WOUND CARE AND SUTURING IN THE EMERGENCY DEPARTMENT



- Slides: 37
WOUND CARE AND SUTURING IN THE EMERGENCY DEPARTMENT Dr. Sinead Fitzpatrick, Dr. Termizi Hassan Antrim Area Hospital February 2016
Wound: Definition • DEFINITION: A wound is a bodily injury caused by physical means, with disruption of the normal continuity of structures. • This can be identified as an acute or a chronic wound. • ACUTE: Heals in approximately 2 weeks to 6 months • CHRONIC: Takes 6 months or more.
Classification of the accidental wound based on the mechanism �I. Mechanical 1. Abraded wound (vulnus abrasum) 2. Punctured wound (v. punctum) 3. Incised wound (v. scissum) 4. Cut wound (v. caesum) 5. Crush wound (v. contusum) 6. Torn wound (v. lacerum) 7. Bite wound (v. morsum) 8. Shot wound (v. sclopetarium) �II. Chemical 1. Acid 2. Base �III. Wound cause by radiation. �IV. Wound caused by thermal forces 1. Burning 2. Freezing �V. Special 3
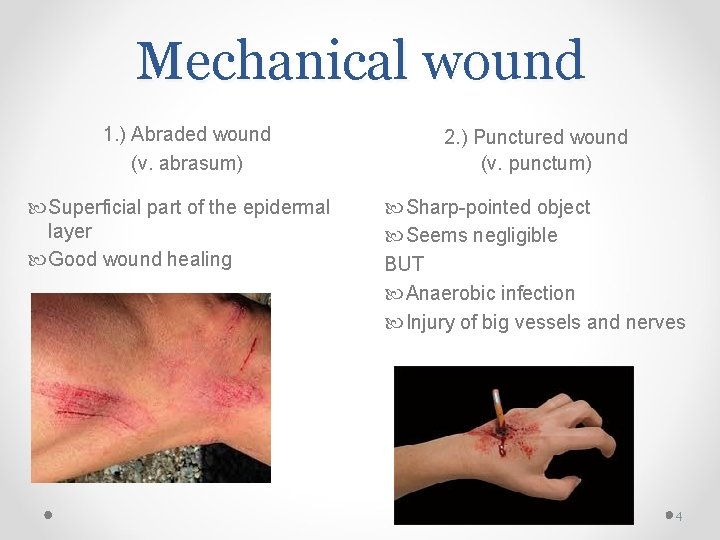
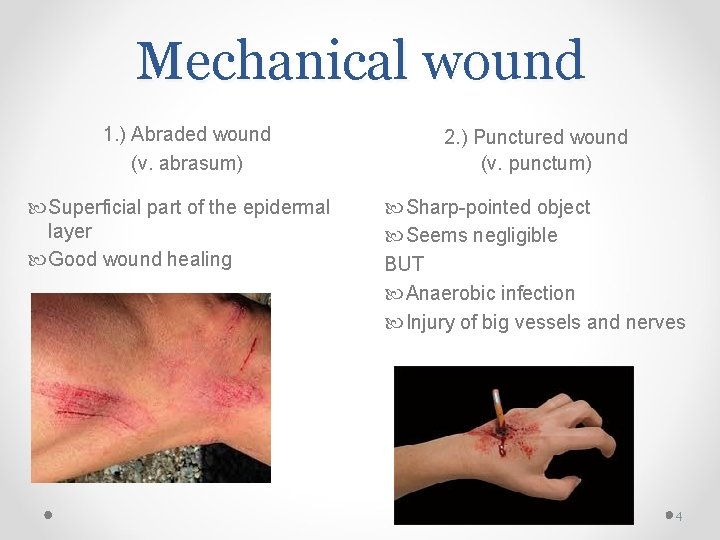
Mechanical wound 1. ) Abraded wound (v. abrasum) Superficial part of the epidermal layer Good wound healing 2. ) Punctured wound (v. punctum) Sharp-pointed object Seems negligible BUT Anaerobic infection Injury of big vessels and nerves 4

Mechanical wound 3. ) Incised wound (v. scissum) • Sharp object • Best healing 4. ) Cut wound (v. caesum) • Sharp object + blunt additional force • Edges - uneven 5
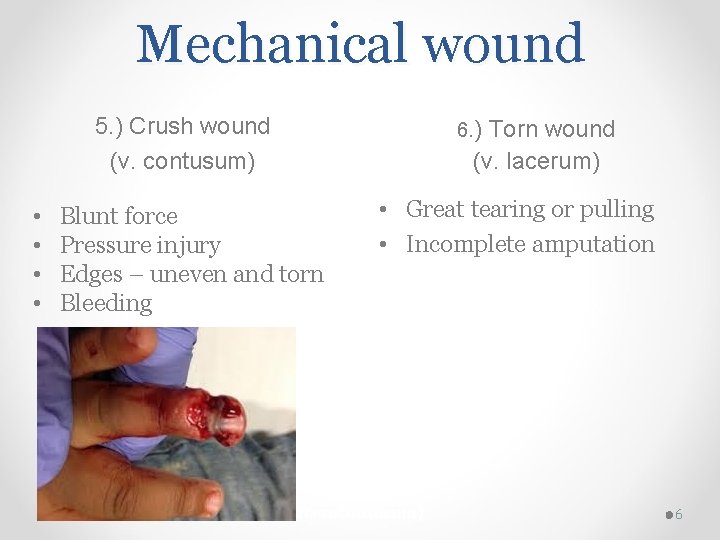
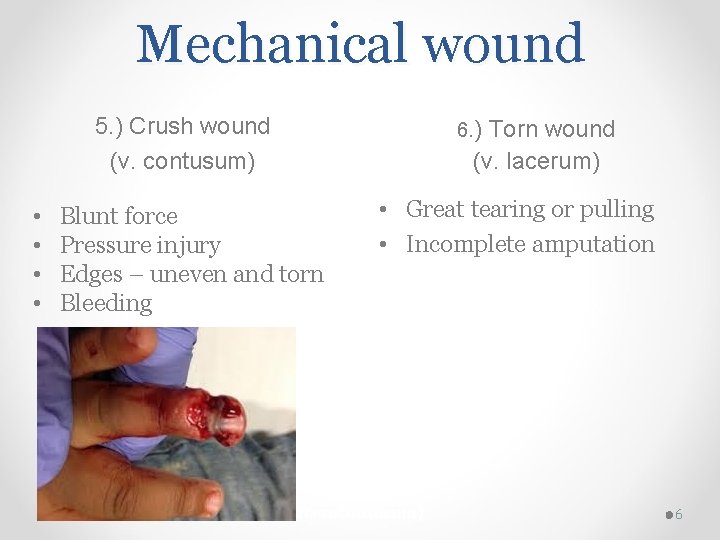
Mechanical wound 5. ) Crush wound (v. contusum) • • Blunt force Pressure injury Edges – uneven and torn Bleeding 6. ) Torn wound (v. lacerum) • Great tearing or pulling • Incomplete amputation (v. lacerocontusum) 6
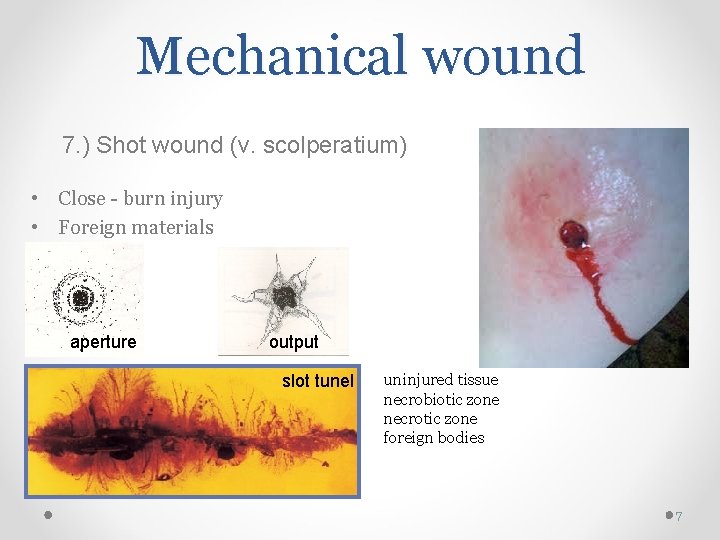
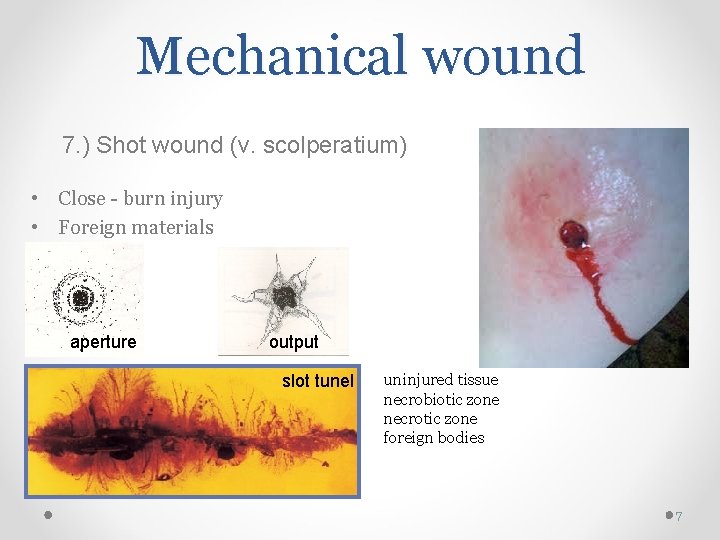
Mechanical wound 7. ) Shot wound (v. scolperatium) • Close - burn injury • Foreign materials aperture output slot tunel uninjured tissue necrobiotic zone necrotic zone foreign bodies 7
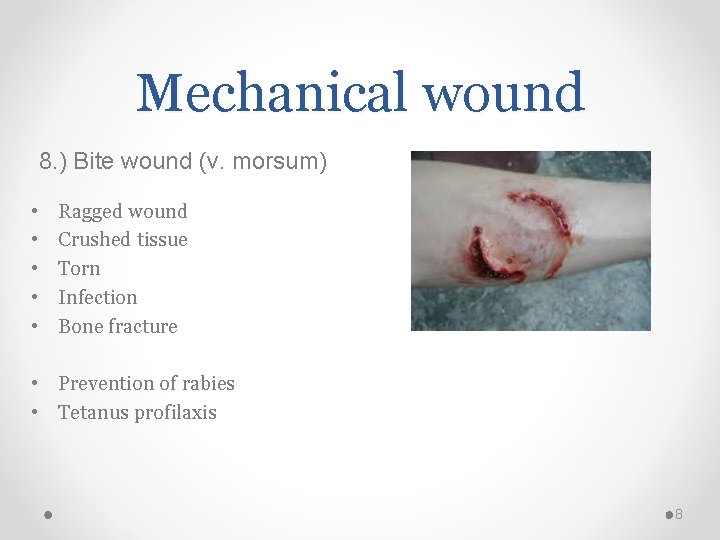
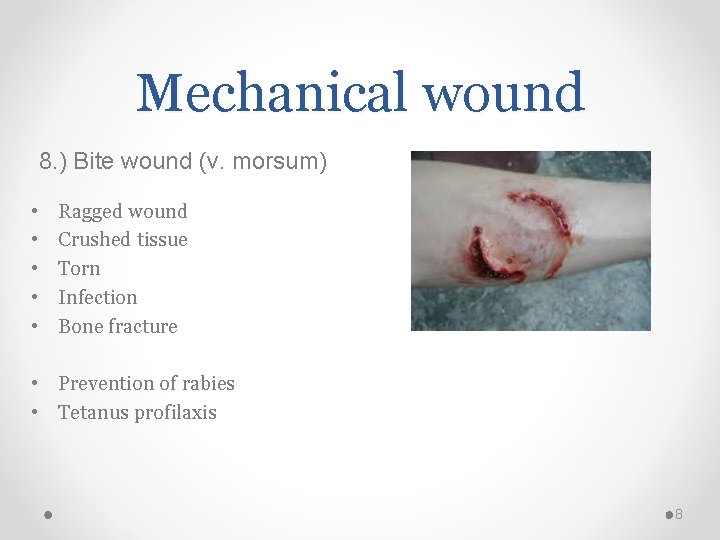
Mechanical wound 8. ) Bite wound (v. morsum) • • • Ragged wound Crushed tissue Torn Infection Bone fracture • Prevention of rabies • Tetanus profilaxis 8
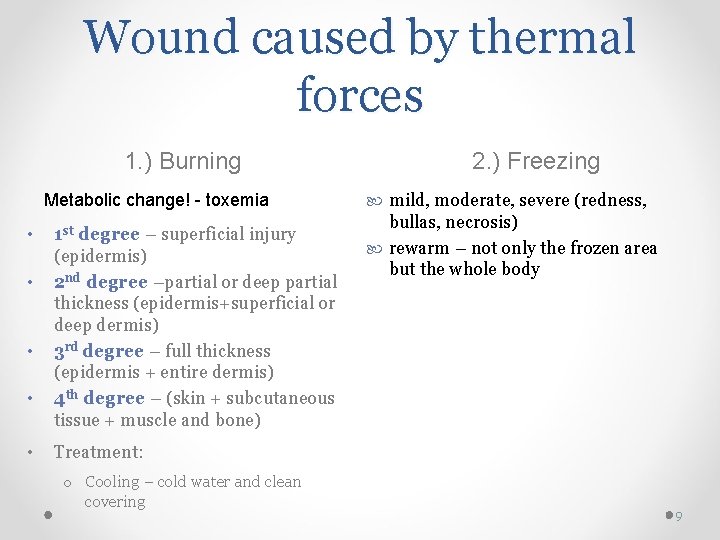
Wound caused by thermal forces 1. ) Burning Metabolic change! - toxemia • • • 1 st degree – superficial injury (epidermis) 2 nd degree –partial or deep partial thickness (epidermis+superficial or deep dermis) 3 rd degree – full thickness (epidermis + entire dermis) 4 th degree – (skin + subcutaneous tissue + muscle and bone) 2. ) Freezing mild, moderate, severe (redness, bullas, necrosis) rewarm – not only the frozen area but the whole body Treatment: o Cooling – cold water and clean covering 9
Wound classification: According to the bacterial contamination • • Clean wound Clean-contaminated wound Contaminated wound Heavily contaminated wound 10
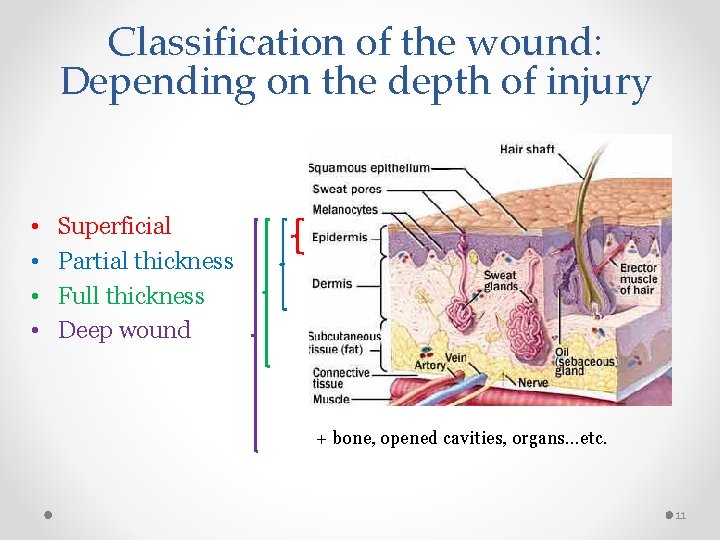
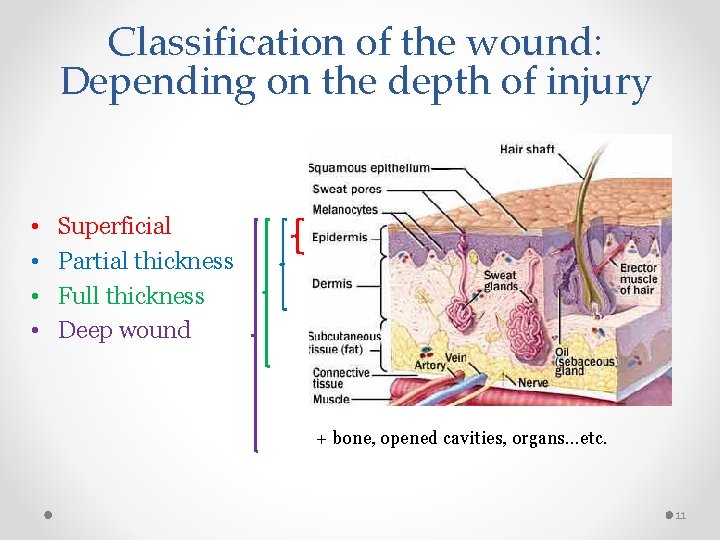
Classification of the wound: Depending on the depth of injury • • Superficial Partial thickness Full thickness Deep wound + bone, opened cavities, organs…etc. 11

Factors that impair wound healing 1. Age 2. Malnutrition 3. Obesity/Emaciation 4. Poor circulation and oxygenation 5. Immunosuppression 6. Smoking 7. Incontinence 8. Medications (steroid) 9. Co-morbidities ( Diabetes) 10. Wound Stress 11. Radiation
Promotion of wound healing • • Dressings: keep wound covered & clean Wound bed moist / Surrounding skin dry Debridement when necessary Remove exudate: o Drains, o Wound VAC, o Irrigation • Pack wounds loosely • Nutritional interventions
Wound infection • Tetanus prone wound o Heavily contaminated wound o Devitalized wound o Infection o Wound > 6 hours o Puncture wound o Animal bites • Bacteria infection are likely- (treat with coamixoclav) o Puncture woundcat/human/dog o Hand wound o Wound > 24 hours o Wounds in Alcoholics, diabetic & immunocompromised • Likely organism o Eikenella corrodens(human bites) o Pasteurella multicoda (cats)
Approach to wound management
History: Key questions • What caused the wound? (glass/knife can cause a deep injury) • Was there a crush component? (considerable swelling may ensue) • Where did it occur? (contaminated or clean environment) • Was broken glass/china involved? (if so, obtain an x-ray) • When did it occur? ( old wound may need delay closure and antibiotic) • Who caused it? (is patient safe to go home) • Is tetanus cover required?
The ABCDE in the injured assessment The mnemonic ABCDE is used to remember the order of assessment with the purpose to treat first that kills first. • • • A: Airway and C-spine stabilization B: Breathing C: Circulation D: Disability E: Environment and Exposure 17
Wound assessment 1. Look at the whole patient not just the hole. 2. Look the appearance of the wound: granulation tissues, eschar, slough, edema, sinus tract, color, tunneling etc 3. Drainage: serous, serosanguineous, purulent AND amount 4. Size & location on body 5. Presence of sutures or staples 6. Presence of drains or tubes 7. Wound edges 8. Other factors: mechanism of injury, need for tetanus booster or IVIG, onset of injury & previous treatment
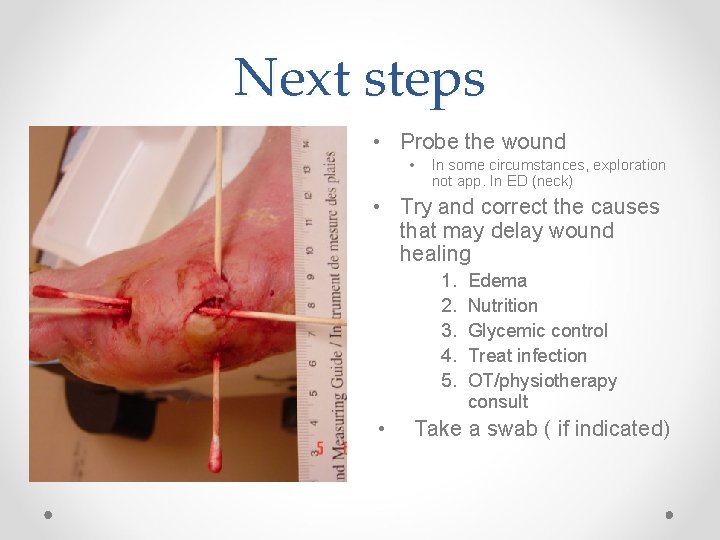
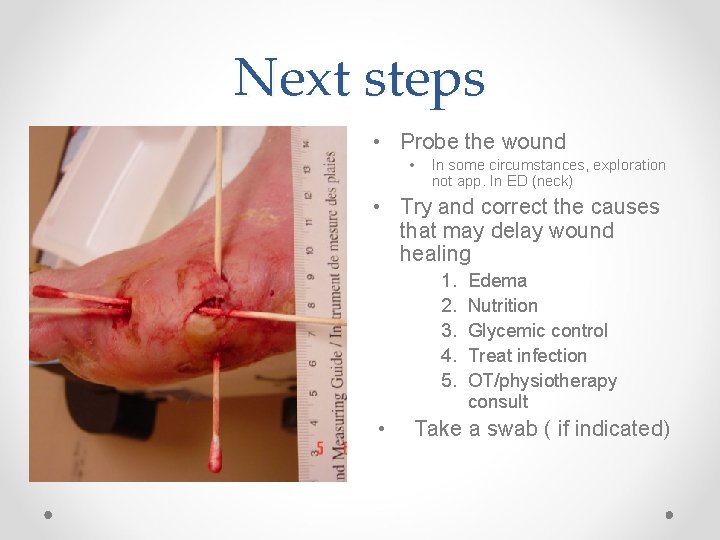
Next steps • Probe the wound • In some circumstances, exploration not app. In ED (neck) • Try and correct the causes that may delay wound healing 1. 2. 3. 4. 5. • Edema Nutrition Glycemic control Treat infection OT/physiotherapy consult Take a swab ( if indicated)
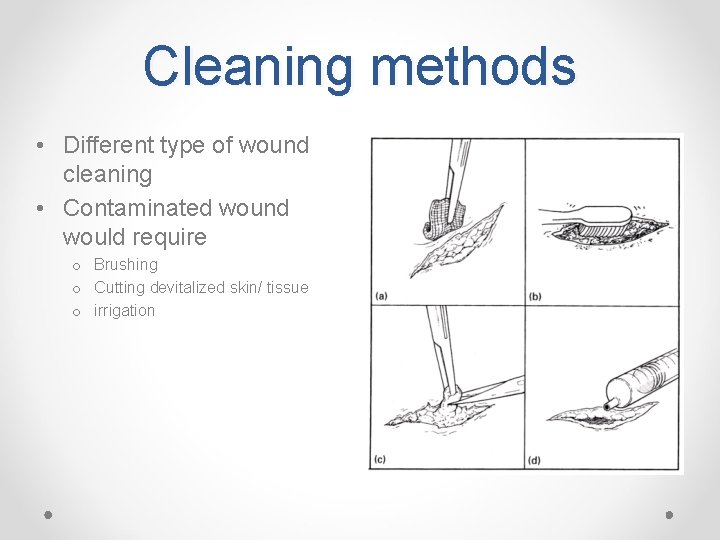
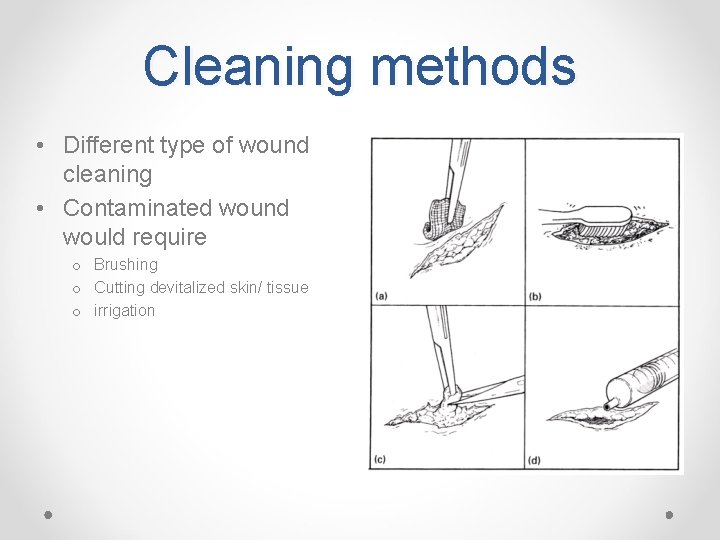
Cleaning methods • Different type of wound cleaning • Contaminated wound would require o Brushing o Cutting devitalized skin/ tissue o irrigation
Wound Cleaning: Irrigation • • Cleanses a wound using pressure Using sterile normal saline Normal Saline Avoids caustic agents such as peroxide, iodine etc Technique: • Irrigate with 19 G needle attached to 20 -30 ml syringe • 5 -15 PSI • Devitalized or grossly contaminated wound edges usually need to be trimmed back
Management of wound: Tissue unifying Skin: o Stiches o Clips o Steri-Strips o Tissue glues Fascia and subcutaneous layers: o Interrupted stiches 22
Wound closure: Principles Preparation is important: • Comfortable patient & operator • Consent • Good light & instruments • Good anesthesia- 1% vs 2% lidocaine, + adrenaline • Assistance • Correct needle & suture • Post wound care including leaflet
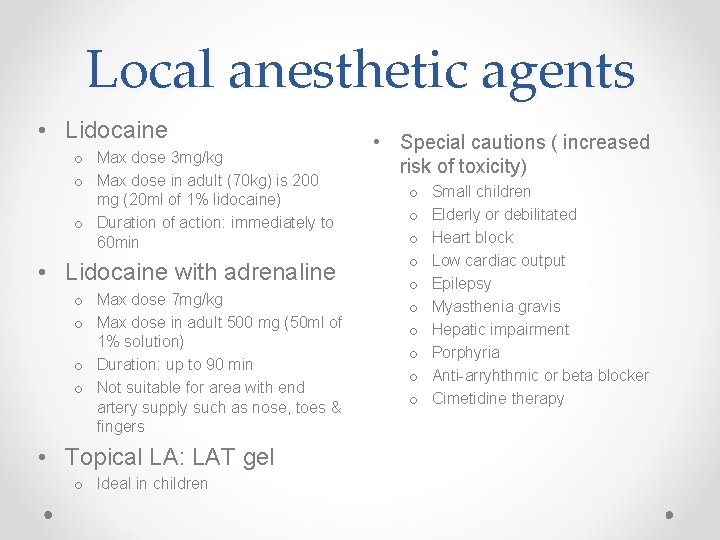
Local anesthetic agents • Lidocaine o Max dose 3 mg/kg o Max dose in adult (70 kg) is 200 mg (20 ml of 1% lidocaine) o Duration of action: immediately to 60 min • Lidocaine with adrenaline o Max dose 7 mg/kg o Max dose in adult 500 mg (50 ml of 1% solution) o Duration: up to 90 min o Not suitable for area with end artery supply such as nose, toes & fingers • Topical LA: LAT gel o Ideal in children • Special cautions ( increased risk of toxicity) o o o o o Small children Elderly or debilitated Heart block Low cardiac output Epilepsy Myasthenia gravis Hepatic impairment Porphyria Anti-arryhthmic or beta blocker Cimetidine therapy
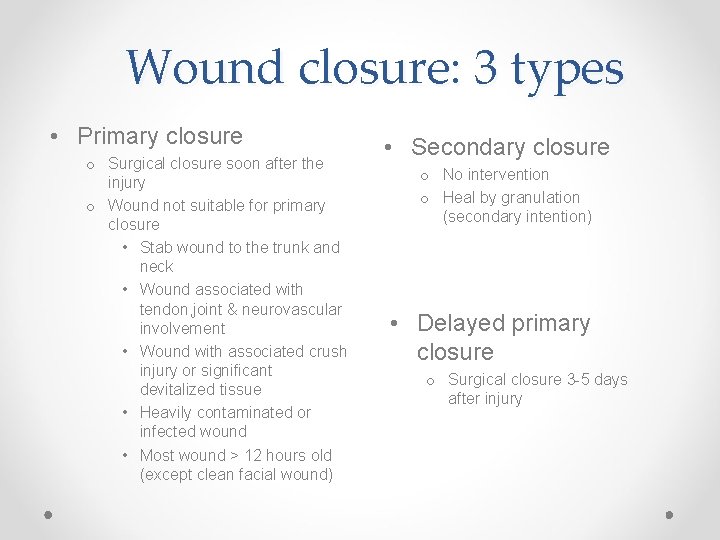
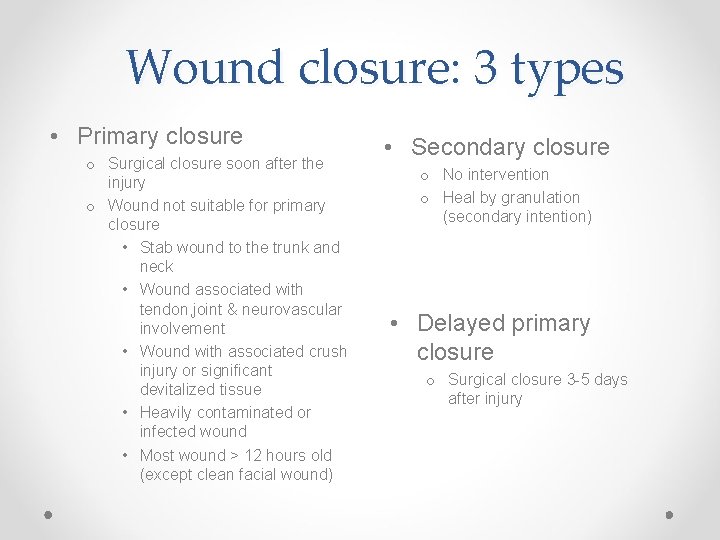
Wound closure: 3 types • Primary closure o Surgical closure soon after the injury o Wound not suitable for primary closure • Stab wound to the trunk and neck • Wound associated with tendon, joint & neurovascular involvement • Wound with associated crush injury or significant devitalized tissue • Heavily contaminated or infected wound • Most wound > 12 hours old (except clean facial wound) • Secondary closure o No intervention o Heal by granulation (secondary intention) • Delayed primary closure o Surgical closure 3 -5 days after injury
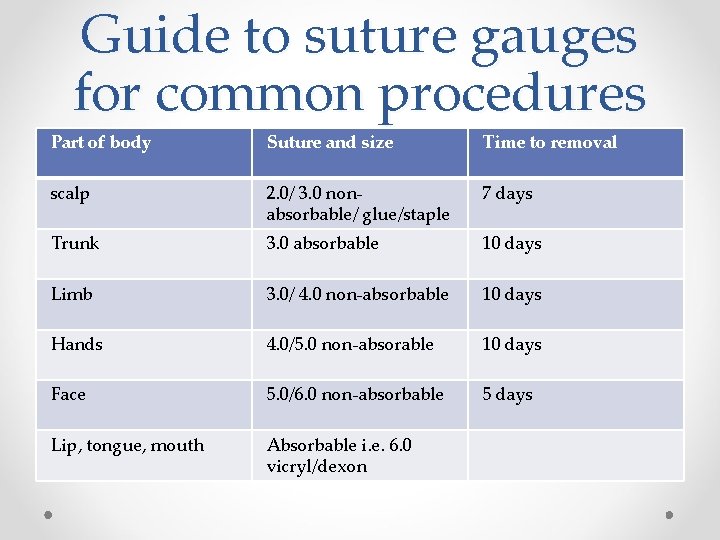
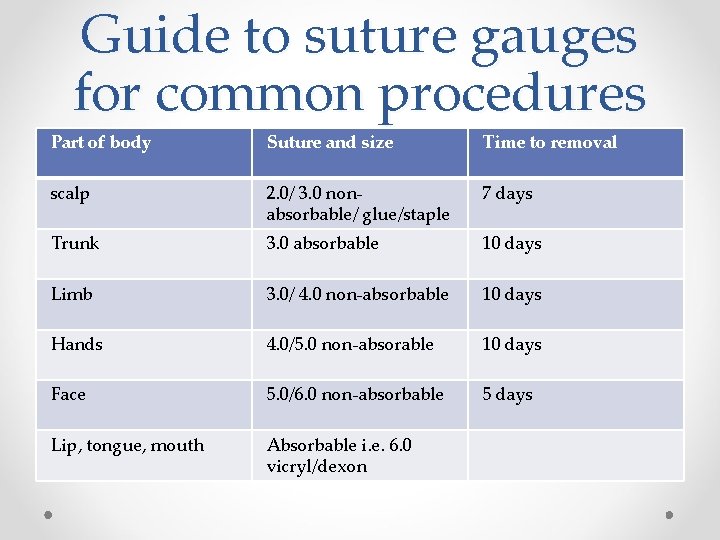
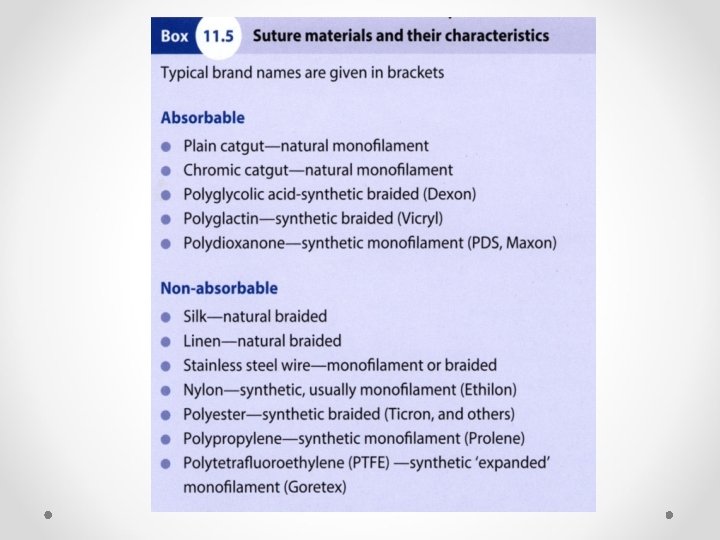
Guide to suture gauges for common procedures Part of body Suture and size Time to removal scalp 2. 0/ 3. 0 nonabsorbable/ glue/staple 7 days Trunk 3. 0 absorbable 10 days Limb 3. 0/ 4. 0 non-absorbable 10 days Hands 4. 0/5. 0 non-absorable 10 days Face 5. 0/6. 0 non-absorbable 5 days Lip, tongue, mouth Absorbable i. e. 6. 0 vicryl/dexon
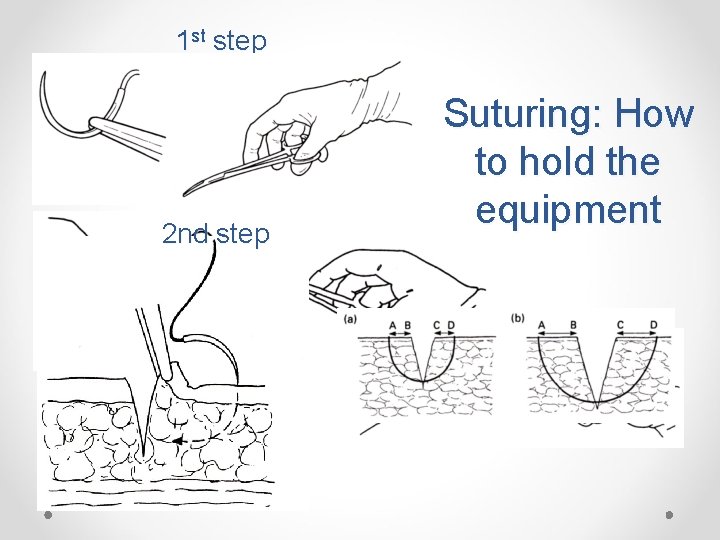
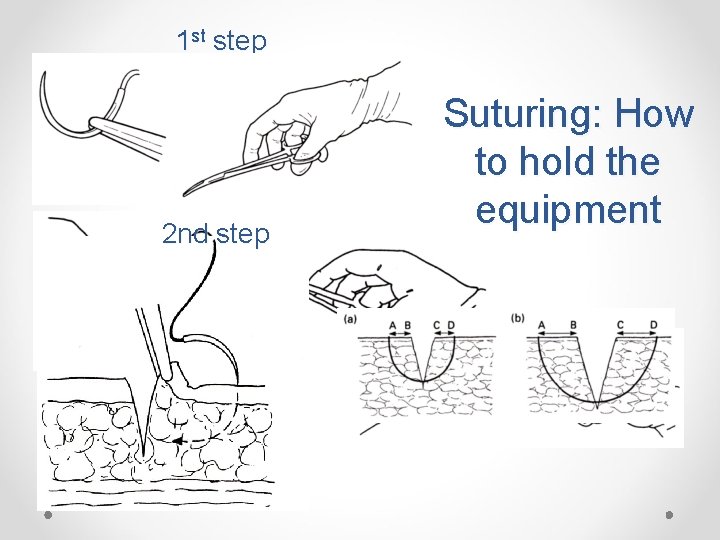
1 st step 2 nd step Suturing: How to hold the equipment

Suturing 3 rd step 4 th step
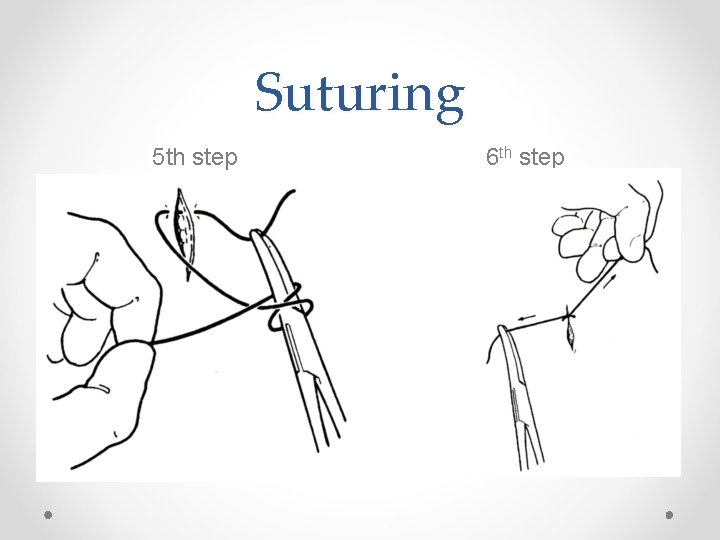
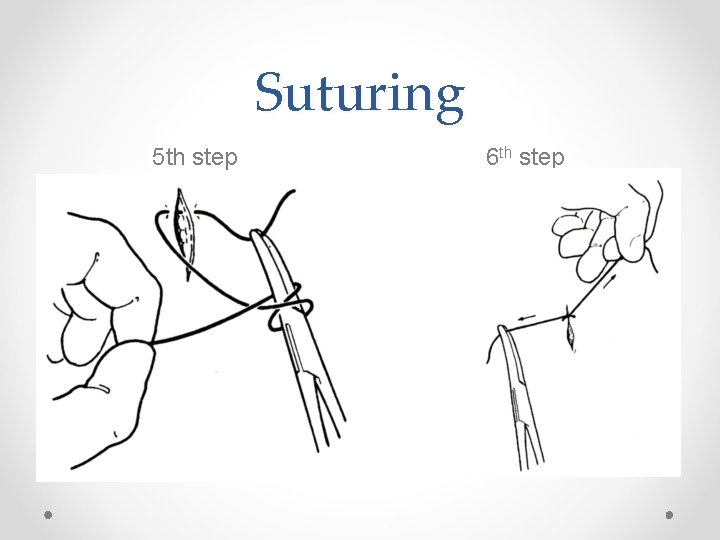
Suturing 5 th step 6 th step
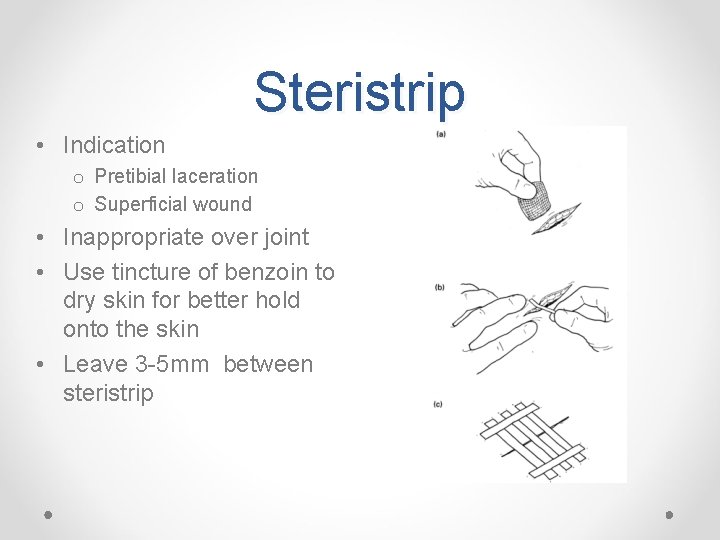
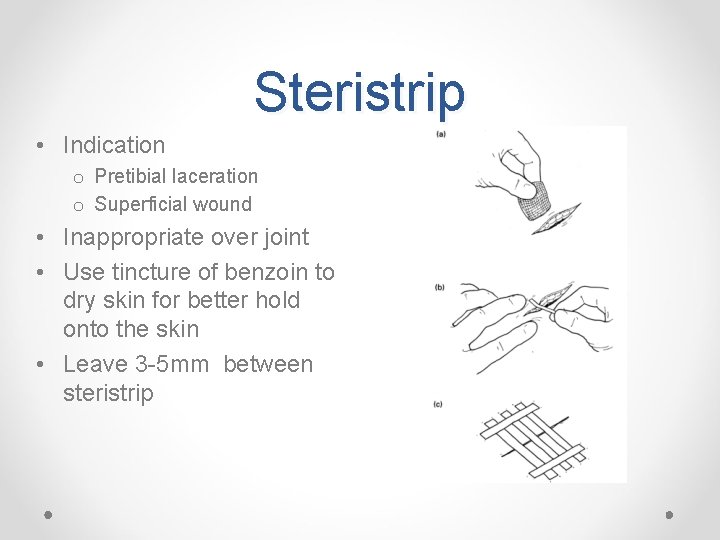
Steristrip • Indication o Pretibial laceration o Superficial wound • Inappropriate over joint • Use tincture of benzoin to dry skin for better hold onto the skin • Leave 3 -5 mm between steristrip
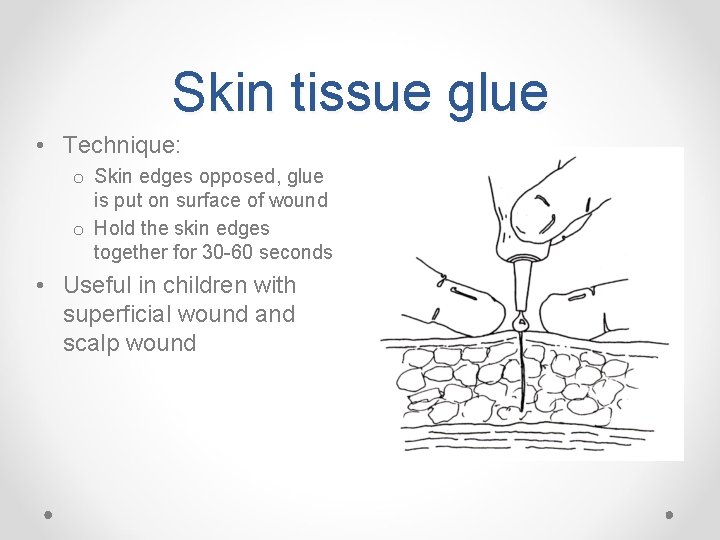
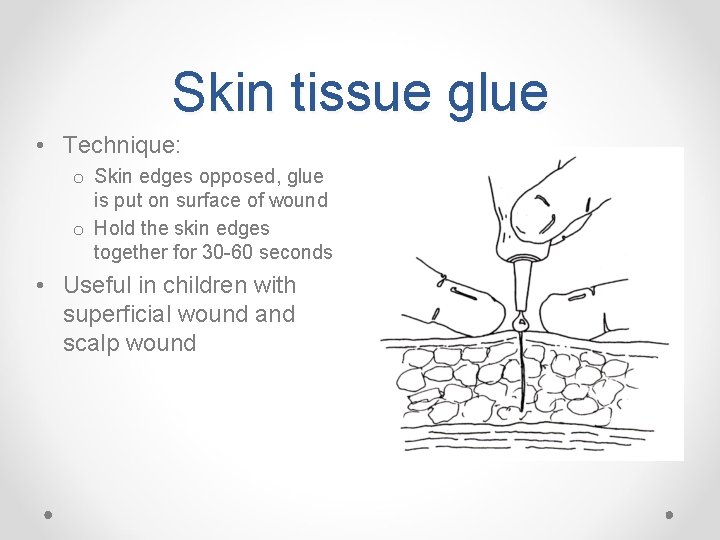
Skin tissue glue • Technique: o Skin edges opposed, glue is put on surface of wound o Hold the skin edges together for 30 -60 seconds • Useful in children with superficial wound and scalp wound
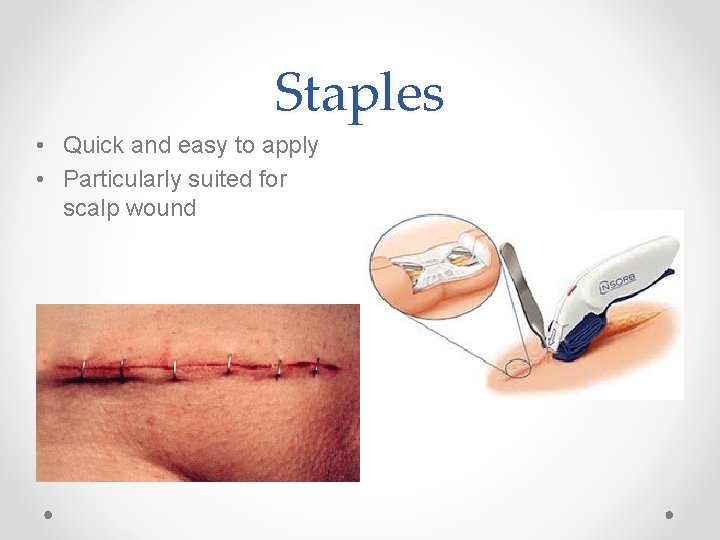
Staples • Quick and easy to apply • Particularly suited for scalp wound
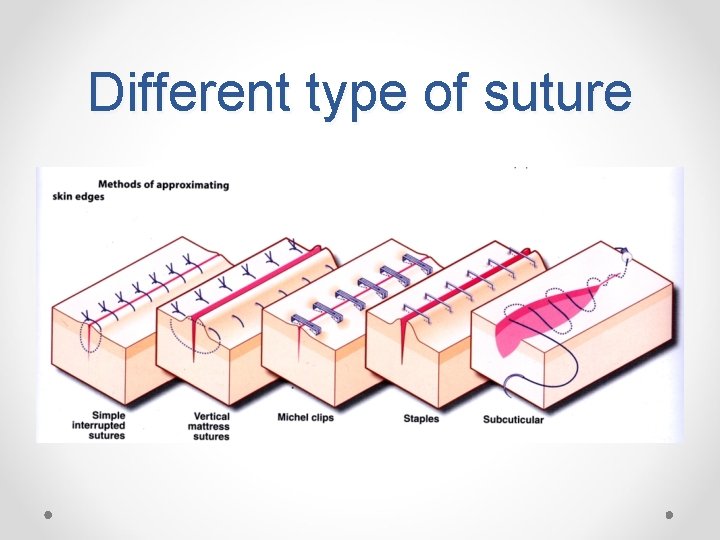
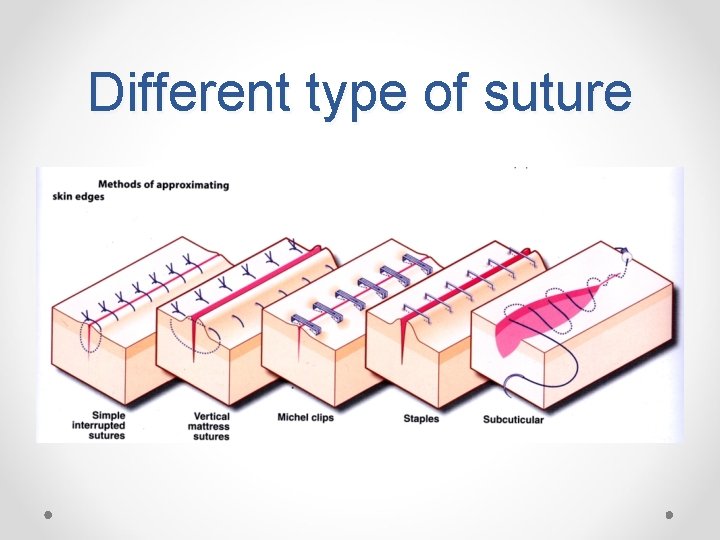
Different type of suture
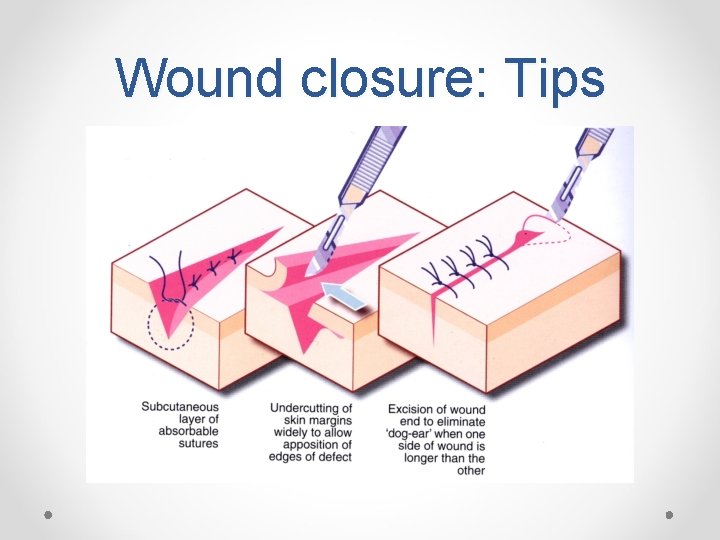
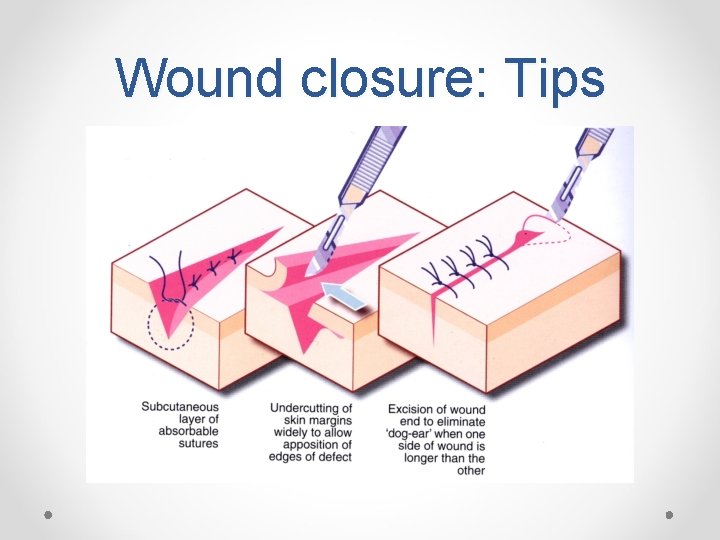
Wound closure: Tips
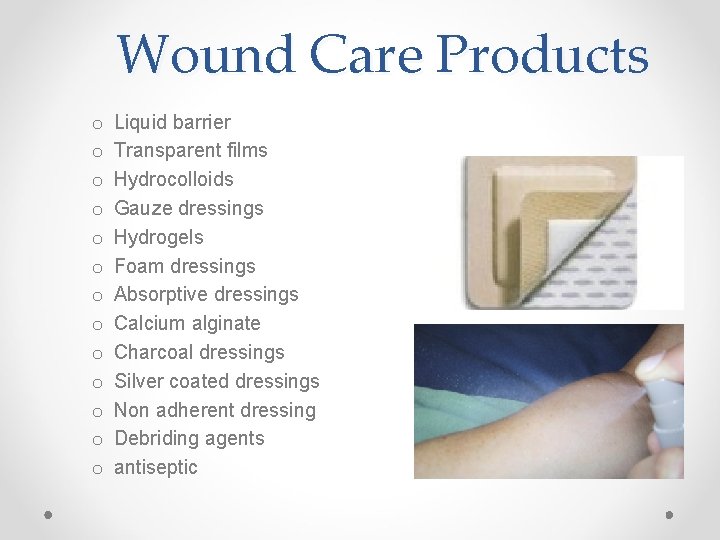
Wound Care Products o o o o Liquid barrier Transparent films Hydrocolloids Gauze dressings Hydrogels Foam dressings Absorptive dressings Calcium alginate Charcoal dressings Silver coated dressings Non adherent dressing Debriding agents antiseptic
Summary • Focused history and detailed assessment of the wound is vital • Consider antibiotic in high risk patients • Consider rabies infection (patient returning from abroad/ animal bites) • Check tetanus status o Tetanus prone wound may need tetanus immunoglobulin • Think of the possibility of FB (X-ray/ US/ CT/ MRI) • Post wound care is important o Leaflet o Informed patient of possible/risk of complication o Analgesia