Your needs assessment process is this enabling you

Your needs assessment process … is this enabling you to develop an accurate and holistic picture of people’s needs (and wishes) and to develop packages of care and support to meet these effectively? Is this process comprehensive enough and does it provide you with the information you need to deliver required outcomes for people?

What is your experience of local authority needs assessments? Do you do your own as well (or instead)?

What evidence do you have to show that staff understand (and are implementing) their responsibilities in relation to promoting equality and respecting diversity?
What evidence do you have to show that staff understand (and are implementing) their responsibilities in relation to preventing discrimination, bullying and harassment?

Use a read and sign system for key policies and procedures

Use of technology and equipment What technology and equipment is the service using to enhance the delivery of effective care and support, and to promote people’s independence?
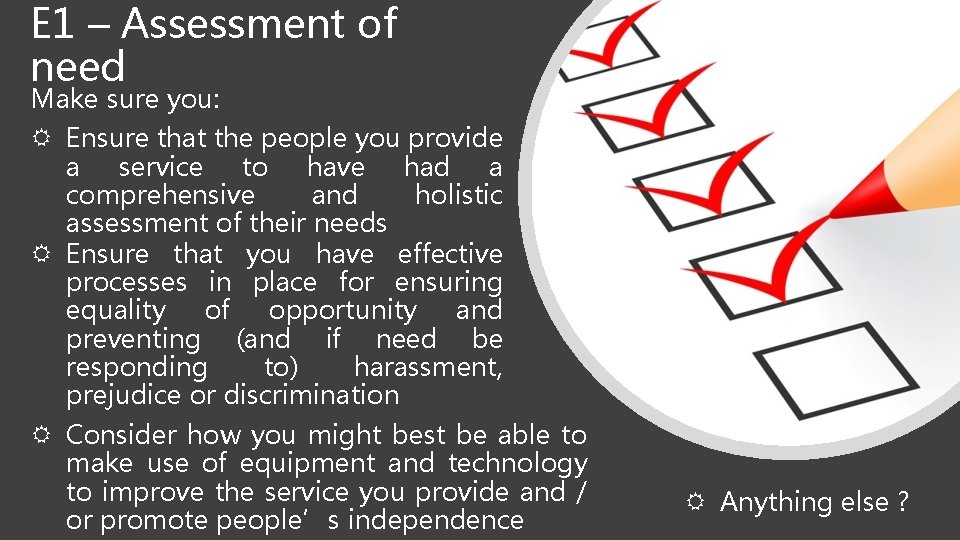
E 1 – Assessment of need Make sure you: Ensure that the people you provide a service to have had a comprehensive and holistic assessment of their needs Ensure that you have effective processes in place for ensuring equality of opportunity and preventing (and if need be responding to) harassment, prejudice or discrimination Consider how you might best be able to make use of equipment and technology to improve the service you provide and / or promote people’s independence Anything else ?
E 2 – Making sure staff have the skills, knowledge and experience they need

How do you ensure that new staff receive a comprehensive induction?

Do you ask staff for feedback about your induction process and how it could be improved?
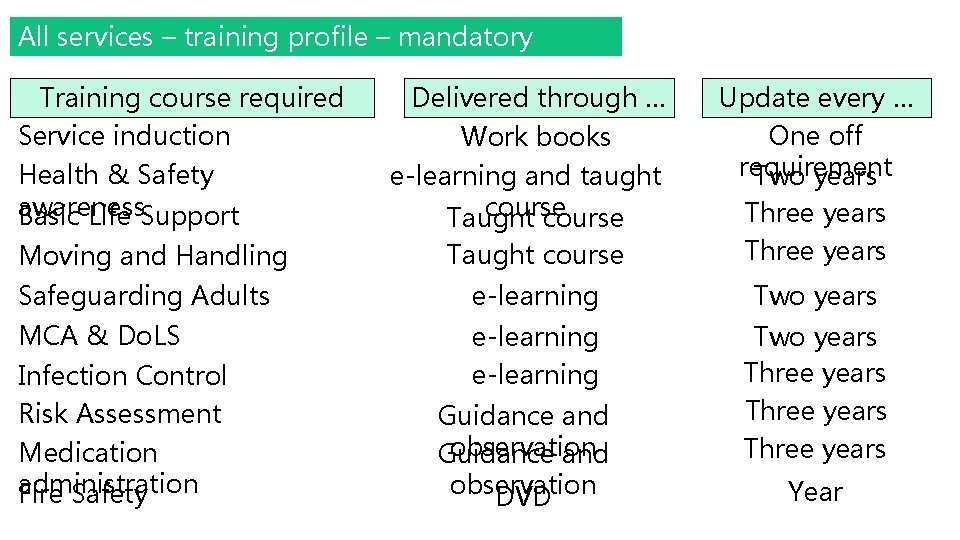
All services – training profile – mandatory courses Training course required Delivered through … Service induction Work books Health & Safety awareness Basic Life Support e-learning and taught course Taught course Update every … One off requirement Two years Taught course Three years Safeguarding Adults e-learning Two years MCA & Do. LS e-learning Two years Three years Moving and Handling Infection Control Risk Assessment Medication administration Fire Safety Guidance and observation DVD Year
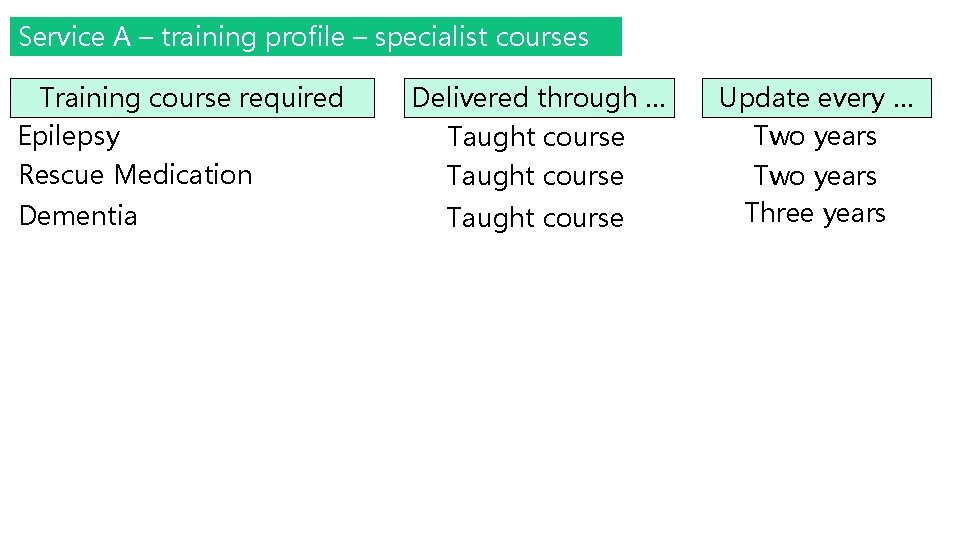
Service A – training profile – specialist courses Training course required Epilepsy Delivered through … Rescue Medication Taught course Dementia Taught course Update every … Two years Three years
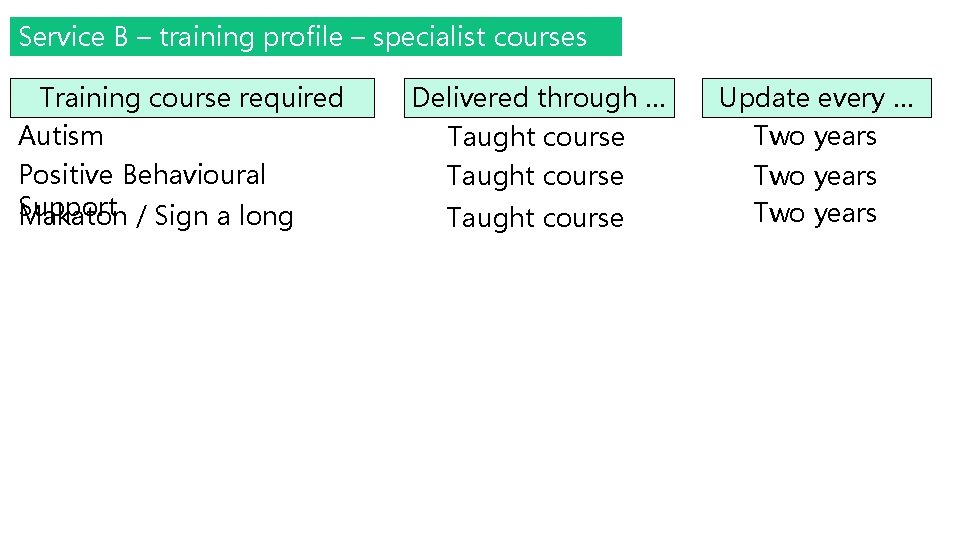
Service B – training profile – specialist courses Training course required Autism Positive Behavioural Support Makaton / Sign a long Delivered through … Taught course Update every … Two years
How are you ensuring that staff receive relevant training in a timely manner? (i. e. before they are required to support or care for someone with specific needs)

What Best Practice guidance are you using?
How are you reassuring yourself that staff have not only ‘done the training’ but actually have the knowledge they need and are implementing this in their day to day practice?

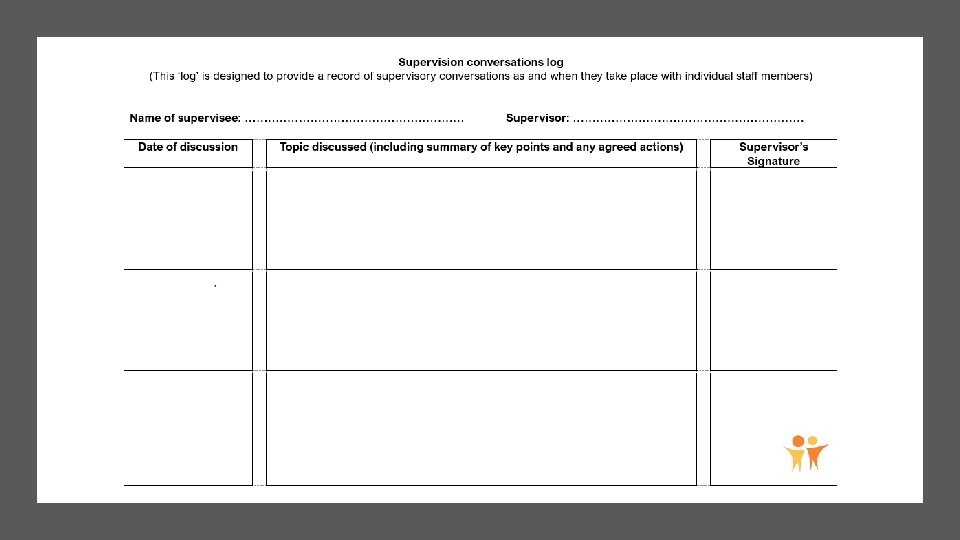
Staff supervision and support Are you confident that you are able to evidence staff receiving regular 1: 1 supervision and an annual appraisal? What are your achieving this? tips Any challenges you face? for
Do you ask staff for feedback about the supervision and support they receive, how well it is working for them and whether it could be improved?
E 2 – Making sure staff have the skills, knowledge and experience they need Make sure you: Have a comprehensive and effective induction programme for orientating new staff Have a training profile for each service which highlights the mandatory and specialist training that staff need to work there Provide staff with relevant training in a timely manner and make sure that this is kept up to date
E 2 – Making sure staff have the skills, knowledge and experience they need Make sure you: Deliver training that is in line with best practice guidelines Ensure staff (including volunteers) receive regular supervision and support Anything else ?

E 3: Supporting people to eat and drink and maintain a balanced diet
What evidence do you have that your service is regularly consulting with people about what they want to eat and drink (including meeting any cultural requirements)?
What are you doing to encourage people to make eating and drinking choices which promote their health and wellbeing?

Do people have healthy eating plans? Is there evidence of people having specific diets if they have a medical need or cultural requirement for this?
What is general practice within the service in relation to mealtimes and where, when and with whom, people choose to eat? What arrangements are there if people want to eat something different, at a different time or in a different room?
What arrangements are in place (including access to specialist advice) for people who need additional support with eating and / or drinking?
Eating and drinking … are you seeking service user feedback? What do service users say about their experience of the food, their choices and mealtimes?
E 3: Supporting people to eat and drink and maintain a balanced diet Make sure you: Involve people in decisions about what they eat and drink (including identifying any cultural requirements) Support people to eat a balanced and healthy diet which promotes their effective nutrition Provide people with an enjoyable (and if necessary flexible) meal time experience Ensure that people with complex needs around eating and drinking get the additional support they need Anything else ?
E 4 – How well do our staff work together and with staff from other agencies to ensure effective person centred care and support?
What evidence would you use to highlight that staff are working effectively together to achieve positive outcomes for service users?
What evidence would you use to highlight that staff are working effectively with staff from other agencies and organisations to achieve positive outcomes for service users?

Are there areas where staff could either work better as a team or with other agencies? Room for improvement
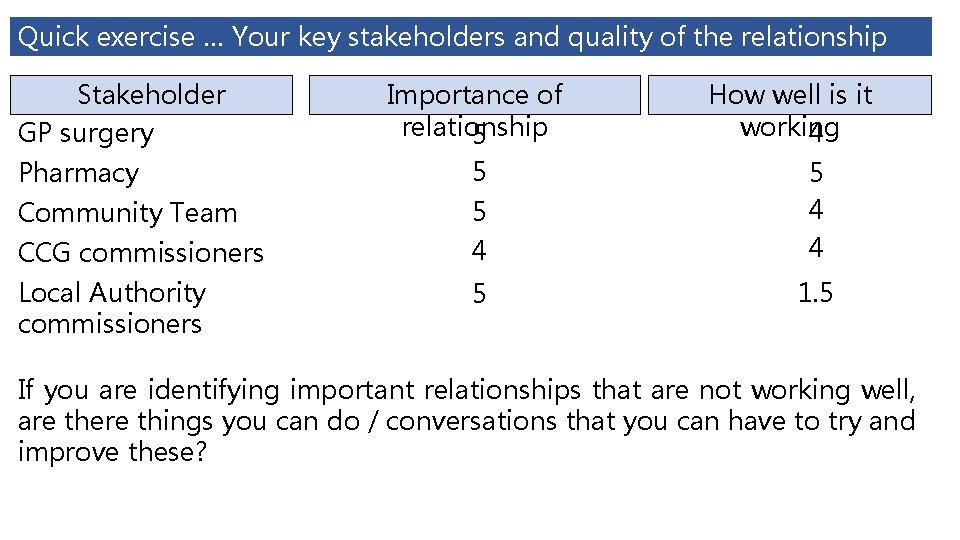
Quick exercise … Your key stakeholders and quality of the relationship Stakeholder GP surgery Importance of relationship 5 How well is it working 4 Pharmacy 5 Community Team 5 CCG commissioners 4 5 4 4 Local Authority commissioners 5 1. 5 If you are identifying important relationships that are not working well, are there things you can do / conversations that you can have to try and improve these?
E 4 – Working as a team and with staff from other agencies Make sure you: Work proactively and effectively to ensure that people receive consistent, timely and coordinated person centred support Anything else?

E 5 – Promoting health lifestyles and enabling access to healthcare professionals

http: //www. bild. org. uk/resour ces/easy-readinformation/health-easy-readlinks/

Do any services use Health Action Plans?
Is the service able to register people with a GP? Is the service able to register people with a dentist? Is the service able to access other healthcare professionals as and when people need them?
Is the service aware of all the medical conditions that its service users have and does it have? Do you have the knowledge, skills and healthcare support required to monitor and manage these effectively? Are you aware of unmet healthcare needs that people may have? How are you dealing with these ?
E 5 – Promoting health lifestyles and enabling access to healthcare professionals Make sure you: Meet people’s day to day health and wellbeing needs Ensure that people are provided with information and explanation about healthcare treatments (including medicines) Involve people in regularly monitoring their health Ensure that people can access appropriate healthcare services in a timely manner Anything else ?
E 6 – Meeting people’s needs with aids and adaptations and the design and decoration of the building
What specific aids and adaptations does your service have to enable it to meet people’s needs?
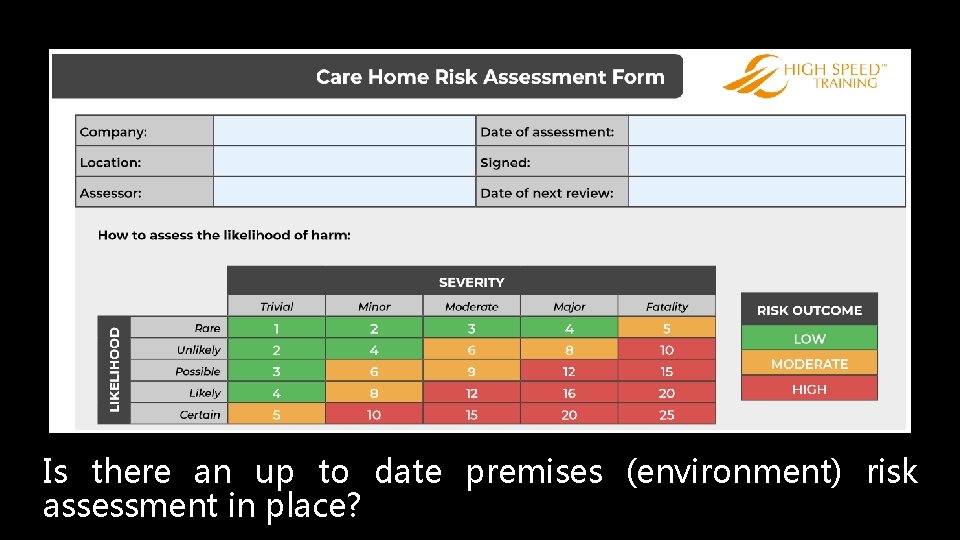
Is there an up to date premises (environment) risk assessment in place?

Is there an up to date fire risk assessment and evacuation plans in place?
Is the service carrying out regular maintenance audits? Are issues raised in these maintenance audits being remedied in a timely manner (and in ways that minimise disruption to people using the service?

Low priorit y Mediu m priority High priorit y

Monitoring and servicing of equipment Is there evidence of: Ongoing checks and monitoring being carried out by staff? Regular servicing and maintenance? Staff receiving relevant training? Equipment being removed from operation if faulty?
What evidence is there that people are involved in choosing the decoration and furnishings in their home?

Do people have the space (and the opportunity) they need to sit outside, meet with their visitors, engage in meaningful activities, spend time with others or on their own? Any problems or

E 6 – Meeting people’s needs with aids and adaptations and the design and decoration of the building Make sure you: Involve people in decisions about their environment Ensure your premises meet people’s diverse needs (including their cultural needs) Provide appropriate space for people § to: sit outside § meet with their visitors § carry out meaningful activities § spend time with others § spend time on their own
E 6 – Meeting people’s needs with aids and adaptations and the design and decoration of the building Make sure you: Ensure signage, decoration and adaptations to the building meet people’s needs Ensure people are not disrupted or distressed by any changes to the environment Anything else?
E 7: Consent to care and treatment
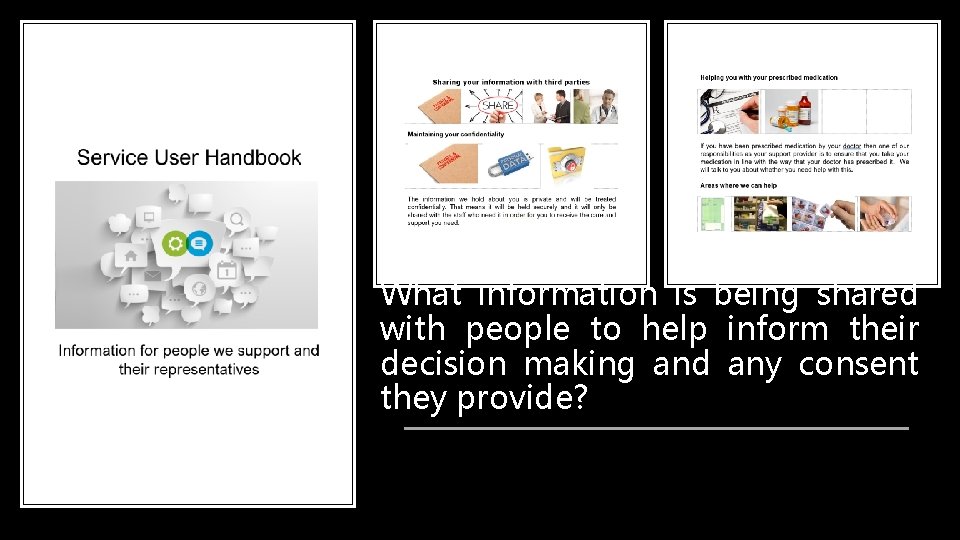
What information is being shared with people to help inform their decision making and any consent they provide?
How can you evidence that people are providing their informed (valid) consent in relation to the care and support you provide them with? In what areas have people provided you with their informed consent? How are you able to evidence that people’s (continued) consent is being reviewed with them?
If Best Interest decisions have been arrived at, are these supported by a corresponding Mental Capacity assessment? How are you able to evidence that people’s Best Interest decisions are being periodically reviewed?
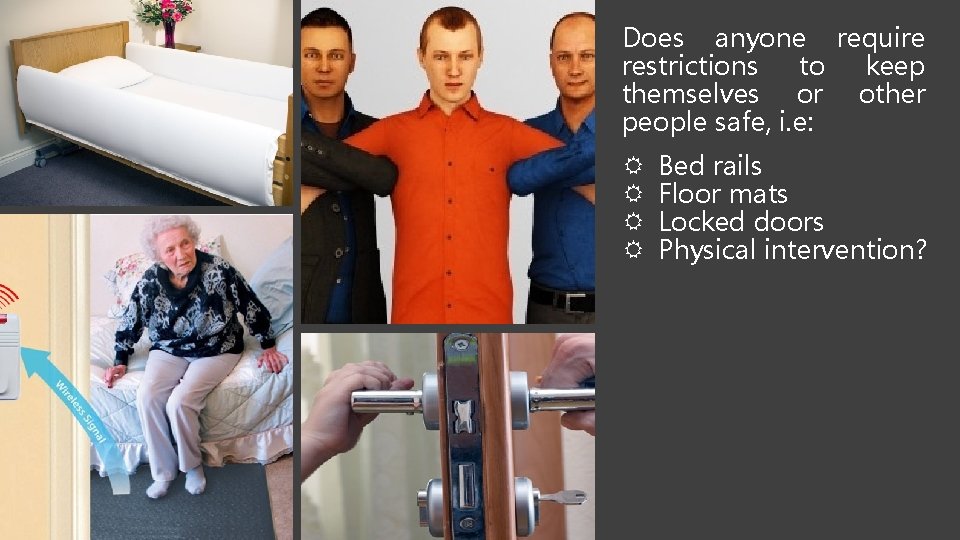
Does anyone require restrictions to keep themselves or other people safe, i. e: Bed rails Floor mats Locked doors Physical intervention?
If they lack capacity to agree to these measures has: a) this been assessed? b) has a Do. LS authorisation been applied for?
If anyone does require restrictions, are there clear protocols in place around these? Where appropriate have relevant external professionals been involved in developing these?
Are there an up to date version of relevant policies and procedures available to staff? Can you provide evidence that staff have read and understand these?
Where restrictive practices are required, is there evidence that staff have relevant and up to date training in place?
E 7: Consent to care and treatment Make sure you: Have ensure staff understand about the need for consent and decision making requirements under the Mental Capacity Act Obtain people’s consent in relation to the care and treatment they receive (both initially and on an ongoing basis) if they have the capacity to provide it promote best interest decision making when a person is assessed as lacking the capacity to make a particular
E 7: Consent to care and treatment Make sure you: Only use physical restraint when: § there is a clearly identified reason for needing to do so § the decision is made with and sanctioned by relevant external professionals § staff have received the relevant accredited training.
E 7: Consent to care and treatment Make sure you: Ensure that where any restrictive measures are put in place (including a person going to live in a care home) and the person lacks capacity toofconsent these § the a Deprivation Liberty to. Safeguard is measures applied forthat: and that CQC are notified (via a Statutory Notification) when this is in place § this is reapplied if necessary before it expires § if additional restrictions are required that these are added on to the Do. LS Anything else ?
- Slides: 66