Wound Closure Technique Professor Magdy Amin RIAD Professor












- Slides: 50

Wound Closure Technique Professor Magdy Amin RIAD Professor of Otolaryngology. Ain shames University Senior Lecturer in Otolaryngology University of Dundee
Three phases of wound healing • Three phases of wound healing have been identified and studied on the cellular and molecular level. • These 3 distinct phases, ie, inflammation, tissue formation, and tissue remodeling, depend on an elaborate cascade of growth factors and cellular components interacting in a directed manner to achieve wound closure

The inflammatory phase • The initial injury leads to the recruitment of inflammatory cells into the wound, once a clot forms in response to disrupted blood vessels. • This scenario entails a complex interaction between local tissue mediators and cells that migrate into the wound.
The inflammatory phase • The inflammatory phase occurs in the first few days as inflammatory cells migrate into the wound. • Migration of epithelial cells has been shown to occur within the first 12 -24 hours, but further new tissue formation occurs over the next 10 -14 days
Epithelialization and neovascularization • Epithelialization and neovascularization result from the increase in cellular activity. • Stromal elements in the form of extracellular matrix materials are secreted and organized.
Epithelialization and neovascularization • This new tissue, called granulation tissue, depends on specific growth factors for further organization to occur in the completion of the healing process. • This physiologic process occurs over several weeks to months in a healthy individual.
Tissue remodeling • Finally, tissue remodeling, in which wound contraction and tensile strength is achieved, occurs in the next 6 -12 months. • Systemic illness and local factors can affect wound healing. • Traditionally, at least 2 types of wound healing have been described, ie, primary intention and secondary intention.
Primary intention • In the primary intention method, surgical wound closure facilitates the biological event of healing by joining the wound edges. • Surgical wound closure directly apposes the tissue layers, which serves to minimize new tissue formation within the wound. • However, remodeling of the wound does occur, and tensile strength is achieved between the newly apposed edges.
Primary intention • Closure can serve both functional and aesthetic purposes. • These purposes include elimination of dead space by approximating the subcutaneous tissues, minimization of scar formation by careful epidermal alignment, and avoidance of a depressed scar by precise eversion of skin edges.

Primary intention • If dead space is limited with opposed wound edges, then new tissue has limited room for growth. • Correspondingly, atraumatic handling of tissues combined with avoidance of tight closures and undue tension contribute to a better result.
Secondary intention • The secondary intention method (spontaneous healing) • It can be used in lieu of complicated reconstruction for certain surgical defects. • This method also depends on the 3 stages of wound healing to achieve the ultimate result.
Absorbable sutures • Absorbable sutures are applicable to a wound that heals quickly and needs minimal temporary support. • Their purpose is to alleviate tension on wound edges. • The newer synthetic absorbable sutures retain their strength until the absorption process starts. • Nonabsorbable sutures offer longer mechanical support.
Monofilaments • Monofilaments have less drag through the tissues but are susceptible to instrumentation damage. • Infection is avoided with the monofilament, unlike the braided multifilament, which potentially can sustain bacterial inocula. • Gut is considered a monofilament
Natural materials • Natural materials include gut, silk, and even cotton. • Gut is absorbable, but cotton and silk are not. • Gut is considered a monofilament, whereas silk and cotton are braided multifilaments.
synthetic materials • The absorbable sutures include: • monofilamentous Monocryl (poliglecaprone), Maxon (polyglycolide-trimethylene carbonate), and PDS (polydioxanone). • Braided absorbable sutures include Vicryl (polyglactin) and Dexon (polyglycolic acid).
synthetic materials • Nonabsorbable sutures comprise nylon, Prolene (polypropylene), Novafil (polybutester), PTFE (polytetrafluoroethylene), steel, and polyester. • Nylon and steel sutures can be monofilaments or multifilaments. • Prolene, Novafil, and PTFE are monofilaments. • Polyester suture is braided.
Absorbable suture tensile strength • Absorbable suture materials lose their tensile strength before complete absorption. • Gut can last 4 -5 days in terms of tensile strength. In the chromic form (ie, treated in chromic acid salts), gut can last up to 3 weeks.
Absorbable suture tensile strength • Vicryl and Dexon maintain tensile strength for 7 -14 days, although complete absorption takes several months. • Maxon and PDS are considered long-term absorbable sutures, lasting several weeks and likewise requiring several months for complete absorption
Non absorbable sutures tensile strengths • Nonabsorbable sutures have varying tensile strengths and may be subject to some degree of degradation. • Silk has the lowest strength and nylon has the highest, although Prolene is comparable.

Non absorbable sutures tensile strengths • Both nylon and Prolene require extra throws to secure knots in place. • Polyester has a high degree of tensile strength, and Novafil is appreciated for its elastic properties
surgical adhesives • Use of surgical adhesives can simplify skin closure in that certain problems inherent to suture use can be avoided. • Problems (eg, reactivity, premature reabsorption) can occur with sutures and lead to an undesirable result, both cosmetically and functionally.
surgical adhesives • One substance, cyanoacrylate, has been used for 25 years and easily forms a strong flexible bond. • It can induce a substantial inflammatory reaction if implanted subcutaneously. • If used superficially on the epidermal surface, little problem with inflammation occurs
Octyl-2 -cyanoacrylate (Dermabond) • The only cyanoacrylate tissue adhesive approved by the U. S. Food and Drug Administration (FDA) for superficial skin closure. • should not be implanted subcutaneously.
Octyl-2 -cyanoacrylate (Dermabond) • Subcutaneous sutures are used to take the tension off the skin edges prior to applying the octyl-2 -cyanoacrylate. • Subcutaneous suture placement will aid in everting the skin edges and minimize the chances of deposition of cyanoacrylate into the subcutaneous tissues.
Fibrin-based tissue adhesives • Fibrin-based tissue adhesives can be created from autologous sources or pooled blood. • They are typically used for hemostasis and can seal tissues. • While they do not have adequate tensile strength to close skin, fibrin tissue adhesives can be used to fixate skin grafts or seal cerebrospinal fluid leaks.

Fibrin-based tissue adhesives • Commercial preparations such as Tisseel (Baxter) and Hemaseel (Haemacure) are FDAapproved fibrin tissue adhesives made from pooled blood sources. • These fibrin tissue adhesives are relatively strong and can be used to fixate tissues.
Fibrin-based tissue adhesives • Autologous forms of fibrin tissue adhesives can be made from patient's plasma. • The concentration of fibrinogen in the autologous preparations is less than the pooled forms; therefore, these forms have a lower tensile strength
Staples • Staples provide a fast method for wound closure and have been associated with decreased wound infection rates. • Staples are composed of stainless steel, which has been shown to be less reactive than traditional suturing material.
Staples • The act of stapling requires minimal skin penetration, and, thus, fewer microorganisms are carried into the lower skin layers. • Staples are more expensive than traditional sutures and also require great care in placement, especially in ensuring the eversion of wound edges. • However, with proper placement, resultant scar formation is cosmetically equivalent to that of other techniques

Bioabsorbable (biodegradable/bioresorbable) • • a) b) c) d) Bioabsorbable surgical devices need no removal Requirements for bioabsorbable materials; noncarcinogenic, tissue compatible, nontoxic, etc Should not cause morbidity Must provide adequate mechanical strength and stiffness Degradation should occur by hydrolysis in aqueous media
Bioabsorbable Polymers for surgical applications 1) Suture Materials - - Polyglycolid acid (PGA) and Polylactic acid (PLA) have been used as synthetic bioabsorbable sutures Bioabsorbable sutures are used in the fixation of bone fractures, closure of soft tissue wound, etc
A Typical Suture Line
Polyglycolid Acid (PGA) and Polylactic (PLA) • PGA - High molecular weight, hard, tough crystalline polymer, Tm at about 224 -226ºC, Tg of 36ºC. • PLA – Tm of 174 -184ºC, Tg of 57ºC. • Such polymers can be processed into fibers, films, rods, screws, plates, clamps, etc • Advantages of polymeric materials compared to metal and ceramics; easy and cheap to make
Bioabsorbable Polymers for surgical applications 2) Porous Composites - Combining bioabsorbable polymers in porous and nonporous materials - Hydroxyapatite powders and blocks have applications in the bone surgery, e. g. to fill the defects - Since porous ceramics are brittle, the toughness has been increased by combining them with polymers
Bioabsorbable Polymers for surgical applications 3) Drug Delivery System - Polymeric devices for the controlled release of drugs and antibiotic have been studied - These polymers show several advantages over traditional repeated dosage methods - This technique can save patients from being exposed to greater amounts of drug at the desired site of action
Bioabsorbable Polymers for surgical applications 4) Partially Bioabsorbable Device - The reinforcement of bioabsorbable polymeric matrices with biostable fibers produce strong, partially bioabsorbable materials - Example; PLA matrix reinforced with carbon fiber, copolymer MMA and Nvinylpyrrolidone reinforced polyamide fibers, etc used for ligaments, tendon,
Example of Bioabsorbable materials in artificial skin • Skin damage following severe burns or ulcers, such as diabetic foot ulcers, is notoriously difficult to heal. • This is because the dermis cells will not regenerate in the absence of a matrix on which to grow • Recently the development of tissue engineering and, in particular, artificial skin has presented advances in this area • These artificial skins (keratinocyte seeded Integra. TM, Dermagraft. TM, and Apligraft. TM which contain neonatal cells in combination with matrices formed from bovine collagen or the soluble suture materials polylactic and polyglycolic acids) provide a matrix for dermis growth and the neonatal cells contained in them produce growth factors which promote healing
3. Adhesives for medical applications • The use of surgical tissue adhesives in medicine has developed over 40 years • Traditionally, the area of tissue reattachment or repair following surgery has been dominated by sutures, staples and wiring • Recently, there is a huge potential for tissue adhesives in clinical practice

Pressure Sensitive Adhesives (PSAs) • PSAs have been used for adhering wound dressing to skin • PSAs have Tg in the range of -20 to -60ºC, which means they are soft materials at room temp. • These soft polymers are able to flow and wet out on to a surface and are able to adherence to that surface

• Pressure Sensitive Adhesives The bond formed between PSA and substrate is (PSAs) not permenant and can be broken with a measurable force • Mid-19 th century, the first adhesive plasters were used, the first aid application of dressing become more demanding, and undergone significant development • Early adhesive formulations were based on blends of natural rubber and resin. • Now PSAs were dominated by acrylic copolymer

Requirement for PSAs 1) Should be permanently and aggressively tacky, adhere with only slight finger pressure 2) Form a strong bond with surfaces 3) Sufficient cohesiveness that it can be removed without leaving a residue 4) Need to be chemically and biologically accepted to the skin-no irritation or sensitization
Requirement for PSAs 5) Adhesives must have sufficient flow to ensure intimate surface contact 6) Must be able to cope with moisture at the skin without compromising performance 7) PSAs should be easily removed with minimal trauma to the skin
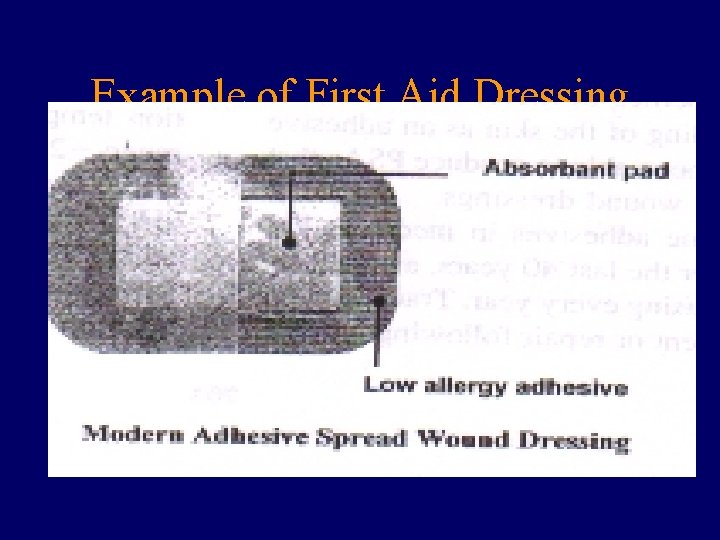
Example of First Aid Dressing
Adhesive Types Acrylic Polymer • Widely used due to natural adhesive behavior and wide scope of formulation/property tailoring • PSAs are typically copolymer composed of ‘hard’ monomer and ‘soft’ monomer • The Tg of the resultant polymer can be controlled by the ratio of hard and soft monomers
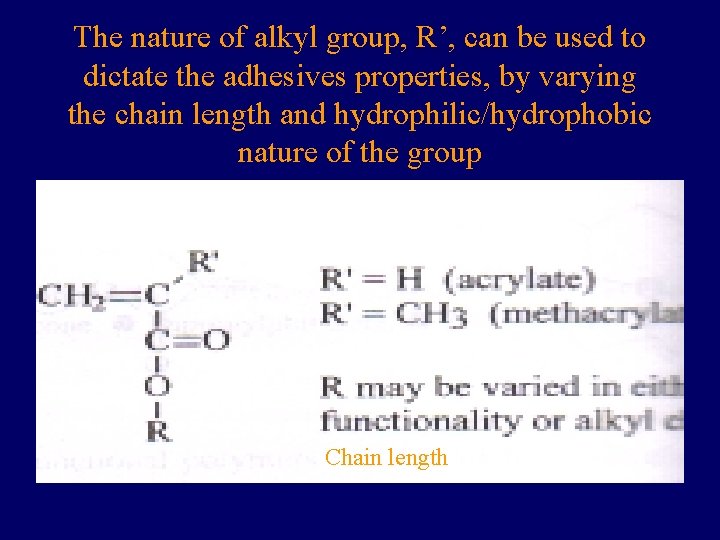
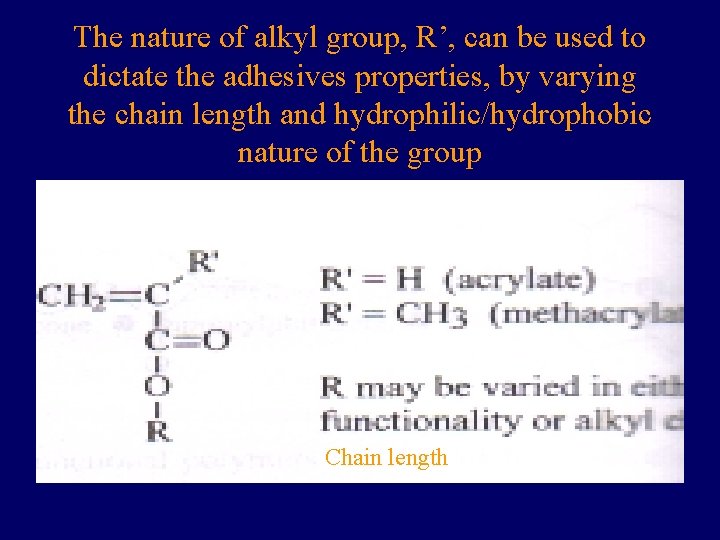
The nature of alkyl group, R’, can be used to dictate the adhesives properties, by varying the chain length and hydrophilic/hydrophobic nature of the group Chain length
Rubber-Based PSAs • Early medical adhesives were based on natural rubber • Now changed to synthetic elastomers such as polyisoprene and polyisobutylene • Polyisobutylene tend to pack tightly, results in low air and moisture permeability • The low Tg of these materials produce flexible material, that are naturally tacky, allowing the polymer to wet out the skin surface


• Silicones - Used since mid 1960, have been utilized for tapes, dressing, bandages • Typically formulated from silicone resins and polydimethyl siloxane gum • To impart cohesive strength, the polymer and resin are crosslink to form a network • The properties of the final adhesives can be controlled by ratio of component and the crosslink density

 Riad ecb
Riad ecb Riad wahby
Riad wahby Riad awwad
Riad awwad Magdy shaaban md
Magdy shaaban md Magdy selim
Magdy selim Magdy saeb
Magdy saeb Watchman flx sizing chart
Watchman flx sizing chart Watchman flx dfu
Watchman flx dfu Prep and drape
Prep and drape Amulet of wound closure
Amulet of wound closure Promotion from associate professor to professor
Promotion from associate professor to professor E.a technique (m) berhad
E.a technique (m) berhad Amin hossein rahimi
Amin hossein rahimi U ime oca i sina i svetoga duha amin
U ime oca i sina i svetoga duha amin Santral etkili sempatolitikler
Santral etkili sempatolitikler 2 metil propan
2 metil propan Php my amin
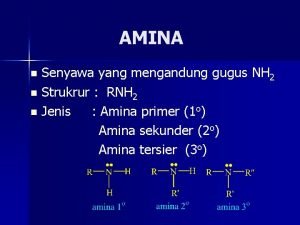
Php my amin Kuaterner amin türevleri
Kuaterner amin türevleri Project management processes
Project management processes Otrzymywanie amin
Otrzymywanie amin Amin azad
Amin azad Athar mahmood
Athar mahmood Jasmine amin chelsea
Jasmine amin chelsea Who founded shintoism
Who founded shintoism Realativ
Realativ Husseini
Husseini Mekanisme reaksi diazotasi
Mekanisme reaksi diazotasi Ghazala amin
Ghazala amin Grace amin
Grace amin Ftalimit deneyi
Ftalimit deneyi Amin kheradmand
Amin kheradmand Contoh urf
Contoh urf đốt amin
đốt amin Qasim amin
Qasim amin Amin rashidi
Amin rashidi Ghazala amin
Ghazala amin Goplar
Goplar Amin thai
Amin thai Pak amin membeli beras di pasar termasuk kegiatan
Pak amin membeli beras di pasar termasuk kegiatan Narrative review vs systematic review
Narrative review vs systematic review Glutamat nedir
Glutamat nedir Amin alipour
Amin alipour Etil propilamina
Etil propilamina Raptor
Raptor Transitive reflexive closure
Transitive reflexive closure Lane closure system
Lane closure system Project closure analysis
Project closure analysis Symmetric relation
Symmetric relation End closure mounting
End closure mounting Chin pik kee
Chin pik kee Set dialogue closure
Set dialogue closure