Workforce Wellbeing in Psychological Therapies Analysis of Trends
Workforce Wellbeing in Psychological Therapies Analysis of Trends, improving our measure & Taking forward the Charter Dr Gita Bhutani & Dr Amra Rao
Workforce Wellbeing Survey 2014 - 2019 Project Team Amra Rao, Jeremy Clarke, Gita Bhutani, Neelam Dosanjh, Lizzie Summers
Wellbeing is Important Range of reports and research studies NHS Staff Surveys, CQu. INs DCP & New Savoy Conference charter Collaborative Network Learning - Pathfinders NHS Staff & Learners Mental Wellbeing Commission Report
HEE Wellbeing Commission Report Recommendations 32 Recommendations • NHS Culture • Staff Wellbeing • NHS Support to staff and learners Key Points • Board Level workforce wellbeing guardians and leaders • Training in self-awareness, self-care, suicide risk and prevention • Post-incident support • Thriving at Work • Clinical supervision • Staff access to psychological treatment services
IAPT and Leadership servi Management ces, Faculty of the BPS, DCP. NSP Core objectives of theset out collaboration to include meas conducting annualure measure the Further of wellbeing in wellb development psychological eing of the services, of measure, developing ato psych include charter of wellologi subscales being, fromcal the a developing thera Work Related strategic piesofand Quality framework Lifestaff scaletool well-being – (WRQo. L) and establishing (Vanbased Laar, a Collaborative on Edwards, & Learning Europ Easton, Network to share ean 2007). good practice Social and drive the Charter for Surve well-being Workforce y agenda. Wellbeing & (NEF, Resilience The NSP and DCP 2009) (2016) disseminated their first The New Savoy Partnership (NSP) and DCP Background 2009 2014 2015 and 2018
What is the Workforce Wellbeing Survey? 2009 Staff Wellbeing Tool based on European Social Survey Questionnaire (NEF 2009) Survey promoted through professional networks Survey focused on feelings about work as well as collecting demographic information Participants increased from 852 (in 2014) to 1106 (in 2015) to 1227 (in 2016) to 1678 (in 2017) but reduced to 1037 in 2019
The 2018 Workforce Wellbeing Survey Psychological Practitioner Workplace Wellbeing Measure New measure developed to be psychometrically robust 6 factors Additional questions Self-reported feelings of depression and stress Bullying & harassment Safety of services Comparable to previous years Demographic and professional information Age, gender, sexual orientation, long-term condition Professional role, banding, hours worked, paid & unpaid overtime Online survey Snowball sampling
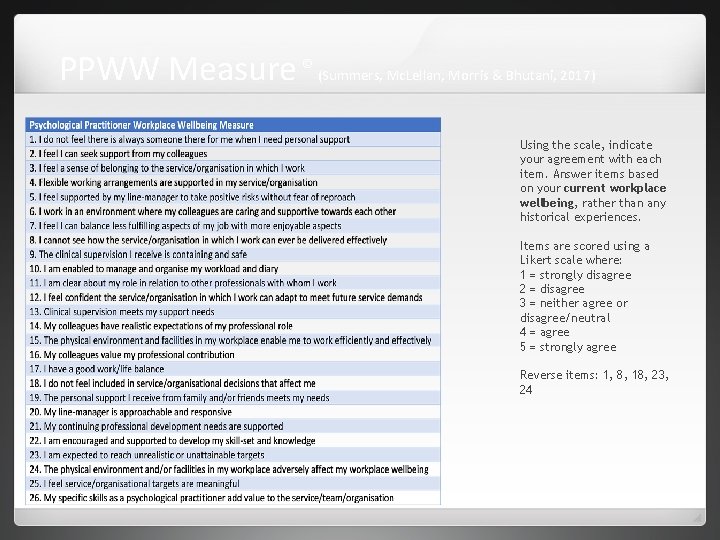
PPWW Measure © (Summers, Mc. Lellan, Morris & Bhutani, 2017) Using the scale, indicate your agreement with each item. Answer items based on your current workplace wellbeing, rather than any historical experiences. Items are scored using a Likert scale where: 1 = strongly disagree 2 = disagree 3 = neither agree or disagree/neutral 4 = agree 5 = strongly agree Reverse items: 1, 8, 18, 23, 24
Demographic results 1037 respondents 80. 8% female Most common age range was 45 - 54 years (29. 1%) Most frequently selected ethnic background was White (89. 8%) Most participants identified as heterosexual (82. 9%) ‘Do you have a long-standing illness, health problem or disability? ’ 15. 8% responded Yes
Demographics: Comparisons across the years No significant differences found in: Gender Sexual Orientation Age (over past three years) Significant Reported differences found in disability increased 2014 to 2015 and has decreased since although not to 2014 levels. Non-white groups completed the survey increased up to 2015 and then reduced to 2014 levels
Professional and work characteristics Clinical psychologists formed the largest proportion of respondents (54. 8%) 93% of the respondents responded Agenda for Change as their main salary scale The most common Agenda for Change band (Af. C) was Band 8 a (29. 7%)
Professional and work characteristics 2 The primary employer for most was the NHS (91%) 31% of respondents worked in IAPT with 24% working in adult mental health Most respondents (56%) worked close to full-time hours (30 to 37. 5 hours per week) Just under 7% reported paid overtime or bank work 26. 5% of the respondents said they did not undertake unpaid overtime or additional unpaid hours 56% reported working up to an additional 5 hours 12% working 6 to 11 hours
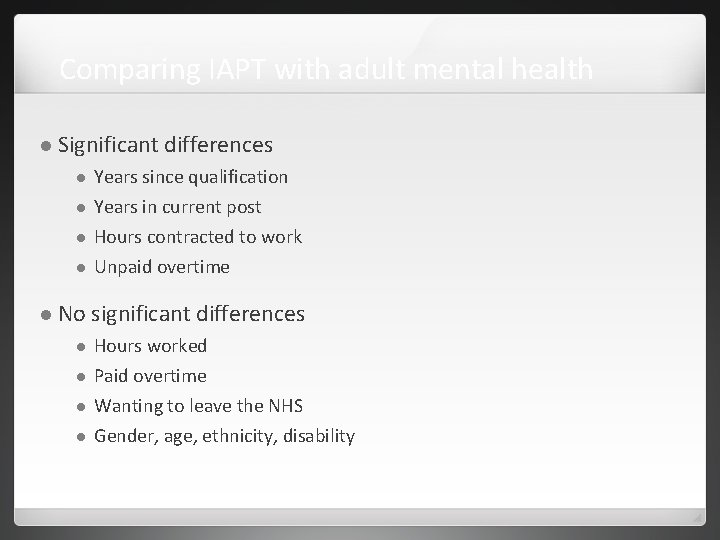
Comparing IAPT with adult mental health Significant differences Years since qualification Years in current post Hours contracted to work Unpaid overtime No significant differences Hours worked Paid overtime Wanting to leave the NHS Gender, age, ethnicity, disability
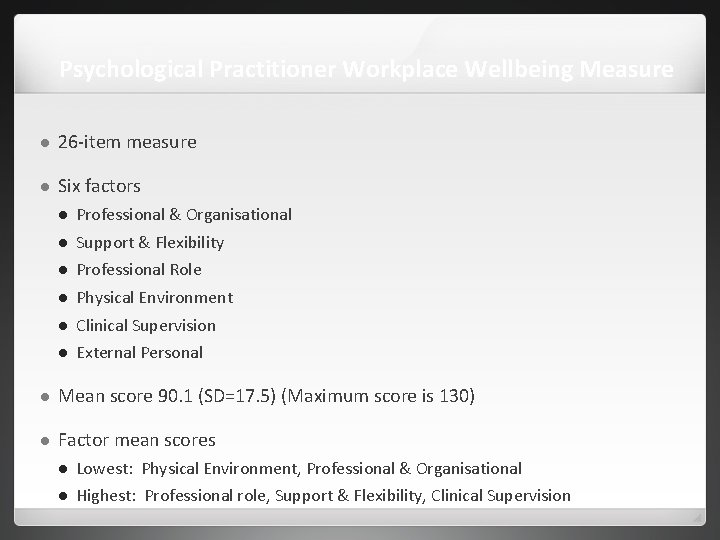
Psychological Practitioner Workplace Wellbeing Measure 26 -item measure Six factors Professional & Organisational Support & Flexibility Professional Role Physical Environment Clinical Supervision External Personal Mean score 90. 1 (SD=17. 5) (Maximum score is 130) Factor mean scores Lowest: Physical Environment, Professional & Organisational Highest: Professional role, Support & Flexibility, Clinical Supervision
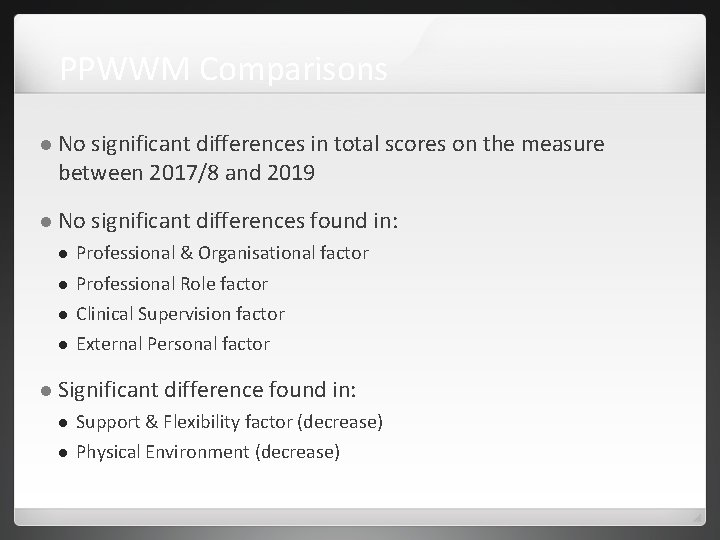
PPWWM Comparisons No significant differences in total scores on the measure between 2017/8 and 2019 No significant differences found in: Professional & Organisational factor Professional Role factor Clinical Supervision factor External Personal factor Significant difference found in: Support & Flexibility factor (decrease) Physical Environment (decrease)
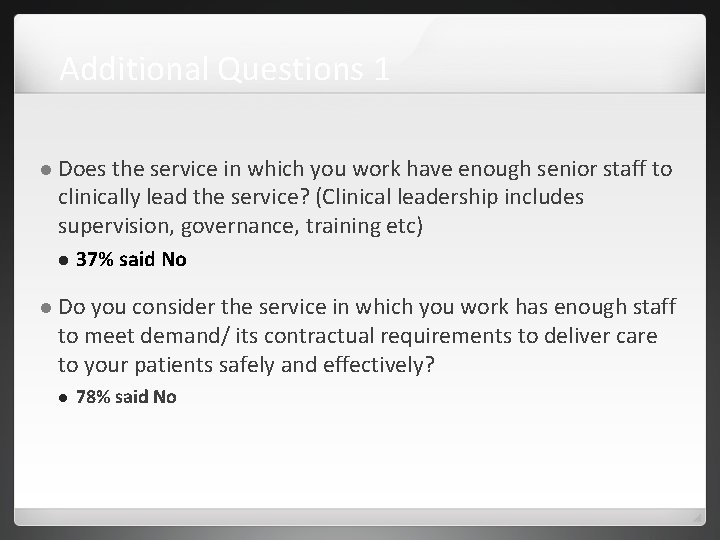
Additional Questions 1 Does the service in which you work have enough senior staff to clinically lead the service? (Clinical leadership includes supervision, governance, training etc) 37% said No Do you consider the service in which you work has enough staff to meet demand/ its contractual requirements to deliver care to your patients safely and effectively? 78% said No
Additional Questions 2 You have indicated that you are employed in the NHS. How often in the past 12 months have you wanted to leave? 23% said Once or twice a week or almost every day 22% said Once or twice a month 22% said Never
Additional Questions 3 40% indicated that they had felt depressed Some of the time or more frequently over the past week. 82% said they had found their job stressful over the past week – some of the time or more frequently 85% found their job enjoyable over the past week some of the time or more frequently 93% found their job interesting over the past week some of the time or more frequently
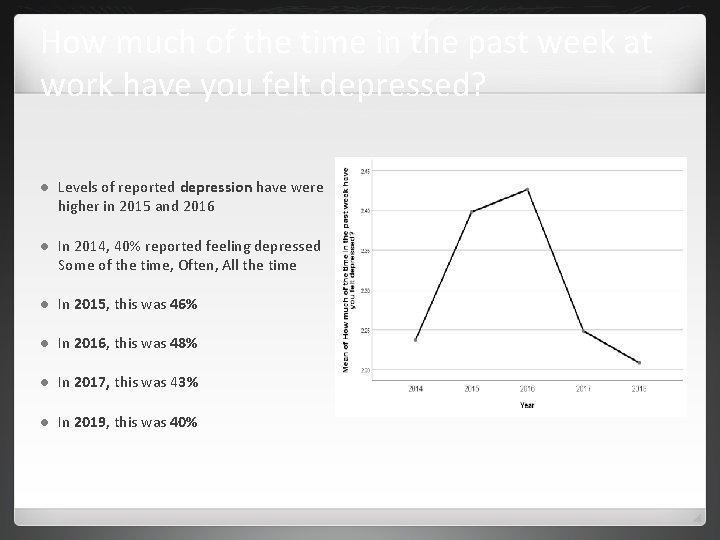
How much of the time in the past week at work have you felt depressed? Levels of reported depression have were higher in 2015 and 2016 In 2014, 40% reported feeling depressed Some of the time, Often, All the time In 2015, this was 46% In 2016, this was 48% In 2017, this was 43% In 2019, this was 40%
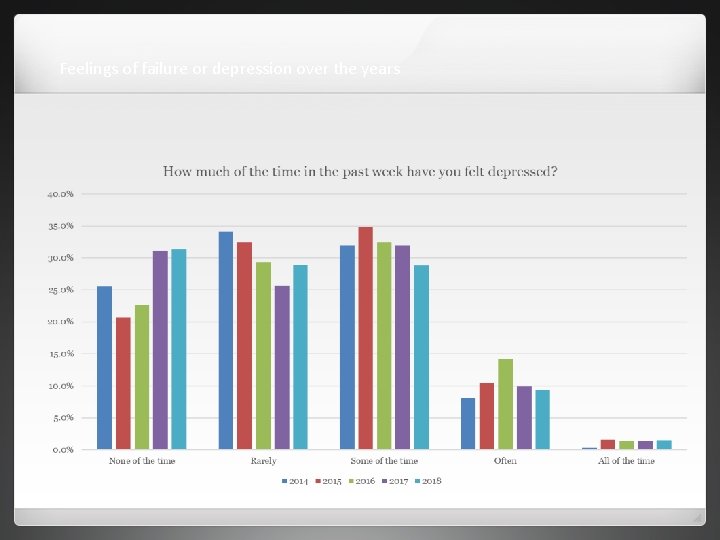
Feelings of failure or depression over the years
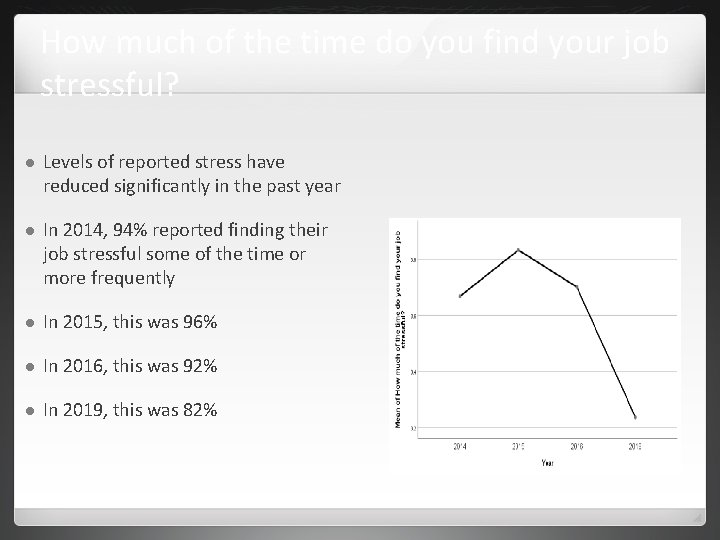
How much of the time do you find your job stressful? Levels of reported stress have reduced significantly in the past year In 2014, 94% reported finding their job stressful some of the time or more frequently In 2015, this was 96% In 2016, this was 92% In 2019, this was 82%
Experience of bullying or discrimination at work 31% reported bullying and harassment occurring more than once in the past 12 months from patients, service users, their relatives or other members of the public 13% reported bullying and harassment from managers occurring once or twice in the past 12 months with an additional 6% reporting more frequently. 10% reported bullying and harassment from other with an additional 6% reporting this occurring more frequently 5. 1% said they had been accused of bullying and/or harassment, highest reporting over the years
In the last 12 months have you personally experienced discrimination at work from any of the following? Patients public 6% / service users, their relatives or other members of the responded Yes Manager / team leader or other colleagues 13% responded Yes Main reasons reported were Age, Gender and Ethnic Background
Accused of bullying and harassment The numbers accused of bullying and harassment as a percentage of the sample has increased significantly. In 2014, this was 1. 2% In 2015, this was 2. 2% In 2016, this was 3. 5% In 2017, this was 4. 1% In 2019, this was 5. 1%
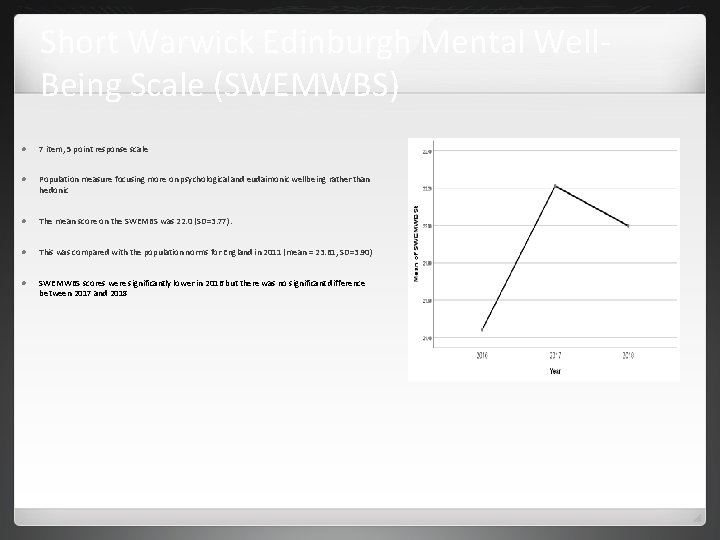
Short Warwick Edinburgh Mental Well. Being Scale (SWEMWBS) 7 item, 5 point response scale Population measure focusing more on psychological and eudaimonic wellbeing rather than hedonic The mean score on the SWEMBS was 22. 0 (SD=3. 77). This was compared with the population norms for England in 2011 (mean = 23. 61, SD=3. 90) SWEMWBS scores were significantly lower in 2016 but there was no significant difference between 2017 and 2018
Summary of the Workforce Wellbeing Survey Mostly NHS respondents and mostly female Increasing proportion of clinical psychologists – perhaps reflecting sampling methods Improvements No in self-report of feelings of depression and stress improvement in the PPWWM or SWEMWBS Bullying and harassment self-report largely unchanged although increase in self-report of being accused
Qualitative Findings : questions asked What is important to you for a good working environment? (853 comments (82%)) What, if anything, would you like to see shifting/ changing to enhance psychological practitioner wellbeing within the workplace? Please enter a maximum of three key points (807 Comments (78%)) Does the service in which you work have enough senior staff to clinically lead the service? (clinical leadership includes supervision, governance, training etc) – No (please provide more details) (274 comments (26%)) If you have thought of leaving, what are the main reasons you would give for wanting to leave? (722 comments (70%))
What is important to you for a good working environment? LEADERSHIP FIT FOR PURPOSE ORGANISATIONAL DESIGNS CULTURE & VALUES FACILITATIVE WORKING ENVIRONMENT WORKFORCE DEVELOPMENT
What is important to you for a good working environment? Effective Fit Supervision & Line Management for purpose working environment with adequate resources Supportive Adequate and trusting relationships staffing and realistic work capacity Compassionate culture and leadership
What is important to you for a good working environment? 30 Having a desk, a computer that works and having access to a clinical room A clear goal - an overall feeling that this is being supported from senior to national management A workload based on reasonable factors ie a properly weighted case load which addresses case complexity A role that is in tune with a persons person style of resilience. Having colleagues you can trust, relate to, joke with, and share experience
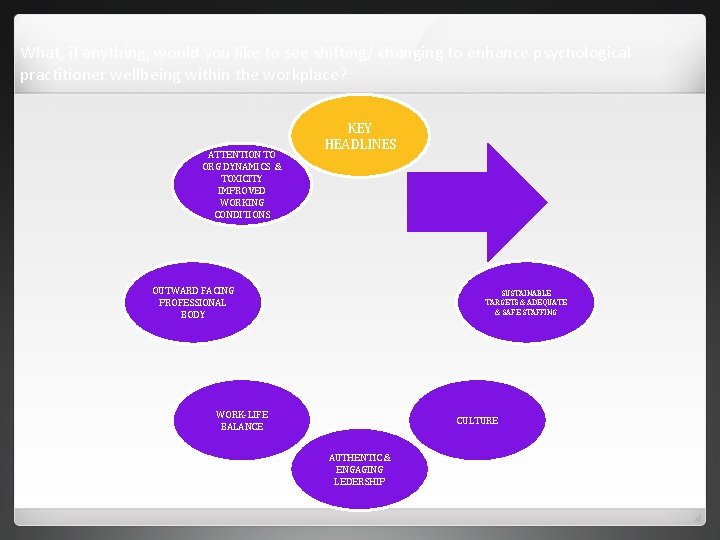
What, if anything, would you like to see shifting/ changing to enhance psychological practitioner wellbeing within the workplace? ATTENTION TO ORG DYNAMICS & TOXICITY IMPROVED WORKING CONDITIONS KEY HEADLINES OUTWARD FACING PROFESSIONAL BODY SUSTAINABLE TARGETS & ADEQUATE & SAFE STAFFING WORK-LIFE BALANCE CULTURE AUTHENTIC & ENGAGING LEDERSHIP
What, if anything, would you like to see shifting/ changing to enhance psychological practitioner wellbeing within the workplace? Improved working conditions for staff, with greater space for clinical work, permanent desks (no hot desking), cleaner and more organised spaces, suitable breaks for staff with a personal and regular space away from the desk Improvements with IT systems and equipment Greater number of clinical and admin staff to meet both service and target demands Achievable targets (less focus on IAPT league tables based on achievement of targets) Improved ratio of senior staff to junior staff to allow for adequate supervision, flexible hours and autonomy More supervision, reflective spaces , team development, CPD opportunities , having dedicated time to develop Improved pay and career progression for retention
What, if anything, would you like to see shifting/ changing to enhance psychological practitioner wellbeing within the workplace? Better awareness of psychological practice as key to any organisation dealing human distress and health Reduction in target based outcomes its terrible. We are treating humans not collecting eggs from chickens. Positive Comment I work in an organisation which I can see has been trying to prioritise and consider how to enhance wellbeing at work over the last few years. I would like to see that continue
Does the service in which you work have enough senior staff to clinically lead the service? (clinical leadership includes supervision, governance, training etc)
Does the service in which you work have enough senior staff to clinically lead the service? (clinical leadership includes supervision, governance, training etc) I am considered the clinical lead but that is not my role and I am not paid accordingly and I do not have that level of authority Head of dept post has been vacant for over a year Too few senior staff to cover supervision, strategic development work, risk management Jobs constantly down-banded as staff have left so there’s only one band 8 in the team Since I have worked here we have had 5 clinical Leads. 2 left with no job to go to and one left to take a lesser role elsewhere. Senior staff struggle and leave (greener grass? ). We have spent way too much time without substantive senior staff.
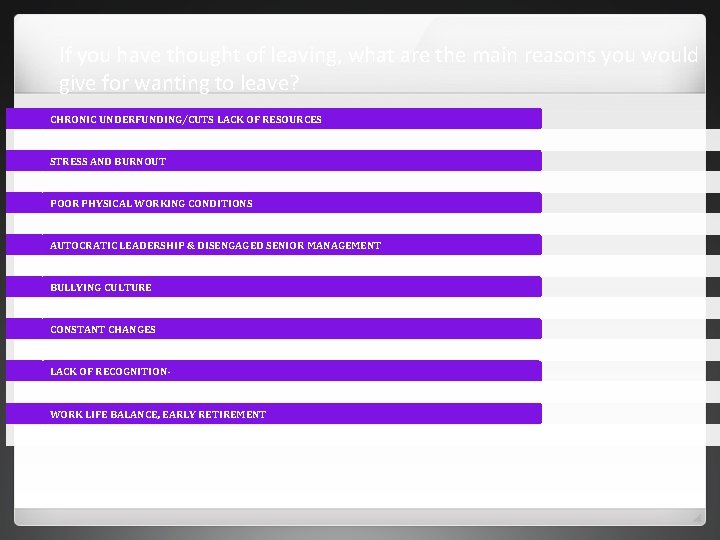
If you have thought of leaving, what are the main reasons you would give for wanting to leave? CHRONIC UNDERFUNDING/CUTS LACK OF RESOURCES STRESS AND BURNOUT POOR PHYSICAL WORKING CONDITIONS AUTOCRATIC LEADERSHIP & DISENGAGED SENIOR MANAGEMENT BULLYING CULTURE CONSTANT CHANGES LACK OF RECOGNITION- WORK LIFE BALANCE, EARLY RETIREMENT
If you have thought of leaving, what are the main reasons you would give for wanting to leave? Being bullied and being underpaid/ under-banded for the job I do Lack of feeling valued by the health board and by the NHS/government in general Almost no opportunities for career progression unless willing to leave the organisation Excessive stress and demands of service make me question if it is worth continuing or better for my health to leave. I feel totally unappreciated and unvalued by managers and some junior colleagues. Having more flexibility and the potential to earn more money Positive quote: I really like the organisation I work for and have a fantastic professional lead who I love working with
Qualitative Findings - Themes Further analysis is required but preliminary highlights for most commented areas are summarised below IAPT survival and at Professional rivalry – who is more valued, hierarchies impacting on team cohesion What influences managers vs clinicians as leaders and managers – is about style or professional allegiance More positives – separating the organisation from service team allowing for professional identity and cohesion, initiatives for wellbeing days and being well led More work – life balance needed and senior management to account for costs in sickness absence, reduced hours or staff leaving More opportunities for varied roles
Methodological Issues Self-selected snowball sampling method New Psychometrically valid questionnaire used Valid scale Factors within the scale Questions have changed over the years Data quality has improved Better online design Qualitative data Not comprehensive or weighted Very rich responses Next steps Consideration of the sampling methodology
Conclusions Despite the methodological limitations, surveys have consistently demonstrated levels of distress in the psychological workforce This is consistent with findings from surveys of NHS staff generally or other staff groups In 2019, reductions in both levels of distress and bullying were found. However, levels are still high Preliminary qualitative analysis indicates some improvements but similar themes highlighted suggesting further work is required
Over to you… Reflections on the findings so far How can the charter be taken forward to consider the NHS Staff & Learners Mental Wellbeing Commission Report recommendations? What would a dedicated psychological services look like for psychological practitioners?

Thank You and Contacts Gita Bhutani : gita. bhutani@lancashirecare. nhs. uk Neelam Dosanjh: ndosanjh 5@gmail. com Amra Rao: psychologicalhorizons@gmail. com Jeremy Clarke : therapy@practice. demon. co. uk Elizabeth Summers - summers. E 3@cardiff. ac. uk
- Slides: 42