Year 3 Neurology History Taking By Dr Amar
Year 3 Neurology History Taking By Dr Amar Sodha
Learning Schedule 1. Important components of a neurology history 2. Common presentations 3. Red flag symptoms 4. Investigations - first line and ‘gold standard’ 5. Small group teaching with more cases

The patient’s experience of the events that unfolded before… during… after… Important components in taking a neurology history Prodromal symptoms - how did they feel immediately beforehand? Collateral history - from someone who witnessed the events and their perception of before… during… after. . . , someone who knows the patient at their baseline, are they any different? Other systemic symptoms, which may seem unrelated but may be significant and a big clinical clue e. g. palpitations in collapse. Previous history of the presenting complaint - has this happened before? How has the clinical presentation changed over time? Any worse or any better? Over how long?

Case 1 - Presenting complaint “Mr Smith is 45 year old man who has been brought in by ambulance following a collapse at his desk at work”

What would you like to ask?
Colleague says “he was holding his head, then passed out, hitting the front of her face against the desk. He started jerking and wouldn’t wake History of presenting complaint and some collateral up. The jerking stopped after a few minutes and he stayed really drowsy” On arrival of the paramedics, he had improved, fully responsive and oriented Mr Smith has no memory of the event. Just that he had the worst headache he has ever had in his life! Never had seizures before and has not had any trauma recently.
Some important further history, including RED FLAGS?

Is the headache still present? – worsening or improving? Nausea/vomiting? How many times? Visual disturbance? – diplopia / decreased acuity / tunnel vision Any weakness / sensory disturbance? Episodes of bladder/bowel incontinence? Any residual confusion? Neck stiffness / photophobia? Fever/rigors ?
Still has mild headache - frontal Feels nauseous - vomited twice already Neck feels “okay”, a little bit stiff but has been lying on bed since he feels dizzy His vision is normal with no photophobia either No fevers and no weakness or sensory abnormality Remains oriented in time, place and person

PMHx - has polycystic kidney disease Important to ask about: syncope, seizures, cardiac history, intracranial haemorrhage, Completing the history malignancy Drug Hx - no regular medications Important to ask about: any drugs which may cause syncope e. g. antihypertensive, anticonvulsant medication, antiplatelets/anticoagulant medication FHx - Mum had IHD, nil other Important to ask about: seizures, syncope and IC bleeds SHx - lives with family, occasional drinker, smokes 10 a day and no recreational drugs
What system(s) would you examine?
Cardiovascular – cardiogenic syncope? Respiratory – hypoxic cause for collapse? Upper / lower limb neurology and cranial nerves – neurogenic cause for collapse? General examination – soft tissue injury/fractures
Mr Smith’s examination is normal. No abnormality detected in cardio, resp or neuro exam. He has some bruising to his forehead where he hit his head.

What are your differential diagnoses?

C ardiac Causes of collapse? R eflexes A rterial CRASH S ystemic H ead
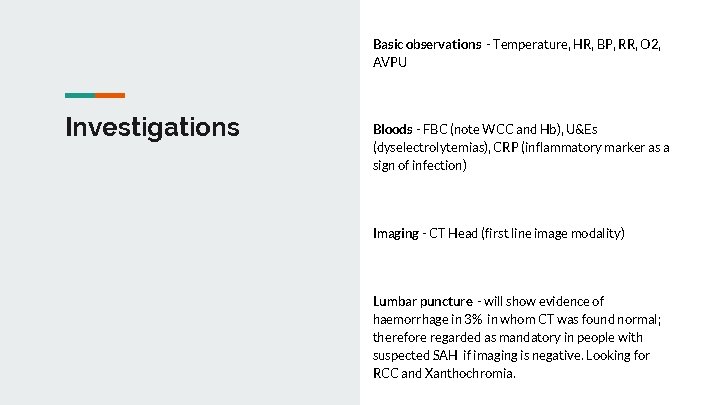
Basic observations - Temperature, HR, BP, RR, O 2, AVPU Investigations Bloods - FBC (note WCC and Hb), U&Es (dyselectrolytemias), CRP (inflammatory marker as a sign of infection) Imaging - CT Head (first line image modality) Lumbar puncture - will show evidence of haemorrhage in 3% in whom CT was found normal; therefore regarded as mandatory in people with suspected SAH if imaging is negative. Looking for RCC and Xanthochromia.
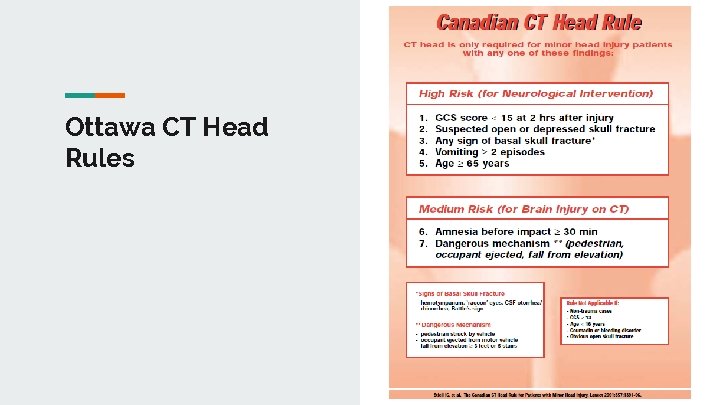
Ottawa CT Head Rules

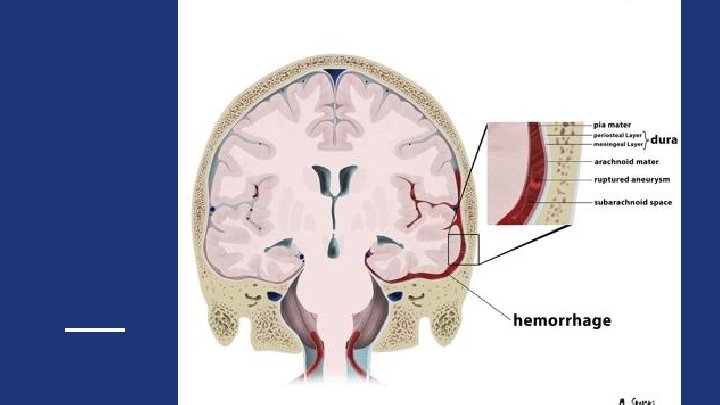
CT Scan showing SAH
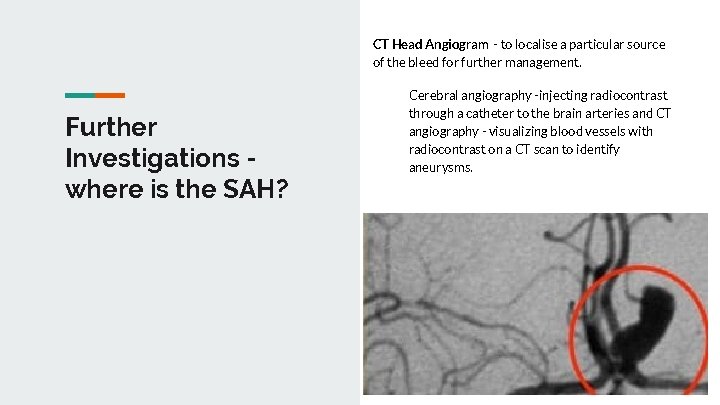
CT Head Angiogram - to localise a particular source of the bleed for further management. Further Investigations where is the SAH? Cerebral angiography -injecting radiocontrast through a catheter to the brain arteries and CT angiography - visualizing blood vessels with radiocontrast on a CT scan to identify aneurysms.
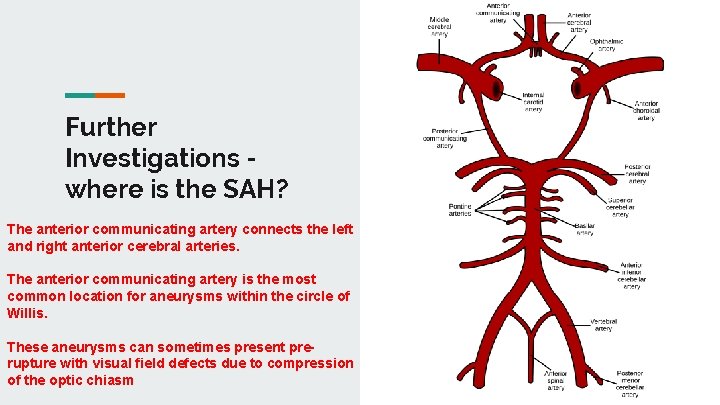
Further Investigations where is the SAH? The anterior communicating artery connects the left and right anterior cerebral arteries. The anterior communicating artery is the most common location for aneurysms within the circle of Willis. These aneurysms can sometimes present prerupture with visual field defects due to compression of the optic chiasm

What are your management options?
Coiling and Clipping Interventional Radiology This involves inserting a catheter into the femoral artery under x-ray guidance. This is then taken up through the aorta, into the carotid vessels and into the cerebral circulation. Once the aneurysm is reached, platinum coils are released into it. This causes coagulation within the aneurysm, obliterating it.
Clipping Coiling and Clipping Neurosurgery This procedure is more invasive, requiring a craniotomy to access the aneurysm. It is often used for aneurysms that have a wide neck and are therefore unsuitable for coiling. The aneurysm is located visually and a clip is placed around the neck of the aneurysm. This method is often not possible for aneurysms of vessels that are difficult to access surgically (e. g. posterior circulation).
Alternative diagnoses for Headache Establish if the headache is acute or chronic
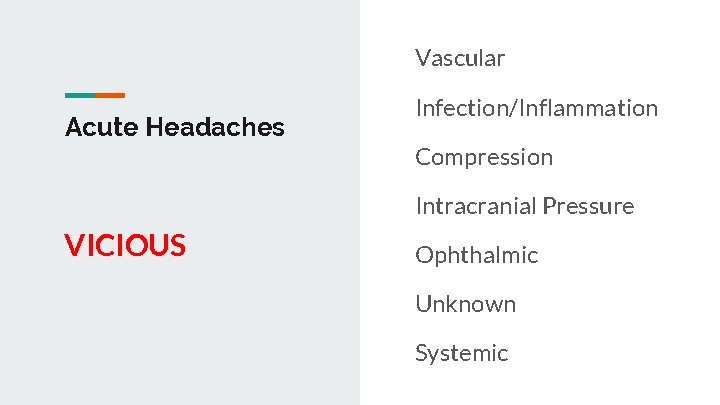
Vascular Acute Headaches Infection/Inflammation Compression Intracranial Pressure VICIOUS Ophthalmic Unknown Systemic
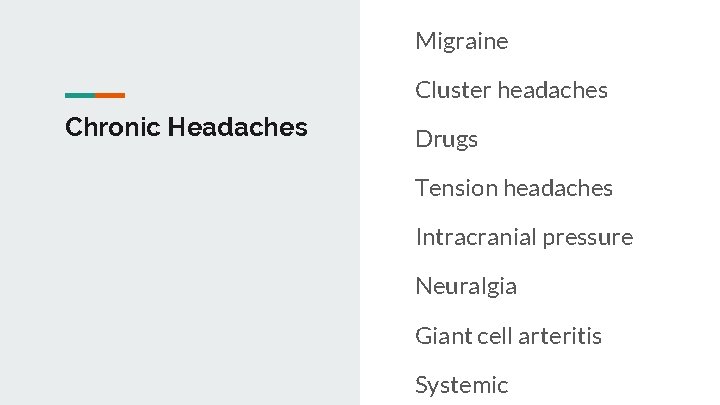
Migraine Cluster headaches Chronic Headaches Drugs Tension headaches Intracranial pressure Neuralgia Giant cell arteritis Systemic
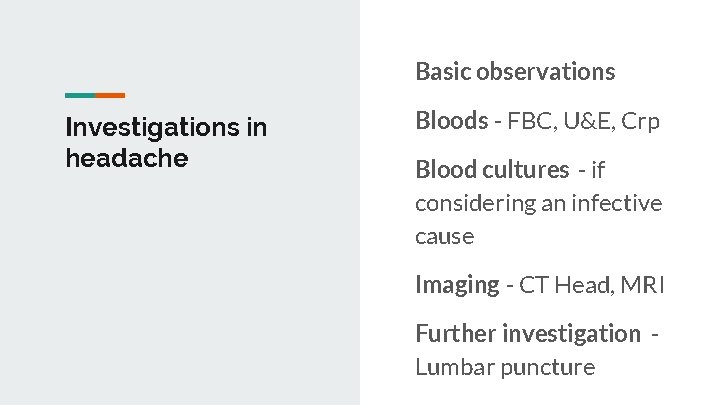
Basic observations Investigations in headache Bloods - FBC, U&E, Crp Blood cultures - if considering an infective cause Imaging - CT Head, MRI Further investigation Lumbar puncture
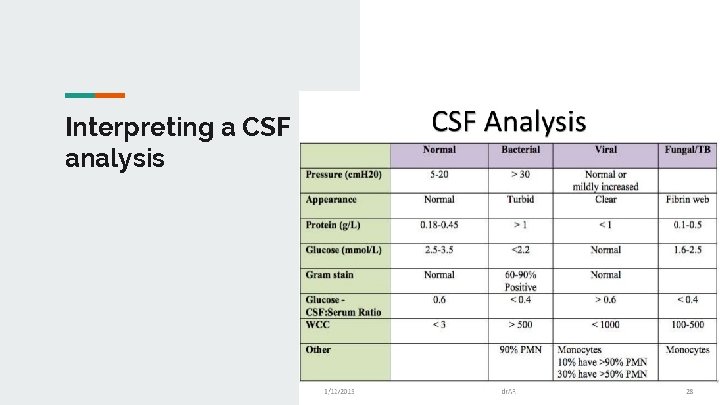
Interpreting a CSF analysis
- Slides: 29