Working with People with Learning Disabilities Directed Enhanced

Working with People with Learning Disabilities Directed Enhanced Service (DES) - Learning Disabilities 2008/09
What is a learning disability? The Department of Health defines learning disability as: • A significantly reduced ability to understand new or complex information, to learn new skills (impaired intelligence with an IQ below 70) with; • A reduced ability to cope independently (impaired social functioning) and; • Which started before adulthood, with a lasting effect on development
Prevalence • Nationally it is estimated 2 -3% of the population have a learning disability • Estimates suggest: - 210, 000 people with severe & profound learning disabilities - 1. 2 million people with mild/moderate learning disabilities • Per GP practice of 2000 patients – average of 40 people with learning disabilities
Degrees of Learning Disability (ICD - 10) • Mild learning disability IQ between 50 - 69 (In adults, mental age from 9 to under 12 years) • Most achieve independence in self care, practical and domestic skills with rate of development considerably slower • Acquire language with delay but achieve ability to use speech for everyday purposes • Capable of work, practical including unskilled or semi skilled manual rather than academic • May not be easily identifiable as having a learning disability
Degrees of Learning Disability (ICD - 10) • Moderate learning disability IQ between 35 - 49 (In adults, mental age from 6 to under 9 years) • Limited development of language and comprehension • Self care, practical and domestic skills are limited. Adults will need varying degrees of support to live and work in the community
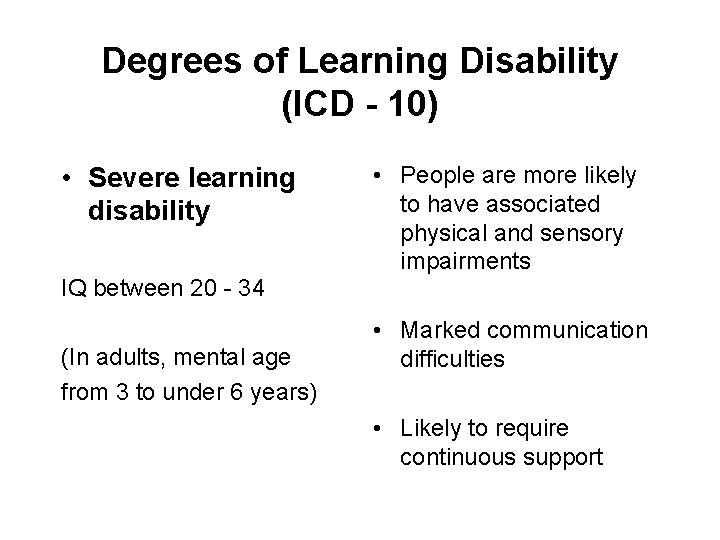
Degrees of Learning Disability (ICD - 10) • Severe learning disability • People are more likely to have associated physical and sensory impairments IQ between 20 - 34 (In adults, mental age from 3 to under 6 years) • Marked communication difficulties • Likely to require continuous support
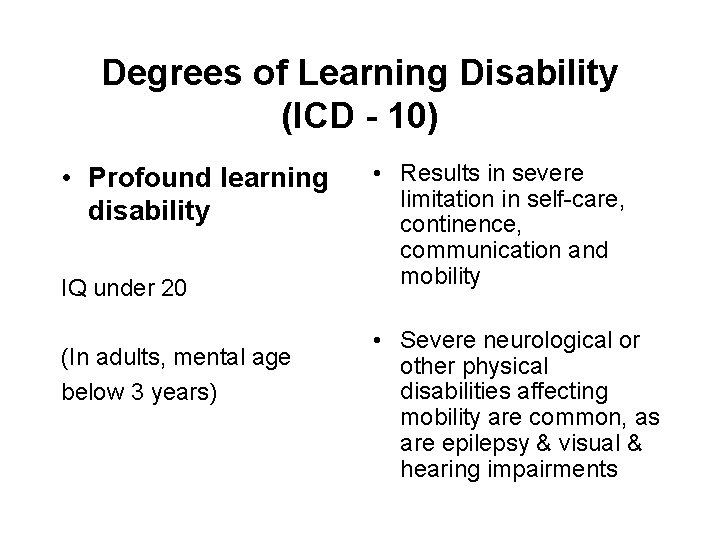
Degrees of Learning Disability (ICD - 10) • Profound learning disability IQ under 20 (In adults, mental age below 3 years) • Results in severe limitation in self-care, continence, communication and mobility • Severe neurological or other physical disabilities affecting mobility are common, as are epilepsy & visual & hearing impairments
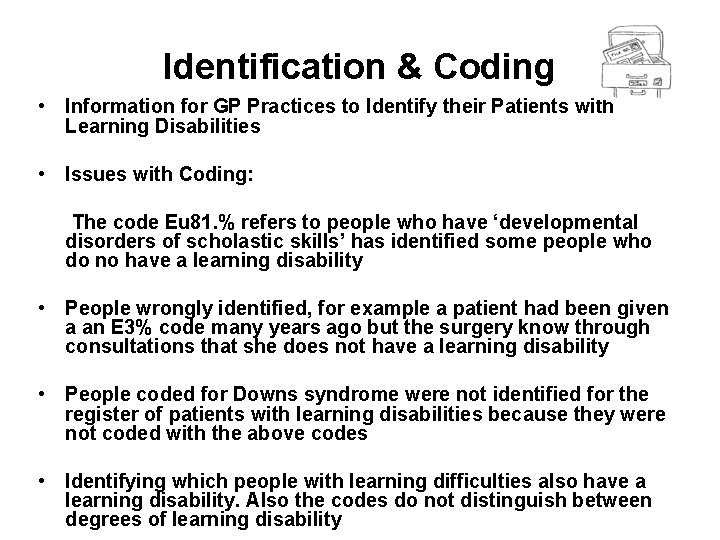
Identification & Coding • Information for GP Practices to Identify their Patients with Learning Disabilities • Issues with Coding: The code Eu 81. % refers to people who have ‘developmental disorders of scholastic skills’ has identified some people who do no have a learning disability • People wrongly identified, for example a patient had been given a an E 3% code many years ago but the surgery know through consultations that she does not have a learning disability • People coded for Downs syndrome were not identified for the register of patients with learning disabilities because they were not coded with the above codes • Identifying which people with learning difficulties also have a learning disability. Also the codes do not distinguish between degrees of learning disability
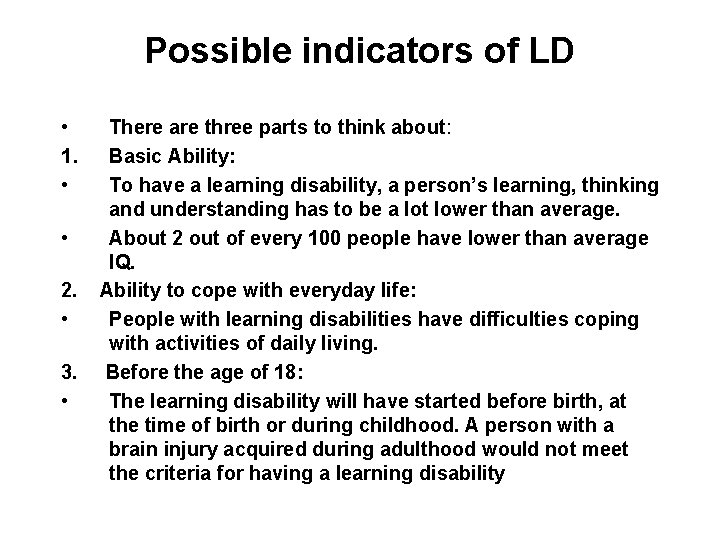
Possible indicators of LD • 1. • • 2. • 3. • There are three parts to think about: Basic Ability: To have a learning disability, a person’s learning, thinking and understanding has to be a lot lower than average. About 2 out of every 100 people have lower than average IQ. Ability to cope with everyday life: People with learning disabilities have difficulties coping with activities of daily living. Before the age of 18: The learning disability will have started before birth, at the time of birth or during childhood. A person with a brain injury acquired during adulthood would not meet the criteria for having a learning disability
Health Issues More likely to: • Die early • Die from breathing problems • Have heart problems • Be overweight, and eat badly • Have certain cancers • Have epilepsy • Have Autism • Be mentally ill
Health Issues More likely to: • Have dementia • Be given psychotropic drugs • Have a physical disability • Be deaf or blind • Have communication problems • Have thyroid dysfunction • Have dental problems. • Use medical hospital services • Be discharged quickly
Health Issues Less likely to: • Have a health check • Be screened for cancer • Use surgical hospital services • Have sight tested • Have hearing tested • Receive pain relief • Get Health Promotion advice • Be included in consultations/ patient forums
Special Health Needs of People with Learning Disabilities • 2. 5 x more likely to have a physical condition that warrants medical intervention • Lack of early intervention/detection • Great difficulty & barriers in accessing all aspects of healthcare • Health outcomes fall short
Diagnostic overshadowing • ‘Diagnostic overshadowing’ is the term used by the Disability Rights Commission to describe the tendency to attribute symptoms and behaviour associated with illness to the learning disability, and for the illness to be overlooked. Healthcare for All (2008) • The Michael Inquiry (2008) argued that although other groups such as older people or people with mental health problems may also suffer from diagnostic overshadowing, learning disability may well represent a special case. This is largely because of the ignorance that still surrounds learning disability. Therefore there is a strong argument in favour of including basic teaching about learning disability in all preregistration courses and involving people with learning disability in providing it.
Barriers to accessing health care • Communication • Physical environment • Low expectation • Poor information from • Physical access • Lack of accessible information • Fear of health professionals • Lack of time carers • Poor support • Lack of education • Lack of preparation • Additional needs e. g. Autism
The Health Check • Weight - Height - BMI More likely to be under or overweight so at greater risk of health problems • BP - Pulse Rate & rhythm • Urine Test for Glucose • TSH Level A fasting blood sugar could be done at the same time if a TSH level is needed. Thyroid problems are more common in people with Down’s Syndrome. Annual TFT’s are recommended • Smoking Status • Alcohol Consumption • Dietary Advice • Exercise Grading 80% of people engage in levels below those recommended by the Department of Health guidance. • Change in behaviour Always consider health problems such ear or dental Infections which could present as changes in behaviour
The Health Check • Speech Communication difficulties are very common in people with learning disabilities • Visual • Hearing 40% of people with learning disabilities have a significant Sensory Impairment Signpost for Success (1998) • Mobility • Chiropody • Bowel – Bladder Assessment Higher rates of gastro-intestinal Cancer (46 -52% V 15 -17%) • Epilepsy 60% people with learning disability have epilepsy. Ensure they are on QOF Register. Anti-convulsant blood level monitoring may be necessary • Mental Health Consider screening for depression if changes in behaviour occur. Dementia is much more common in people with Down’s Syndrome
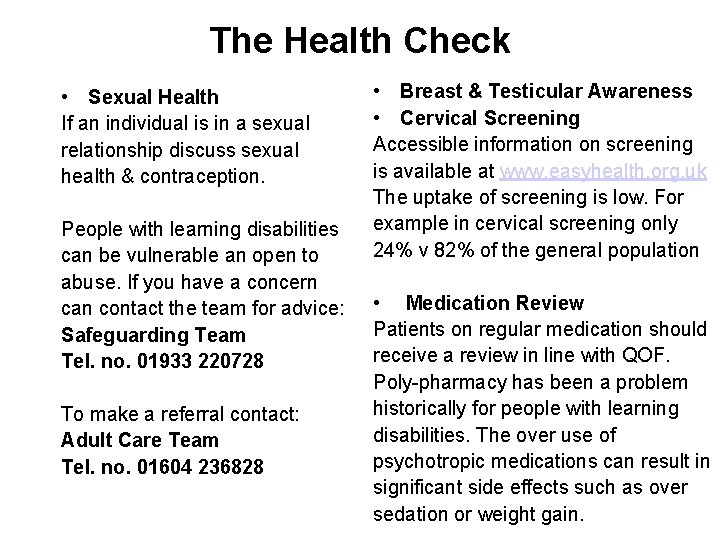
The Health Check • Sexual Health If an individual is in a sexual relationship discuss sexual health & contraception. People with learning disabilities can be vulnerable an open to abuse. If you have a concern can contact the team for advice: Safeguarding Team Tel. no. 01933 220728 To make a referral contact: Adult Care Team Tel. no. 01604 236828 • Breast & Testicular Awareness • Cervical Screening Accessible information on screening is available at www. easyhealth. org. uk The uptake of screening is low. For example in cervical screening only 24% v 82% of the general population • Medication Review Patients on regular medication should receive a review in line with QOF. Poly-pharmacy has been a problem historically for people with learning disabilities. The over use of psychotropic medications can result in significant side effects such as over sedation or weight gain.
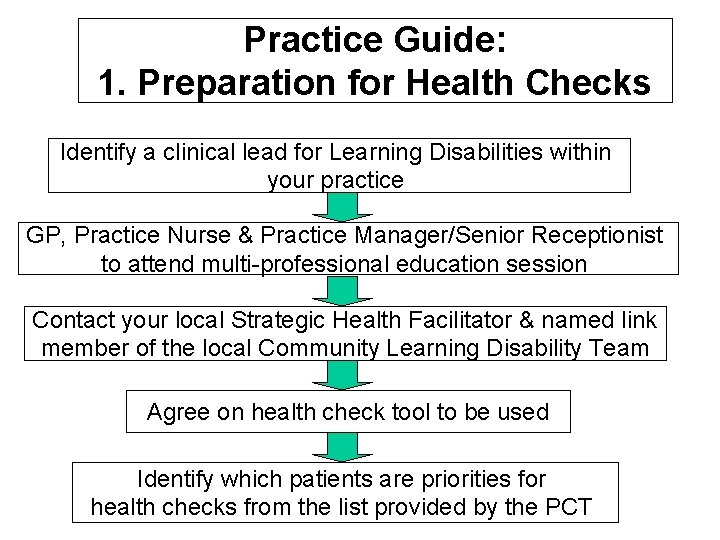
Practice Guide: 1. Preparation for Health Checks Identify a clinical lead for Learning Disabilities within your practice GP, Practice Nurse & Practice Manager/Senior Receptionist to attend multi-professional education session Contact your local Strategic Health Facilitator & named link member of the local Community Learning Disability Team Agree on health check tool to be used Identify which patients are priorities for health checks from the list provided by the PCT
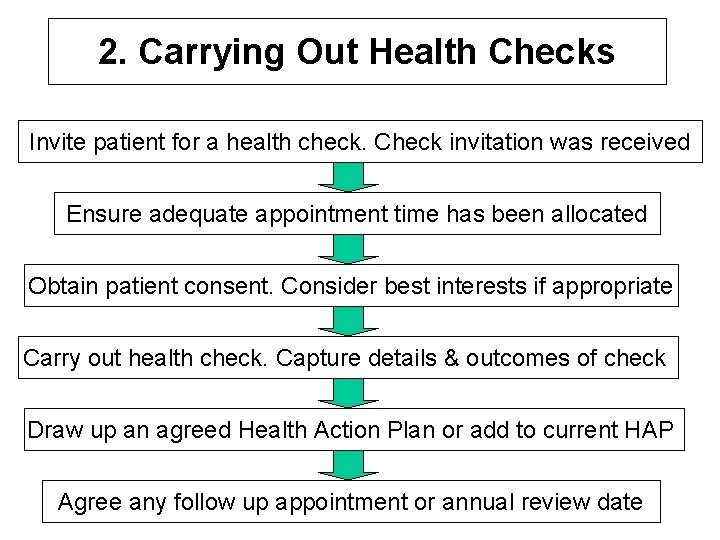
2. Carrying Out Health Checks Invite patient for a health check. Check invitation was received Ensure adequate appointment time has been allocated Obtain patient consent. Consider best interests if appropriate Carry out health check. Capture details & outcomes of check Draw up an agreed Health Action Plan or add to current HAP Agree any follow up appointment or annual review date
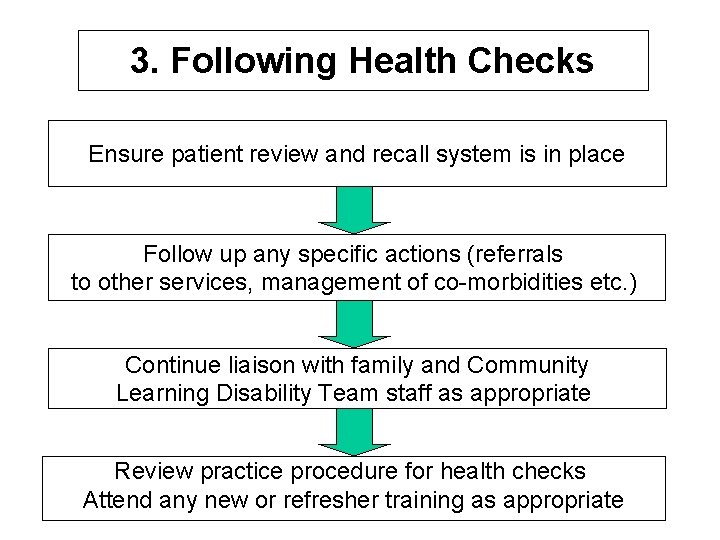
3. Following Health Checks Ensure patient review and recall system is in place Follow up any specific actions (referrals to other services, management of co-morbidities etc. ) Continue liaison with family and Community Learning Disability Team staff as appropriate Review practice procedure for health checks Attend any new or refresher training as appropriate
DDA/Disability Equality Duty Disability Discrimination Act – 2005 • To promote equality of opportunity for disabled people Disability Equality Duty – Requires all public authorities to promote disability equality by: • Eliminating unlawful discrimination • Making ‘reasonable’ adjustments for disabled people • Promoting positive attitudes and encouraging participation
Consent The Mental Capacity Act (2005) è 5 Key Principles: 1. Every adult has the right to make their own decisions & must be assumed capable of doing so until proved otherwise 2. Everyone should be given all the support they need to make their own decisions before conclusions are made that they cannot
Consent 3. People should be able to make unwise or eccentric decisions - it is capacity to make decisions, not decisions themselves, that is the issue 4. Any decisions or anything done for or on behalf of a person who lacks capacity must be made or done in their best interests 5. Anything done for or on behalf of people without capacity should restrict their rights & freedoms as little as possible
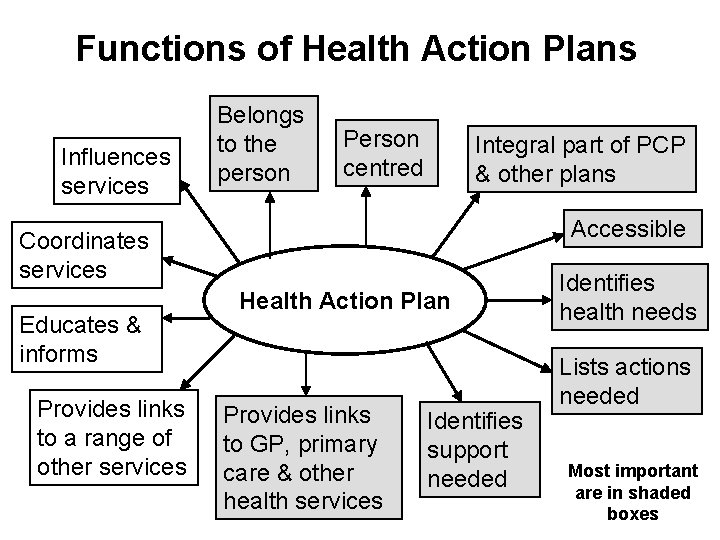
Functions of Health Action Plans Influences services Belongs to the person Person centred Integral part of PCP & other plans Accessible Coordinates services Educates & informs Provides links to a range of other services Health Action Plan Provides links to GP, primary care & other health services Identifies support needed Identifies health needs Lists actions needed Most important are in shaded boxes
What should be in a HAP? • Identified health needs or issues • What actions are needed to maintain health • What actions are needed to improve health • Who will help ensure these actions take place (especially if this is someone other than the health facilitator) • Timescales for various actions and when there will be a follow up or a review.
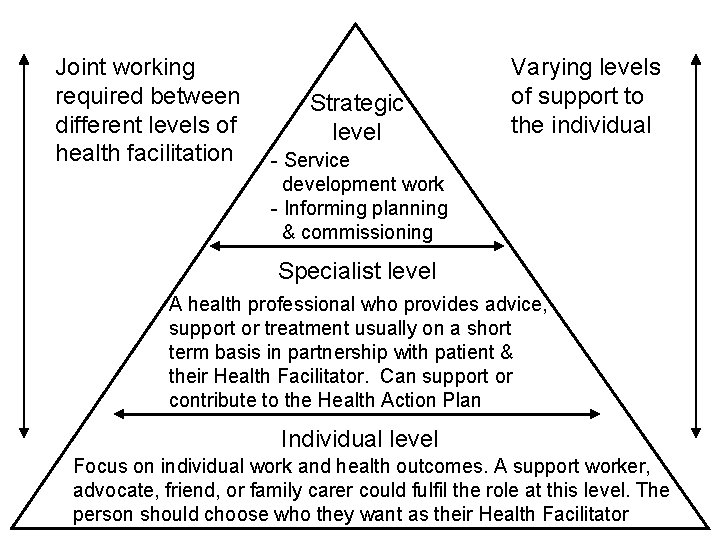
Joint working required between different levels of health facilitation Strategic level Varying levels of support to the individual - Service development work - Informing planning & commissioning Specialist level A health professional who provides advice, support or treatment usually on a short term basis in partnership with patient & their Health Facilitator. Can support or contribute to the Health Action Plan Individual level Focus on individual work and health outcomes. A support worker, advocate, friend, or family carer could fulfil the role at this level. The person should choose who they want as their Health Facilitator
Working together At different times of their lives people with learning disabilities require different levels of support from different services: • Role of the Community Learning Disability Team - Specialist multi disciplinary assessment -Therapeutic interventions to help with physical & mental wellbeing Role of carers - Advocacy - Emotional & physical support - Monitoring changes in health • Social care support - Housing - Work/day opportunities - Individual Budgets
- Slides: 28