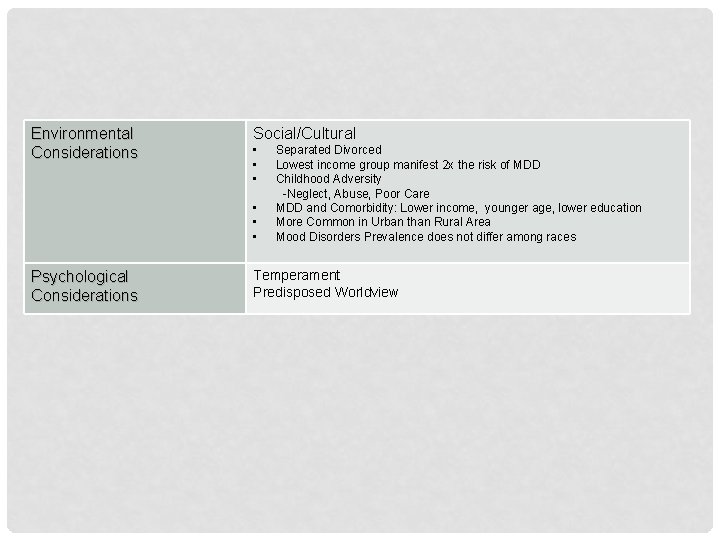
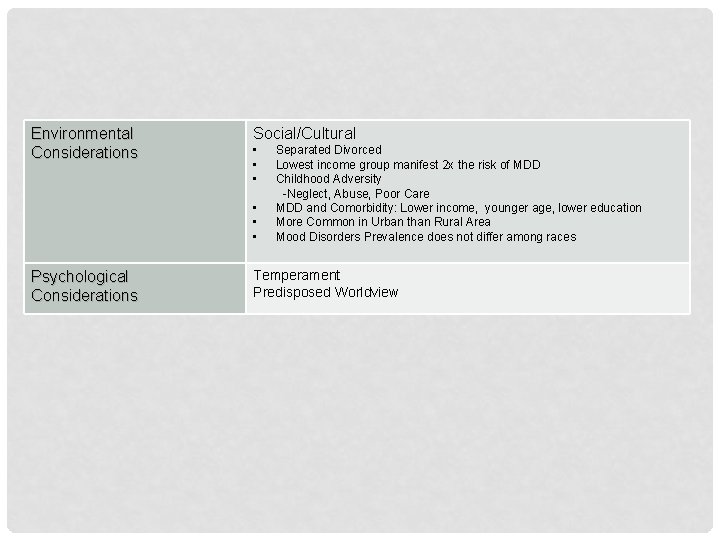
Environmental Considerations Social/Cultural • • • Psychological Considerations Separated Divorced Lowest income group manifest 2 x the risk of MDD Childhood Adversity -Neglect, Abuse, Poor Care MDD and Comorbidity: Lower income, younger age, lower education More Common in Urban than Rural Area Mood Disorders Prevalence does not differ among races Temperament Predisposed Worldview
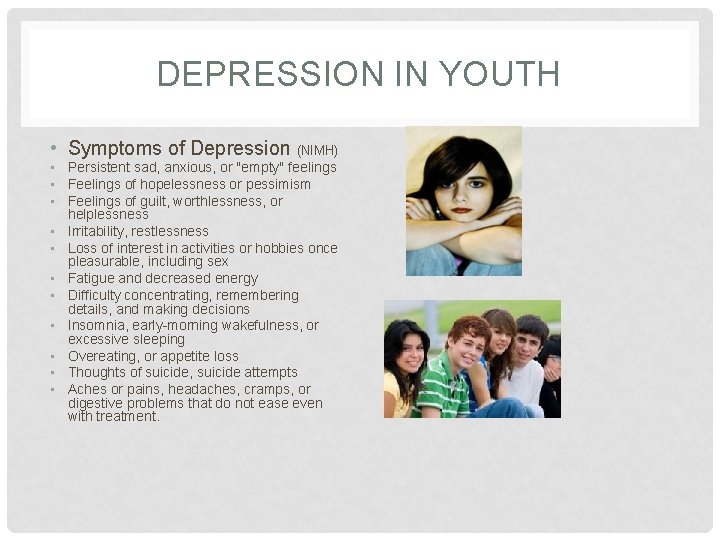
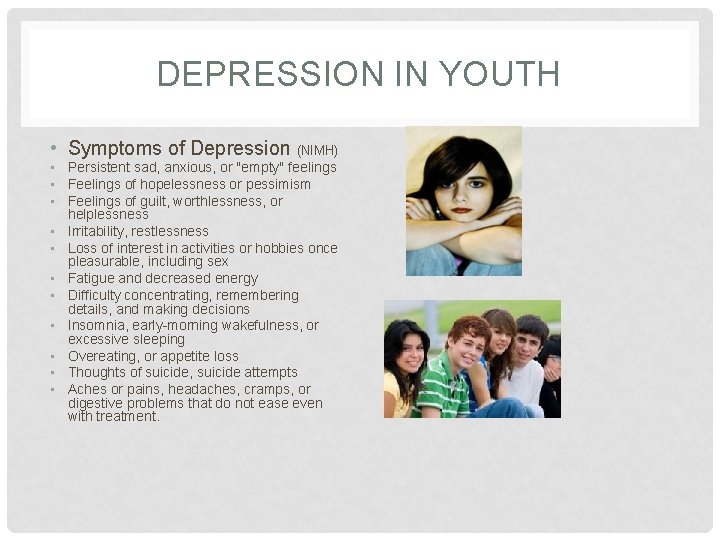
DEPRESSION IN YOUTH • Symptoms of Depression (NIMH) • Persistent sad, anxious, or "empty" feelings • Feelings of hopelessness or pessimism • Feelings of guilt, worthlessness, or helplessness • Irritability, restlessness • Loss of interest in activities or hobbies once pleasurable, including sex • Fatigue and decreased energy • Difficulty concentrating, remembering details, and making decisions • Insomnia, early-morning wakefulness, or excessive sleeping • Overeating, or appetite loss • Thoughts of suicide, suicide attempts • Aches or pains, headaches, cramps, or digestive problems that do not ease even with treatment.
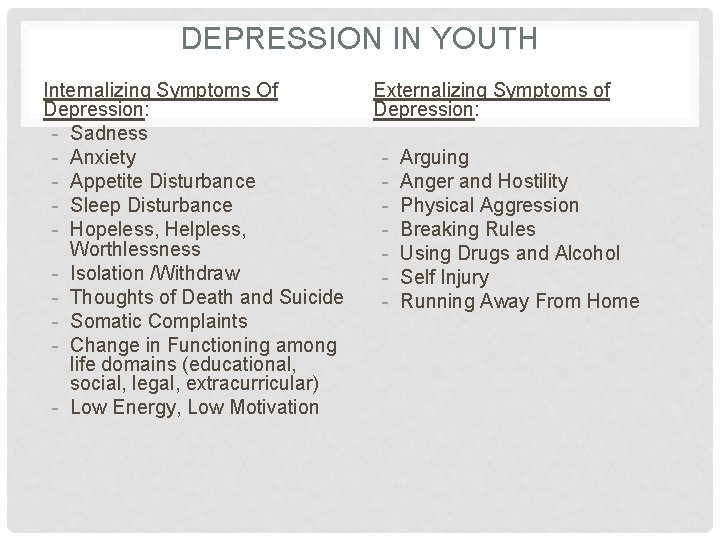
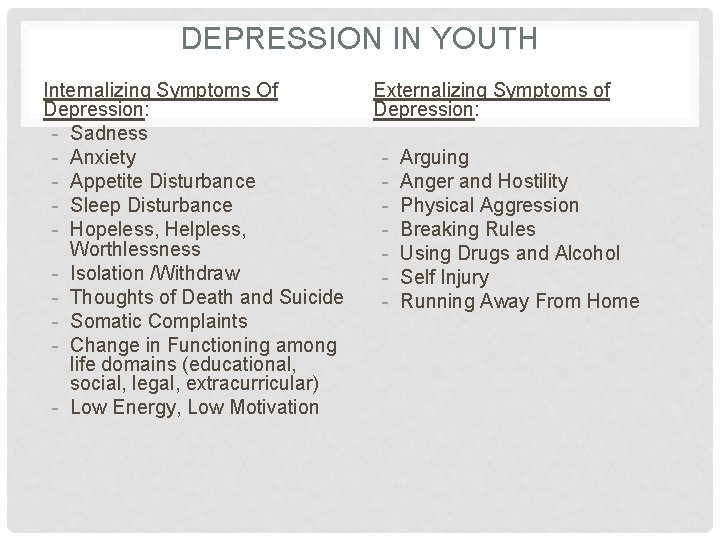
DEPRESSION IN YOUTH Internalizing Symptoms Of Depression: - Sadness - Anxiety - Appetite Disturbance - Sleep Disturbance - Hopeless, Helpless, Worthlessness - Isolation /Withdraw - Thoughts of Death and Suicide - Somatic Complaints - Change in Functioning among life domains (educational, social, legal, extracurricular) - Low Energy, Low Motivation Externalizing Symptoms of Depression: - Arguing Anger and Hostility Physical Aggression Breaking Rules Using Drugs and Alcohol Self Injury Running Away From Home
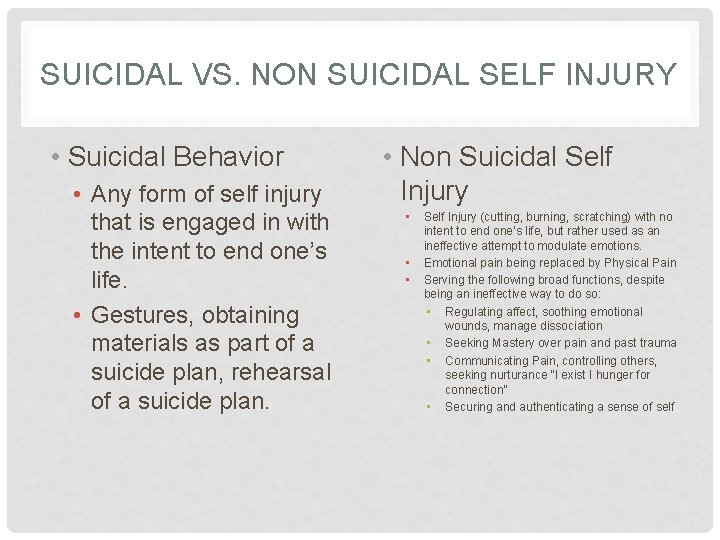
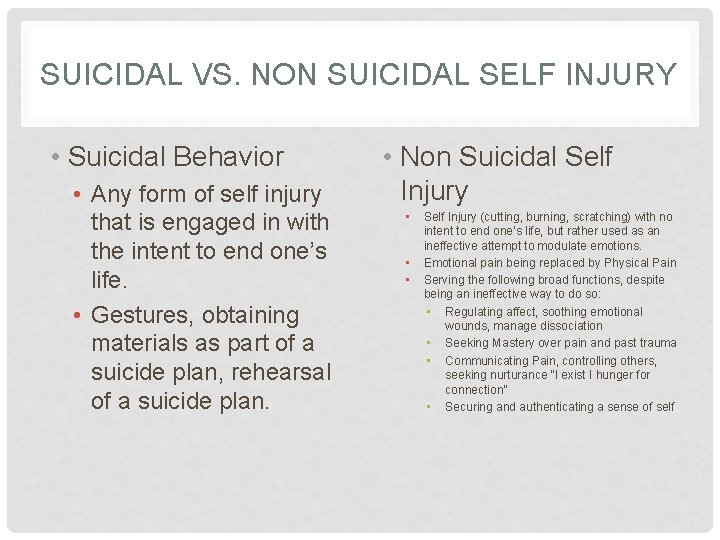
SUICIDAL VS. NON SUICIDAL SELF INJURY • Suicidal Behavior • Any form of self injury that is engaged in with the intent to end one’s life. • Gestures, obtaining materials as part of a suicide plan, rehearsal of a suicide plan. • Non Suicidal Self Injury • • • Self Injury (cutting, burning, scratching) with no intent to end one’s life, but rather used as an ineffective attempt to modulate emotions. Emotional pain being replaced by Physical Pain Serving the following broad functions, despite being an ineffective way to do so: • Regulating affect, soothing emotional wounds, manage dissociation • Seeking Mastery over pain and past trauma • Communicating Pain, controlling others, seeking nurturance “I exist I hunger for connection” • Securing and authenticating a sense of self

CO-MORBIDITY OF DEPRESSION AND OTHER MENTAL HEALTH ISSUES • Diagnoses that are often Co-Morbid with Depression include • • • Post Traumatic Stress Disorder Generalized Anxiety Disorder Conduct Disorder Oppositional Defiant Disorder Alcohol and Drug Use • Depression is a significant risk factor for suicide; therefore, lessening the number of individuals with depression should result in decreasing suicide. A study from the island of Gotland, Sweden, found that when primary care physicians were trained to identify and treat depression in their patients, the suicide rate of islanders went down (Rihmer, Rutz, & Pihlgren, 1995)
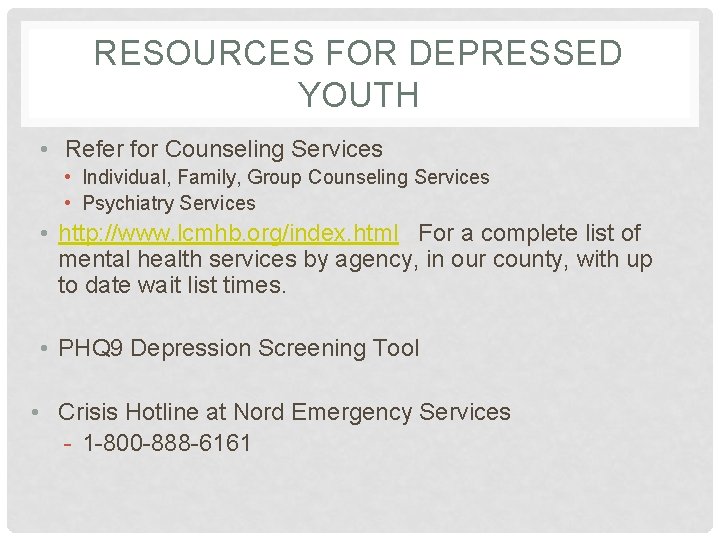
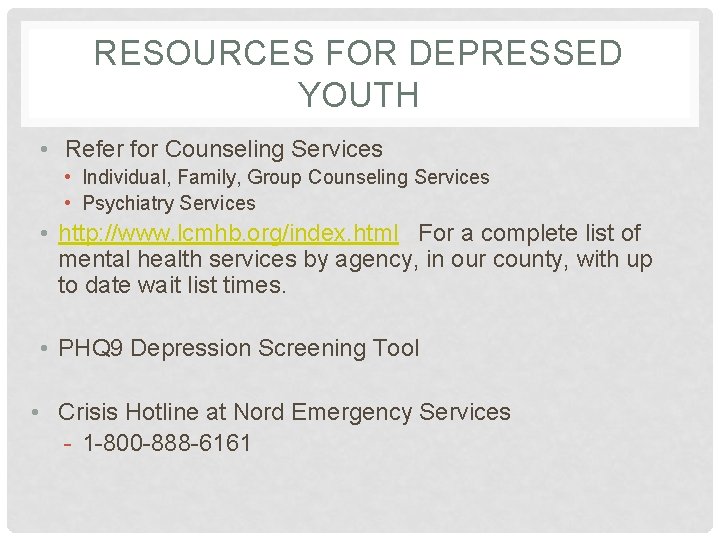
RESOURCES FOR DEPRESSED YOUTH • Refer for Counseling Services • Individual, Family, Group Counseling Services • Psychiatry Services • http: //www. lcmhb. org/index. html For a complete list of mental health services by agency, in our county, with up to date wait list times. • PHQ 9 Depression Screening Tool • Crisis Hotline at Nord Emergency Services - 1 -800 -888 -6161
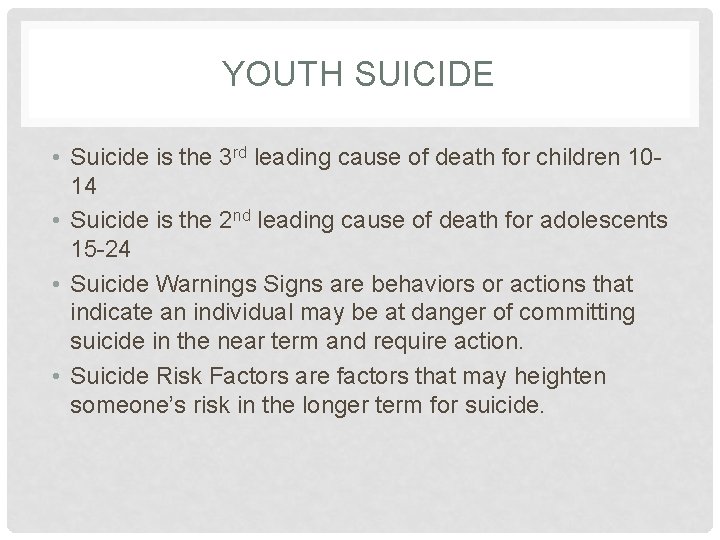
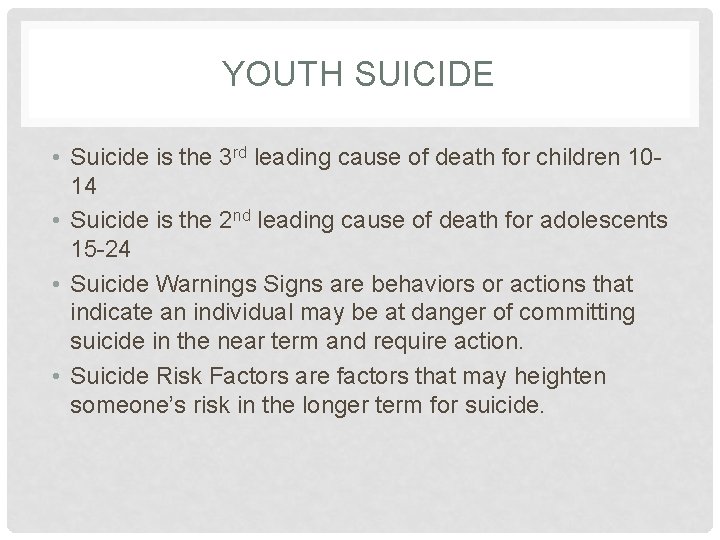
YOUTH SUICIDE • Suicide is the 3 rd leading cause of death for children 1014 • Suicide is the 2 nd leading cause of death for adolescents 15 -24 • Suicide Warnings Signs are behaviors or actions that indicate an individual may be at danger of committing suicide in the near term and require action. • Suicide Risk Factors are factors that may heighten someone’s risk in the longer term for suicide.

WARNING SIGNS FOR SUICIDE (HTTP: //WWW. SPRC. ORG/BPR/SECTION-II/WARNING-SIGNS-SUICIDE-PREVENTION) • Someone threatening to hurt or kill themselves • Someone looking for ways to kill themselves: seeking access to pills, weapons, or other means • Someone talking or writing about death, dying, or suicide • Crisis Hotline at Nord Emergency Services - 1 -800 -888 -6161
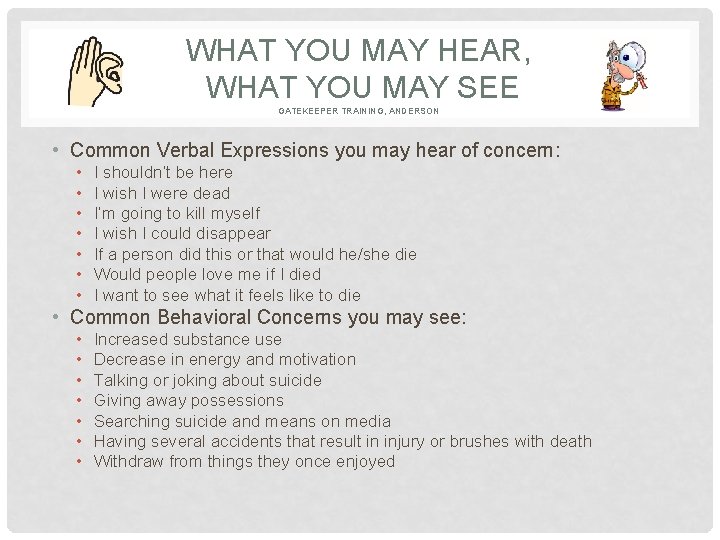
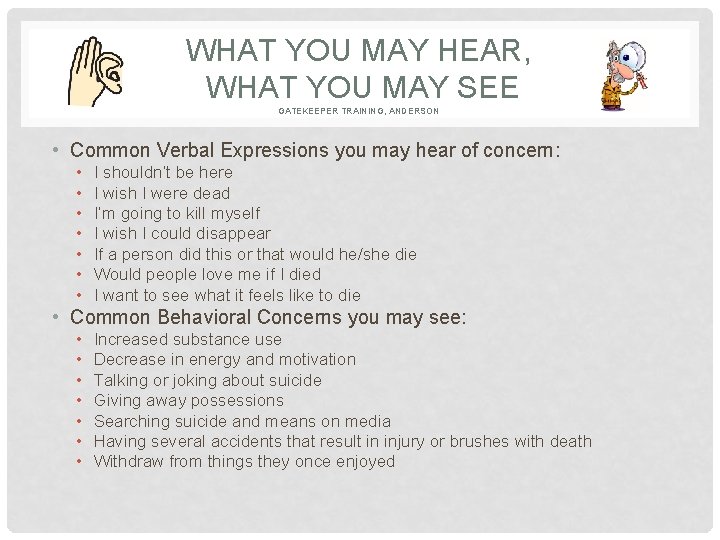
WHAT YOU MAY HEAR, WHAT YOU MAY SEE GATEKEEPER TRAINING, ANDERSON • Common Verbal Expressions you may hear of concern: • • I shouldn’t be here I wish I were dead I’m going to kill myself I wish I could disappear If a person did this or that would he/she die Would people love me if I died I want to see what it feels like to die • Common Behavioral Concerns you may see: • • Increased substance use Decrease in energy and motivation Talking or joking about suicide Giving away possessions Searching suicide and means on media Having several accidents that result in injury or brushes with death Withdraw from things they once enjoyed
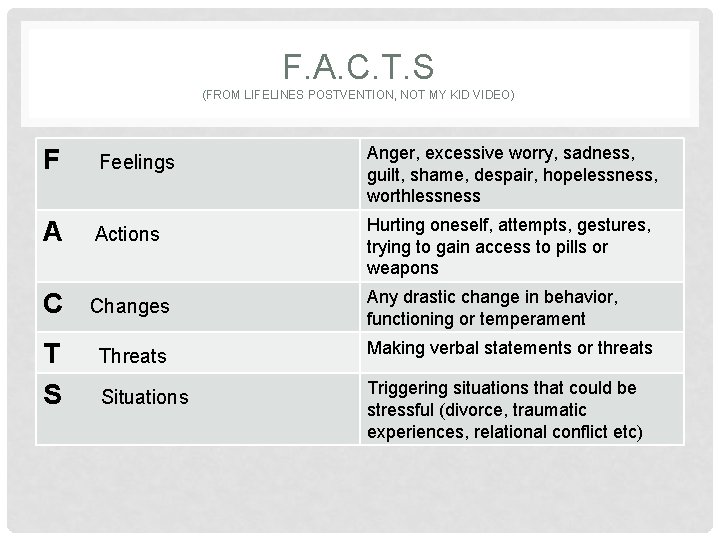
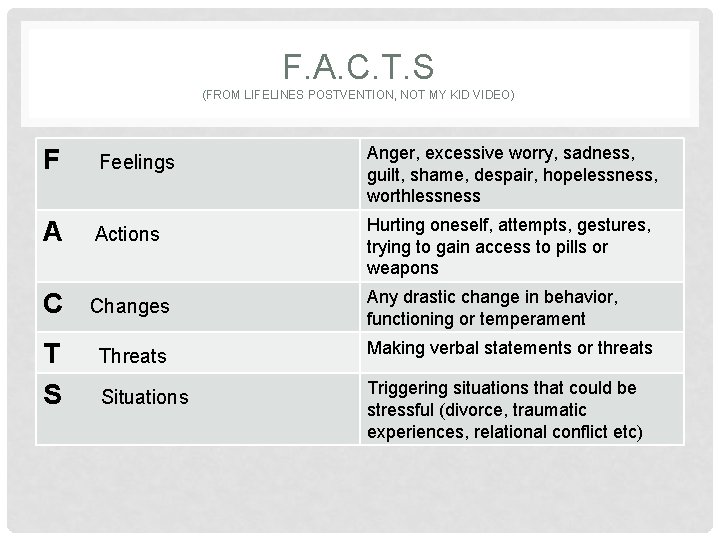
F. A. C. T. S (FROM LIFELINES POSTVENTION, NOT MY KID VIDEO) F Feelings Anger, excessive worry, sadness, guilt, shame, despair, hopelessness, worthlessness A Actions Hurting oneself, attempts, gestures, trying to gain access to pills or weapons C Changes Any drastic change in behavior, functioning or temperament T S Threats Making verbal statements or threats Situations Triggering situations that could be stressful (divorce, traumatic experiences, relational conflict etc)
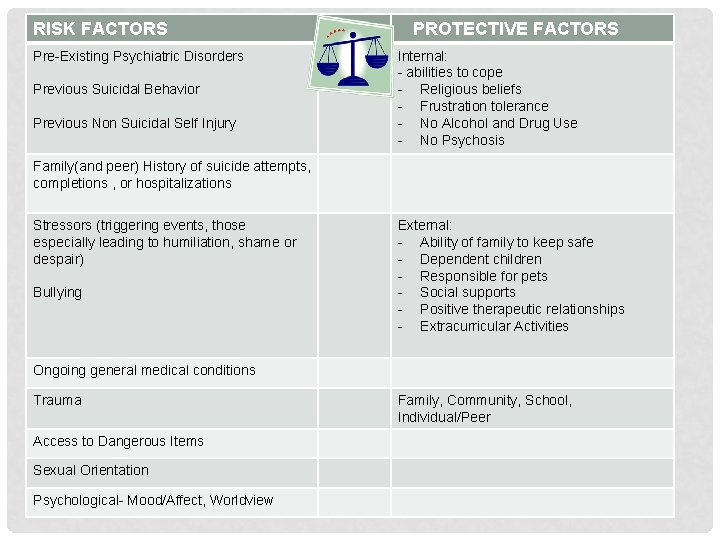
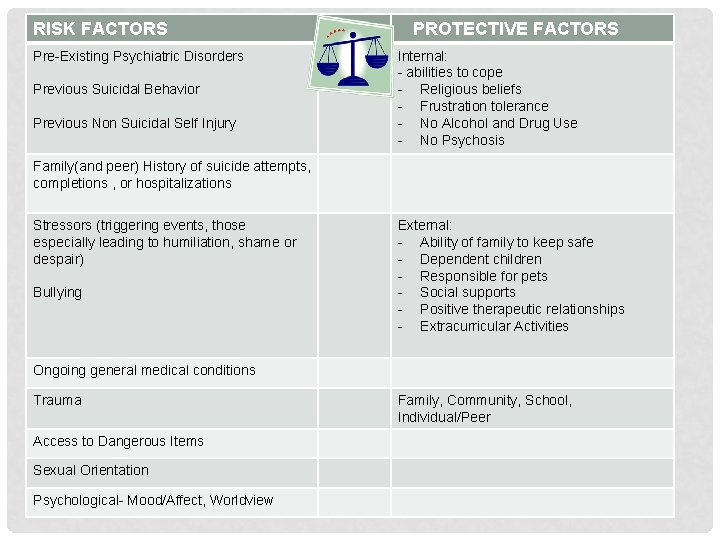
RISK FACTORS Pre-Existing Psychiatric Disorders Previous Suicidal Behavior Previous Non Suicidal Self Injury PROTECTIVE FACTORS Internal: - abilities to cope - Religious beliefs - Frustration tolerance - No Alcohol and Drug Use - No Psychosis Family(and peer) History of suicide attempts, completions , or hospitalizations Stressors (triggering events, those especially leading to humiliation, shame or despair) Bullying External: - Ability of family to keep safe - Dependent children - Responsible for pets - Social supports - Positive therapeutic relationships - Extracurricular Activities Ongoing general medical conditions Trauma Access to Dangerous Items Sexual Orientation Psychological- Mood/Affect, Worldview Family, Community, School, Individual/Peer
SUICIDE AND YOUTH • http: //www. sptsusa. org/not-my-kid/
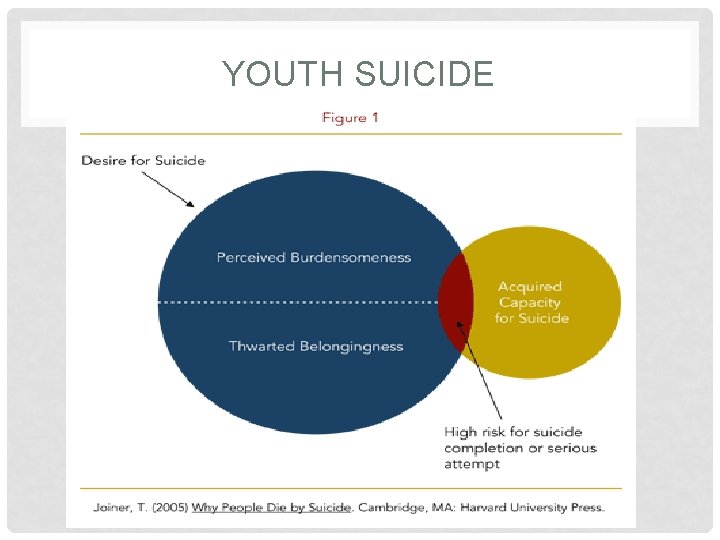
YOUTH SUICIDE
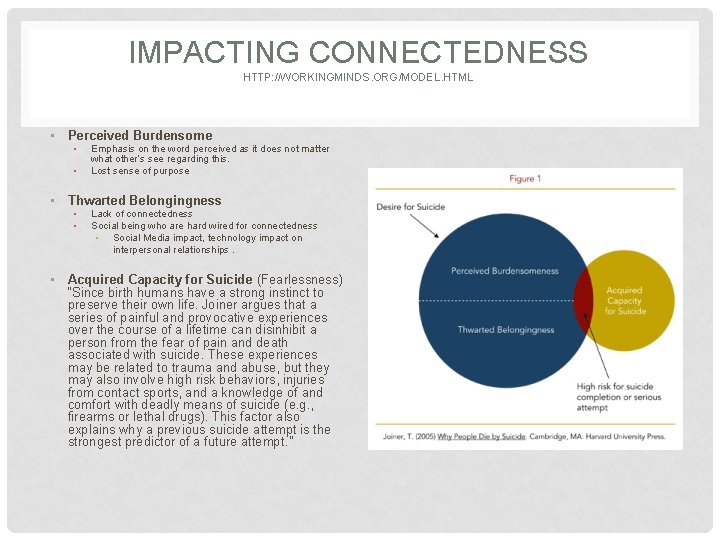
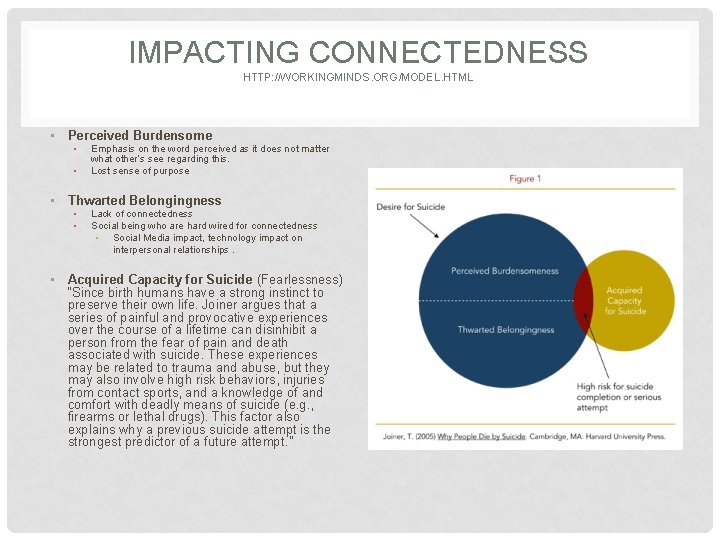
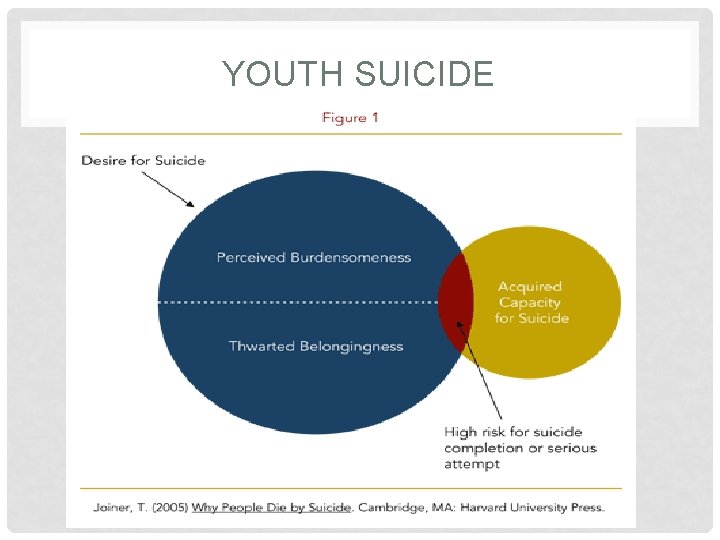
IMPACTING CONNECTEDNESS HTTP: //WORKINGMINDS. ORG/MODEL. HTML • Perceived Burdensome • • Emphasis on the word perceived as it does not matter what other’s see regarding this. Lost sense of purpose • Thwarted Belongingness • • Lack of connectedness Social being who are hard wired for connectedness • Social Media impact, technology impact on interpersonal relationships. • Acquired Capacity for Suicide (Fearlessness) “Since birth humans have a strong instinct to preserve their own life. Joiner argues that a series of painful and provocative experiences over the course of a lifetime can disinhibit a person from the fear of pain and death associated with suicide. These experiences may be related to trauma and abuse, but they may also involve high risk behaviors, injuries from contact sports, and a knowledge of and comfort with deadly means of suicide (e. g. , firearms or lethal drugs). This factor also explains why a previous suicide attempt is the strongest predictor of a future attempt. ”
IMPACTING CONNECTEDNESS • In the Classroom • • • First Five Office Hours Student leaders Student responsibilities Give students voice in decision making policies and development of such • “Teachable moments” connecting after discipline • In the Community • Attending extracurricular activities • School Family Liaison’s (CDC) • Service learning opportunities

RESTRICTING MEANS • Adequate Supervision • Dangerous Objects Secured • Lock Boxes • Fire Arms Secured • (Removed from premises, Trigger Locked, Ammo separate and secured, Gun safes) • Modifying Environment • Motion Sensors, Door and Window Alarms • Bedroom Doors open • Modified Sleep Arrangements
CONTAGION IMPACT OF SUICIDAL BEHAVIOR (SUICIDE POSTVENTION IN THE SCHOOL COMMUNITY, F. ZENERE) • Suicide Contagion. The process in which suicidal behavior is initiated by one or more individuals following the awareness of a recent suicide threat, attempt or completion or a fictional depiction of such behavior. The occurrence of a single suicide in a community (especially an adolescent suicide) increase the risk of further suicides with in that community (Gould, Wallenstein, Kleinmain, O'Carroll and Mercy, 1990 and Philips and Cartensen 1988) • Suicide Cluster. A group of suicides or suicide attempts, or both that occur closer in time and space than would normally be expected in a given community (CDC 1988) Clusters in the united states tend to occur among adolescents and young adults under the age of 24 years (Gould, Wallenstein, Kleinman, 1990, Gould, Wallenstein, Kleinman, O'Carroll and Mercy, 1990) Between 1 -2% of annual teenage suicides occur in clusters (Gould, Petrie, Kleinman and Wallenstein, 1994) 100 -200 teens die in clusters annually (CDC) Sensationalized information regarding suicides that have previously occurred is often the vehicle for contagion
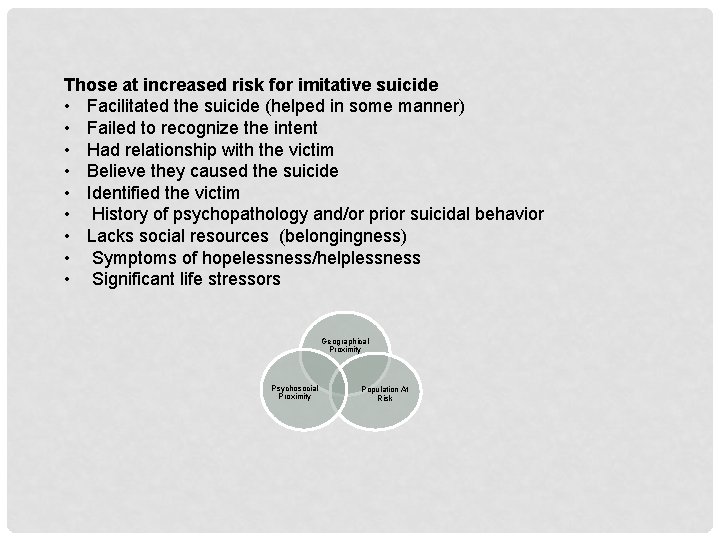
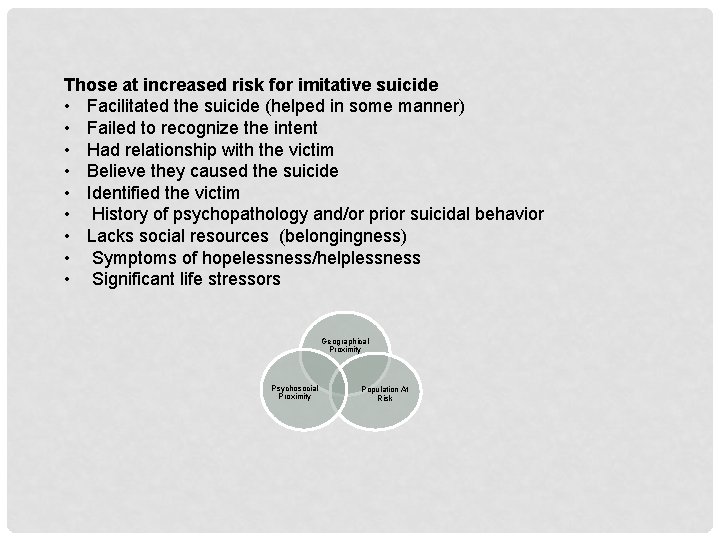
Those at increased risk for imitative suicide • Facilitated the suicide (helped in some manner) • Failed to recognize the intent • Had relationship with the victim • Believe they caused the suicide • Identified the victim • History of psychopathology and/or prior suicidal behavior • Lacks social resources (belongingness) • Symptoms of hopelessness/helplessness • Significant life stressors Geographical Proximity Psychosocial Proximity Population At Risk
QUESTION AND ANSWER • SAMSHA Web and Mobile APP Resources • http: //www. cdc. gov/health yyouth/protective/pdf/con nectedness. pdf PHQ 9 SAFE-T Mobile APP
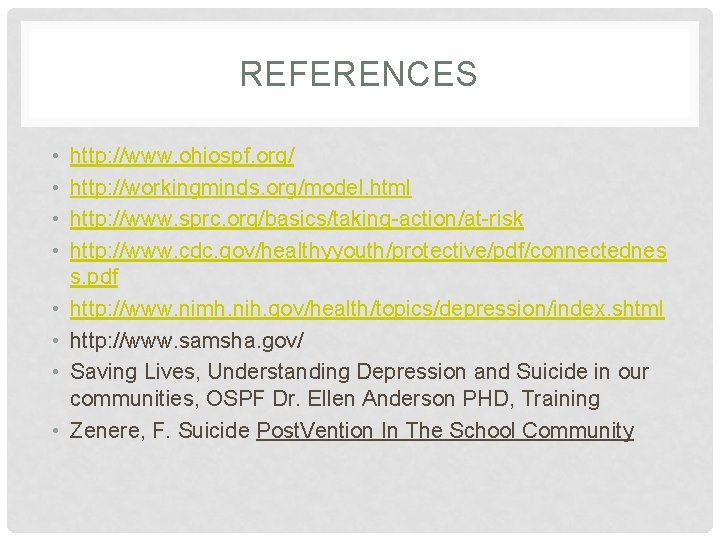
REFERENCES • • http: //www. ohiospf. org/ http: //workingminds. org/model. html http: //www. sprc. org/basics/taking-action/at-risk http: //www. cdc. gov/healthyyouth/protective/pdf/connectednes s. pdf http: //www. nimh. nih. gov/health/topics/depression/index. shtml http: //www. samsha. gov/ Saving Lives, Understanding Depression and Suicide in our communities, OSPF Dr. Ellen Anderson PHD, Training Zenere, F. Suicide Post. Vention In The School Community
 Depression lorain
Depression lorain Youth suicide research consortium
Youth suicide research consortium Lorain county child services
Lorain county child services Lorain county metropolitan housing
Lorain county metropolitan housing Lorain county medical examiner
Lorain county medical examiner Esc of lorain county
Esc of lorain county Mercy regional medical center lorain
Mercy regional medical center lorain Lorain journal
Lorain journal Chapter 25 suicide and nonsuicidal self injury
Chapter 25 suicide and nonsuicidal self injury Suicide girls sara calixto
Suicide girls sara calixto Mad acronym suicide prevention
Mad acronym suicide prevention The citadel counseling center
The citadel counseling center Bill nye the science guy life cycles
Bill nye the science guy life cycles Chapter 20 icd 10
Chapter 20 icd 10 Glencoe health chapter 5
Glencoe health chapter 5 Egoistic suicide
Egoistic suicide Suicide cuts across all social categories
Suicide cuts across all social categories Why people die by suicide joiner
Why people die by suicide joiner Suicide chain teach
Suicide chain teach Texas suicide prevention symposium
Texas suicide prevention symposium Mental health faucets
Mental health faucets Lcps suicide
Lcps suicide Break up suicide
Break up suicide Suicide inhibitor
Suicide inhibitor Enzymes examples
Enzymes examples