Youre Getting Very Sleepy Updated Notes on Narcolepsy
- Slides: 33
You're Getting Very Sleepy: Updated Notes on Narcolepsy Andrea Haller, M. D.
Objectives At the end of this talk you should be able to: 1. Describe the basic clinical features of narcolepsy 2. Understand the Diagnostic Criteria and differences between Type 1 and Type 2 Narcolepsy 3. Appreciate that Type 1 Narcolepsy is an autoimmune disorder
Narcolepsy • A central nervous system disorder that is an important cause of persistent and excessive sleepiness • The second most common cause of disabling daytime sleepiness after sleep apnea. From: “Deuce Bigalow, Male Gigolo” (1999)
Clinical Features 1862: Jean Baptiste Gelineau applied the term “narcolepsy” to a clinical syndrome of daytime sleepiness with: • hypnagogic hallucinations • sleep paralysis • cataplexy
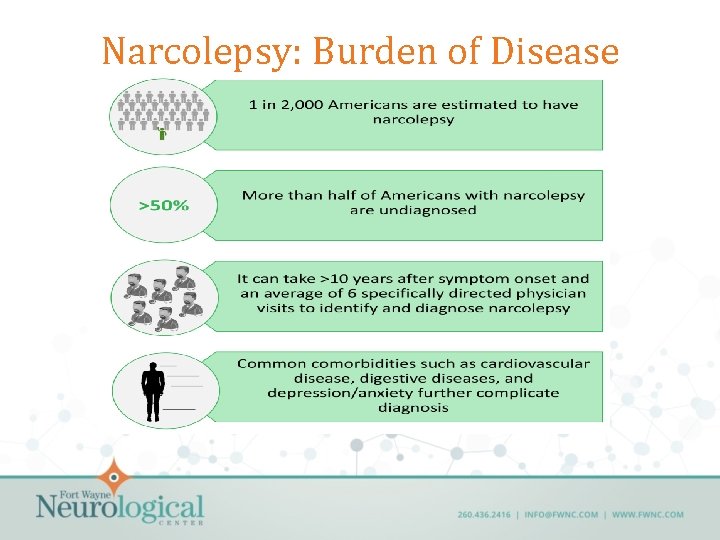
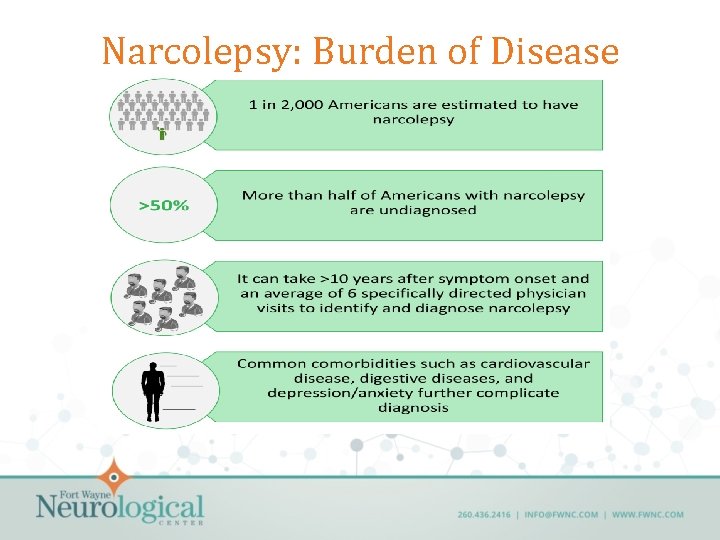
Narcolepsy: Burden of Disease
Narcolepsy: Epidemiology • Equal prevalence in men and women • Typically begins in teens and early twenties, but can occur as early as age 5 or after age 40 • Symptoms may worsen over the first few years and then persist for life • Half of all patients report that symptoms interfere with job, marriage, or social life.
Narcolepsy • Can be considered a disorder of state control • Elements of sleep intrude into wakefulness and elements of wakefulness intrude into sleep • This state instability results in characteristic symptoms
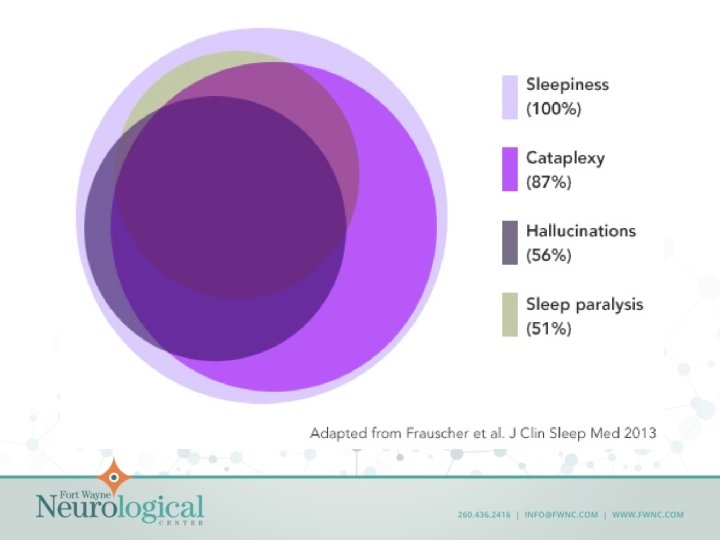
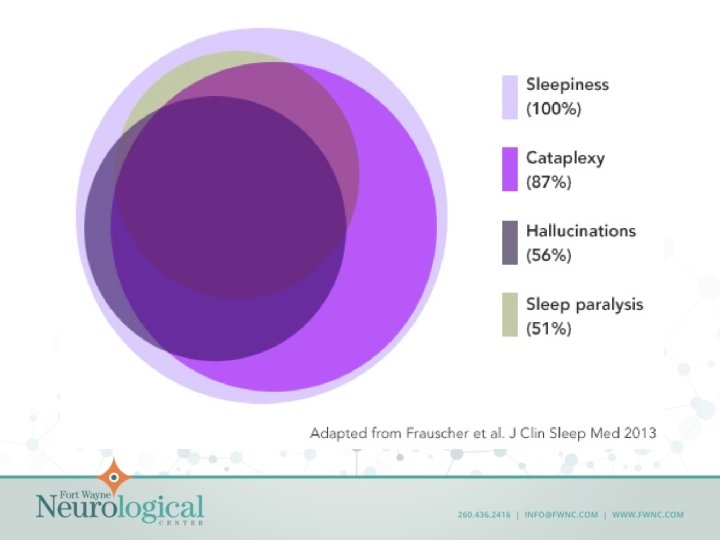
Excessive daytime sleepiness • All patients with narcolepsy have excessive daytime sleepiness • Over 24 hours, they do not sleep more than normal controls, but they are prone to fall asleep throughout the day, often at inappropriate times. • “Sleep attacks” • Often improved temporarily by a brief nap • Patients with untreated narcolepsy have an ESS score greater than 15.
Associated Features: Hypnagogic hallucinations • Vivid, often frightening hallucinations that occur just as the patient is falling asleep • Can be visual, auditory or tactile sensations • Hypnopompic: occur upon awakening • Likely result from wakefulness during REM sleep dreaming
Associated Features: Sleep paralysis • Complete inability to move a minute or two after awakening • Episodes may be accompanied by hypnagogic hallucinations. • Can be ended by falling back to sleep or by sensory stimulation such as a touch
Associated Features: Cataplexy • Sudden episodes of bilateral muscle weakness leading to partial or complete collapse • Most often triggered by strong emotions such as laughter, anger or excitement – Can also be triggered by a large meal, periods of stress • Typical episodes last one to two minutes, and are not associated with impairment of consciousness • Between 60 -80% of narcoleptic individuals develop cataplexy
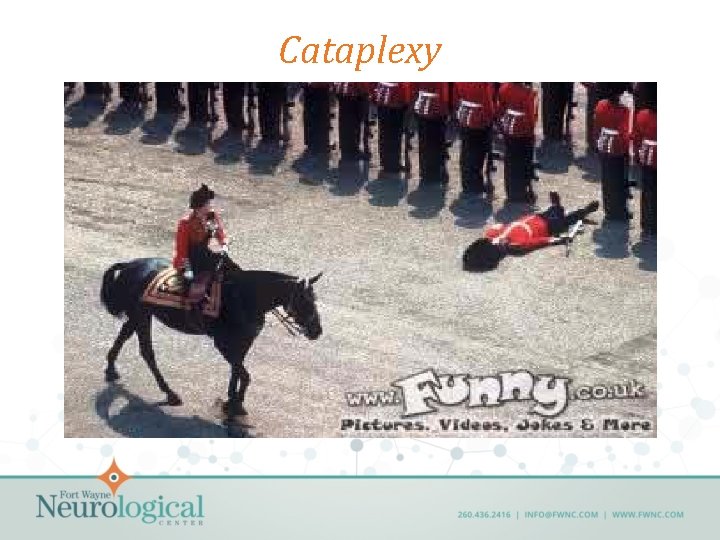
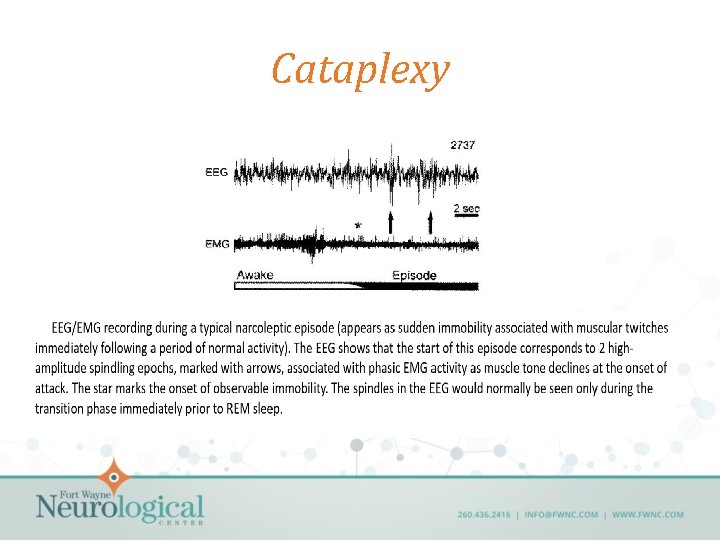
Cataplexy
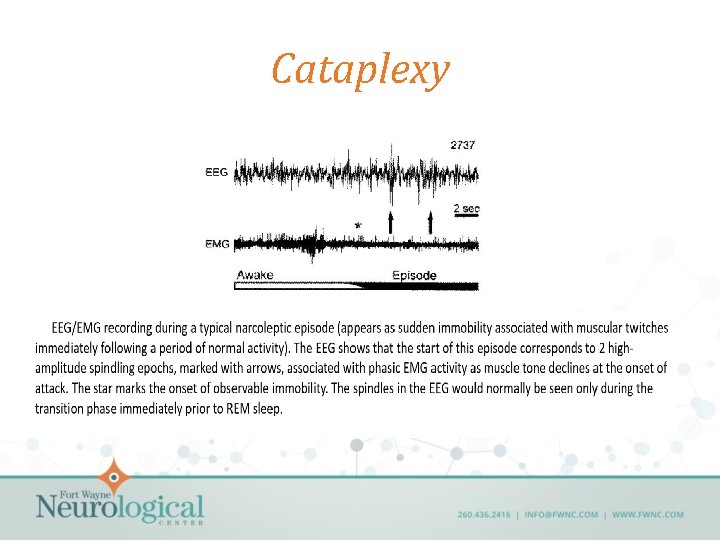
Cataplexy
Other symptoms… Sleep maintenance insomnia Microsleep episodes Automatic behaviors Fragmented nighttime sleep Higher than expected incidence of other sleep disorders • Slightly higher incidence of adult onset diabetes mellitus, migraine headaches and obesity • • •
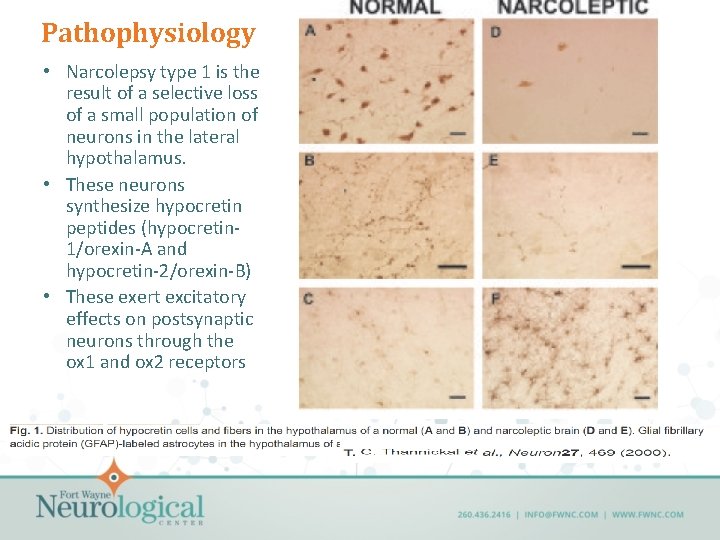
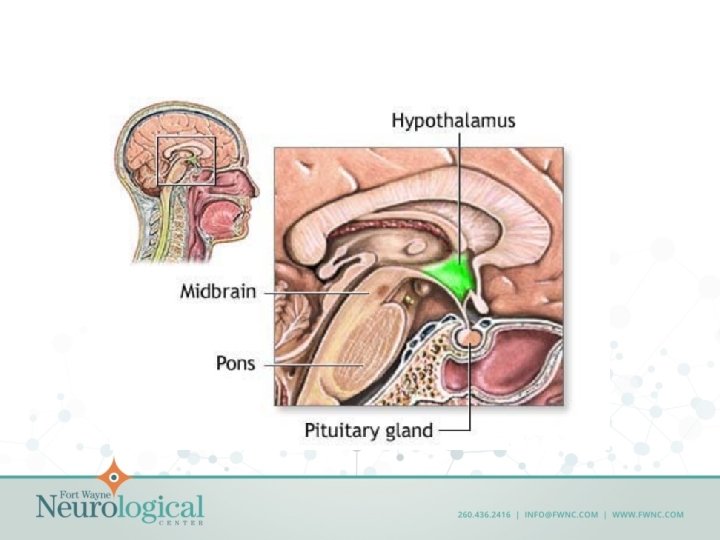
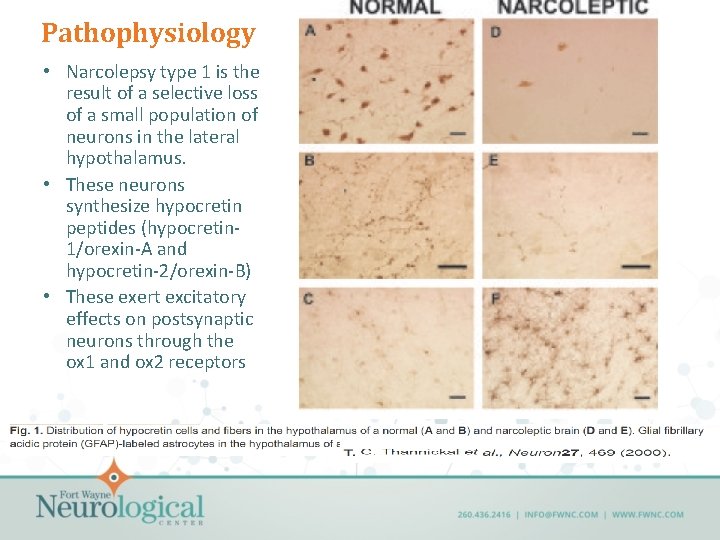
Pathophysiology • Narcolepsy type 1 is the result of a selective loss of a small population of neurons in the lateral hypothalamus. • These neurons synthesize hypocretin peptides (hypocretin 1/orexin-A and hypocretin-2/orexin-B) • These exert excitatory effects on postsynaptic neurons through the ox 1 and ox 2 receptors
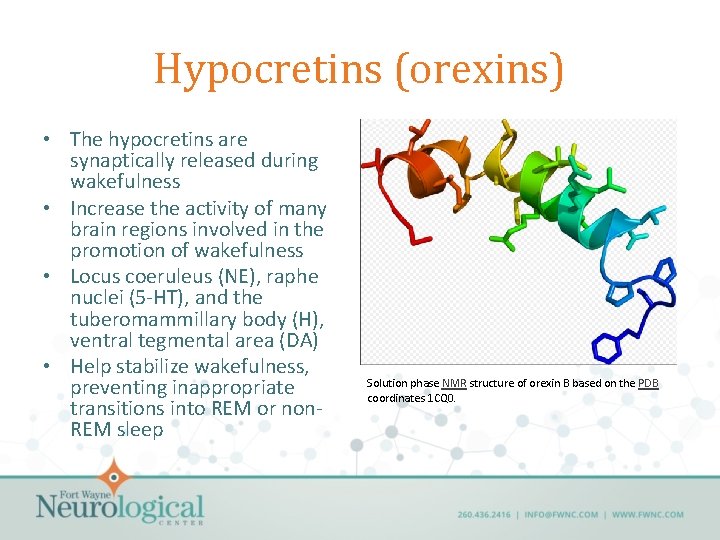
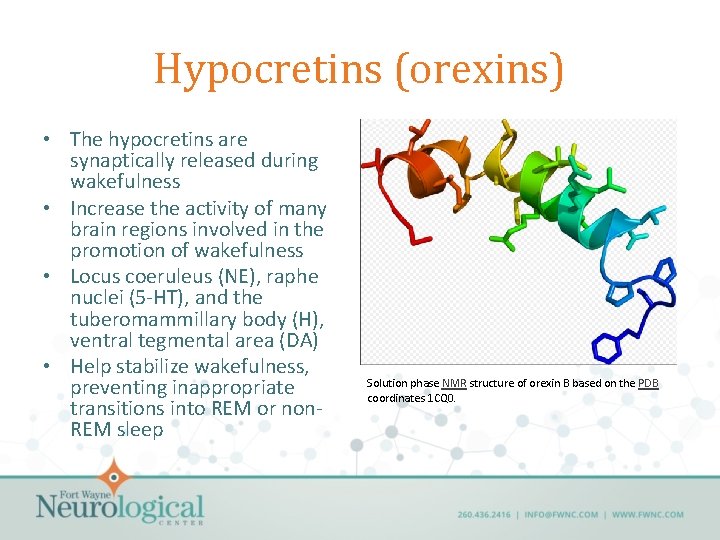
Hypocretins (orexins) • The hypocretins are synaptically released during wakefulness • Increase the activity of many brain regions involved in the promotion of wakefulness • Locus coeruleus (NE), raphe nuclei (5 -HT), and the tuberomammillary body (H), ventral tegmental area (DA) • Help stabilize wakefulness, preventing inappropriate transitions into REM or non. REM sleep Solution phase NMR structure of orexin B based on the PDB coordinates 1 CQ 0.
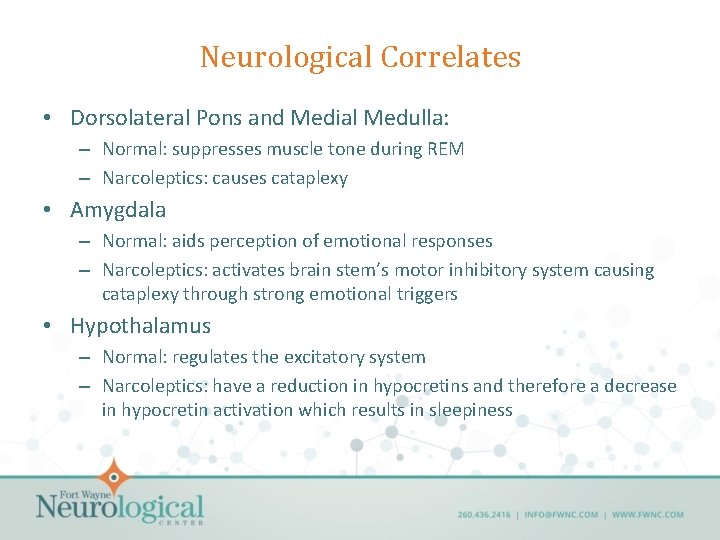
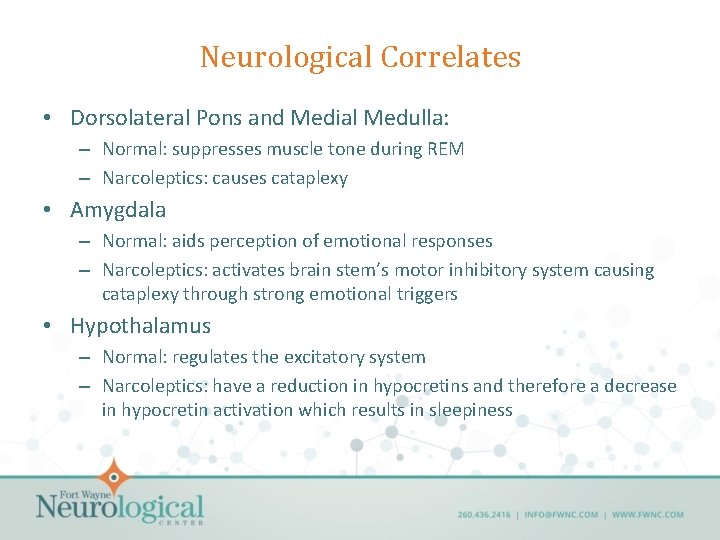
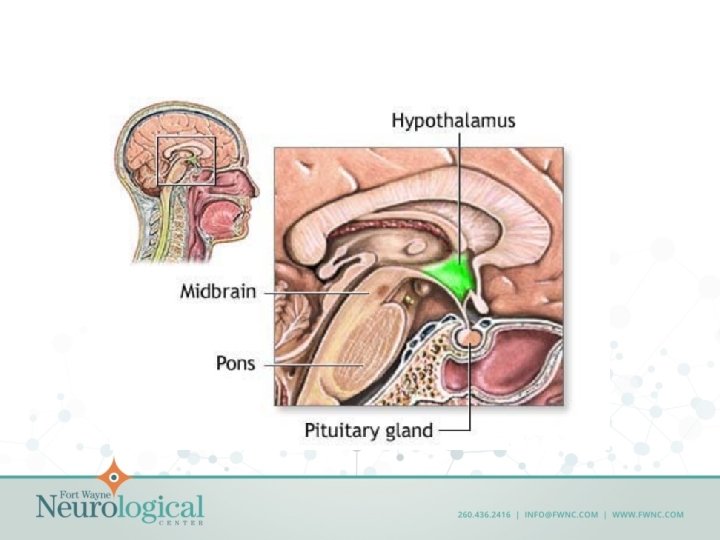
Neurological Correlates • Dorsolateral Pons and Medial Medulla: – Normal: suppresses muscle tone during REM – Narcoleptics: causes cataplexy • Amygdala – Normal: aids perception of emotional responses – Narcoleptics: activates brain stem’s motor inhibitory system causing cataplexy through strong emotional triggers • Hypothalamus – Normal: regulates the excitatory system – Narcoleptics: have a reduction in hypocretins and therefore a decrease in hypocretin activation which results in sleepiness
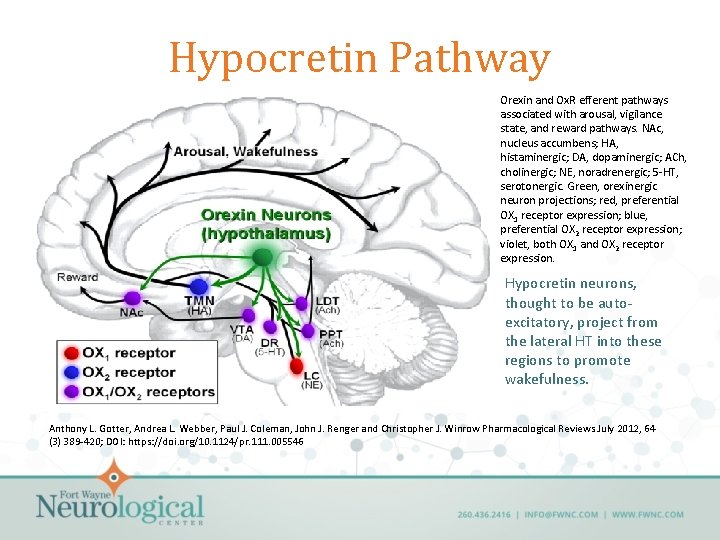
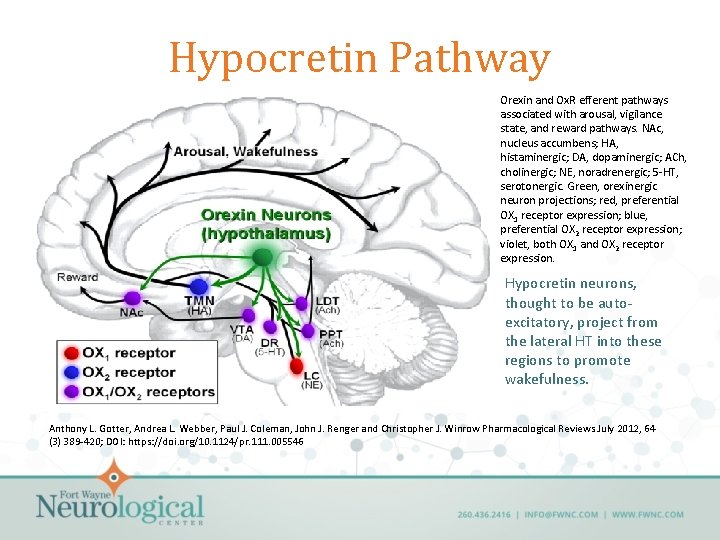
Hypocretin Pathway Orexin and Ox. R efferent pathways associated with arousal, vigilance state, and reward pathways. NAc, nucleus accumbens; HA, histaminergic; DA, dopaminergic; ACh, cholinergic; NE, noradrenergic; 5 -HT, serotonergic. Green, orexinergic neuron projections; red, preferential OX 1 receptor expression; blue, preferential OX 2 receptor expression; violet, both OX 1 and OX 2 receptor expression. Hypocretin neurons, thought to be autoexcitatory, project from the lateral HT into these regions to promote wakefulness. Anthony L. Gotter, Andrea L. Webber, Paul J. Coleman, John J. Renger and Christopher J. Winrow Pharmacological Reviews July 2012, 64 (3) 389 -420; DOI: https: //doi. org/10. 1124/pr. 111. 005546
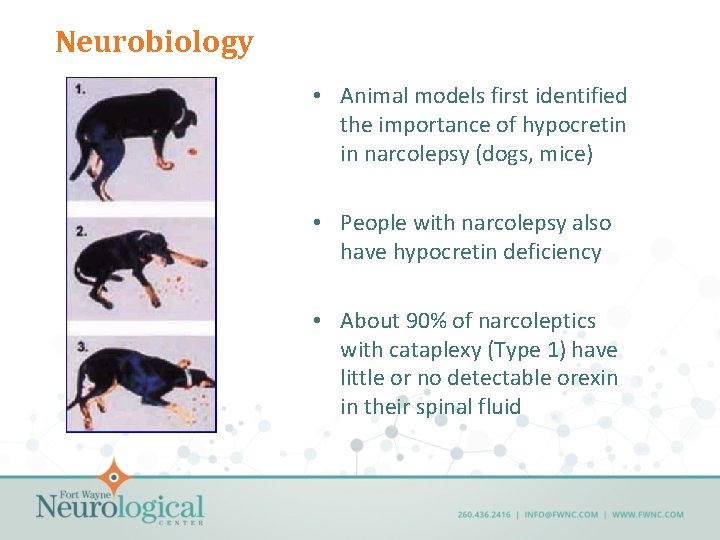
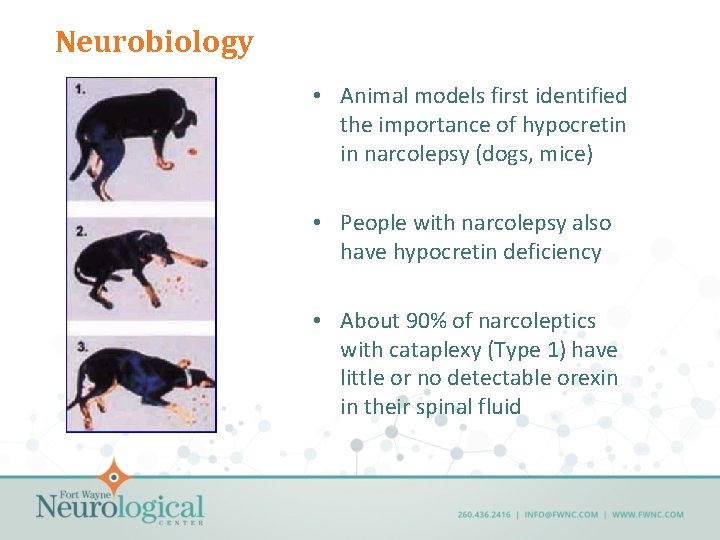
Neurobiology • Animal models first identified the importance of hypocretin in narcolepsy (dogs, mice) • People with narcolepsy also have hypocretin deficiency • About 90% of narcoleptics with cataplexy (Type 1) have little or no detectable orexin in their spinal fluid
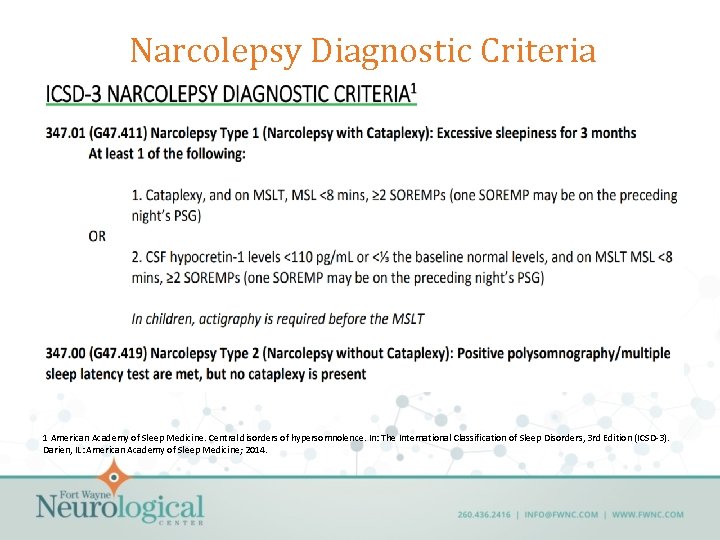
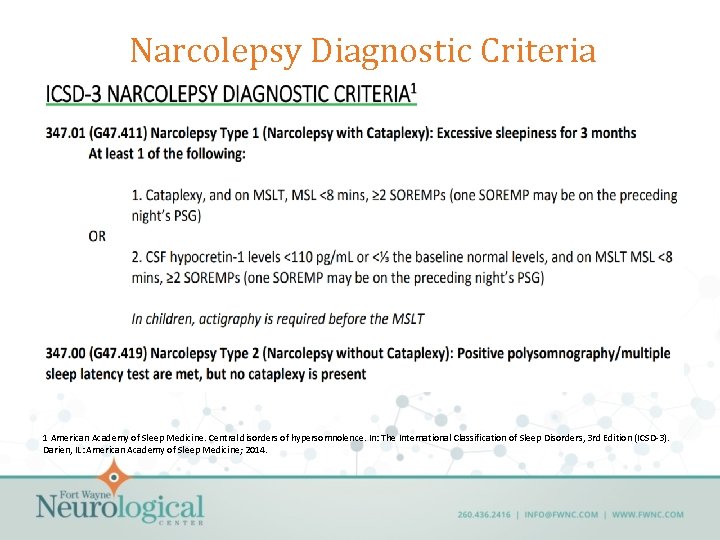
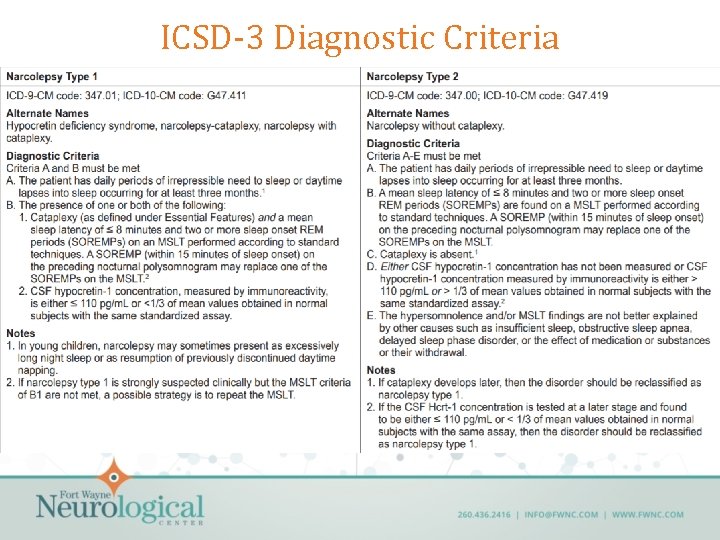
Narcolepsy Diagnostic Criteria 1 American Academy of Sleep Medicine. Central disorders of hypersomnolence. In: The International Classification of Sleep Disorders, 3 rd Edition (ICSD-3). Darien, IL: American Academy of Sleep Medicine; 2014.
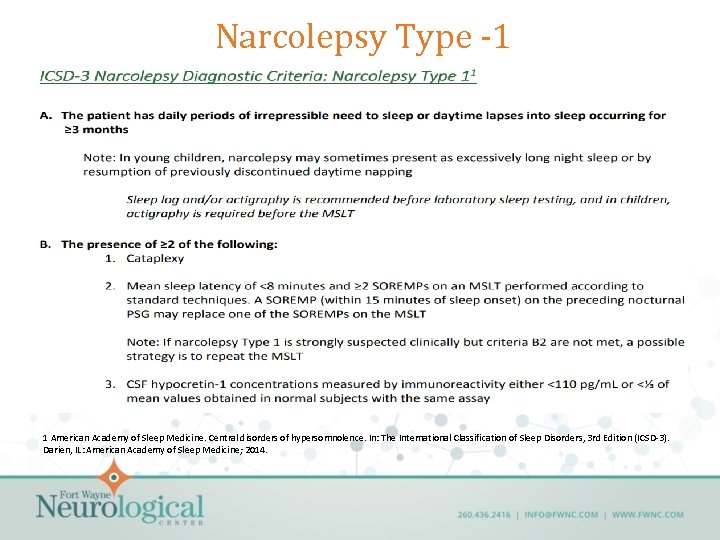
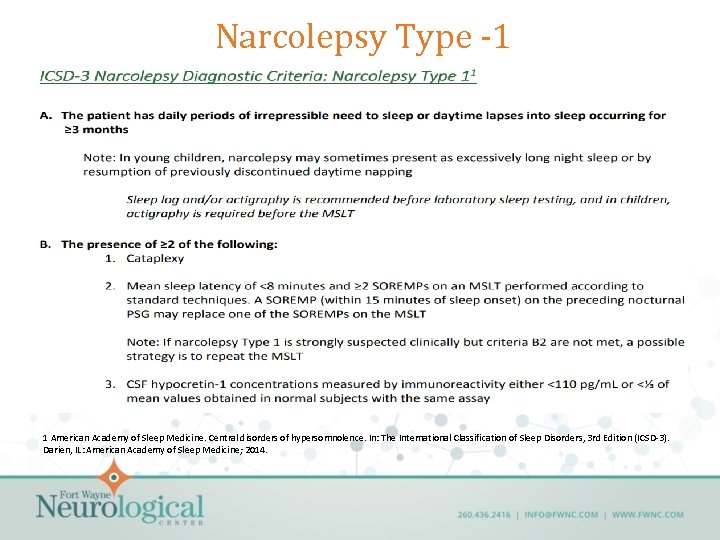
Narcolepsy Type -1 1 American Academy of Sleep Medicine. Central disorders of hypersomnolence. In: The International Classification of Sleep Disorders, 3 rd Edition (ICSD-3). Darien, IL: American Academy of Sleep Medicine; 2014.
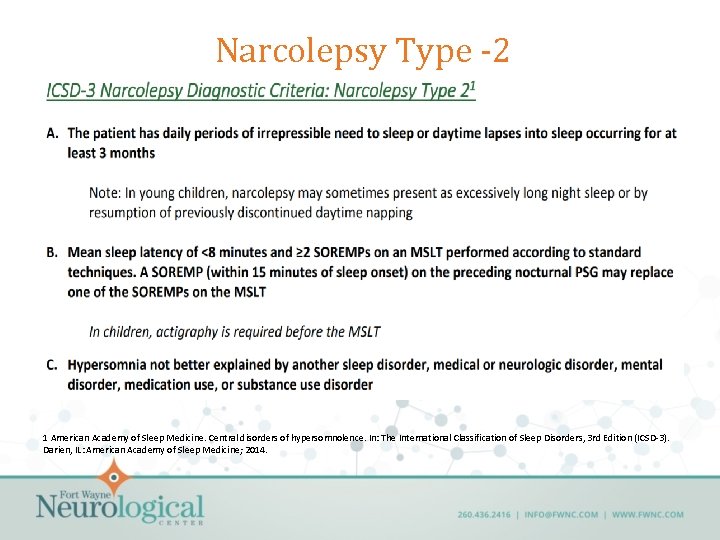
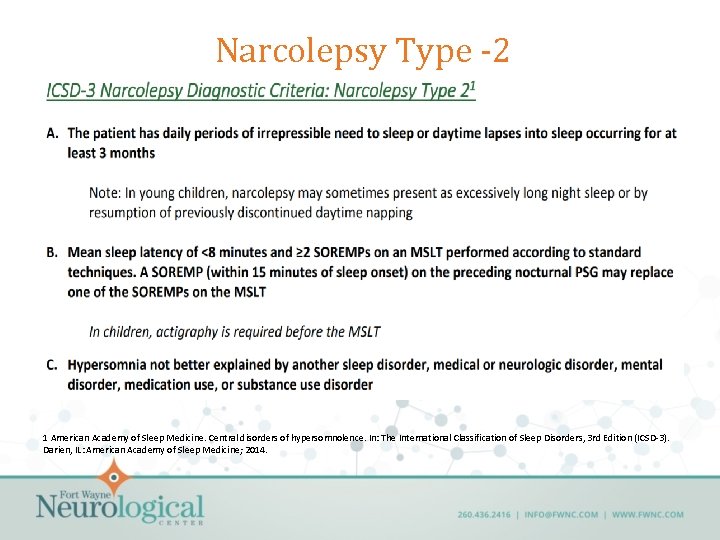
Narcolepsy Type -2 1 American Academy of Sleep Medicine. Central disorders of hypersomnolence. In: The International Classification of Sleep Disorders, 3 rd Edition (ICSD-3). Darien, IL: American Academy of Sleep Medicine; 2014.
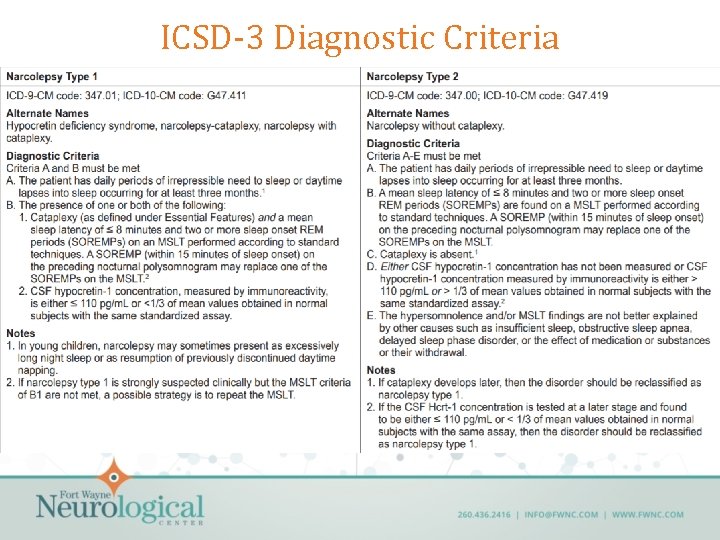
ICSD-3 Diagnostic Criteria
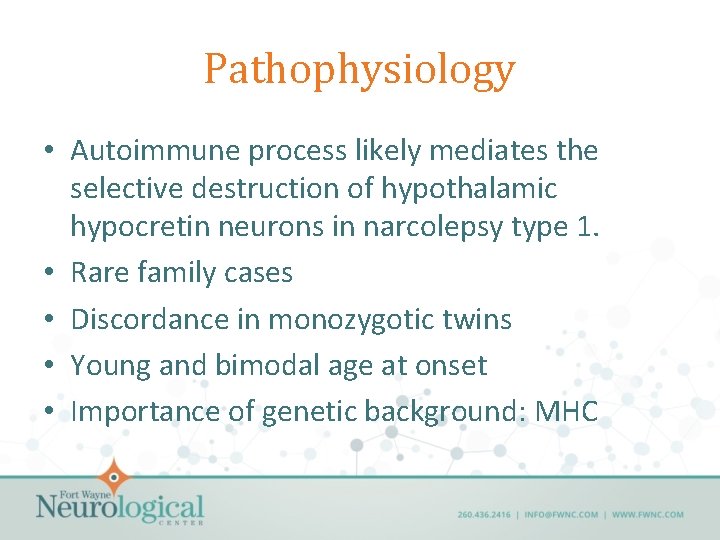
Pathophysiology • Autoimmune process likely mediates the selective destruction of hypothalamic hypocretin neurons in narcolepsy type 1. • Rare family cases • Discordance in monozygotic twins • Young and bimodal age at onset • Importance of genetic background: MHC
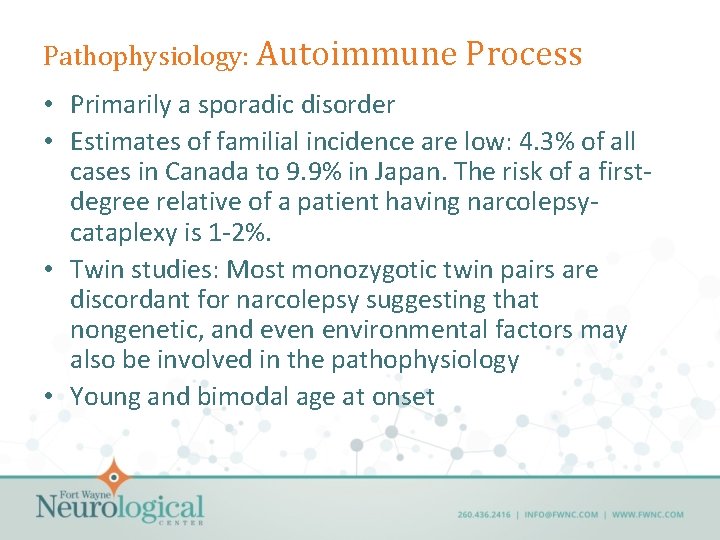
Pathophysiology: Autoimmune Process • Primarily a sporadic disorder • Estimates of familial incidence are low: 4. 3% of all cases in Canada to 9. 9% in Japan. The risk of a firstdegree relative of a patient having narcolepsycataplexy is 1 -2%. • Twin studies: Most monozygotic twin pairs are discordant for narcolepsy suggesting that nongenetic, and even environmental factors may also be involved in the pathophysiology • Young and bimodal age at onset
Autoimmune Process: Major Histocompatability Locus (MHC) • DQB 1*06: 02 is the most important factor predisposing to narcolepsy type 1 • >98% of patients with narcolepsy type 1 carry HLA class II HLA-DQB 1*06: 02 allele. • Still, common in the population—frequency varies across ethnic groups from 12% in Japanese) to 38% in African Americans • Not sufficient for the development of the disease. • Homozygotes have additional 2 -4 fold risk for narcolepsy compared to heterozygotes, and may also exhibit more severe symptoms
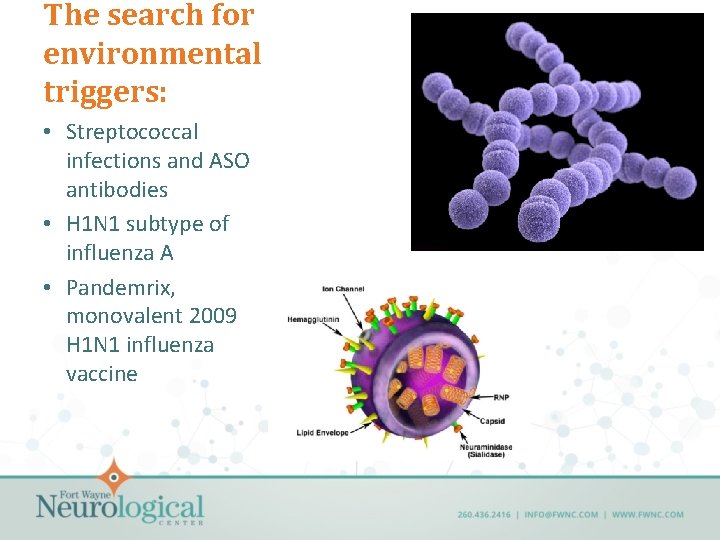
The search for environmental triggers: • Streptococcal infections and ASO antibodies • H 1 N 1 subtype of influenza A • Pandemrix, monovalent 2009 H 1 N 1 influenza vaccine
Non-HLA, Non-HCRT Genes in Narcolepsy • T cell receptor alpha (TCRA): – encodes the alpha chain of the mature T cell receptor αβ heterodimer – this protein is localized on the surface of T cells and recognizes antigens bound and presented by class I or class II MHC molecules – following engagement with the antigen-MHC complex, initiates an immune response – functional TCRs are only expressed in immune T-cells
Non-HLA, Non-HCRT Genes in Narcolepsy • CPT 1 B: rate-limiting enzyme in long chain fatty acid β oxidation in muscle mitochondria, a pathway implicated in regulation of theta frequency in REM sleep in mouse models • CHKB is a kinase involved in phosphatidylcholine synthesis- a precursor to acetylcholine which is a known regulator of REM sleep and wakefulness. • P 2 RY 11 purinergic receptor gene (a susceptibility locus), appear to play a role in modulating the immune response
Autoimmune? • In narcolepsy, females are not at increased risk • It has been difficult to find direct evidence of humoral or cellular autoimmune attack – Recent identification of reactive autoantibodies against the Tribbles 2 homolog (TRIB 2) protein in sera of narcolepsy cases.
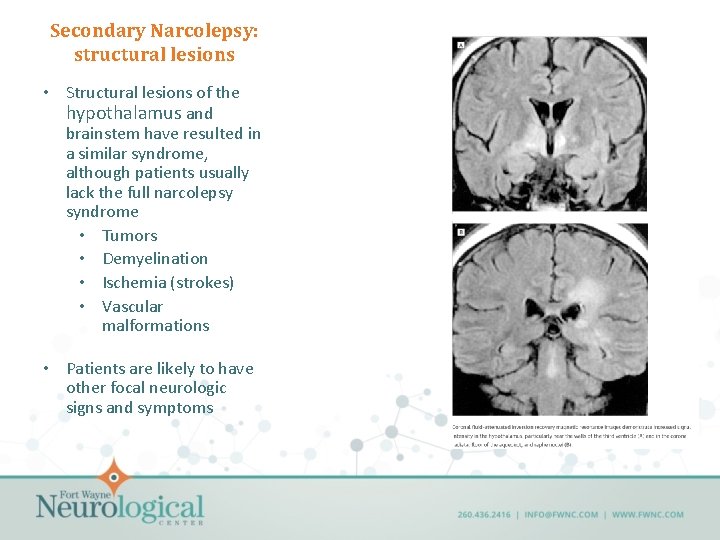
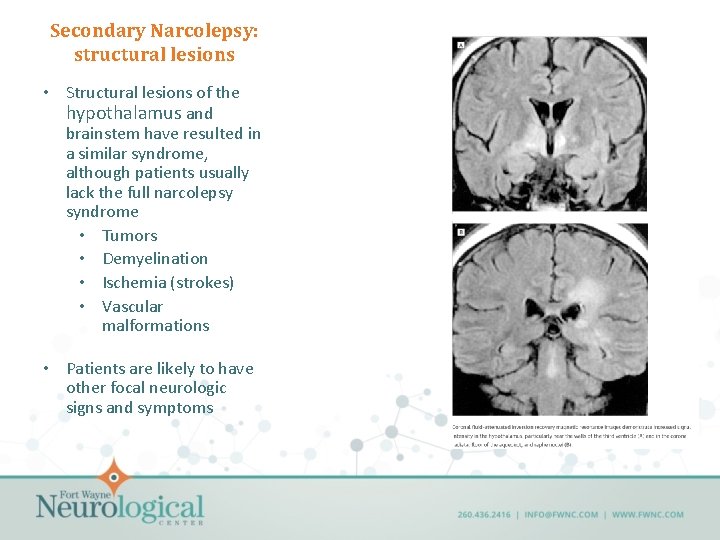
Secondary Narcolepsy: structural lesions • Structural lesions of the hypothalamus and brainstem have resulted in a similar syndrome, although patients usually lack the full narcolepsy syndrome • Tumors • Demyelination • Ischemia (strokes) • Vascular malformations • Patients are likely to have other focal neurologic signs and symptoms