Workshop 5 Ethics in Quality and Patient Safety









- Slides: 47

Workshop 5 “Ethics in Quality and Patient Safety” Al-Hareth M. Al-Khater, MB. BCh, LRCPI, LRCSI, BAO (NUI) Deputy Medical Director, National Center for Cancer Care & Research Chairman, Corporate Healthcare Ethics Committee, Hamd Medical Corporation Nabila Almeer, RN, BSN, MS, Ph. D, Fellow Ad Eundem Deputy Chief of Continuing Care Group & MOPH Nursing Affairs
2
Conflict of Interest Declaration Al-Hareth M. Al-Khater & Nabila Almeer - have no actual or potential conflict of interest in relation to this presentation - will not be discussing any off label or unapproved use of drugs or products in this presentation
The Prophet (PBUH) said: “I was sent to complete the best of ethics. ”

Why all the talk about ethics? http: //ki. se/en/news/macchiarini
OBJECTIVES 1. Be aware of the ethical principles in health care organizations in order to provide quality care and ensure patients’ safety. 2. Gain more knowledge about ethical dilemmas that maybe encountered by healthcare practitioners and learn how to manage them effectively. 3. Understand the differences between professional ethics, research ethics and healthcare ethics.
OBJECTIVES cont. 4. Have better understanding of the definitions of terms related to healthcare ethics. 5. Understand ethics within the cultural, philosophical and religious contexts underpinning medical ethics to make ethical decisions.
OUTLINE OF PRESENTATION - Background - Definitions - Principles of Professional Ethics - Principles of Healthcare Ethics - Principles of Research Ethics - Framework of Ethical Decision Making - Common Ethical Issues in Healthcare - Evidence Based Medicine (EBM) and Quality Improvement - Conclusion - Interactive discussions

BACKGROUND Ethics is the foundation for quality healthcare and a driver for achieving the desired result – which is quality patient care. From genetic testing before conception to dilemmas at the end of life healthcare practitioners, patients and their families are called upon to make ethical decisions.
DEFINITIONS Ethics Professional Ethics Research Ethics Healthcare Ethics Ethical framework Healthcare dilemmas Quality in Healthcare Patient Safety
DEFINITION WHAT IS ETHICS? Ethics provide a set of standards for behavior that help us decide how we ought to act in a range of situations. It is about making choices and providing reasons for such choices. Ethics provide good reasons for why something is moral. http: //brown. edu/academics/science-and-technology-studies/framework
DEFINITION ETHICS cont. Ethics is often confused with morals but there are key differences between the two. Morality is something that defines the difference between the goodness or badness of a thing or rightness and wrongness of a particular thing and living according to that. While ethics is a kind of philosophy of how such morality guides the individual and group behavior.
DEFINITION PROFESSIONAL ETHICS Professional ethics are accepted standards of personal and business behavior, values and guiding principles. Codes of professional ethics are often established by professional organizations to help guide members in performing their job functions according to sound and consistent ethical principles. Read more: http: //www. businessdictionary. com/definition/professional-ethics. html
DEFINITION PROFESSIONAL ETHICS cont. Some of the important components of professional ethics that professional organizations necessarily include in their code of conduct: - Integrity - Honesty - Transparency - Respectfulness - Confidentiality - Objectivity
DEFINITIONS RESEARH ETHICS Research ethics is specifically interested in the analysis of ethical issues that are raised when people are involved as participants in research. Research ethics concerns the responsibility of researchers to be honest and respectful to all individuals who are affected by their research studies and the results. Read more at: https: //www. skillsyouneed. com/learn/research-ethics. html
DEFINITIONS RESEARCH ETHICS cont. There are three objectives in research ethics. 1. 2. 3. Protect human participants. Ensure that research is conducted in a way that serves interests of individuals, groups and/or society as a whole. Examine specific research activities and projects for their ethical soundness, looking at issues such as the process of consent, the management of risk/benefit, & equity
DEFINITIONS HEALTHCARE ETHICS Healthcare ethics defined at its simplest, is a set of principles, beliefs and values that guide us in making choices about healthcare.
DEFINITIONS ETHICAL BEHAVIOR Ethical behavior is acting in a manner that is in tandem with what society considers to be good morals. Our code of conduct is also derived from our ethical behavior which includes: -Integrity -Fairness -Honesty -Dignity
Definitions Ethical Framework Ethical framework is a set of codes that an individual uses to guide his or her behavior. HMC ethical framework includes the following : - Professional ethics - Research ethics - Healthcare ethics/dilemmas - Professional Councils - Institutional Review Board - Healthcare Ethics committee - Policies and Guidelines
DEFINITION The Healthcare Ethics Committee at HMC works in an advisory capacity with healthcare providers to facilitate decisions in helping patients and families to reach informed decisions and develop policies for example: End of Life Care Advance Directives Withholding and Withdrawing life Sustaining treatment Do Not Attempt Resuscitation (DNAR) Abuse and Neglect of Children and Adults Termination of Pregnancy
DEFINITION HEALTHCARE DILEMMA An ethical dilemma occurs when an individual must choose between two unfavorable alternatives An ethical dilemma usually has no perfect solution, and those making decisions may find themselves in the position of having to defend their decisions.

22
DEFINITION QUALITY Institute of Medicine (IOM) defines quality as the degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge. Quality in healthcare is the degree to which its processes and results meet or exceed the needs and desires of the recipients of care.
DEFINITION PATIENT SAFETY Patient safety as defined by WHO is the prevention of errors and adverse effects to patients that are associated to healthcare. It is the central aim of quality. Safety is what patients, families, staff expect from the healthcare facilities. While patient safety events may not be completely eliminated, harm to patients can be reduced, and the goal is always zero harm.
FUNDAMENTAL PRINCIPLES OF HEALTHCARE ETHICS The fundamental principles and values are featured in most health care professional code of ethics and conduct and relevant to patient specific clinical dilemmas: 1. Autonomy: Right of the patient to retain control of his/her body. 2. Beneficence: Promote what is best for the patients. 3. Non–maleficence: Do no harm to the patient.
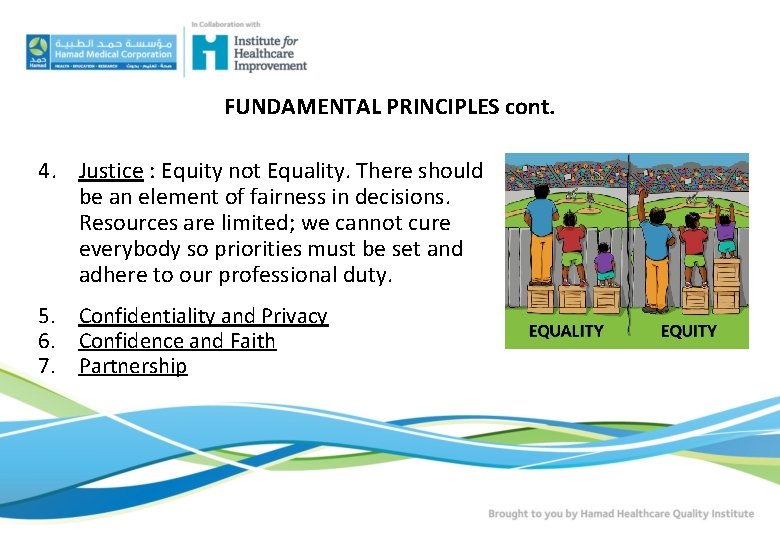
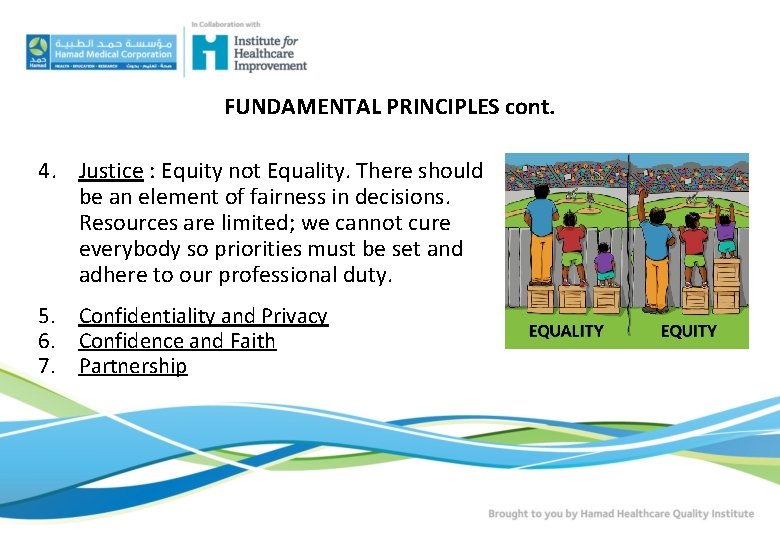
FUNDAMENTAL PRINCIPLES cont. 4. Justice : Equity not Equality. There should be an element of fairness in decisions. Resources are limited; we cannot cure everybody so priorities must be set and adhere to our professional duty. 5. Confidentiality and Privacy 6. Confidence and Faith 7. Partnership
BASIC PRINCIPLES OF RESEARCH ETHICS 1. 2. 3. 4. 5. 6. Minimizing the risk of harm. Obtaining informed consent. Protecting anonymity/confidentiality. Avoiding deceptive practices. Providing the right to withdraw. Justice/Equity http: //dissertation. laerd. com/principles-of-research-ethics. php

RESEARCH cont. Ethical codes in research cover the following areas: - Honesty and Integrity - Objectivity - Carefulness - Openness - Respect for Intellectual Property - Confidentiality - Responsible Publication - Legality
FRAMEWORK FOR ETHICAL DECISION MAKING (Acronym ISSUES) I dentify issue and decision making process S tudy the facts S elect reasonable options U nderstand values and duties E valuate and justify options S ustain and review the plan
ETHICAL FRAMEWORK cont. The framework includes seven obligations, six of which fall on health professionals and institutions, and the 7 th on patients: 1. 2. 3. 4. Respect the rights and dignity of patients Re spect the clinical judgment of clinicians Provide opti mal care to each patient Avoid imposing nonclinical risks and burdens on patients
ETHICAL FRAMEWORK cont. 5. Address health inequalities among populations 6. Conduct continuous learning activities that improve the quality of clinical care and health care systems 7. Contribute to the common purpose of improving the quality and value of clinical care and health care systems
EVIDENCE BASED MEDICINE (EBM) AND QUALITY IMPROVEMENT The two concepts of evidence-based medicine and quality improvement are complementary. While evidence-based medicine justifies clinical decisions with evidence, quality improvement is ‘translational’; putting evidence-based medicine into practice in healthcare systems.
EBM AND QUALITY IMPROVEMENT cont. Concerns about the ethics of EBM relate to possible alterations in the humane basis of clinical care. In collecting the evidence for EBM, scientists and doctors, not consumers, determine research objectives, interpret the data and implement the findings, and in doing so may disregard patients' priorities.
EBM AND QUALITY IMPROVEMENT cont. Quality improvement becomes difficult to justify or measure without evidence. EBM may lead and suggests that, to be ethically valid, EBM must be aimed at the patient's best interests and not at the financial interests of others. While financial considerations are by no means trivial, it is hypocritical -- if not dangerous -- to hide them behind words like "evidence" or "quality. "

TOP ETHICAL ISSUES IN HEALTHCARE

TOP ETHICAL ISSUES IN HEALTHCARE 1. 2. 3. 4. 5. Balancing care quality and efficiency Improving access to care Building and sustaining the healthcare workforce of the future Addressing beginning of life & end of life issues Allocating limited medications and donor organs
CONCLUSION Quality care and ethical principles cannot be separated. Quality care is built on ethical standards and principles , and ethical practices foster quality care that is: safe, effective, patientcentered, timely, efficient and equitable. Quality care is a patient expectation and a responsibility of clinicians and healthcare executives

38
1. INTERACTIVE DISCUSSIONS A 37 year old woman is involved in a car accident. She is resuscitated and intubated at the site of the accident and transferred to the hospital. She is pregnant and her fetus is at 24 weeks gestation. Fetal ultrasound is consistent with a viable fetus. Her clinical exam and her EEG are consistent with brain death. Her husband was also involved in the accident and he is in a critical comatose condition. The physician and the patient’s family should make a decision whether to continue mechanical ventilation or stop. What are the ethical issues raised?
DISCUSSION POINTS Engagement of the respective experts Vulnerable patients Maternal and fetal rights Legal guardian decision-maker(s) Conflicts of Interest
2. INTERACTIVE DISCUSSIONS A patient wants to donate to his physician’s research proposal which recruits subjects (including patients of the physician) and which is sponsored by a pharmaceutical company. What are the ethical issues raised?
DISCUSSION POINTS Gifts, honoraria, funding, consultation fees Conflicts of Interest Disclosures Coercion/Influence
3. INTERACTIVE DISCUSSIONS A physician suspects that a patient with terminal cancer may have a genetic risk for the cancer. The patient is counseled with regard to genetic testing and she consents but her husband insists that the results are not be given to her since this “will not help her and will damage her psychologically since she will die worrying about her children developing cancer. ” What are the ethical issues raised?
DISCUSSION POINTS Genetic testing Results, discrimination, stigma Disclosure of results What results? - to whom? - follow up? Patient autonomy Beneficence vs. Non-maleficence
References HMC Intranet: Clinical Policies CL 6077 – End of Life Care CL 6041 – Advance Directives CL 7231 – Withholding and Withdrawing Life Sustaining Treatment CL 6009 – Do Not Attempt to Resuscitate (DNAR) https: //www. ama-assn. org/delivering-care/ama-code-medical-ethics http: //www. ucalgary. edu. qa/files/Code_of_Ethics_2008_e. pdf
References cont. Hamilton Health Sciences “Ethics Framework” Approved by HHS Board of Directors January 28, 2010 https: //www. ncbi. nlm. nih. gov. pmc/articles/PMC 3284300 Patient Safety Systems (PS) CAMH Update 2, January 2016 https: //www. ache. org. policy/environ. cfm https: //online. sju. edu/graduate/master-healthadministration/resources/articles https: //researchethics. ca/what-is-research-ethics/

“We are committed to our principles and values” HH Sheikh Tamim Bin Hamad Al-Thani The Emir of the State of Qatar THANK YOU QUESTIONS & ANSWERS aalkhater 1@hamad. qa