WOUND BIOBURDEN AND INFECTION Dr Kanwal Fatima LEC6
WOUND BIOBURDEN AND INFECTION Dr. Kanwal Fatima LEC-6
• Human body is in constant contact with multiple microorganisms • A balance exists between host resistance and microbial growth. Infection occurs when this equilibrium is upset • Skin colonizers, or normal flora, serve a protective function too. • Commensal relationship. • Breaks in the skin, including wounds, allow microorganisms to access deeper tissue • Host responses a) Nonspecific host response b) Specific host response
• a) Nonspecific host response • Endogenous mediators Exogenous mediators • Contamination and colonization of a wound with microorganisms doesn’t constitute infection.
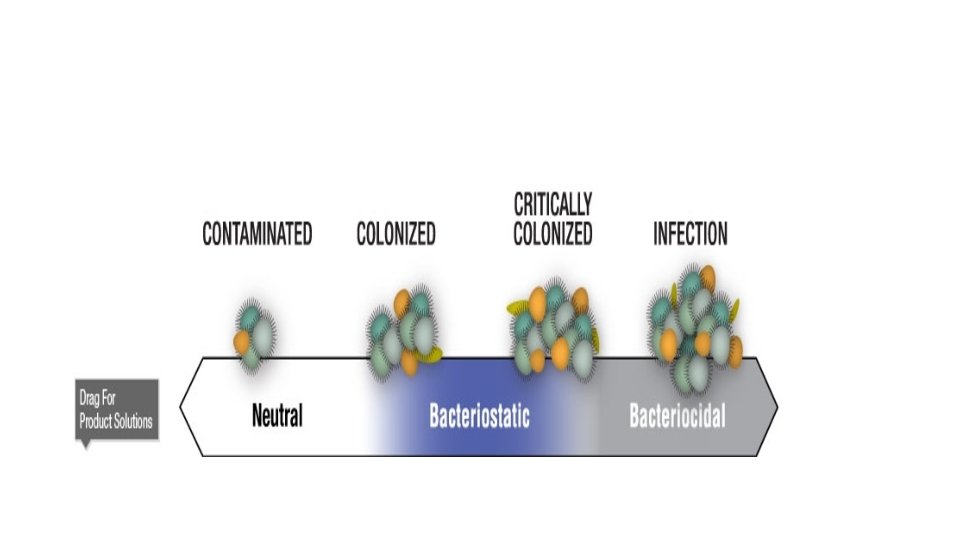
Bioburden • CONTAMINATION – • presence of non-replicating microorganisms on wound surface –not causing a clinical response • COLONIZATION – • presence of replicating micro-organisms attached to wound surface without host injury –and wound healing continues to heal predictably
• CRITICAL COLONIZATION • involves replicating microbial burden in the wound surface compartment –without signs of wound injury and delayed healing • WOUND INFECTION • refers to multiplying microorganisms within a deep compartment of the wound –clinical signs of infection are detectable
WOUND INFECTION • Wound infection: the invasion and multiplication of microbes in wound tissue resulting in pathophysiologic effects or tissue injury • Wound infection is not a phenomenon of necrotic tissue or wound debris but occurs in viable tissue • Wound infection occurs in wound tissue–not on the surface of the wound • the inflammatory response to bacteria may be influenced by • age, • diabetes, • tissue perfusion • oxygenation, • other aspects of immunocompetence • anti-infl ammatory drug use.
4 classic signs of infection • The classic signs of infection • are pain, erythema, edema, heat, (signs of inflammation) and purulent exudate. • The classic signs and symptoms of infection are believed to be reliable indicators of infection in acute wounds such as surgical incisions.
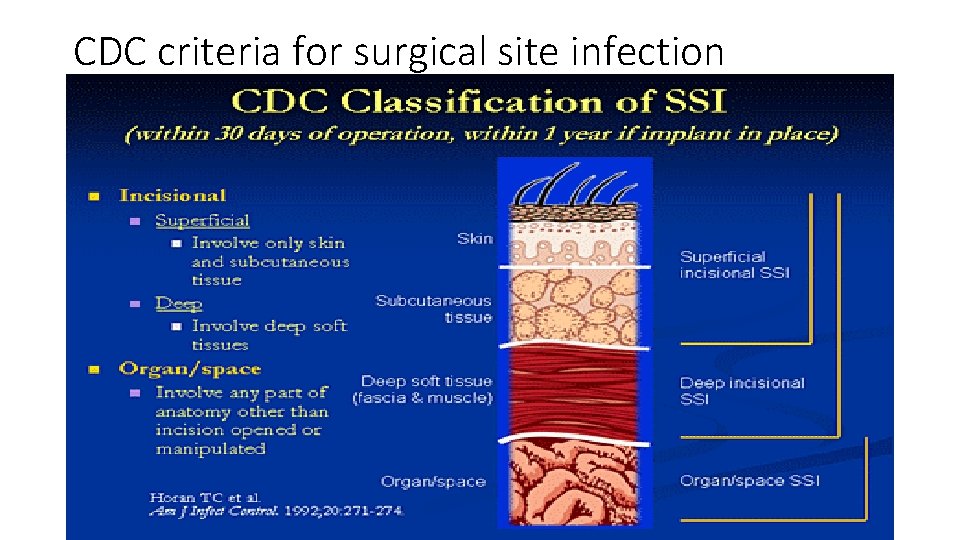
CDC criteria for surgical site infection
Signs of infection associated with chronic wounds 1. 2. 3. 4. 5. Increased serous drainage/inflammation Increased tenderness or pain Friable/bleeding granulation tissue Foul odor Increased wound breakdown with increased size & satellite areas of new ulceration 6. Delayed healing
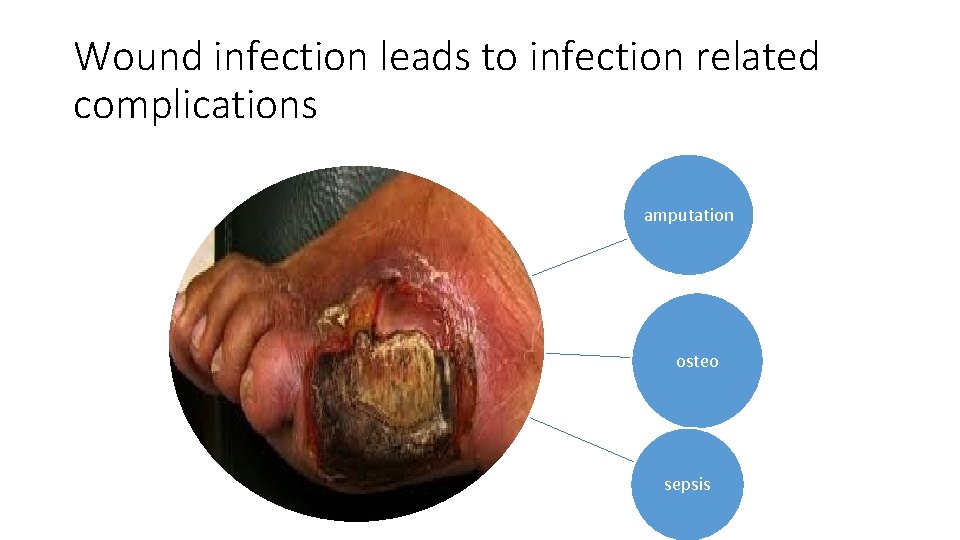
Wound infection leads to infection related complications amputation osteo sepsis
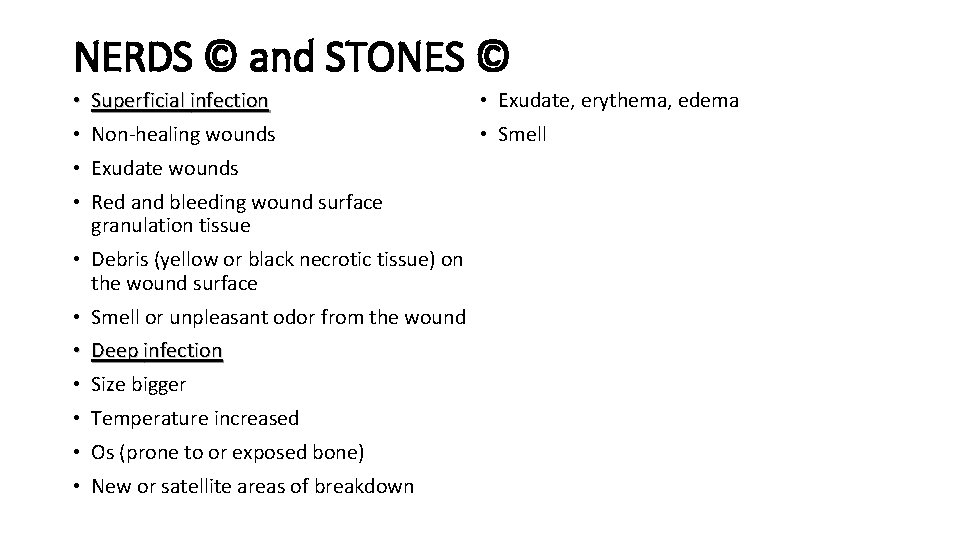
NERDS © and STONES © • Superficial infection • Non-healing wounds • Exudate wounds • Red and bleeding wound surface granulation tissue • Debris (yellow or black necrotic tissue) on the wound surface • Smell or unpleasant odor from the wound • Deep infection • Size bigger • Temperature increased • Os (prone to or exposed bone) • New or satellite areas of breakdown • Exudate, erythema, edema • Smell
Diagnostic tests of wound bioburden • Quantitative cultures • Qualitative cultures
MANAGING WOUND BIOBURDEN • CLEANING AGENTS • CLEANING DEVICES • ANTIMICROBIAL THERAPY
Wound cleaning • The management of wounds should be based on a consideration of the bioburden. • a process that removes less adherent inflammatory contaminants from the wound surface and renders the wound less conducive to microbial growth. • Effective wound cleaning requires selection of methods that minimize chemical and mechanical trauma to wound tissue while removing surface debris and contaminants.
CLEANING AGENTS • The usefulness of specific agents to correct host factors depends on a balance between their antibacterial properties and their cytotoxicity to wound healing cells, such as white blood cells (WBCs) and fibroblasts. • For the majority of wounds, isotonic saline is adequate to clean the wound surface. • If the wound surface is heavily laden with surface debris, a commercial wound cleaner may be used. • These agents contain surface-active agents that by the nature of their chemical polarity break the bonds that attach wound contaminants. • skin cleaners, which are formulated to break the chemical bonds that bind fecal matter to the skin, are stronger and more toxic than wound cleaners.
cleaning wounds • agent must be able to penetrate into contaminated tissue in an active form and in sufficient Concentration to achieve bactericidal activity. because antiseptics bind chemically to multiple Organic substrates that are normally present in Chronic wounds, they may fail to reach bacteria in the wound tissue when used in standard clinical concentrations. • Thus, they’re unable to create an effective antibacterial effect. • Furthermore, antiseptics are toxic to all cells with which they come into contact, including WBCs and fibroblasts. • some clinicians have reported using antiseptics for specific clinical indications, such as to demarcate a gangrenous wound and limit bacterial invasion of surrounding tissue
CLEANING DEVICES • The effectiveness of wound cleaning is influenced by the type of cleaning device used to deliver the solution to the wound surface. It’s essential that the method used provide sufficient force to remove surface contaminants and debris while minimizing trauma to the wound. • Wound irrigation, as opposed to a cleaning device, promotes wound cleaning by creating hydraulic forces generated by the fluid stream. • In order for the irrigation to be effective in cleaning the wound, the force of the irrigation stream must be greater than the adhesion forces that hold the debris to the surface of the wound. • Multiple studies have substantiated that increasing pressure of a fluid stream improves removal of bacteria and debris from the wound.
• When irrigation is delivered with a mechanical irrigation device, such as those used for dental hygiene, greater pressures are attain • The use of a needle and syringe to deliver fluid to wound tissue is generally regarded as a convenient method of providing effective irrigation pressure. • A variety of needle and syringe combinations can be used to achieve the desired range Of irrigation pressure. The size of the syringe And the needle gauge determine the amount Of pressure of the flUid stream. Since the force Depressing the plunger is distributed over a Larger surface area, the larger the syringe, the Less the force. • whirlpool bath. • negative-pressure wound therapy (NPWT).
ANTIMICROBIAL THERAPY • When removal of necrotic tissue doesn’t reduce bacterial burden to a level compatible with healing, additional interventions to reduce the number of organisms on the wound surface are indicated. These antimicrobial therapies consist of elemental topical antimicrobials and antibiotics, both topical and systemic. These agents act directly on the microorganisms, destroying the bacteria and preventing development of new colonies. • main indications for topical antibiotic use revolve around superficial wound infection, or critical colonization, in which there is impaired wound healing, pale fragile granulation tissue, or suspected or confirmed high microbial burden, without periwound cellulitis.
- Slides: 20