Womens Sexual Health Ashley E Fuller MD NCMP


- Slides: 64
Women’s Sexual Health Ashley E. Fuller, MD, NCMP Gynecologist, Women’s Sexual Health Specialist Swedish OB/GYN Specialists First Hill
Disclosures • None
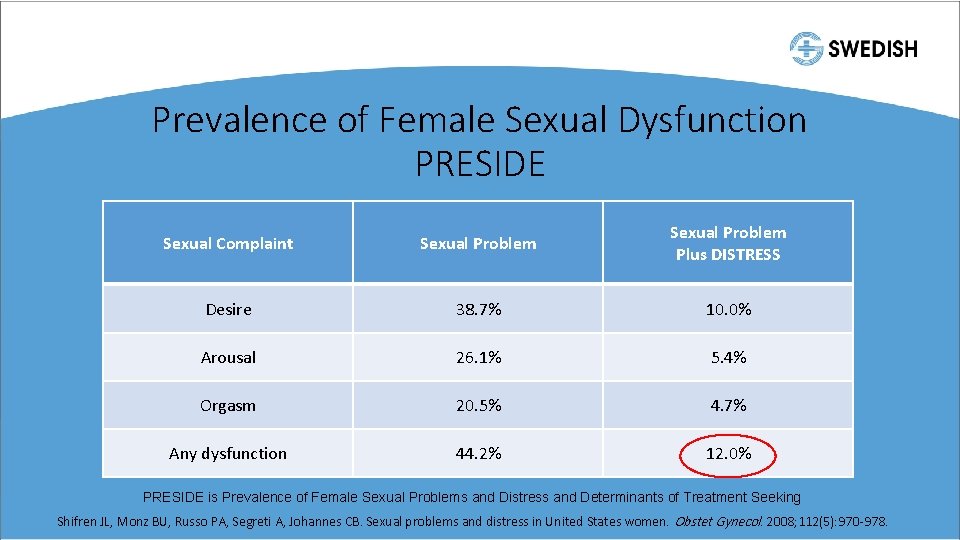
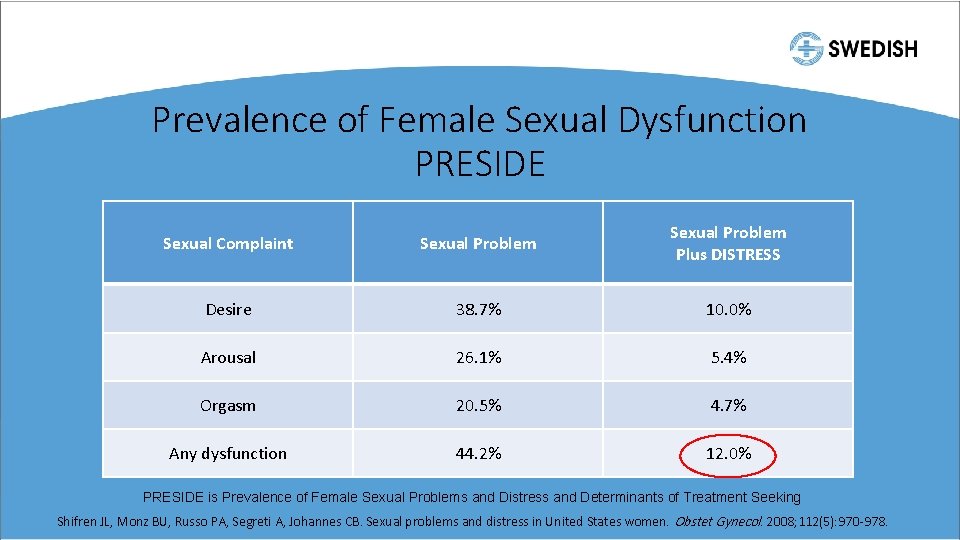
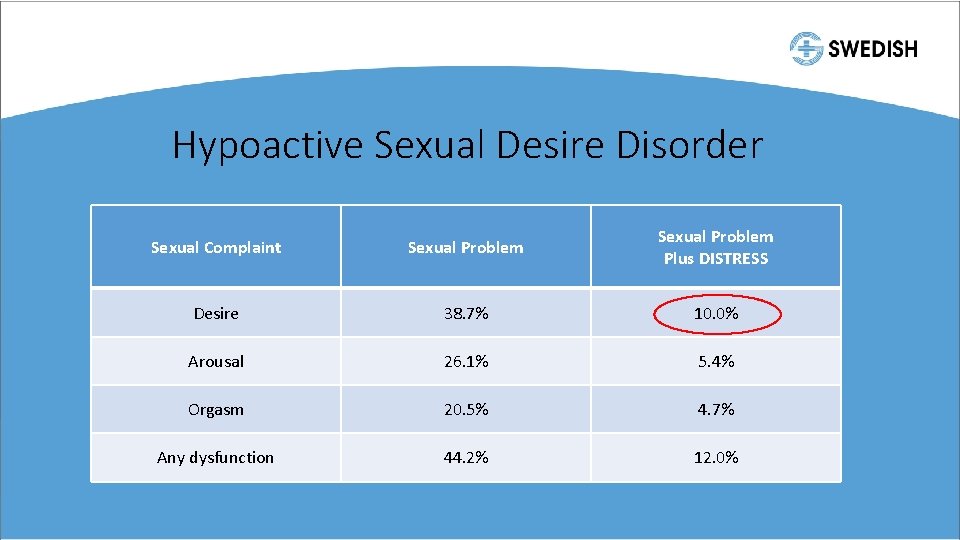
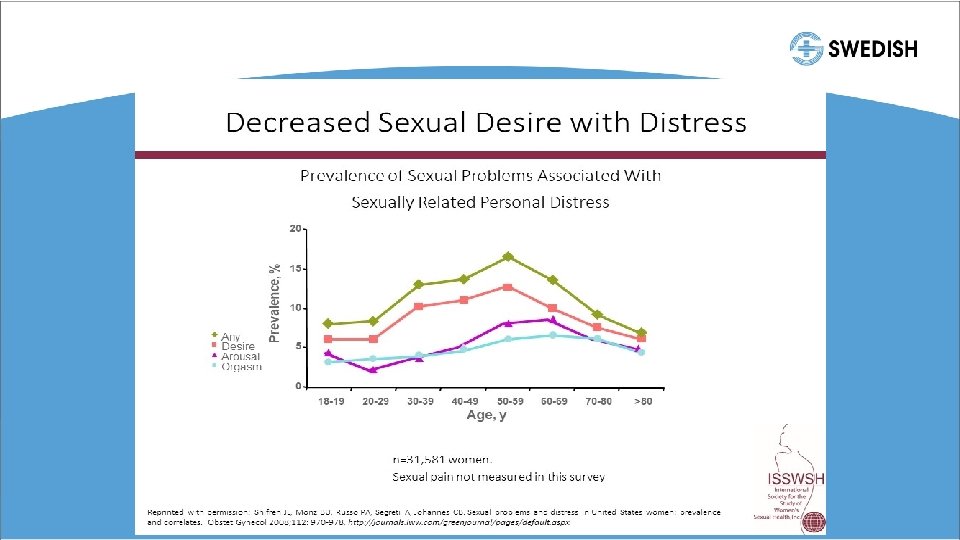
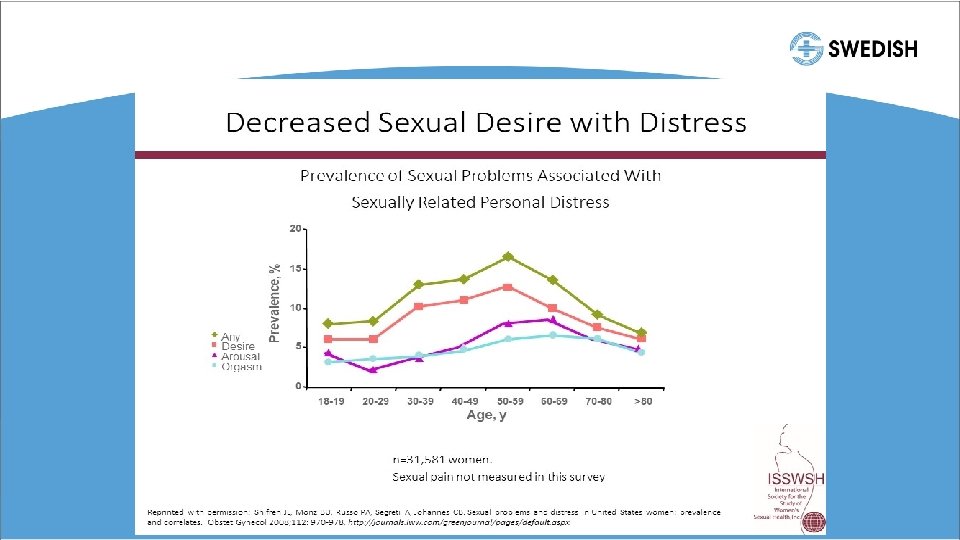
Prevalence of Female Sexual Dysfunction PRESIDE Sexual Complaint Sexual Problem Plus DISTRESS Desire 38. 7% 10. 0% Arousal 26. 1% 5. 4% Orgasm 20. 5% 4. 7% Any dysfunction 44. 2% 12. 0% PRESIDE is Prevalence of Female Sexual Problems and Distress and Determinants of Treatment Seeking Shifren JL, Monz BU, Russo PA, Segreti A, Johannes CB. Sexual problems and distress in United States women. Obstet Gynecol. 2008; 112(5): 970 -978.
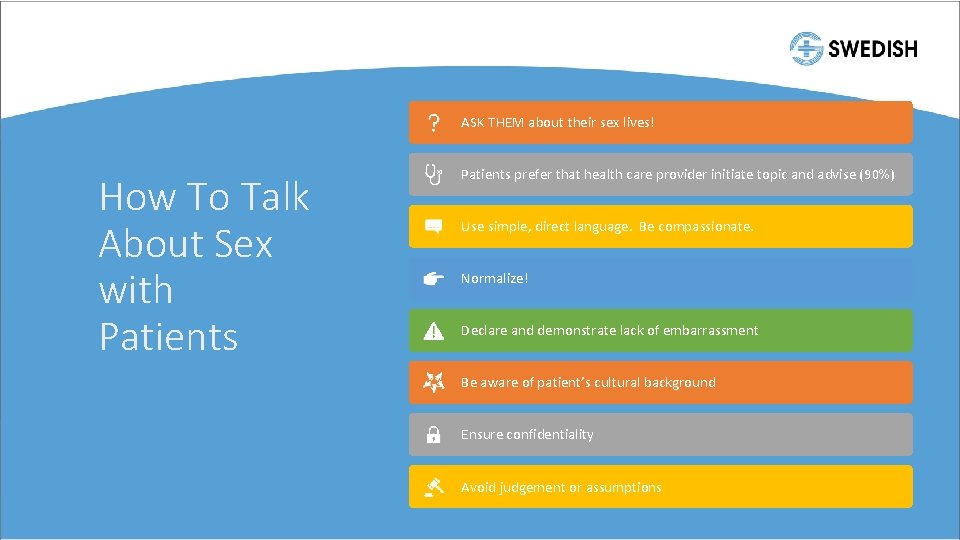
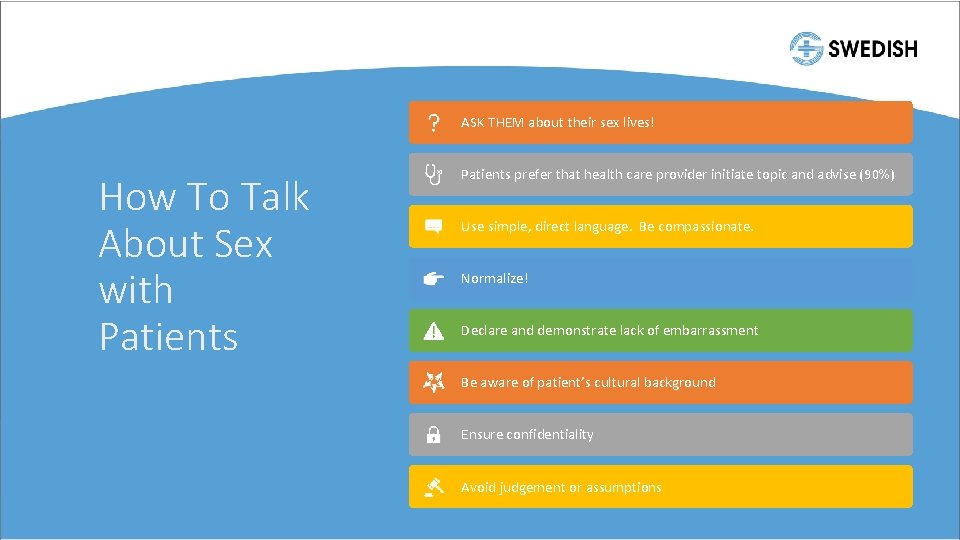
ASK THEM about their sex lives! How To Talk About Sex with Patients prefer that health care provider initiate topic and advise (90%) Use simple, direct language. Be compassionate. Normalize! Declare and demonstrate lack of embarrassment Be aware of patient’s cultural background Ensure confidentiality Avoid judgement or assumptions
• 48 y/o G 2 P 2 here for annual • Some hot flashes, some night sweats. Still having periods. • “We’ve been having less frequent sex over the last few years and I was fine with it, but he’s not. I love him but I just don’t have any desire to have sex anymore. It’s definitely putting stress on our relationship. ”
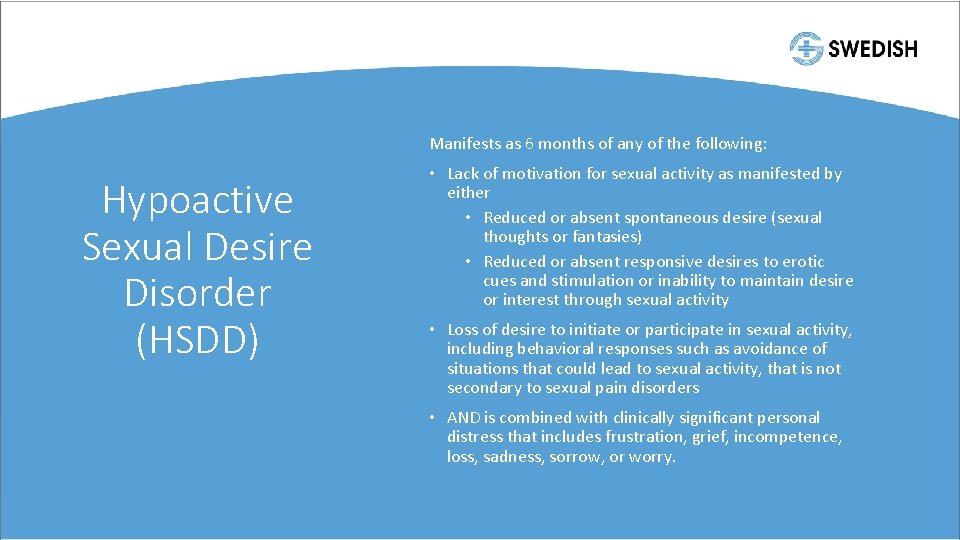
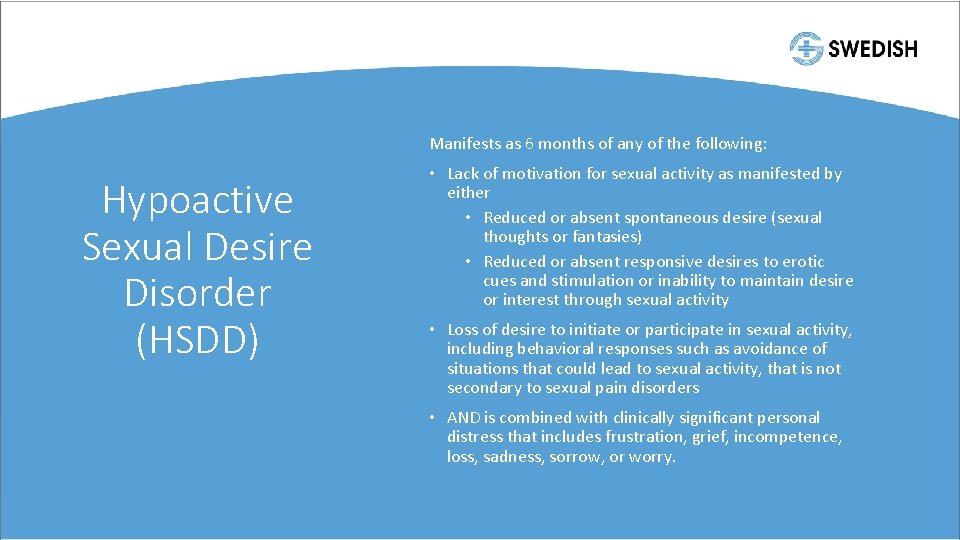
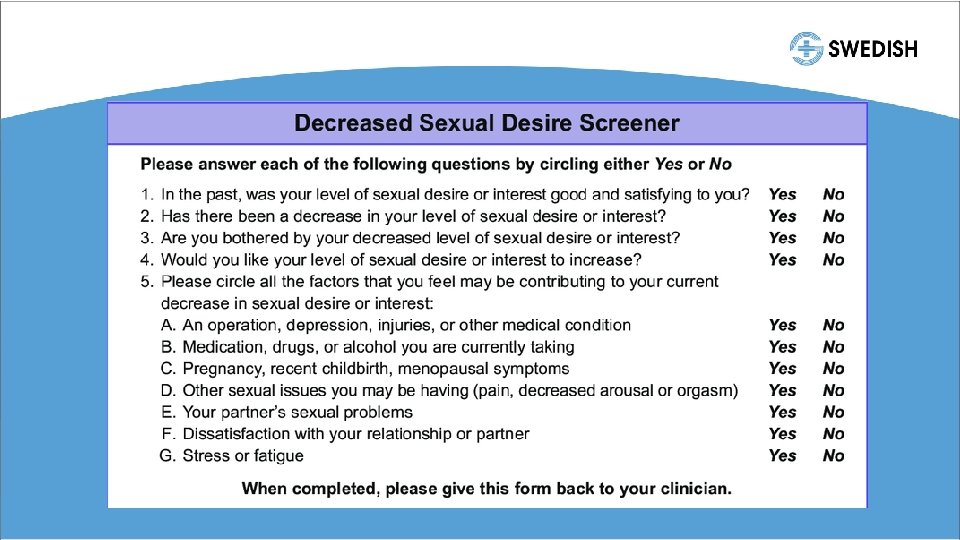
Manifests as 6 months of any of the following: Hypoactive Sexual Desire Disorder (HSDD) • Lack of motivation for sexual activity as manifested by either • Reduced or absent spontaneous desire (sexual thoughts or fantasies) • Reduced or absent responsive desires to erotic cues and stimulation or inability to maintain desire or interest through sexual activity • Loss of desire to initiate or participate in sexual activity, including behavioral responses such as avoidance of situations that could lead to sexual activity, that is not secondary to sexual pain disorders • AND is combined with clinically significant personal distress that includes frustration, grief, incompetence, loss, sadness, sorrow, or worry.
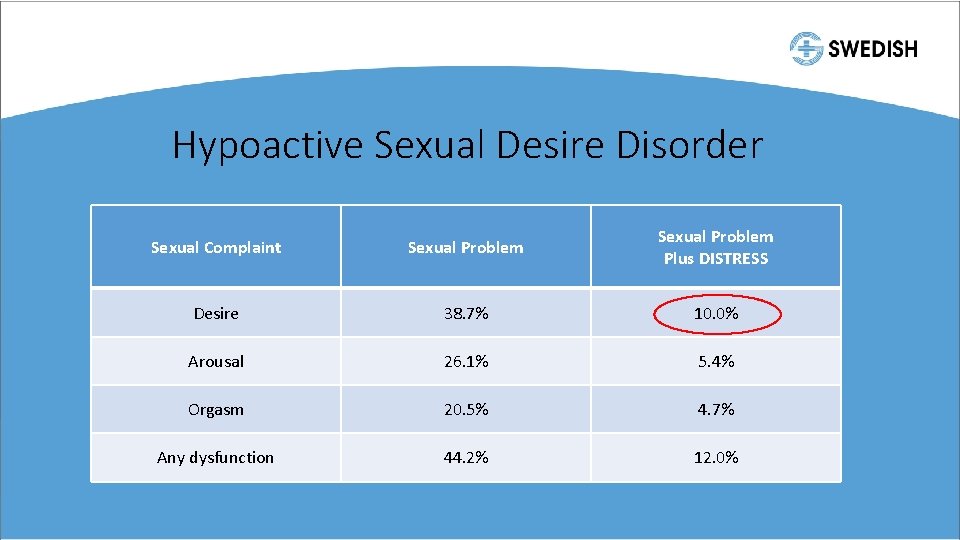
Hypoactive Sexual Desire Disorder Sexual Complaint Sexual Problem Plus DISTRESS Desire 38. 7% 10. 0% Arousal 26. 1% 5. 4% Orgasm 20. 5% 4. 7% Any dysfunction 44. 2% 12. 0%
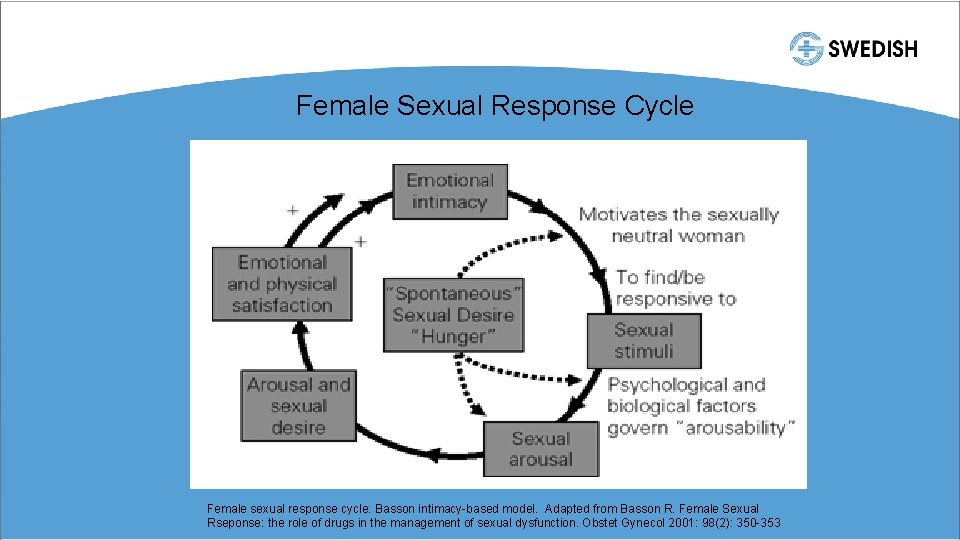
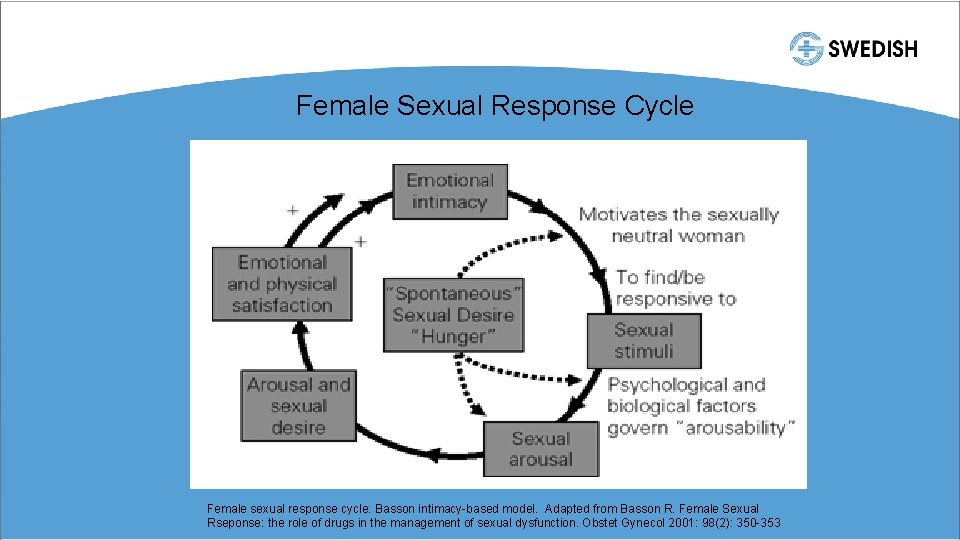
Female Sexual Response Cycle Female sexual response cycle: Basson intimacy-based model. Adapted from Basson R. Female Sexual Rseponse: the role of drugs in the management of sexual dysfunction. Obstet Gynecol 2001: 98(2): 350 -353
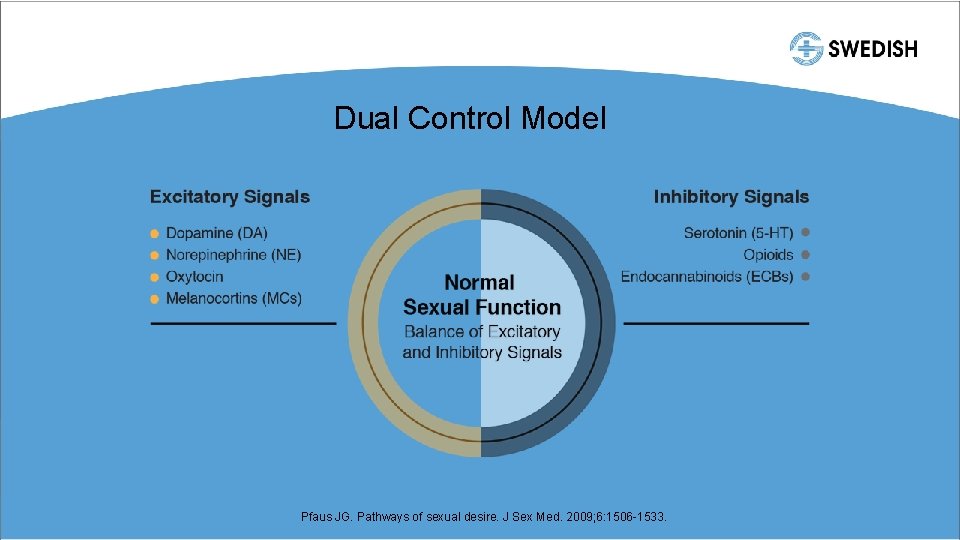
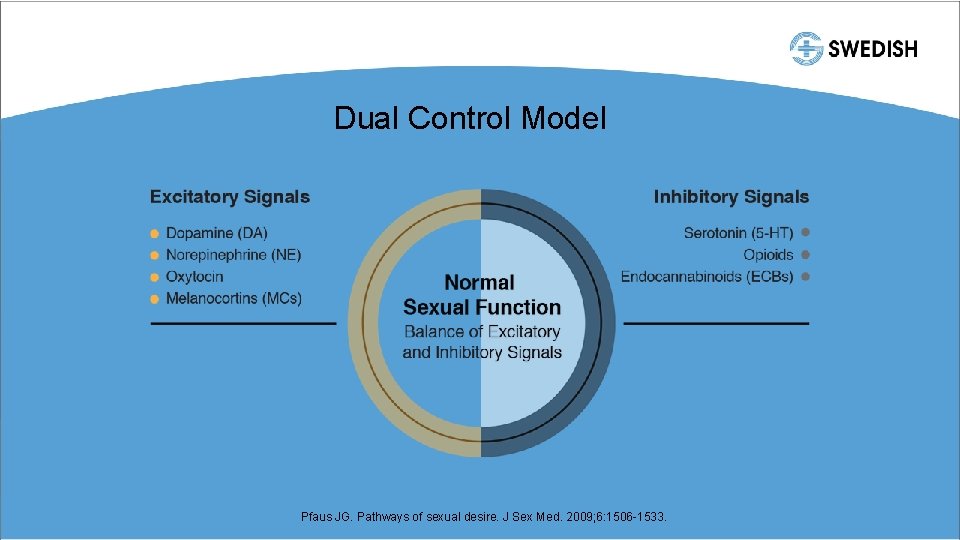
Dual Control Model Pfaus JG. Pathways of sexual desire. J Sex Med. 2009; 6: 1506 -1533.
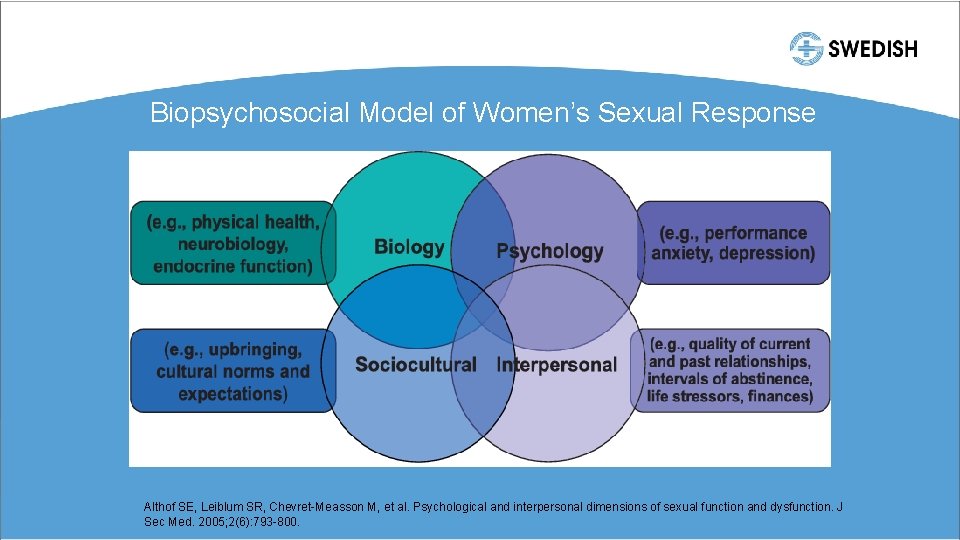
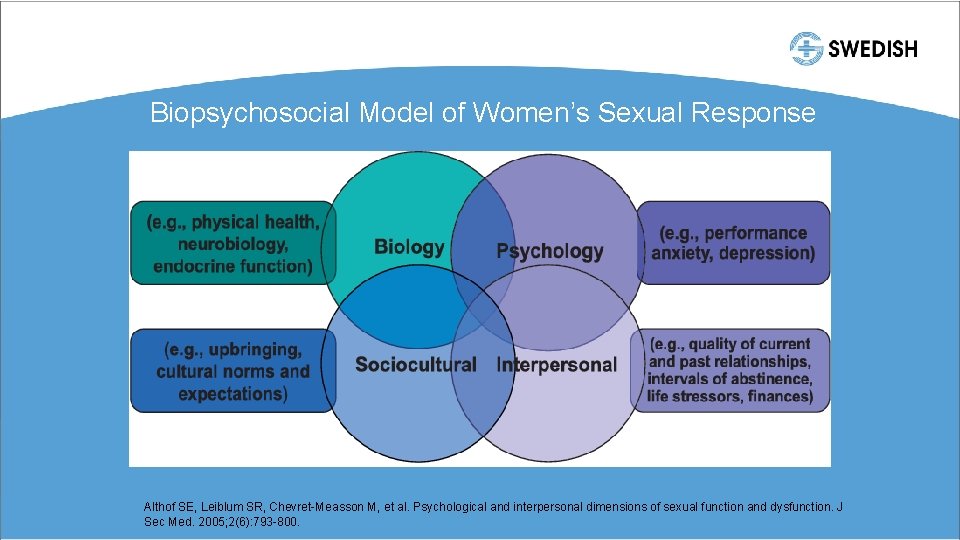
Biopsychosocial Model of Women’s Sexual Response Althof SE, Leiblum SR, Chevret-Measson M, et al. Psychological and interpersonal dimensions of sexual function and dysfunction. J Sec Med. 2005; 2(6): 793 -800.
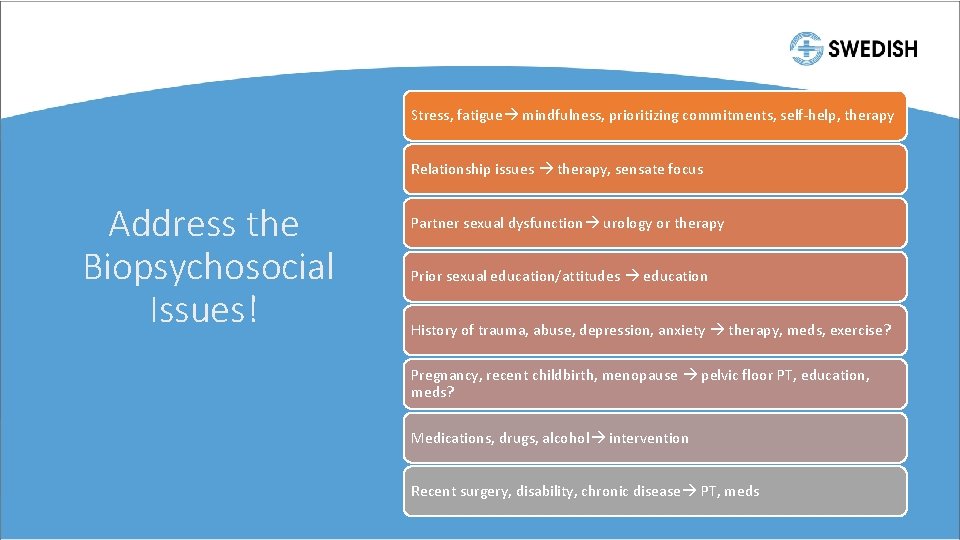
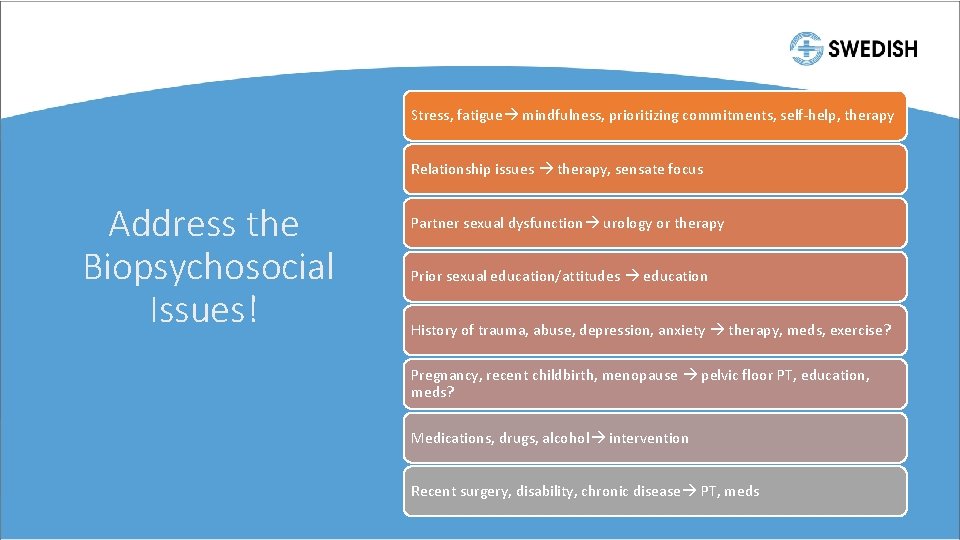
Stress, fatigue mindfulness, prioritizing commitments, self-help, therapy Relationship issues therapy, sensate focus Address the Biopsychosocial Issues! Partner sexual dysfunction urology or therapy Prior sexual education/attitudes education History of trauma, abuse, depression, anxiety therapy, meds, exercise? Pregnancy, recent childbirth, menopause pelvic floor PT, education, meds? Medications, drugs, alcohol intervention Recent surgery, disability, chronic disease PT, meds
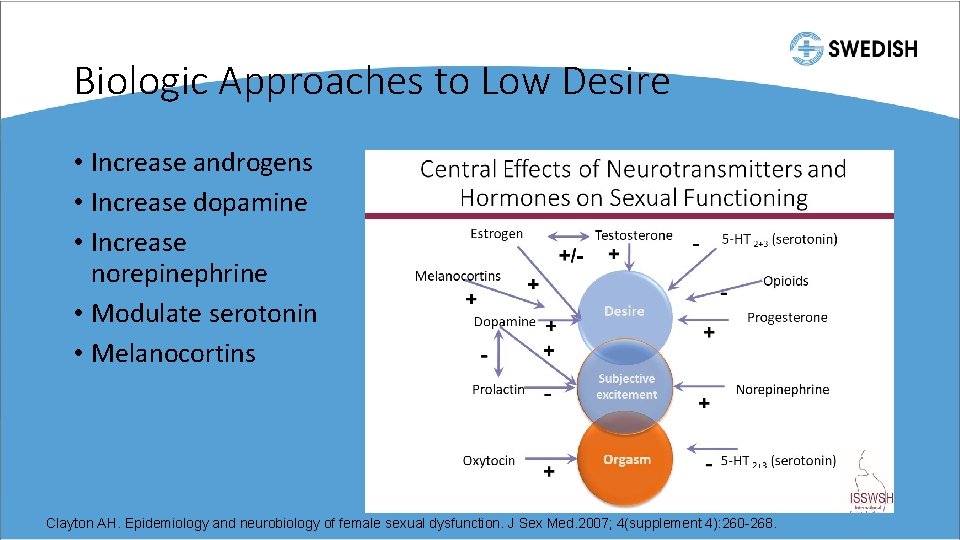
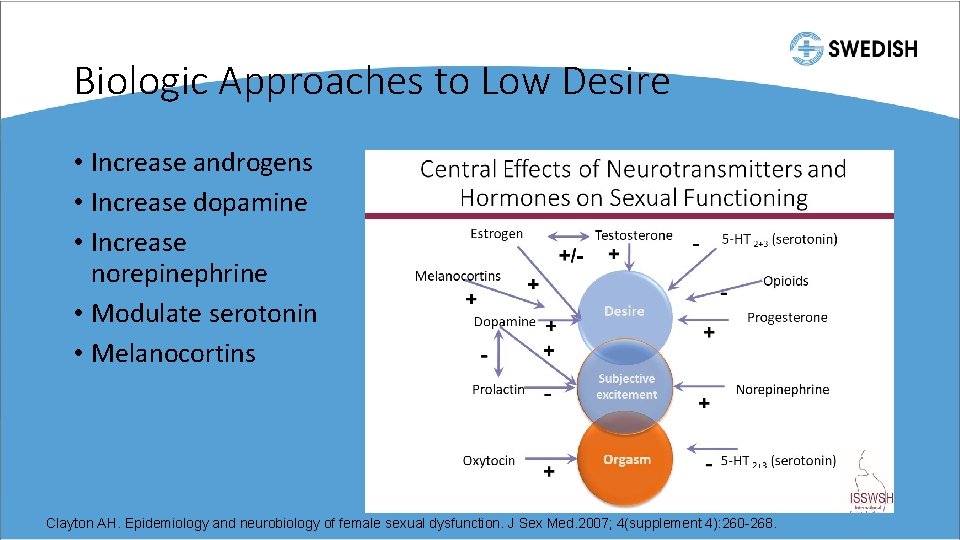
Biologic Approaches to Low Desire • Increase androgens • Increase dopamine • Increase norepinephrine • Modulate serotonin • Melanocortins Clayton AH. Epidemiology and neurobiology of female sexual dysfunction. J Sex Med. 2007; 4(supplement 4): 260 -268.
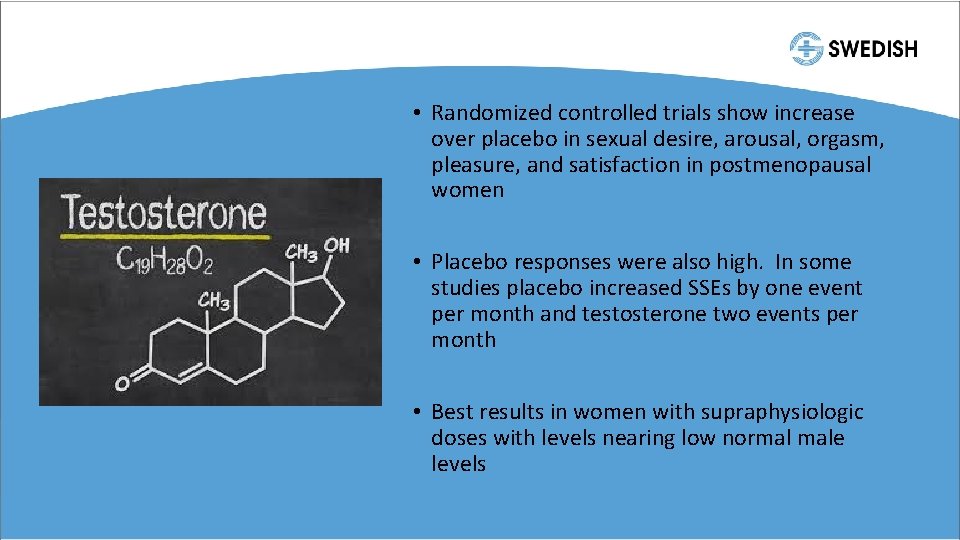
• Randomized controlled trials show increase over placebo in sexual desire, arousal, orgasm, pleasure, and satisfaction in postmenopausal women • Placebo responses were also high. In some studies placebo increased SSEs by one event per month and testosterone two events per month • Best results in women with supraphysiologic doses with levels nearing low normal male levels
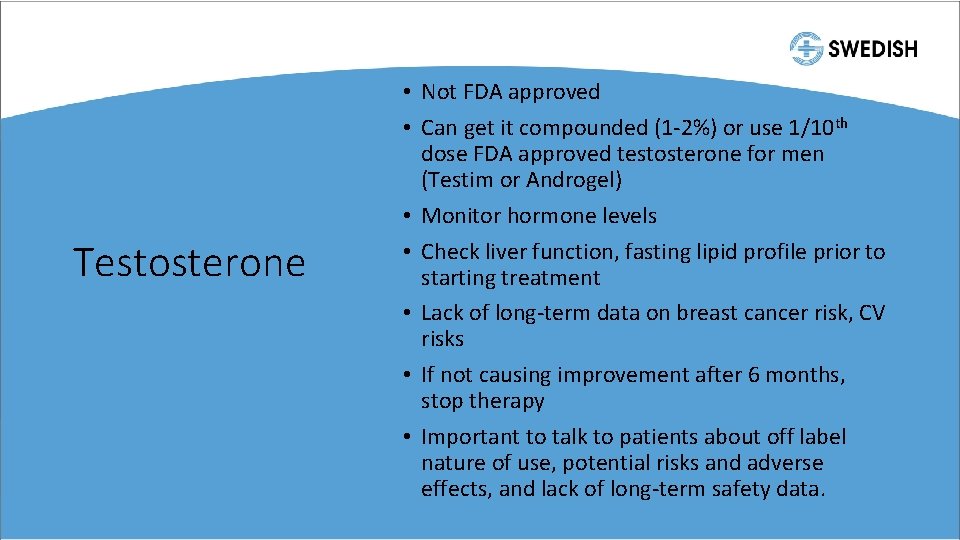
Testosterone • Not FDA approved • Can get it compounded (1 -2%) or use 1/10 th dose FDA approved testosterone for men (Testim or Androgel) • Monitor hormone levels • Check liver function, fasting lipid profile prior to starting treatment • Lack of long-term data on breast cancer risk, CV risks • If not causing improvement after 6 months, stop therapy • Important to talk to patients about off label nature of use, potential risks and adverse effects, and lack of long-term safety data.
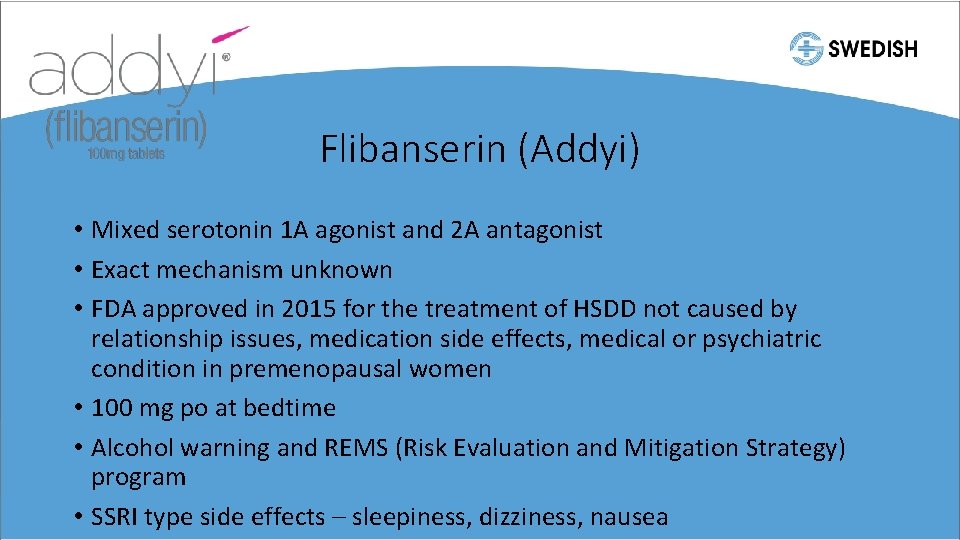
Flibanserin (Addyi) • Mixed serotonin 1 A agonist and 2 A antagonist • Exact mechanism unknown • FDA approved in 2015 for the treatment of HSDD not caused by relationship issues, medication side effects, medical or psychiatric condition in premenopausal women • 100 mg po at bedtime • Alcohol warning and REMS (Risk Evaluation and Mitigation Strategy) program • SSRI type side effects – sleepiness, dizziness, nausea
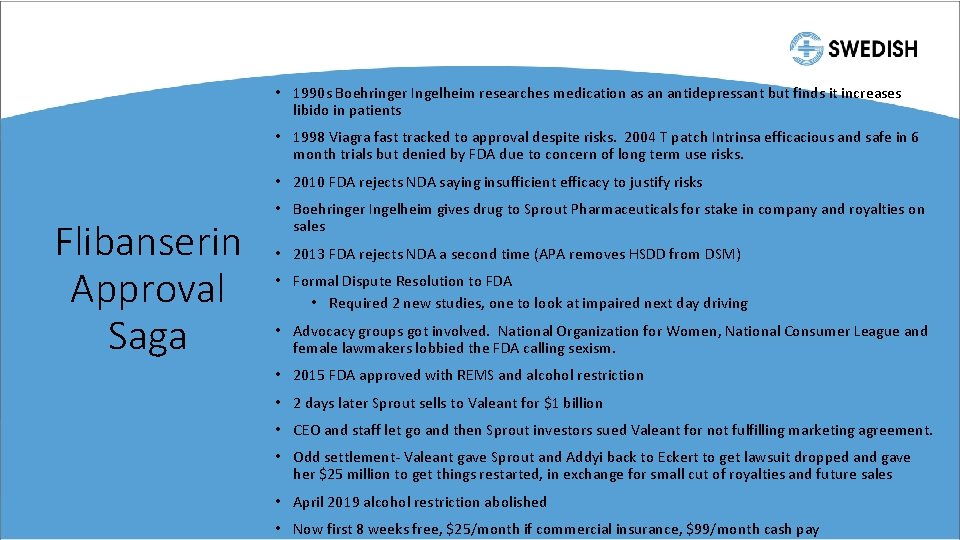
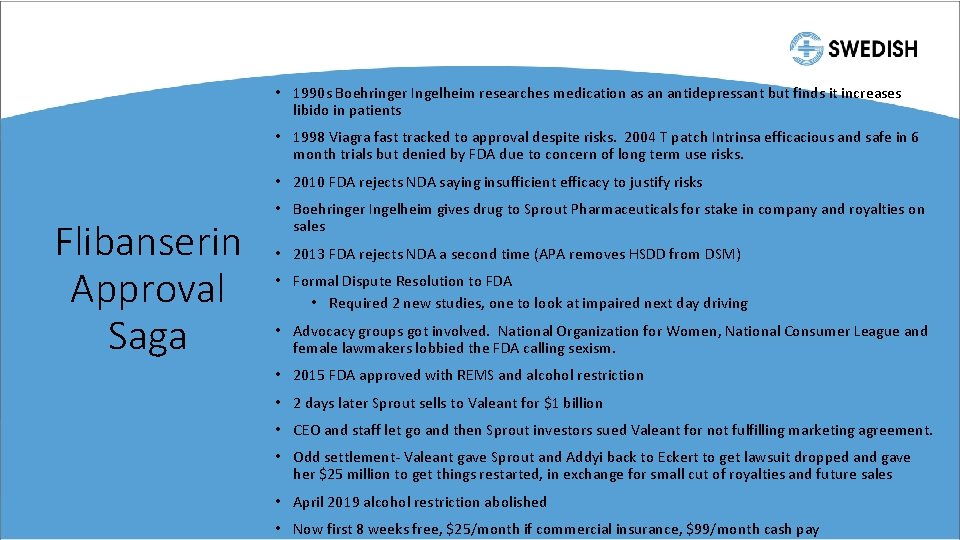
• 1990 s Boehringer Ingelheim researches medication as an antidepressant but finds it increases libido in patients • 1998 Viagra fast tracked to approval despite risks. 2004 T patch Intrinsa efficacious and safe in 6 month trials but denied by FDA due to concern of long term use risks. • 2010 FDA rejects NDA saying insufficient efficacy to justify risks Flibanserin Approval Saga • Boehringer Ingelheim gives drug to Sprout Pharmaceuticals for stake in company and royalties on sales • 2013 FDA rejects NDA a second time (APA removes HSDD from DSM) • Formal Dispute Resolution to FDA • Required 2 new studies, one to look at impaired next day driving • Advocacy groups got involved. National Organization for Women, National Consumer League and female lawmakers lobbied the FDA calling sexism. • 2015 FDA approved with REMS and alcohol restriction • 2 days later Sprout sells to Valeant for $1 billion • CEO and staff let go and then Sprout investors sued Valeant for not fulfilling marketing agreement. • Odd settlement- Valeant gave Sprout and Addyi back to Eckert to get lawsuit dropped and gave her $25 million to get things restarted, in exchange for small cut of royalties and future sales • April 2019 alcohol restriction abolished • Now first 8 weeks free, $25/month if commercial insurance, $99/month cash pay
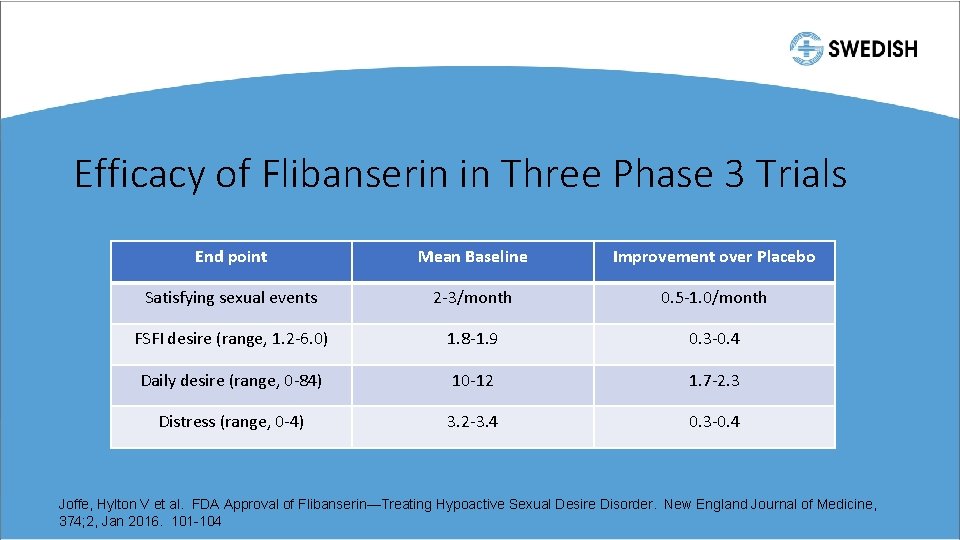
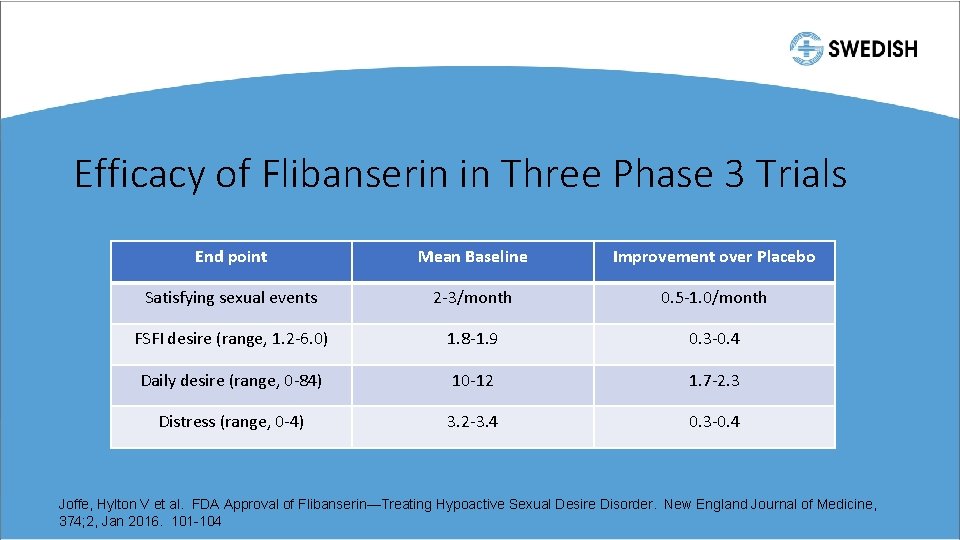
Efficacy of Flibanserin in Three Phase 3 Trials End point Mean Baseline Improvement over Placebo Satisfying sexual events 2 -3/month 0. 5 -1. 0/month FSFI desire (range, 1. 2 -6. 0) 1. 8 -1. 9 0. 3 -0. 4 Daily desire (range, 0 -84) 10 -12 1. 7 -2. 3 Distress (range, 0 -4) 3. 2 -3. 4 0. 3 -0. 4 Joffe, Hylton V et al. FDA Approval of Flibanserin—Treating Hypoactive Sexual Desire Disorder. New England Journal of Medicine, 374; 2, Jan 2016. 101 -104
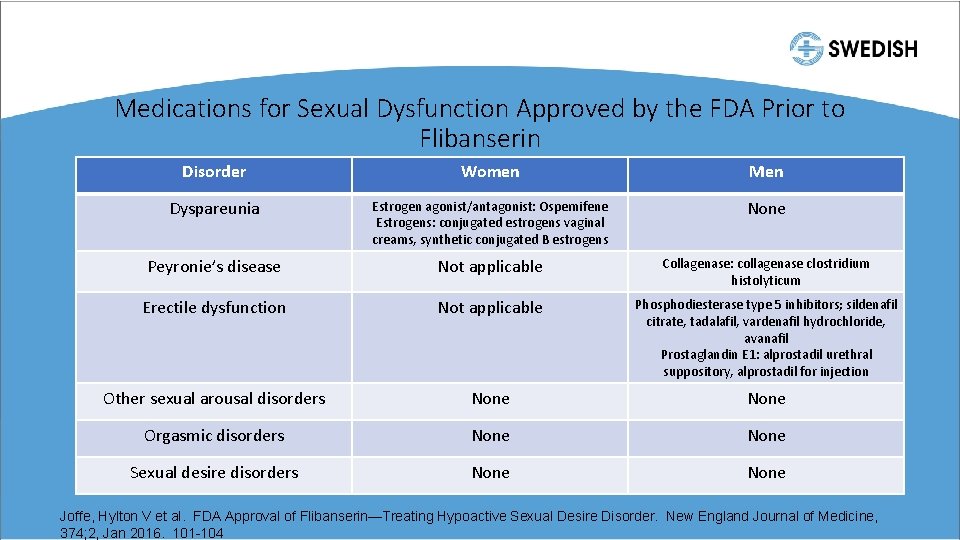
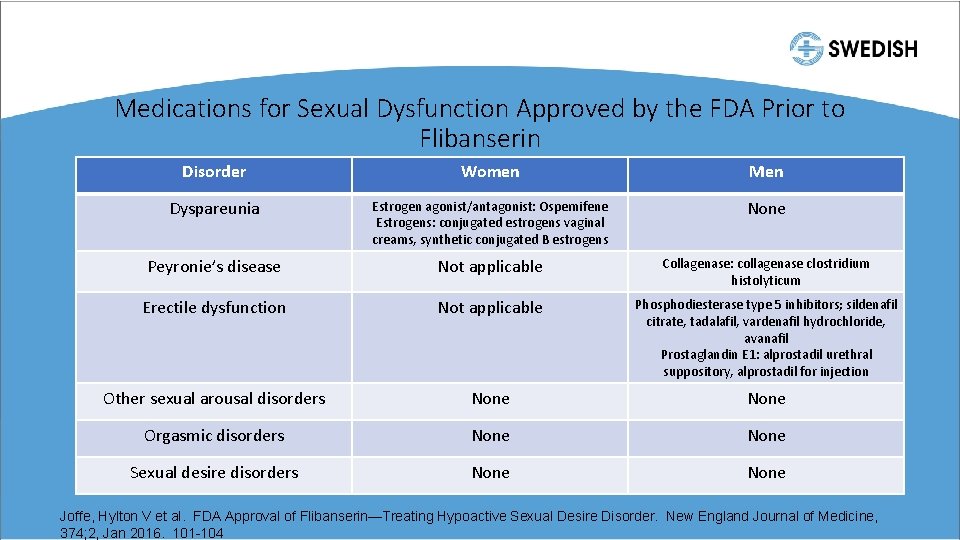
Medications for Sexual Dysfunction Approved by the FDA Prior to Flibanserin Disorder Women Men Dyspareunia Estrogen agonist/antagonist: Ospemifene Estrogens: conjugated estrogens vaginal creams, synthetic conjugated B estrogens None Peyronie’s disease Not applicable Collagenase: collagenase clostridium histolyticum Erectile dysfunction Not applicable Phosphodiesterase type 5 inhibitors; sildenafil citrate, tadalafil, vardenafil hydrochloride, avanafil Prostaglandin E 1: alprostadil urethral suppository, alprostadil for injection Other sexual arousal disorders None Orgasmic disorders None Sexual desire disorders None Joffe, Hylton V et al. FDA Approval of Flibanserin—Treating Hypoactive Sexual Desire Disorder. New England Journal of Medicine, 374; 2, Jan 2016. 101 -104
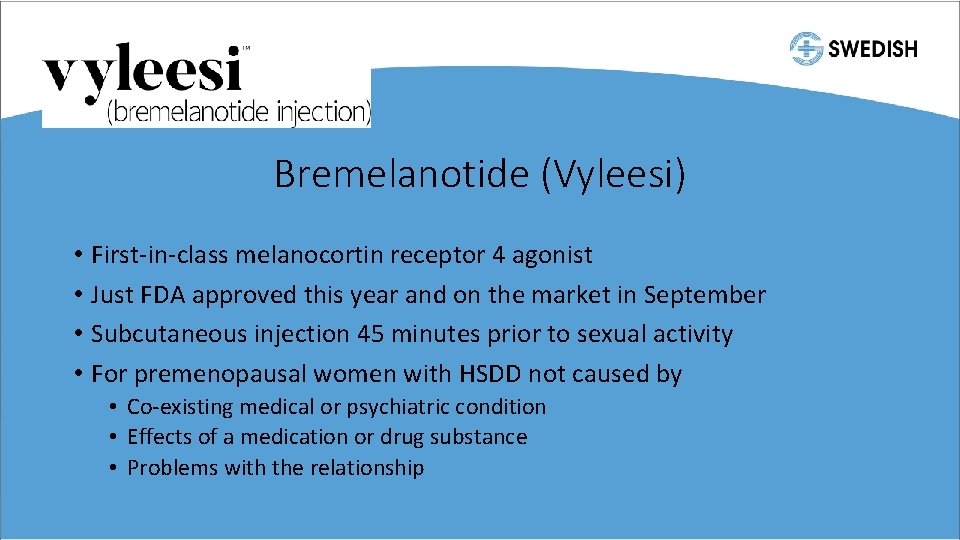
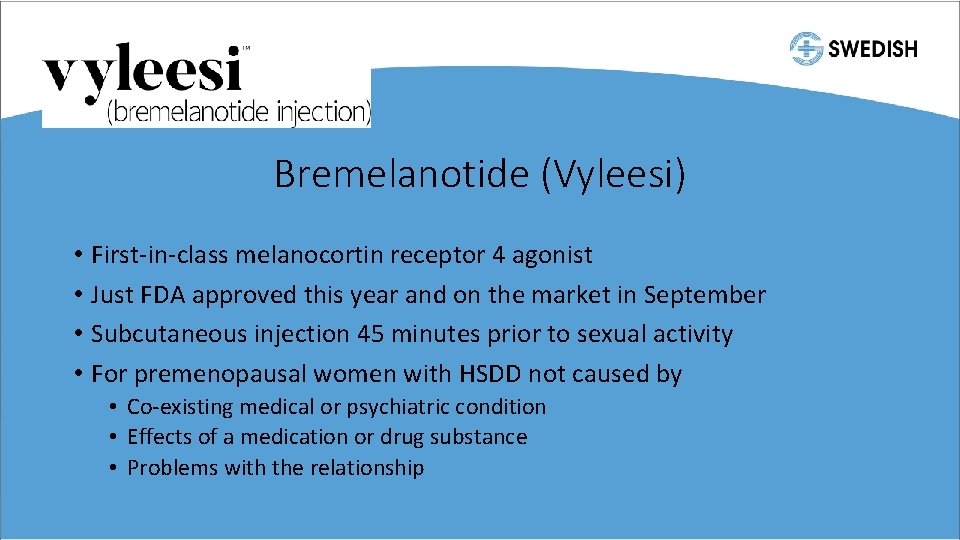
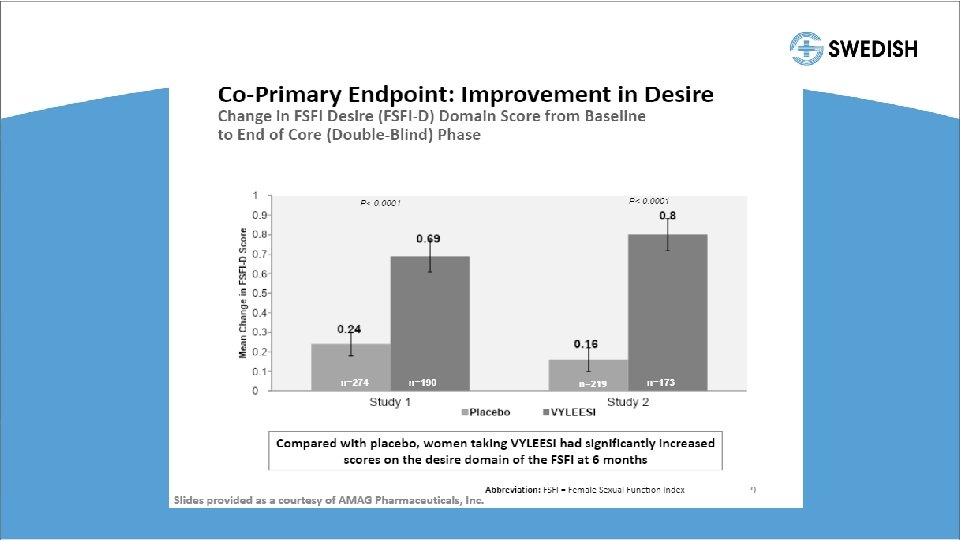
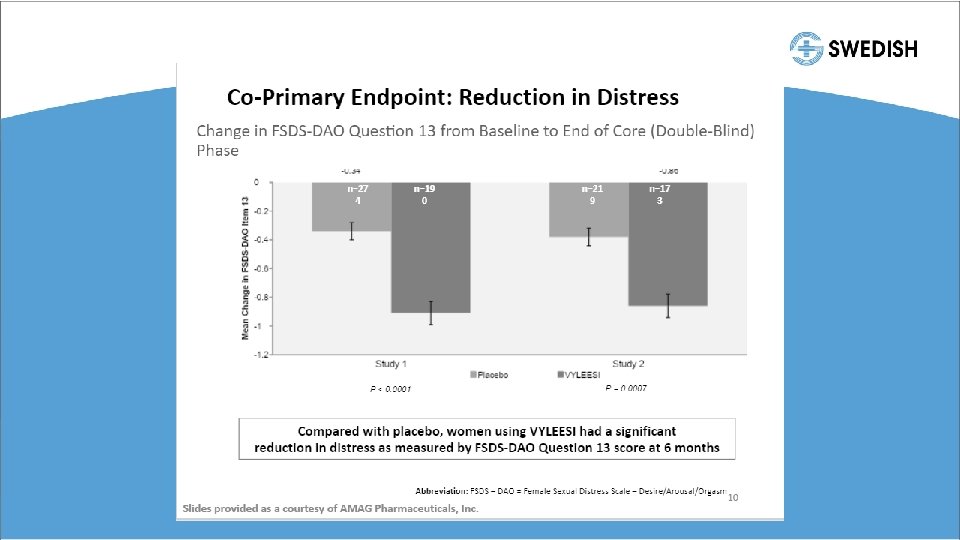
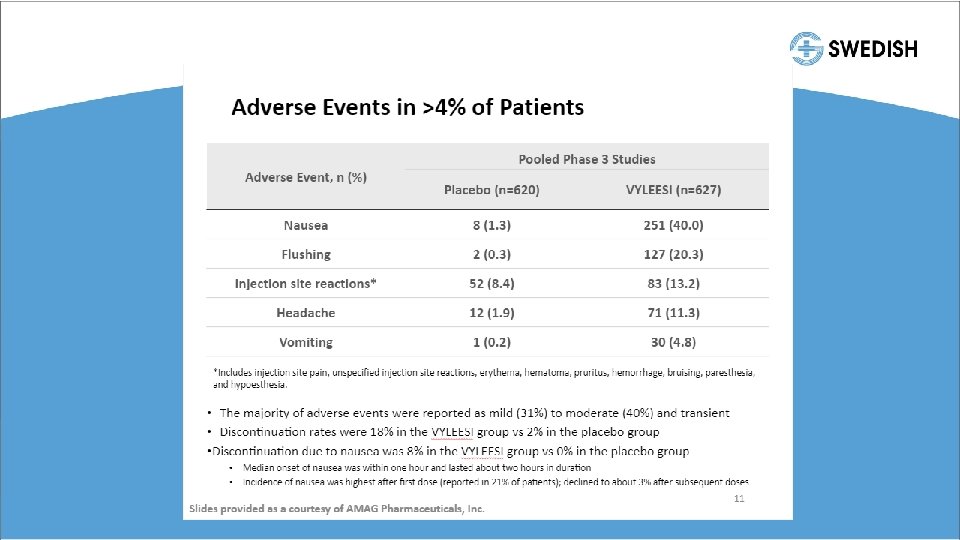
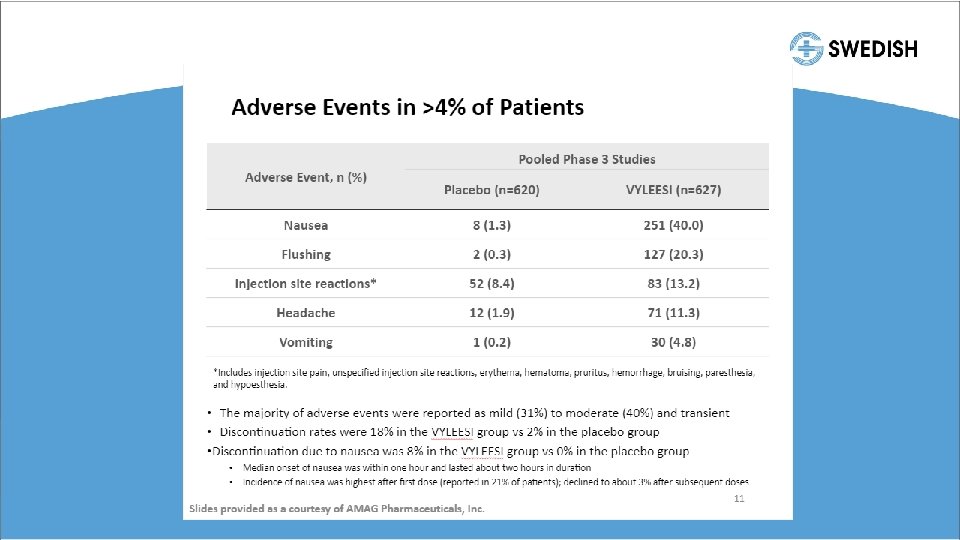
Bremelanotide (Vyleesi) • First-in-class melanocortin receptor 4 agonist • Just FDA approved this year and on the market in September • Subcutaneous injection 45 minutes prior to sexual activity • For premenopausal women with HSDD not caused by • Co-existing medical or psychiatric condition • Effects of a medication or drug substance • Problems with the relationship
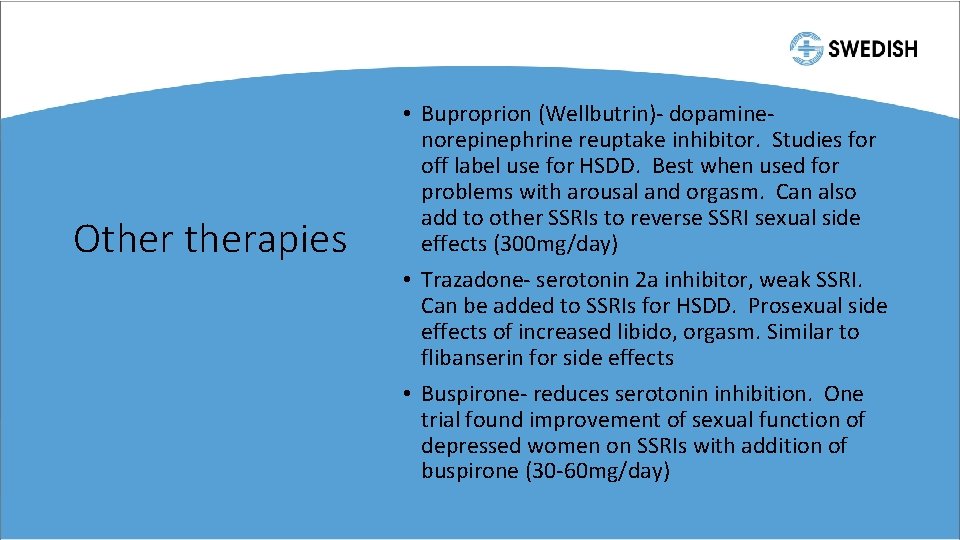
Otherapies • Buproprion (Wellbutrin)- dopaminenorepinephrine reuptake inhibitor. Studies for off label use for HSDD. Best when used for problems with arousal and orgasm. Can also add to other SSRIs to reverse SSRI sexual side effects (300 mg/day) • Trazadone- serotonin 2 a inhibitor, weak SSRI. Can be added to SSRIs for HSDD. Prosexual side effects of increased libido, orgasm. Similar to flibanserin for side effects • Buspirone- reduces serotonin inhibition. One trial found improvement of sexual function of depressed women on SSRIs with addition of buspirone (30 -60 mg/day)
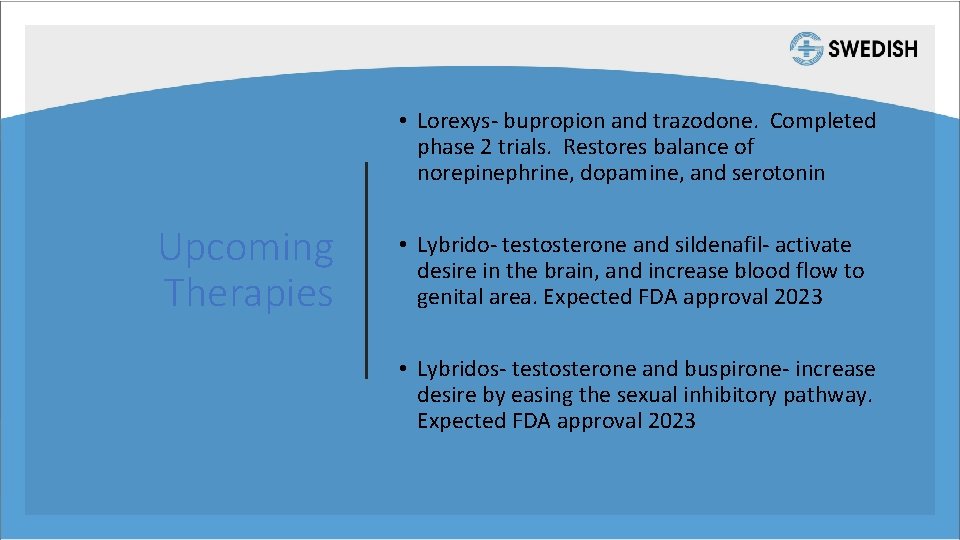
• Lorexys- bupropion and trazodone. Completed phase 2 trials. Restores balance of norepinephrine, dopamine, and serotonin Upcoming Therapies • Lybrido- testosterone and sildenafil- activate desire in the brain, and increase blood flow to genital area. Expected FDA approval 2023 • Lybridos- testosterone and buspirone- increase desire by easing the sexual inhibitory pathway. Expected FDA approval 2023
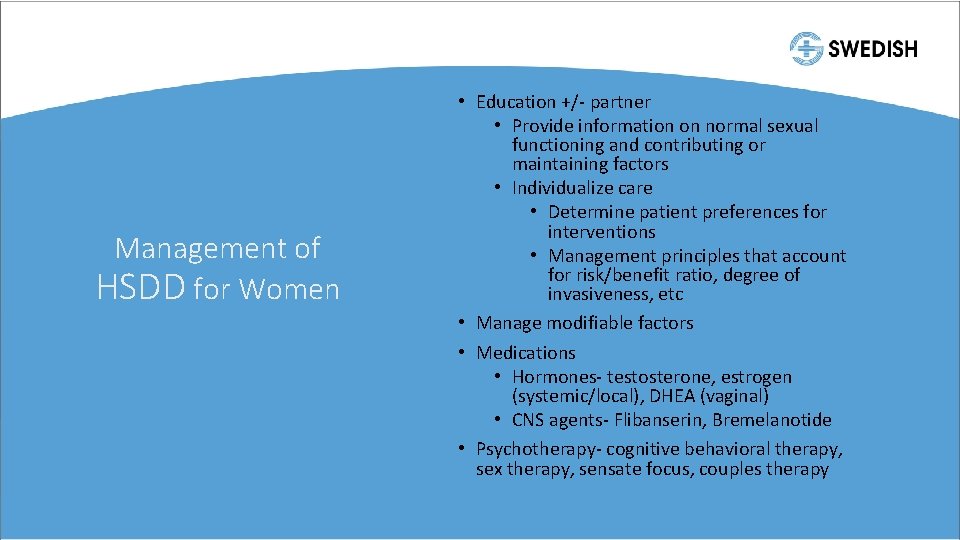
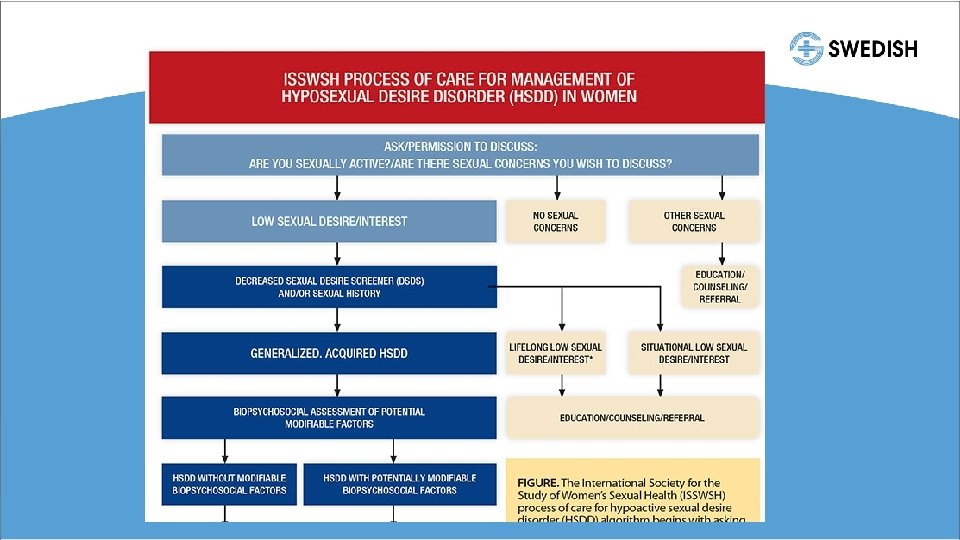
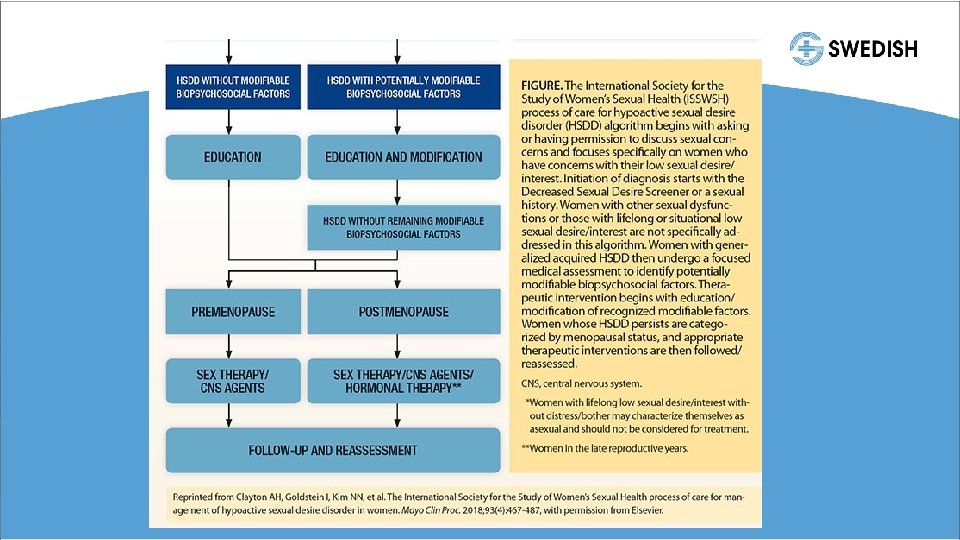
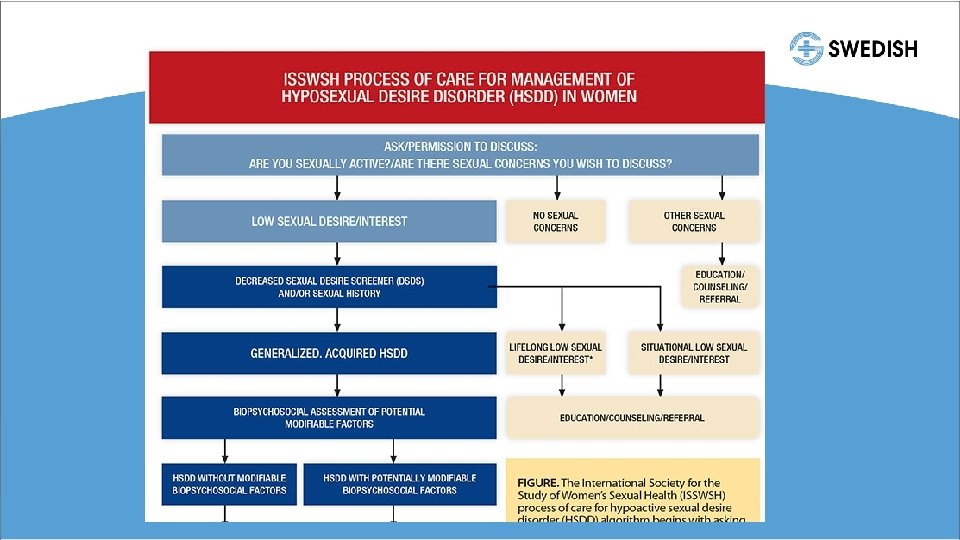
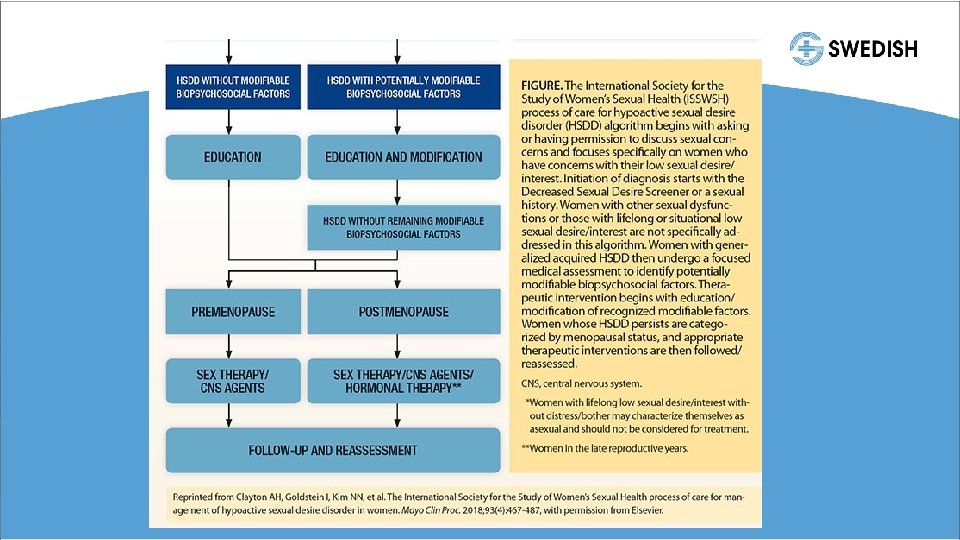
Management of HSDD for Women • Education +/- partner • Provide information on normal sexual functioning and contributing or maintaining factors • Individualize care • Determine patient preferences for interventions • Management principles that account for risk/benefit ratio, degree of invasiveness, etc • Manage modifiable factors • Medications • Hormones- testosterone, estrogen (systemic/local), DHEA (vaginal) • CNS agents- Flibanserin, Bremelanotide • Psychotherapy- cognitive behavioral therapy, sex therapy, sensate focus, couples therapy
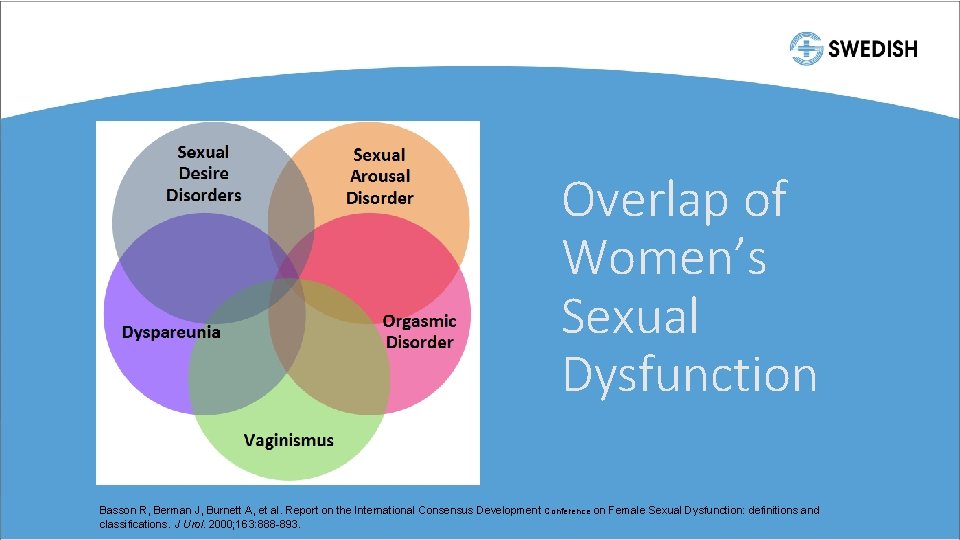
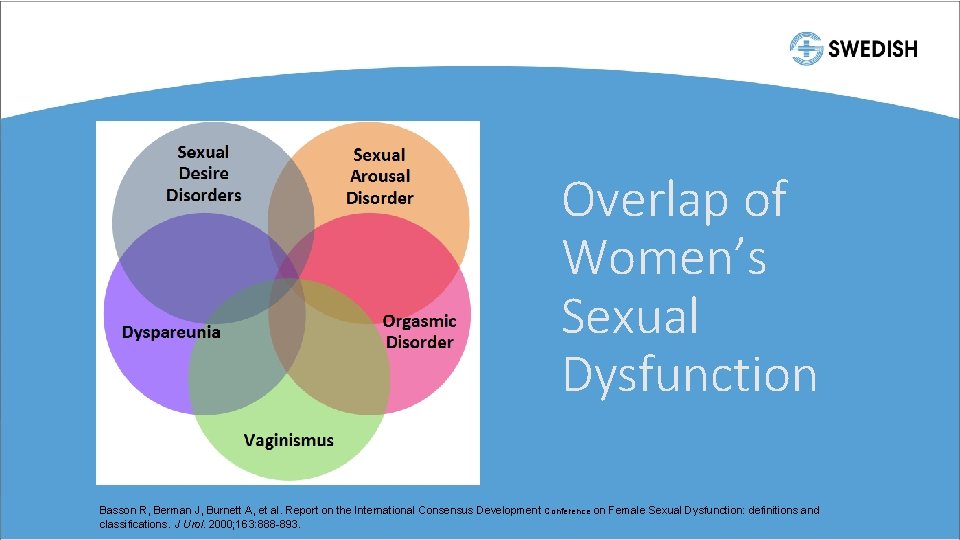
Overlap of Women’s Sexual Dysfunction Basson R, Berman J, Burnett A, et al. Report on the International Consensus Development Conference on Female Sexual Dysfunction: definitions and classifications. J Urol. 2000; 163: 888 -893.
New patient • • 62 y/o with dyspareunia Hasn’t had penetrative intercourse in 3 years Husband wants to be having sex Cries in pain when they try anything with penetration
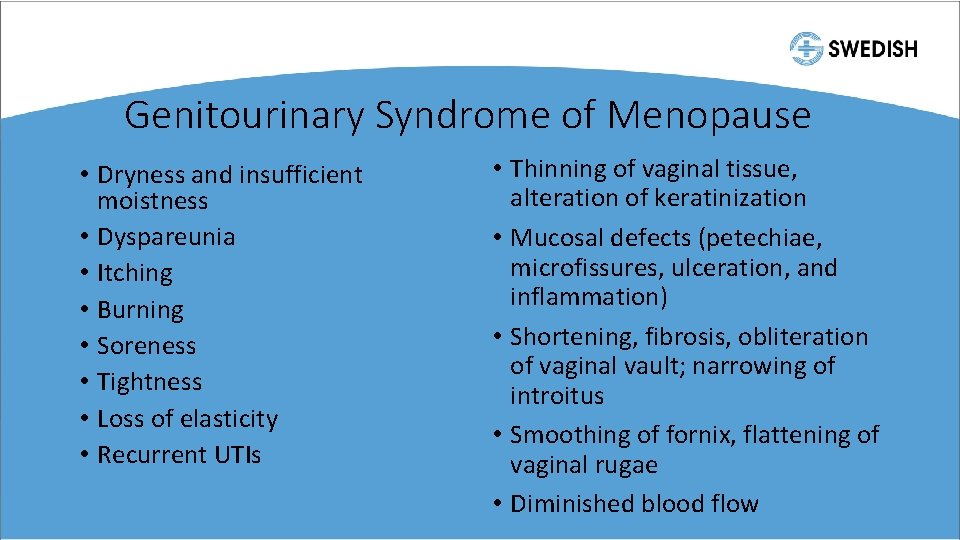
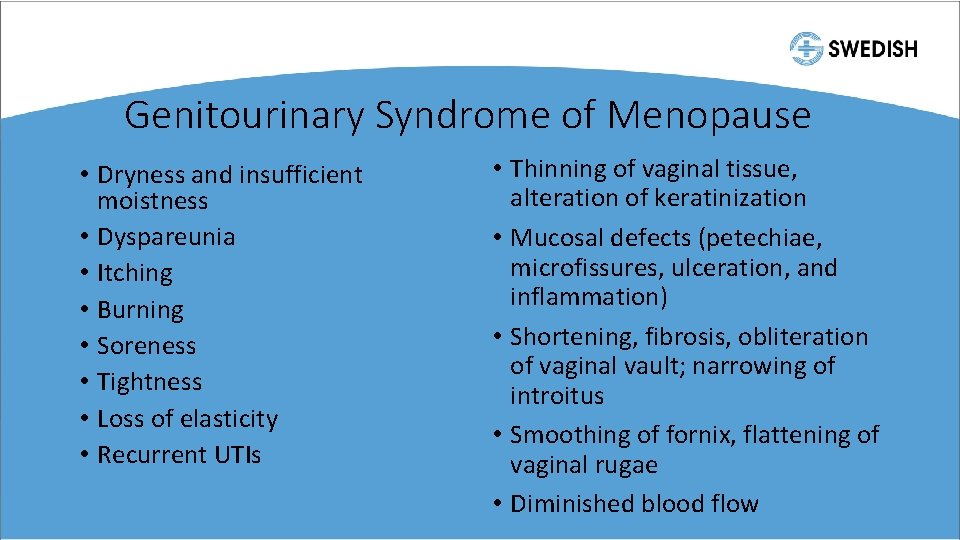
Genitourinary Syndrome of Menopause • Dryness and insufficient moistness • Dyspareunia • Itching • Burning • Soreness • Tightness • Loss of elasticity • Recurrent UTIs • Thinning of vaginal tissue, alteration of keratinization • Mucosal defects (petechiae, microfissures, ulceration, and inflammation) • Shortening, fibrosis, obliteration of vaginal vault; narrowing of introitus • Smoothing of fornix, flattening of vaginal rugae • Diminished blood flow
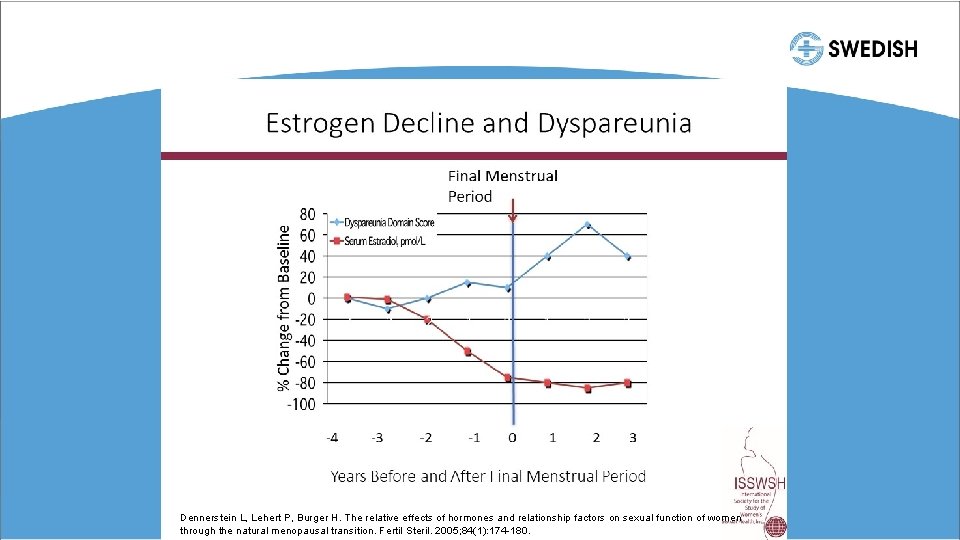
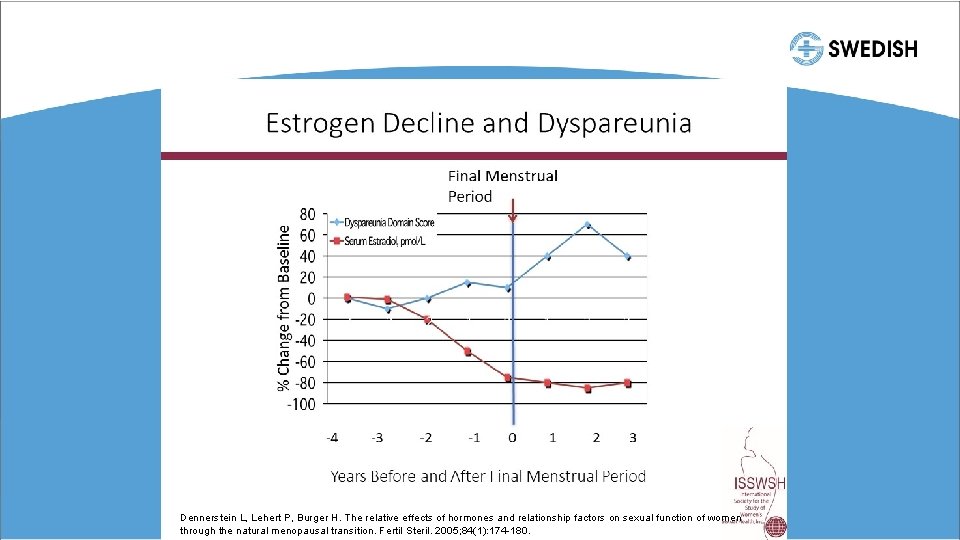
Dennerstein L, Lehert P, Burger H. The relative effects of hormones and relationship factors on sexual function of women through the natural menopausal transition. Fertil Steril. 2005; 84(1): 174 -180.
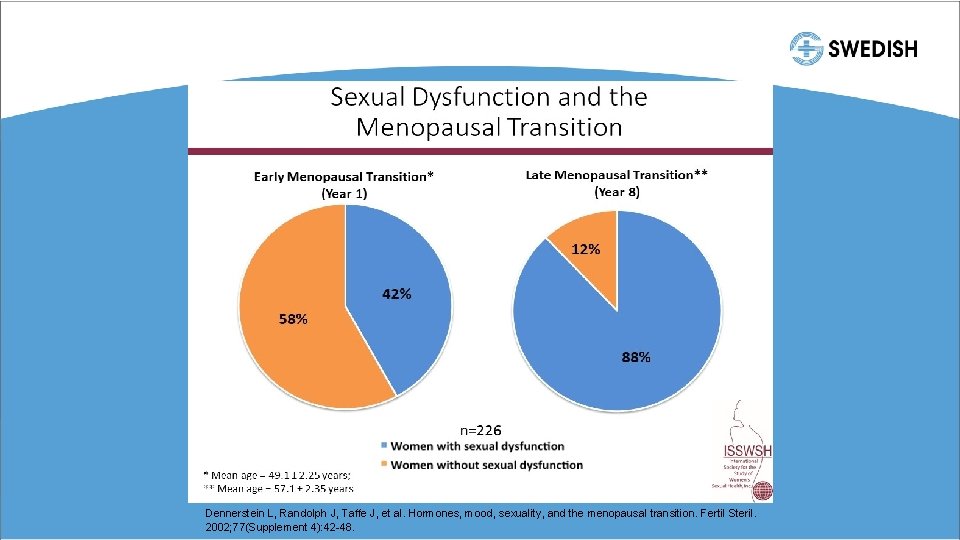
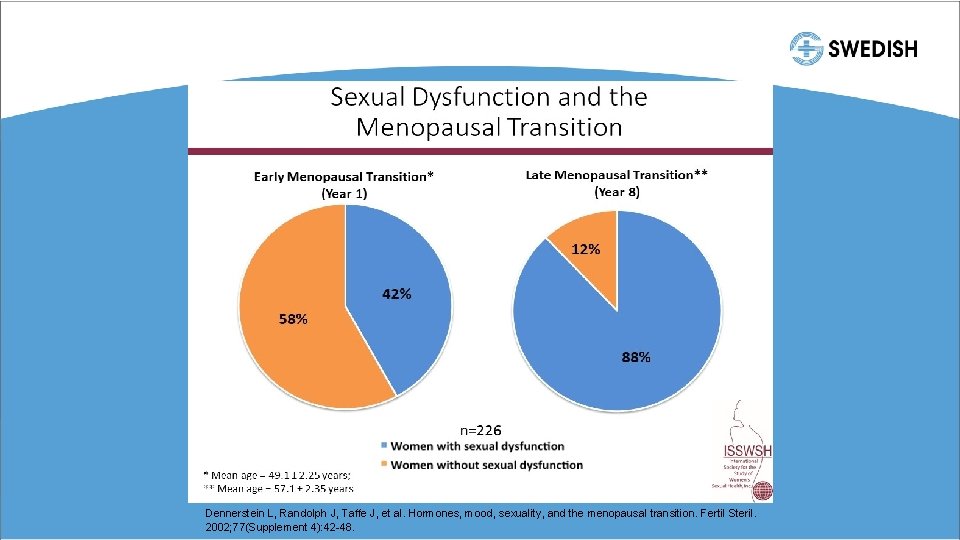
Dennerstein L, Randolph J, Taffe J, et al. Hormones, mood, sexuality, and the menopausal transition. Fertil Steril. 2002; 77(Supplement 4): 42 -48.
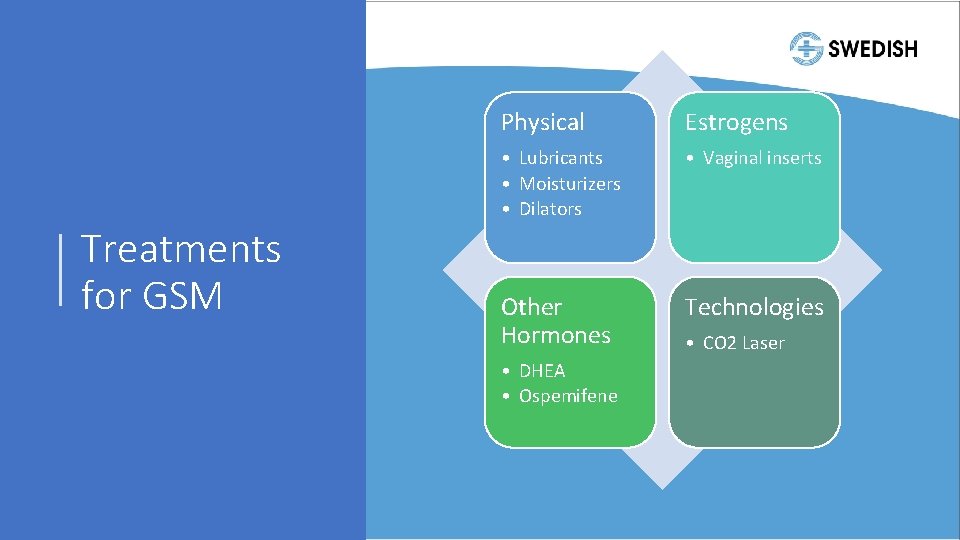
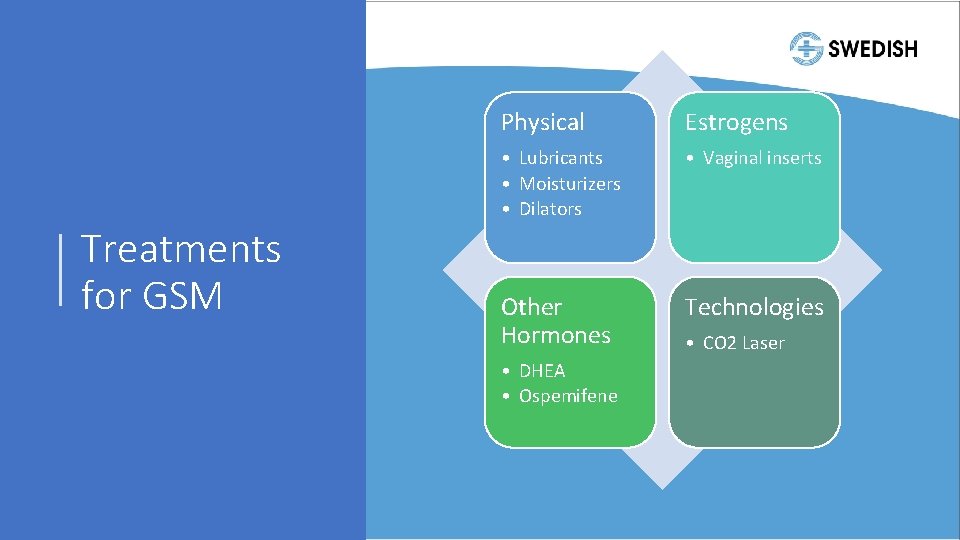
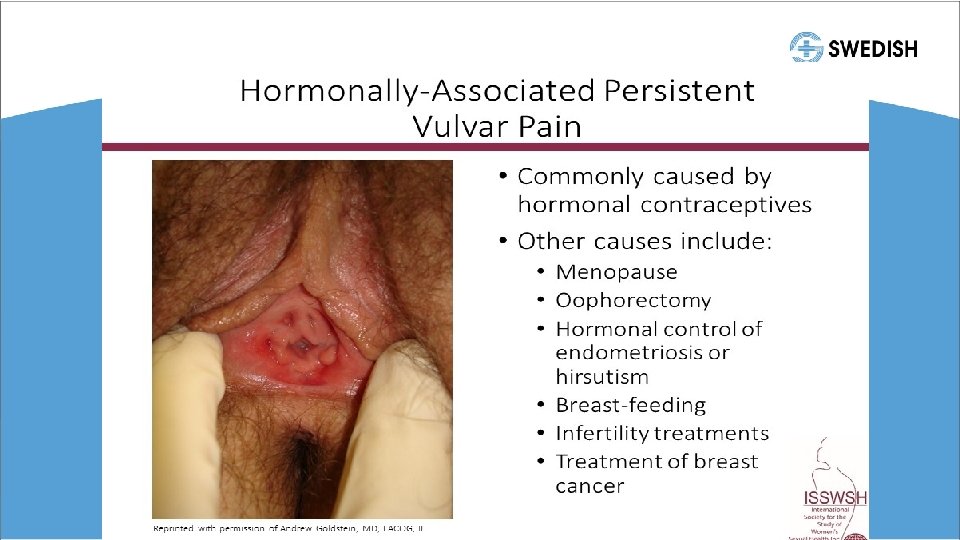
Treatments for GSM Physical Estrogens • Lubricants • Moisturizers • Dilators • Vaginal inserts Other Hormones Technologies • DHEA • Ospemifene • CO 2 Laser
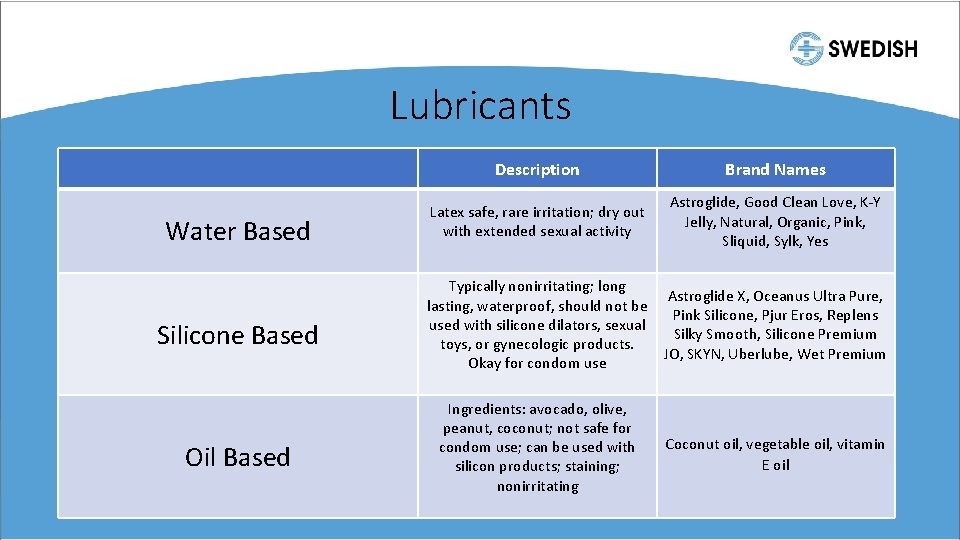
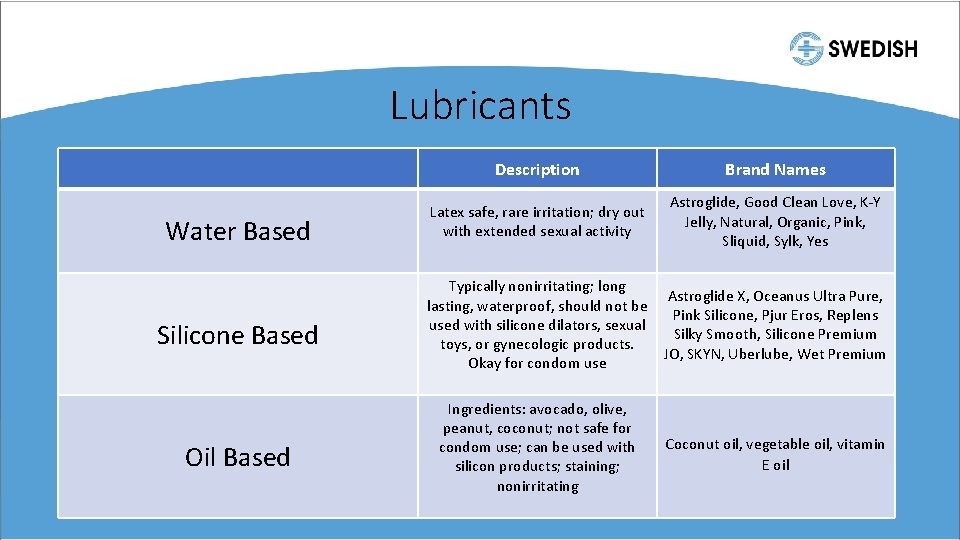
Lubricants Water Based Silicone Based Oil Based Description Brand Names Latex safe, rare irritation; dry out with extended sexual activity Astroglide, Good Clean Love, K-Y Jelly, Natural, Organic, Pink, Sliquid, Sylk, Yes Typically nonirritating; long Astroglide X, Oceanus Ultra Pure, lasting, waterproof, should not be Pink Silicone, Pjur Eros, Replens used with silicone dilators, sexual Silky Smooth, Silicone Premium toys, or gynecologic products. JO, SKYN, Uberlube, Wet Premium Okay for condom use Ingredients: avocado, olive, peanut, coconut; not safe for condom use; can be used with silicon products; staining; nonirritating Coconut oil, vegetable oil, vitamin E oil
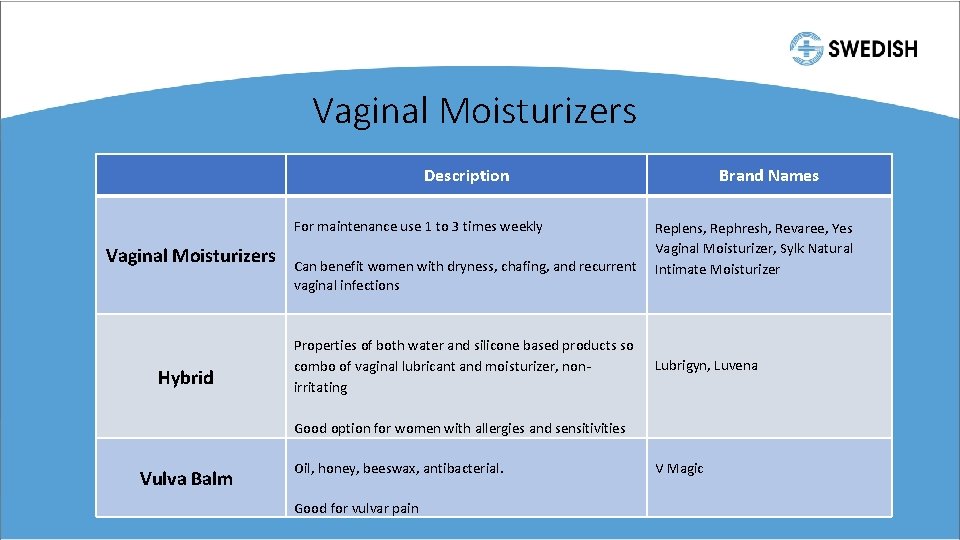
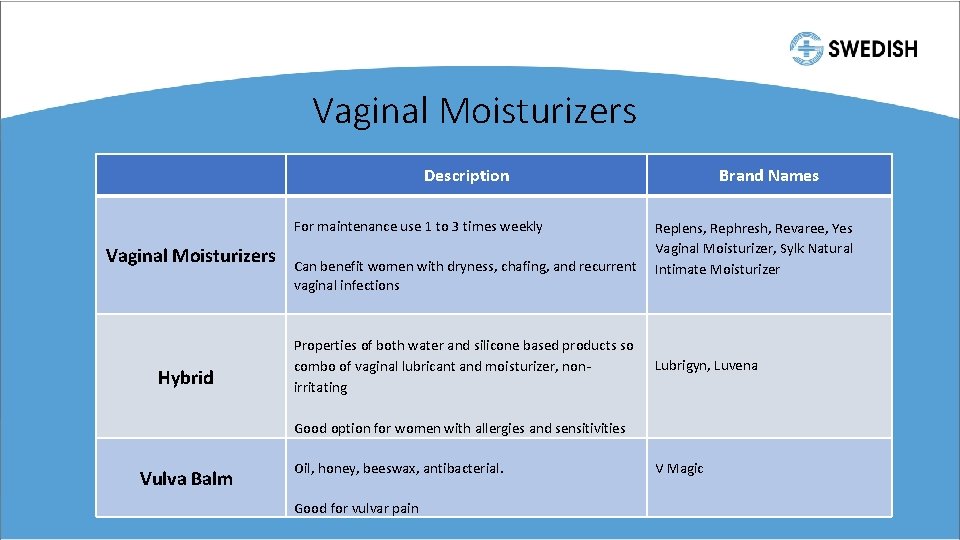
Vaginal Moisturizers Description Vaginal Moisturizers Hybrid Vulva Balm For maintenance use 1 to 3 times weekly Can benefit women with dryness, chafing, and recurrent vaginal infections Properties of both water and silicone based products so combo of vaginal lubricant and moisturizer, nonirritating Good option for women with allergies and sensitivities Oil, honey, beeswax, antibacterial. Good for vulvar pain Brand Names Replens, Rephresh, Revaree, Yes Vaginal Moisturizer, Sylk Natural Intimate Moisturizer Lubrigyn, Luvena V Magic
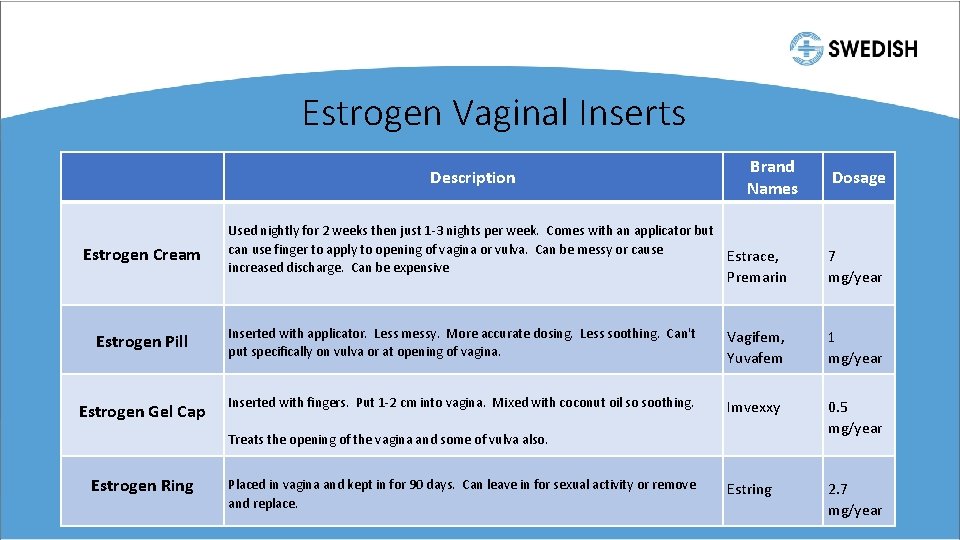
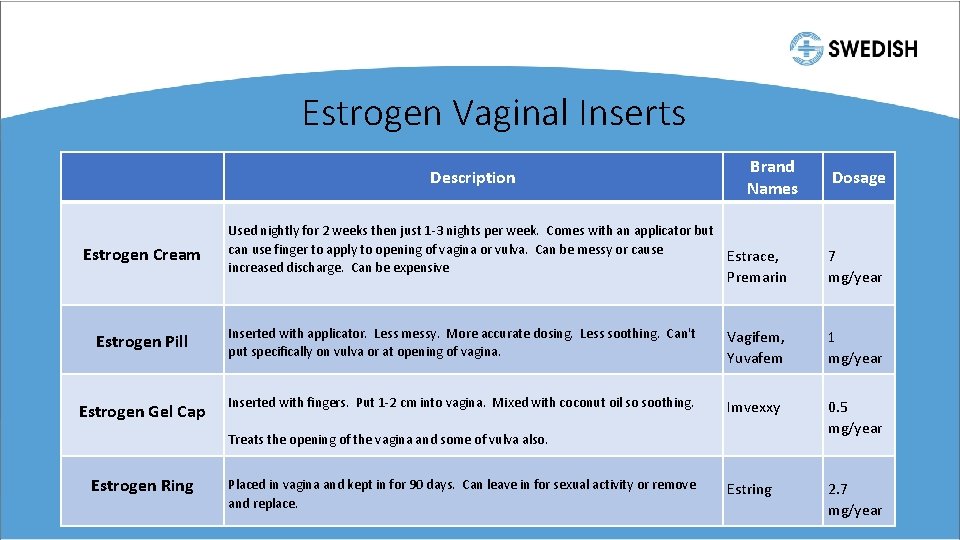
Estrogen Vaginal Inserts Description Brand Names Dosage Used nightly for 2 weeks then just 1 -3 nights per week. Comes with an applicator but can use finger to apply to opening of vagina or vulva. Can be messy or cause increased discharge. Can be expensive Estrace, Premarin 7 mg/year Estrogen Pill Inserted with applicator. Less messy. More accurate dosing. Less soothing. Can't put specifically on vulva or at opening of vagina. Vagifem, Yuvafem 1 mg/year Estrogen Gel Cap Inserted with fingers. Put 1 -2 cm into vagina. Mixed with coconut oil so soothing. Treats the opening of the vagina and some of vulva also. Imvexxy 0. 5 mg/year Placed in vagina and kept in for 90 days. Can leave in for sexual activity or remove and replace. Estring 2. 7 mg/year Estrogen Cream Estrogen Ring
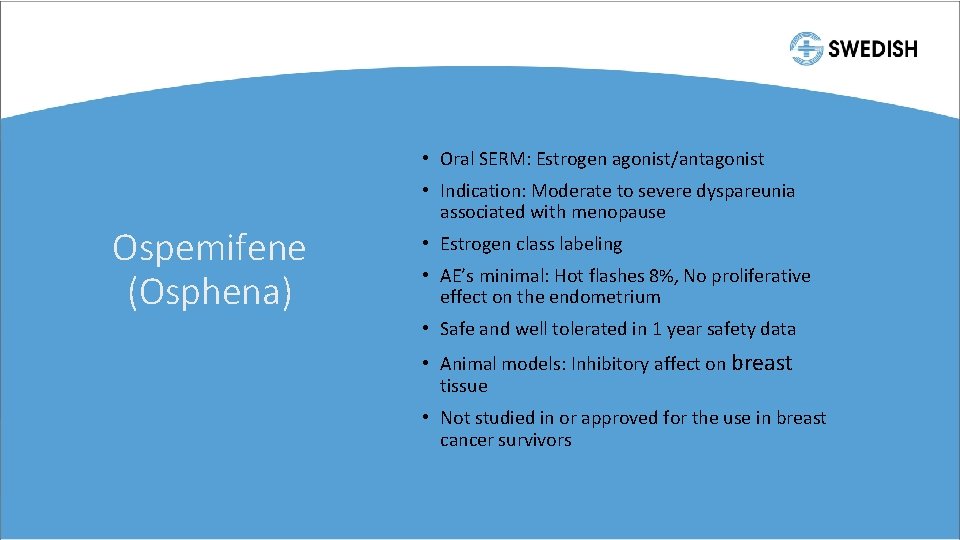
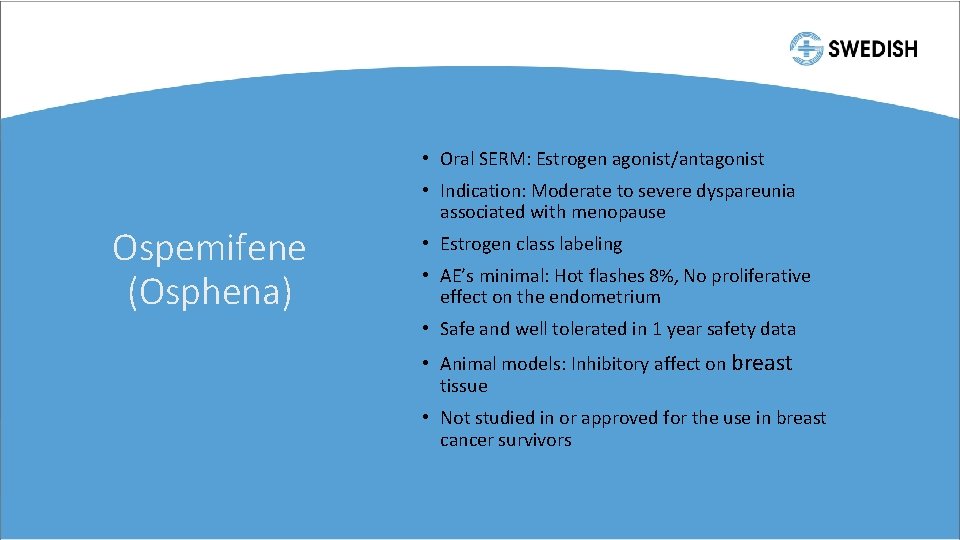
• Oral SERM: Estrogen agonist/antagonist Ospemifene (Osphena) • Indication: Moderate to severe dyspareunia associated with menopause • Estrogen class labeling • AE’s minimal: Hot flashes 8%, No proliferative effect on the endometrium • Safe and well tolerated in 1 year safety data • Animal models: Inhibitory affect on breast tissue • Not studied in or approved for the use in breast cancer survivors
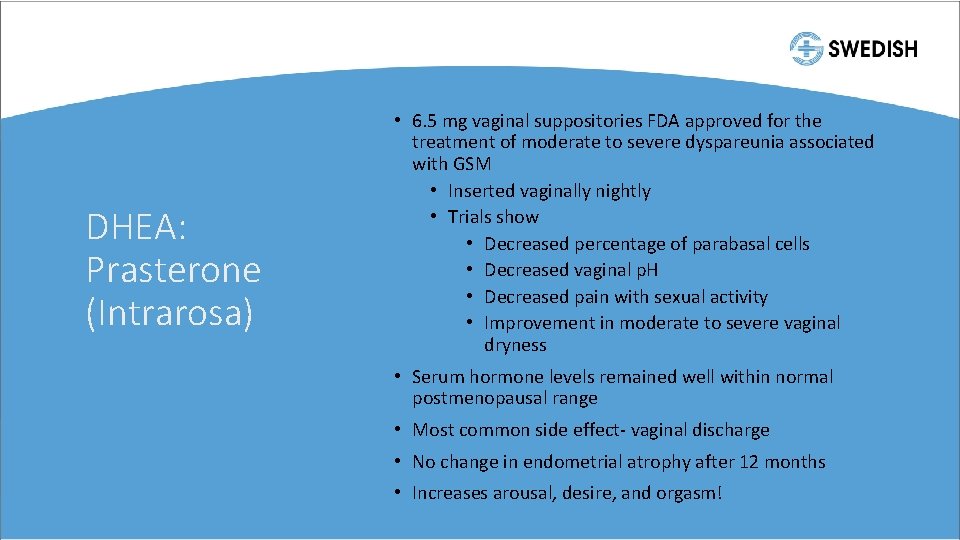
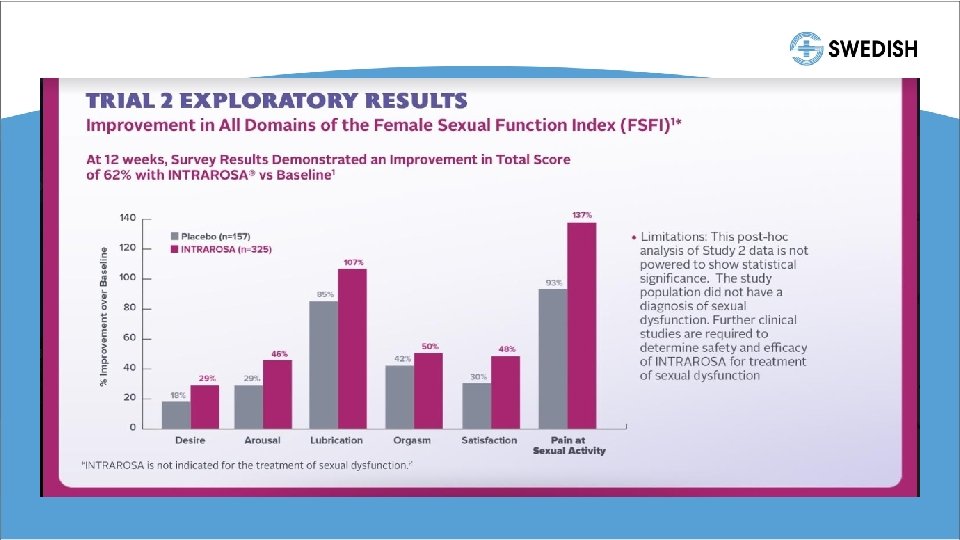
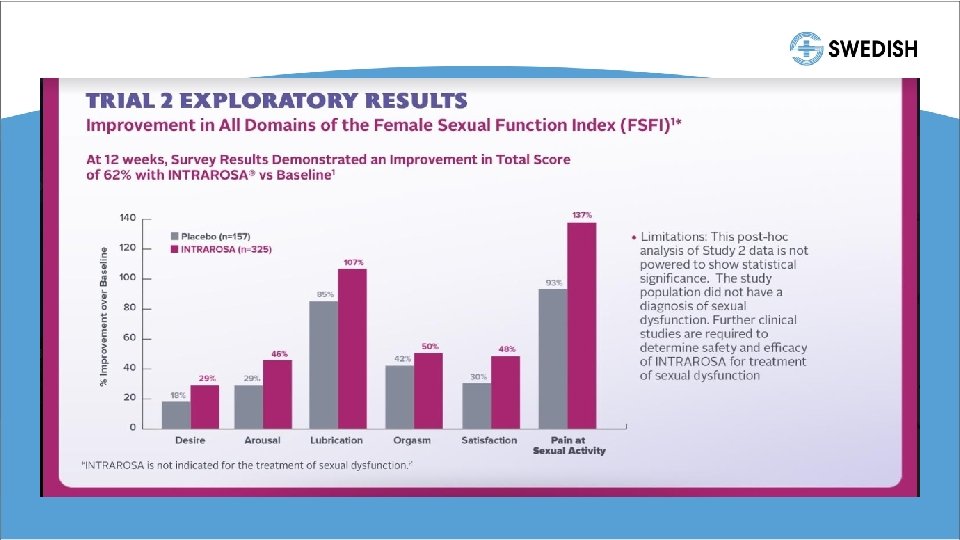
DHEA: Prasterone (Intrarosa) • 6. 5 mg vaginal suppositories FDA approved for the treatment of moderate to severe dyspareunia associated with GSM • Inserted vaginally nightly • Trials show • Decreased percentage of parabasal cells • Decreased vaginal p. H • Decreased pain with sexual activity • Improvement in moderate to severe vaginal dryness • Serum hormone levels remained well within normal postmenopausal range • Most common side effect- vaginal discharge • No change in endometrial atrophy after 12 months • Increases arousal, desire, and orgasm!
Fractional CO 2 Laser • Rapid superficial ablation of low water content epithelial component of atrophic mucosa • Tissue coagulation by laser energy penetrates into deeper tissues to stimulate synthesis of new collagen and ground substance of the matrix • Inflammatory response stimulates fibroblasts to produce new collagen and extracellular matrix • Shown to be effective for dryness and dyspareunia
• 28 y/o G 0 presents with concern of pain with sex. • It hurts with initial penetration but also feels like he’s hitting a wall further inside. • Going on for 6 months • Has tried lubricant that doesn’t help
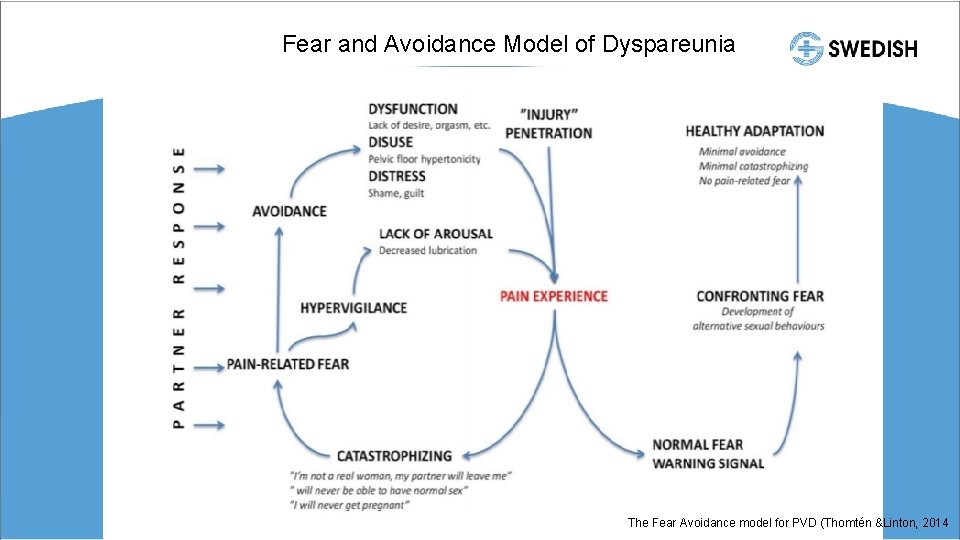
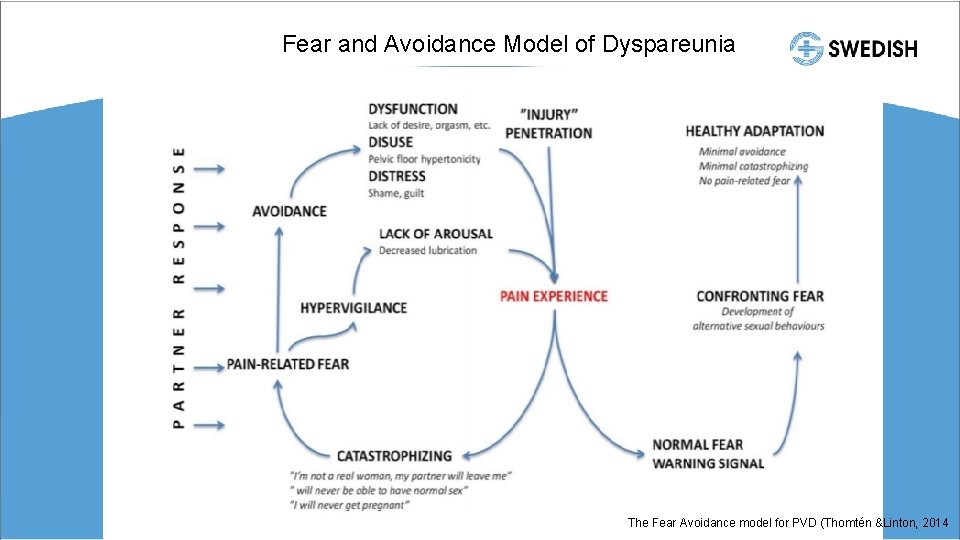
Fear and Avoidance Model of Dyspareunia The Fear Avoidance model for PVD (Thomtén &Linton, 2014
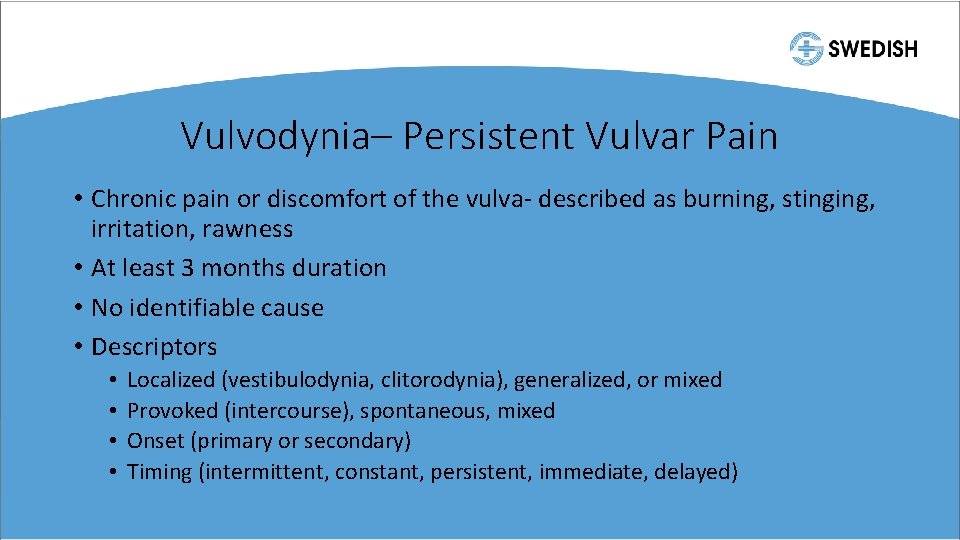
Vulvodynia– Persistent Vulvar Pain • Chronic pain or discomfort of the vulva- described as burning, stinging, irritation, rawness • At least 3 months duration • No identifiable cause • Descriptors • • Localized (vestibulodynia, clitorodynia), generalized, or mixed Provoked (intercourse), spontaneous, mixed Onset (primary or secondary) Timing (intermittent, constant, persistent, immediate, delayed)
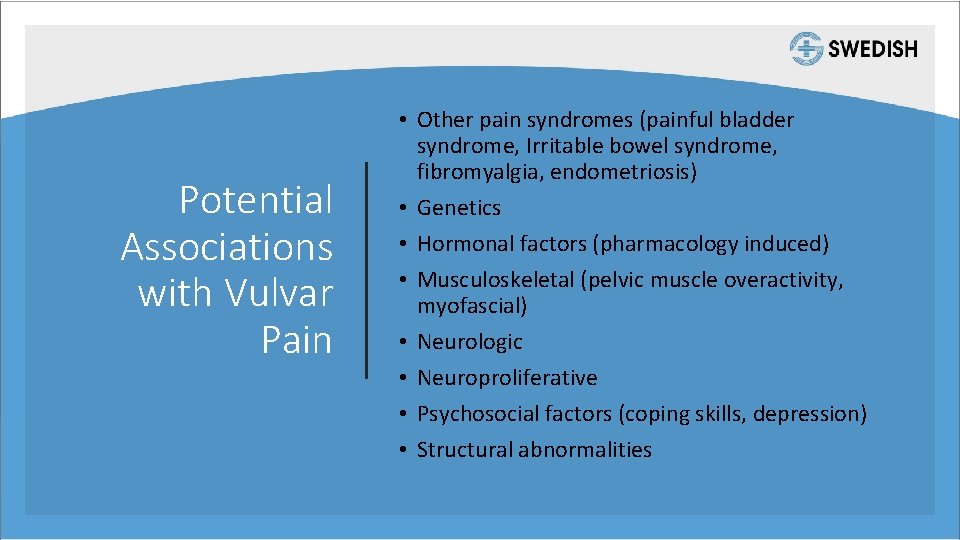
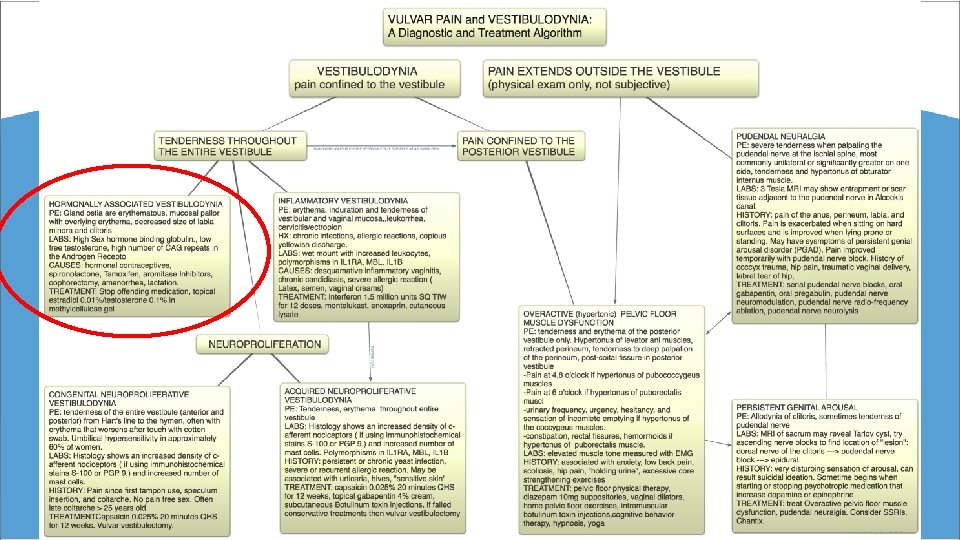
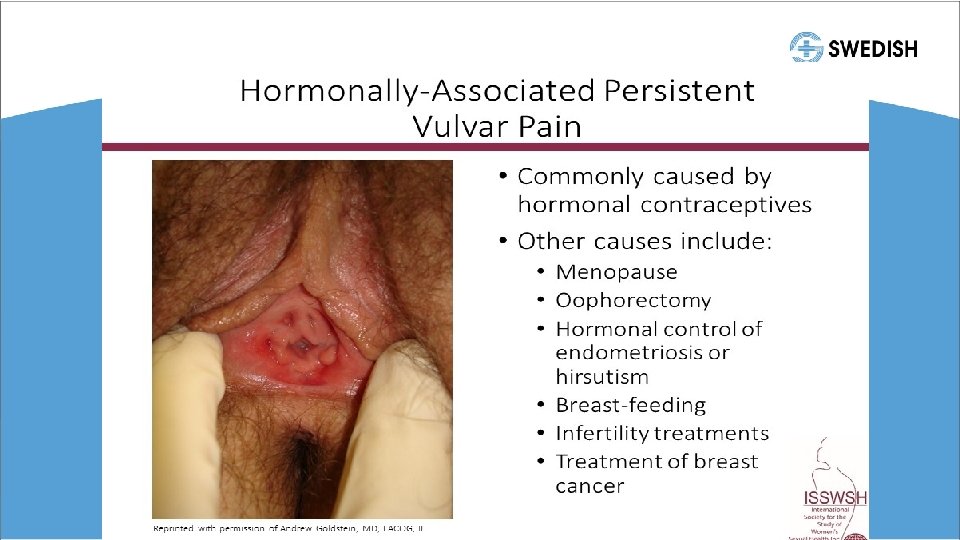
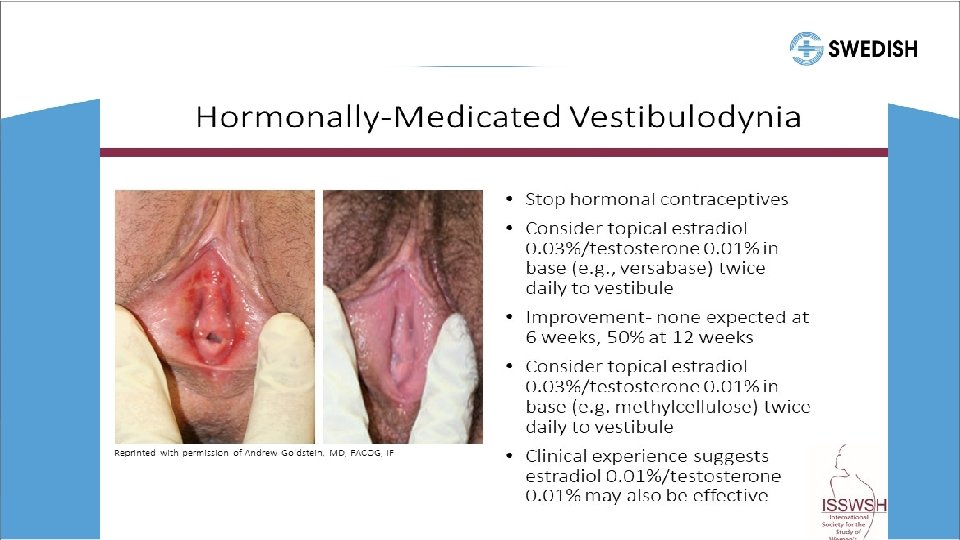
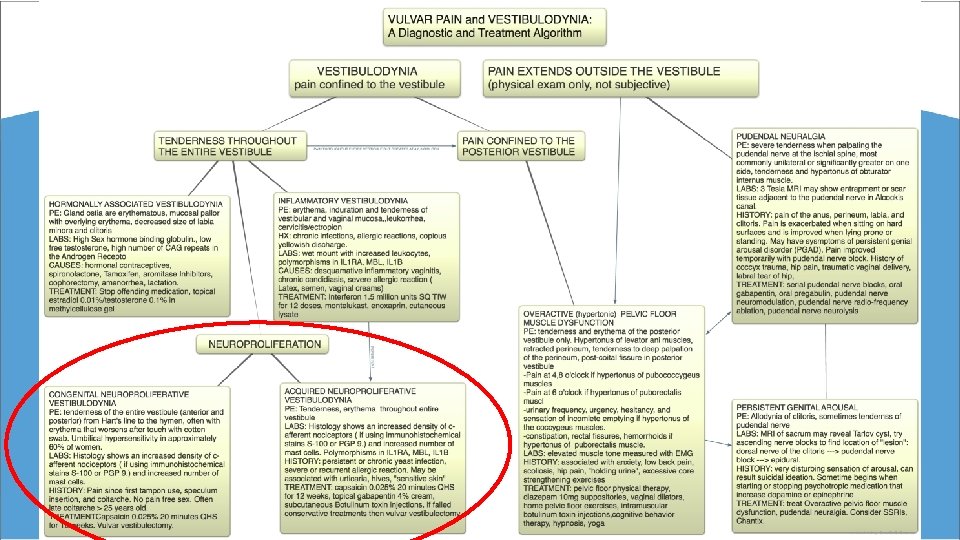
Potential Associations with Vulvar Pain • Other pain syndromes (painful bladder syndrome, Irritable bowel syndrome, fibromyalgia, endometriosis) • Genetics • Hormonal factors (pharmacology induced) • Musculoskeletal (pelvic muscle overactivity, myofascial) • Neurologic • Neuroproliferative • Psychosocial factors (coping skills, depression) • Structural abnormalities
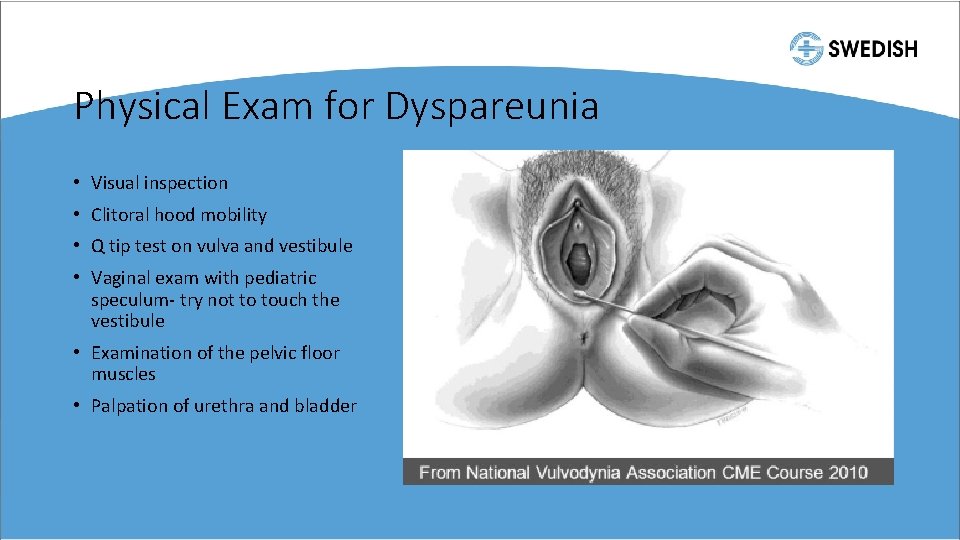
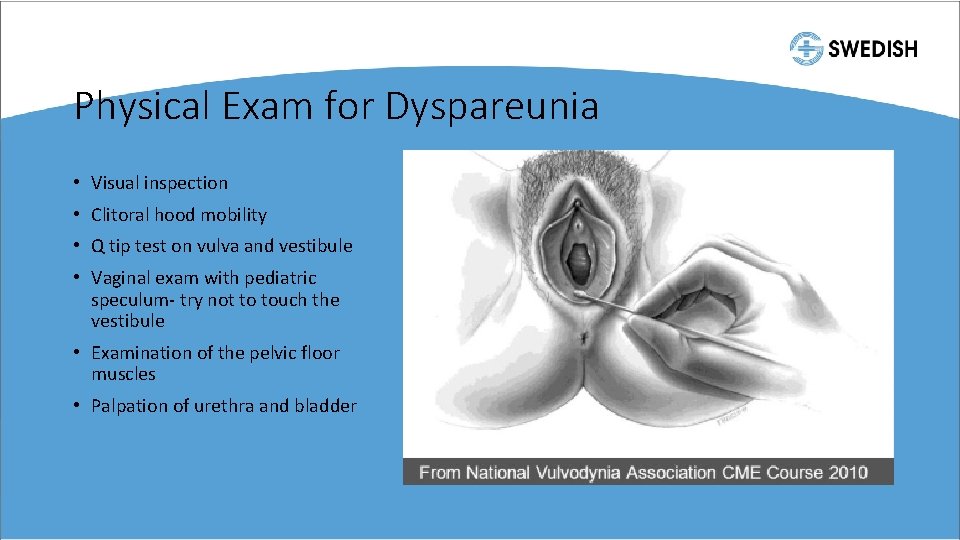
Physical Exam for Dyspareunia • Visual inspection • Clitoral hood mobility • Q tip test on vulva and vestibule • Vaginal exam with pediatric speculum- try not to touch the vestibule • Examination of the pelvic floor muscles • Palpation of urethra and bladder
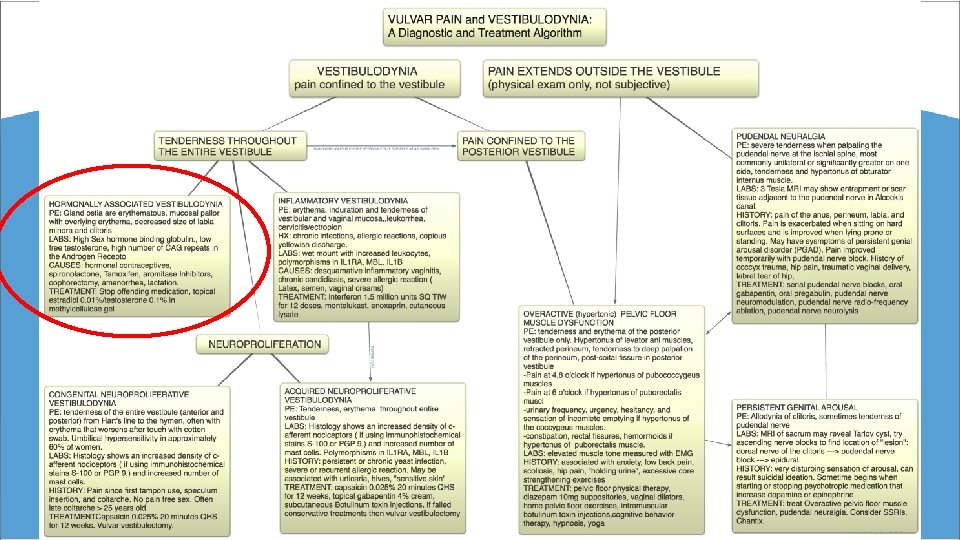
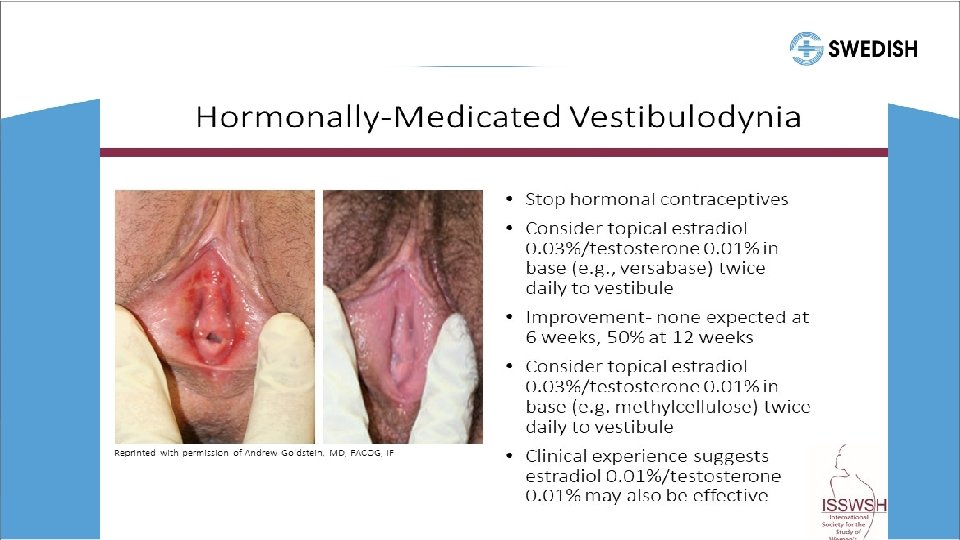
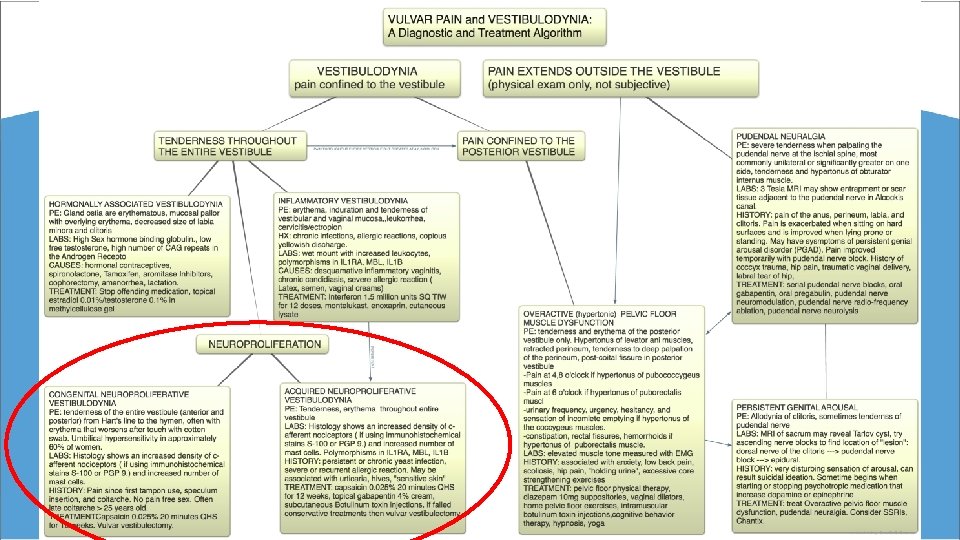
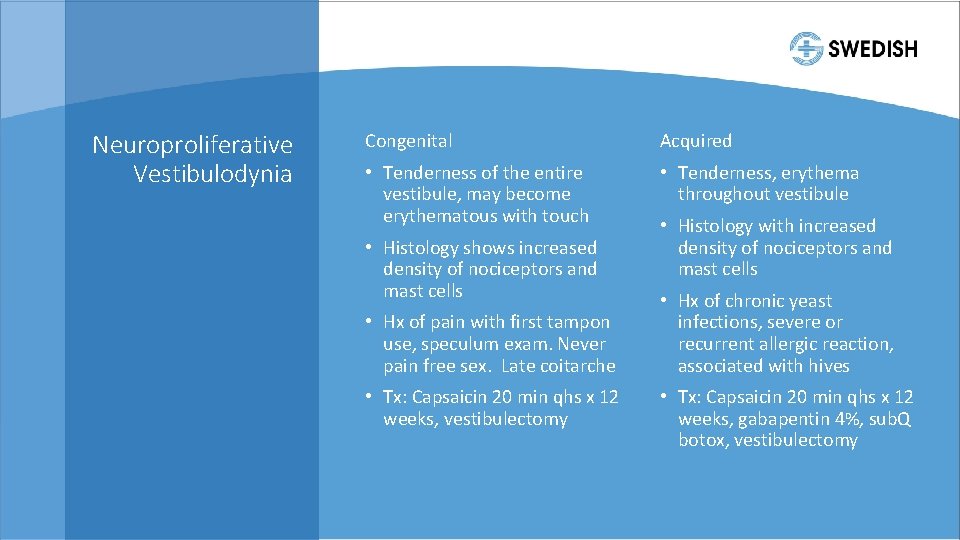
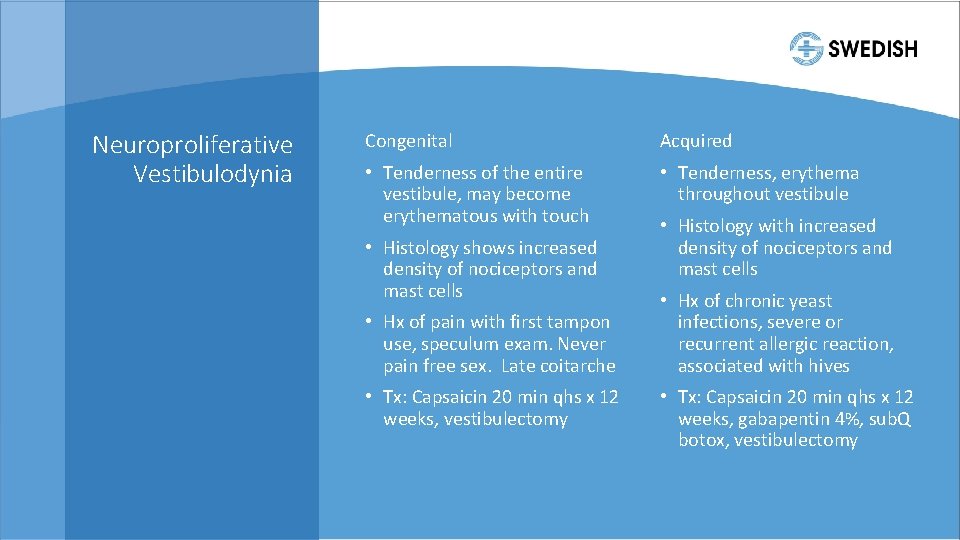
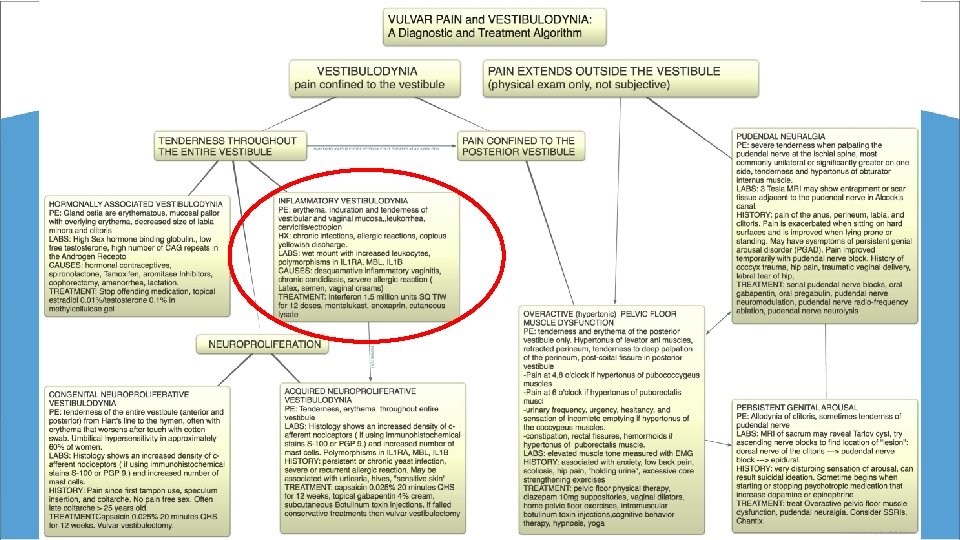
Neuroproliferative Vestibulodynia Congenital Acquired • Tenderness of the entire vestibule, may become erythematous with touch • Tenderness, erythema throughout vestibule • Histology shows increased density of nociceptors and mast cells • Hx of pain with first tampon use, speculum exam. Never pain free sex. Late coitarche • Tx: Capsaicin 20 min qhs x 12 weeks, vestibulectomy • Histology with increased density of nociceptors and mast cells • Hx of chronic yeast infections, severe or recurrent allergic reaction, associated with hives • Tx: Capsaicin 20 min qhs x 12 weeks, gabapentin 4%, sub. Q botox, vestibulectomy
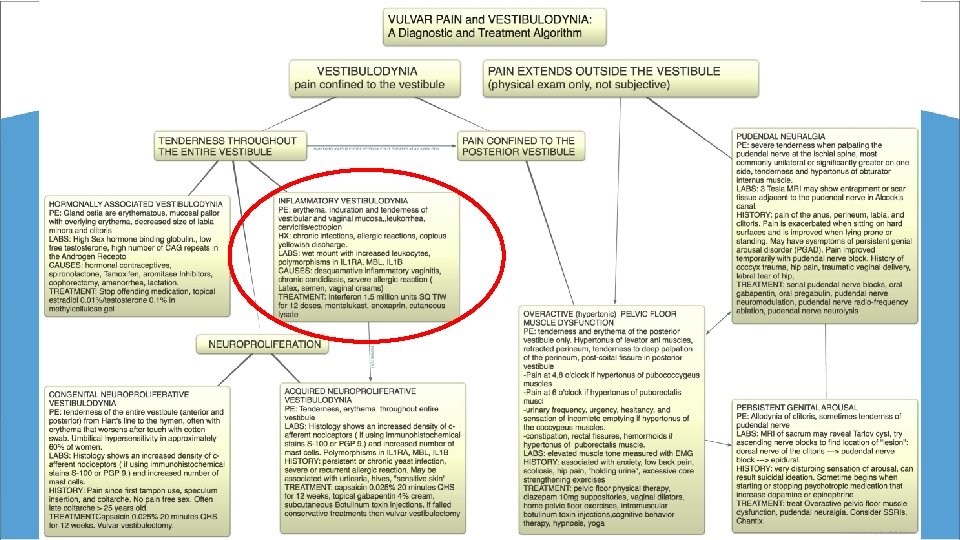
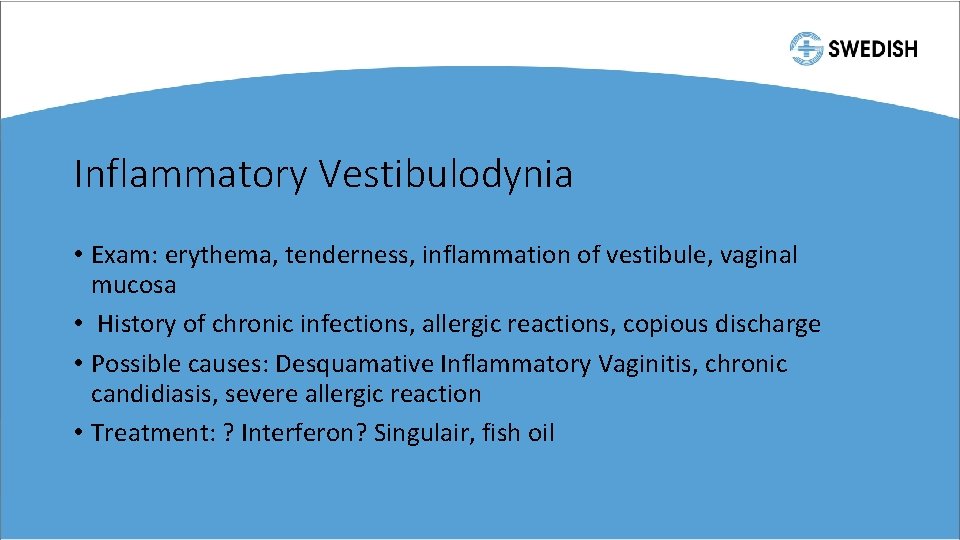
Inflammatory Vestibulodynia • Exam: erythema, tenderness, inflammation of vestibule, vaginal mucosa • History of chronic infections, allergic reactions, copious discharge • Possible causes: Desquamative Inflammatory Vaginitis, chronic candidiasis, severe allergic reaction • Treatment: ? Interferon? Singulair, fish oil
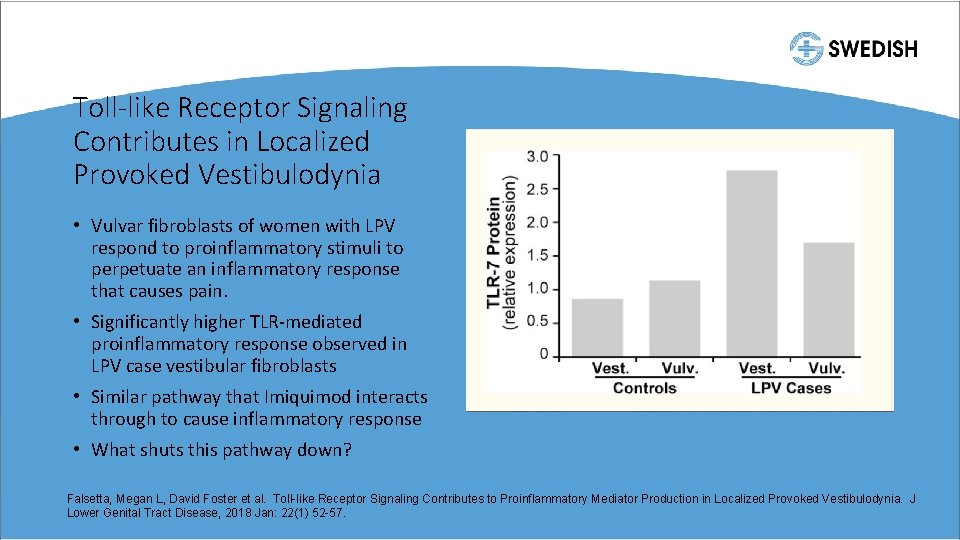
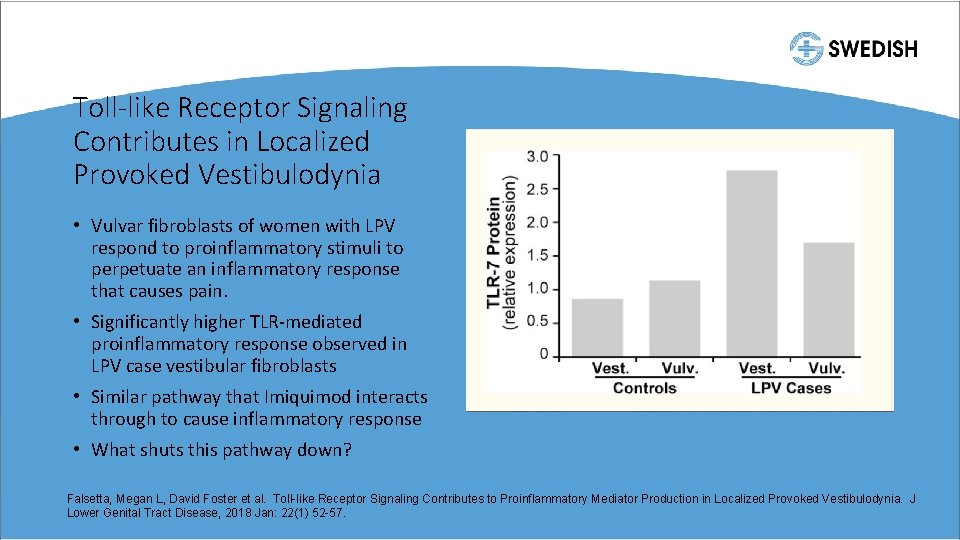
Toll-like Receptor Signaling Contributes in Localized Provoked Vestibulodynia • Vulvar fibroblasts of women with LPV respond to proinflammatory stimuli to perpetuate an inflammatory response that causes pain. • Significantly higher TLR-mediated proinflammatory response observed in LPV case vestibular fibroblasts • Similar pathway that Imiquimod interacts through to cause inflammatory response • What shuts this pathway down? Falsetta, Megan L, David Foster et al. Toll-like Receptor Signaling Contributes to Proinflammatory Mediator Production in Localized Provoked Vestibulodynia. J Lower Genital Tract Disease, 2018 Jan: 22(1) 52 -57.
Overactive Pelvic Floor Muscle Dysfunction • Increased tone leads to decreased blood flow and oxygenation to the muscles, leading to increased lactic acid and soreness • Symptoms • Generalized vulvar pain or burning • Superficial mucosal tenderness where muscles insert- 4, 6, 8 o’clock in the vestibule • Resulting in • Introital dyspareunia • Urinary symptoms- hesitancy, frequency, incomplete emptying • Constipation, hemorrhoids, fissures • Physical exam • Redness or erythema in vestibule where muscles insert • Multiple trigger points or muscle weakness
Vaginismus • A penetration disorder where any form of vaginal penetration with tampons, digits, vaginal dilators, pelvic exams, intercourse is painful or impossible • Persistent or recurrent difficulties of vaginal entry with penis, finger, or other object, despite the desire to do so • Fear and anxiety of pain with penetration • Attempted intercourse feels like “hitting a wall” • Feels like tampons “get stuck” at a certain point and can’t place them
Treatment of Vaginismus • Pelvic floor physical therapy with and without biofeedback • Vaginal dilators • Biofeedback • Sex and relationship counseling • Psychotherapy • Lubricants • Botox

New Ideas for Sexual Health Oh. Nut for Painful Sex Lorals for safe oral sex OMGyes. com
Summary • Sexual health matters and has a large impact on life satisfaction at all ages • Many women have sexual dysfunction but are afraid to bring it up. Ask them about their sex lives. Let them know it’s common to have sexual dysfunction. Let them know they are NORMAL. • If you don’t feel comfortable with these patients, refer them. • There are treatments out there for sexual dysfunction. They aren’t perfect. There are more on the horizon • Sex is good for you!!
Ashley E. Fuller, MD Swedish OB/GYN Specialists First Hill 1101 Madison Street, Suite 700 (206) 215 -6300 ashley. fuller@Swedish. org
References • Althof SE, Leiblum SR, Chevret-Measson M, et al. Psychological and interpersonal dimensions of sexual function and dysfunction. J Sec Med. 2005; 2(6): 793 -800. • Basson R, Berman J, Burnett A, et al. Report on the International Consensus Development Conference on Female Sexual Dysfunction: definitions and classifications. J Urol. 2000; 163: 888 -893. • Labrie F, Archer DF, Koltun W et al. Efficacy of intravaginal dehydroepiandrosterone (DHEA) on moderate to severe dyspareunia and vaginal dryness, symptoms of vulvovaginal atrophy, and of the genitourinary syndrome of menopause. Menopause. 2016; 23(3): 243 -256. • Pfaus JG. Pathways of sexual desire. J Sex Med. 2009; 6: 1506 -1533. • Dennerstein L, Lehert P, Burger H. The relative effects of hormones and relationship factors on sexual function of women through the natural menopausal transition. Fertil Steril. 2005; 84(1): 174 -180. • Dennerstein L, Dudley EC, Hopper JL, et al. A prospective population-based study of menopausal symptoms. Obstet Gynecol. 2000; 96(3): 351 -358. • Labrie F, Diamond P, Cusan L et al. Effect of 12 -month dehydroepiandrosterone replacement therapy on bone, vagina, and endometrium in postmenopausal women. J Clin Endocrinol Metab. 1997; 82(10): 3498 -3505. • Clayton AH et al. The International Society for the Study of Women’s Sexual Health Process of Care for Management of Hypoactive Sexual Desire Disorder in Women. Mayo Clin Proc. 2018; 93(4): 467 -487. • Goldstein, SR, Bachmann GA, Koninckx PR, et al. Ospemifene 12 -month safety and efficacy in postmenopausal women with vulvar and vaginal atrophy. Climacteric. 2014; 17(2): 173 -183. • North American Menopause Society. (2014). Menopause practice: a clinician's guide (5 th ed. ). • Simon J, Portman D, Mabey RG. Long-term safety of ospemifene (52 -week extension) in the treatment of vulvar and vaginal atrophy in hysterectomized postmenopausal women. Maturitas. 2014; 77(3): 274 -281. • Berga SL. Profile of ospemifene in the breast. Reprod Sci. 2013; 20(10): 1130 -1136. • Wierman ME, Arlt W, Basson R, et al. Androgen therapy in women: a reappraisal: an endocrine society clinical practice guideline. J Endocrinol Metab. 2014; 99(10): 3489 -3510. • Lindau ST, Schumm LP, Laumann EO, et al. A study of sexuality and health among older adults in the United States. N Engl J Med. 2007; 357(8): 762 -774. • Adapted from Kingsberg SA et al. CNS Drugs. 2015; 1(1): 1 -19.

References • J Sex Marital Ther. 2000 Jul-Sep; 26(3): 231 -40. Effect of bupropion-SR on orgasmic dysfunction in nondepressed subjects: a pilot study. Modell JG 1, May RS, Katholi CR. • NAMS Practice Pearl, Testosterone for Midlife Women: the Hormone of Desire? June 24, 2015. Shifren, Jan. • The Women’s Libido Pill is Back and So is the Controversy. Bloomberg Newsweek, June 2018 • ISSWSH Slide Deck • Falsetta, Megan L, David Foster et al. Toll-like Receptor Signaling Contributes to Proinflammatory Mediator Production in Localized Provoked Vestibulodynia. J Lower Genital Tract Disease, 2018 Jan: 22(1) 52 -57. • Dooley, Erin, Melanie K Miller, Anita H Clayton. Flibanserin: From Bench to Bedside. Sexual Medicine Review 2017; 5: 461 -469 • AMAG slides Bremelanotide • Harlow BL. Allergic reactions and risk of vulvodynia. Ann Epidemiol. 2009; 19(11): 771 -777. • Goldstein AT, Burrows L. Vulvodynia (CME). J Sex Med. 2008; 5(1): 5 -15. • Bornstein J, Goldstein AT, Stockdale CK, et al. 2015 ISSVD, ISSWSH and IPPS consensus terminology and classification of persistent vulvar pain and vulvodynia. Obstet Gynecol. 2016; 127(4): 745 -751.