Womb for Improvement A Critical Review of Thin
Womb for Improvement: A Critical Review of Thin or Damaged Uterine Lining Jeanette Tomasino, MS, RNC, MNN Senior Director Nurse Education
Disclosure § Presenter is Senior Director of Nurse Education at Progyny which is a for-profit vendor of IVF and egg banking cycles. § Presenter will not be discussing or referring to unlabeled/unapproved uses of drugs, devices, products, protocols or therapeutic strategies.
Learning Objectives Describe the causative factors of intrauterine adhesions Specify impact of Asherman’s syndrome on fertility Summarize the management and treatment of Asherman’s syndrome
Background § The first case of intrauterine adhesion was published in 1894 by Heinrich Fritsch § 54 years later, a full description was given by gynecologist Joseph Asherman § Joseph Asherman identified pathology in 29 women who showed amenorrhea with stenosis of the internal cervical ostium § He speculated manifestation could be a consequence of endometrial trauma
Definition of Intrauterine Adhesions (IUA) § Partial adherence of endometrial surfaces with fibrotic tissue § Symptoms are related to degree and location
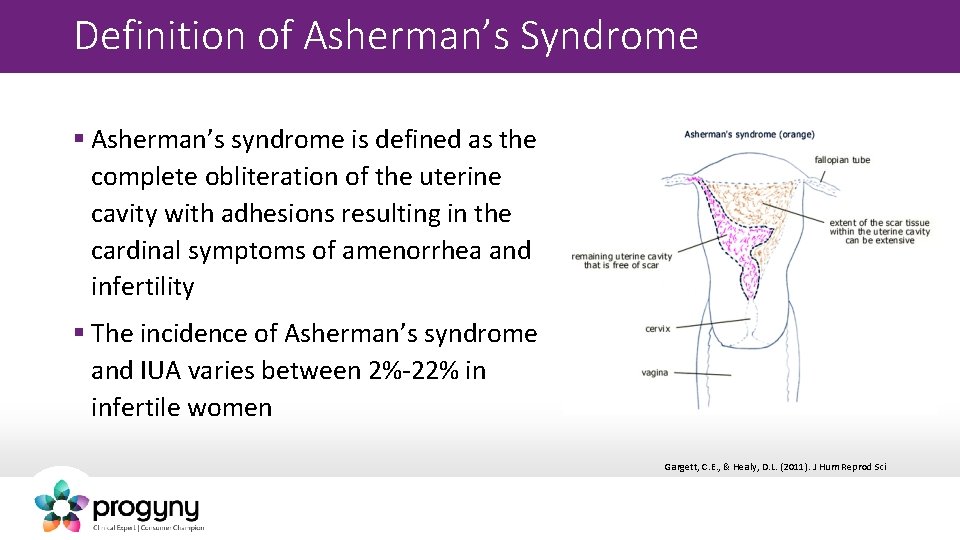
Definition of Asherman’s Syndrome § Asherman’s syndrome is defined as the complete obliteration of the uterine cavity with adhesions resulting in the cardinal symptoms of amenorrhea and infertility § The incidence of Asherman’s syndrome and IUA varies between 2%-22% in infertile women Gargett, C. E. , & Healy, D. L. (2011). J Hum Reprod Sci
Geographic Variations in Asherman’s Result from differences in several factors: § Incidence of both illegal and legal abortions § Techniques for puerperal and post-abortion evacuation § Criteria for diagnosis of IUA § Awareness of clinicians § Incidence of puerperal infection and genital tuberculosis Hanstede, M. F et al. (2015) Fert & Stert, 104(6)
A Constellation of Clinical Signs and Symptoms Pain Menstrual Dysfunction (hypomenorrhea, amenorrhea) Infertility Recurrent Pregnancy Loss
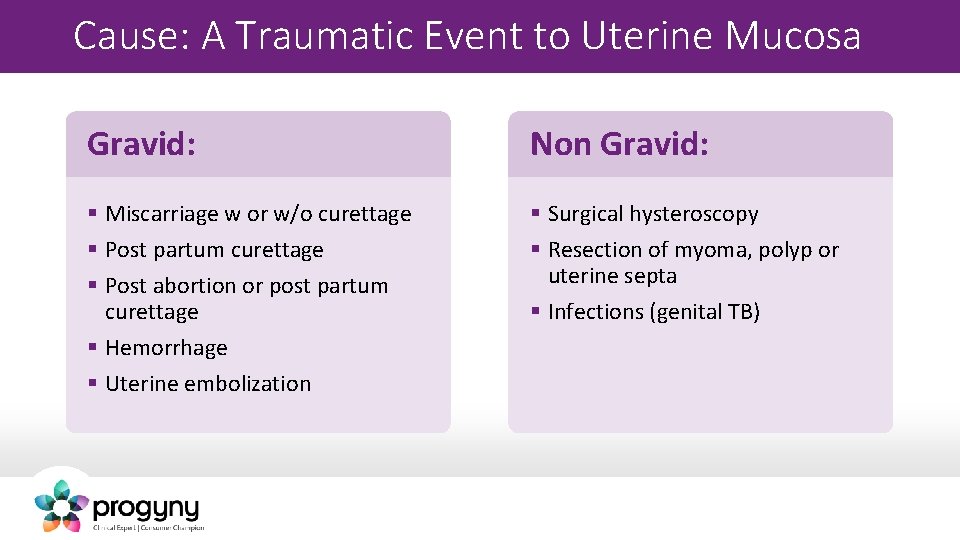
Cause: A Traumatic Event to Uterine Mucosa Gravid: Non Gravid: § Miscarriage w or w/o curettage § Post partum curettage § Post abortion or post partum curettage § Hemorrhage § Uterine embolization § Surgical hysteroscopy § Resection of myoma, polyp or uterine septa § Infections (genital TB)

Endometrial Curettage: Retained POC § In this situation, the myometrium is softened by the pregnancy and often accompanied by a low grade infectious process § The traumatizing effect of a sharp curettage contributes to the likelihood that a full depth endometrium will be removed Lo, S. T. , et al. (2008) Human Reproduction Vol 23, No. 306 -309
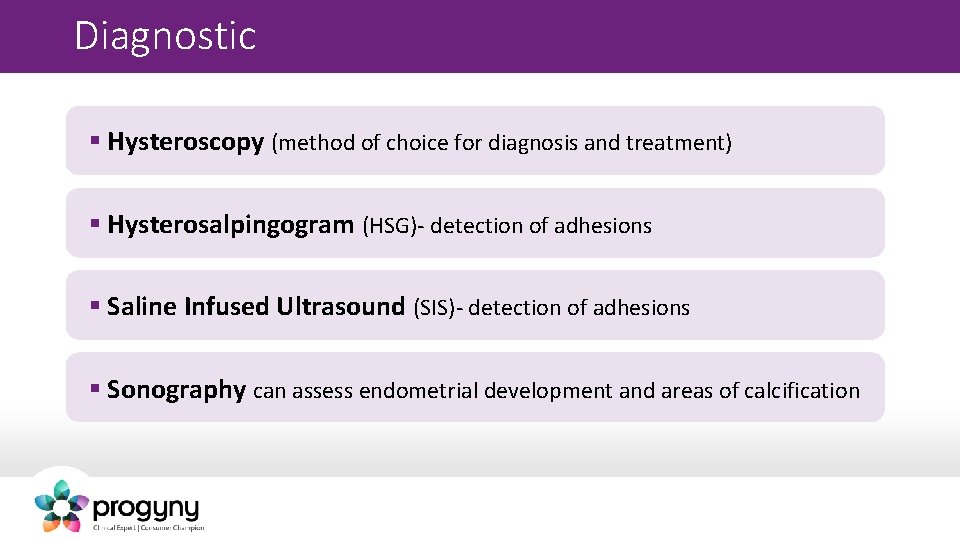
Diagnostic § Hysteroscopy (method of choice for diagnosis and treatment) § Hysterosalpingogram (HSG)- detection of adhesions § Saline Infused Ultrasound (SIS)- detection of adhesions § Sonography can assess endometrial development and areas of calcification
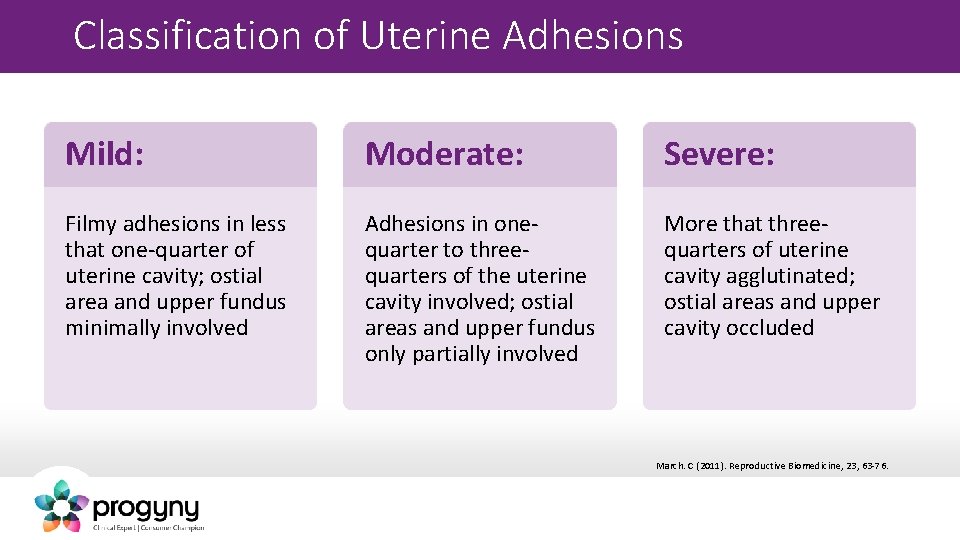
Classification of Uterine Adhesions Mild: Moderate: Severe: Filmy adhesions in less that one-quarter of uterine cavity; ostial area and upper fundus minimally involved Adhesions in onequarter to threequarters of the uterine cavity involved; ostial areas and upper fundus only partially involved More that threequarters of uterine cavity agglutinated; ostial areas and upper cavity occluded March. C (2011). Reproductive Biomedicine, 23, 63 -76.
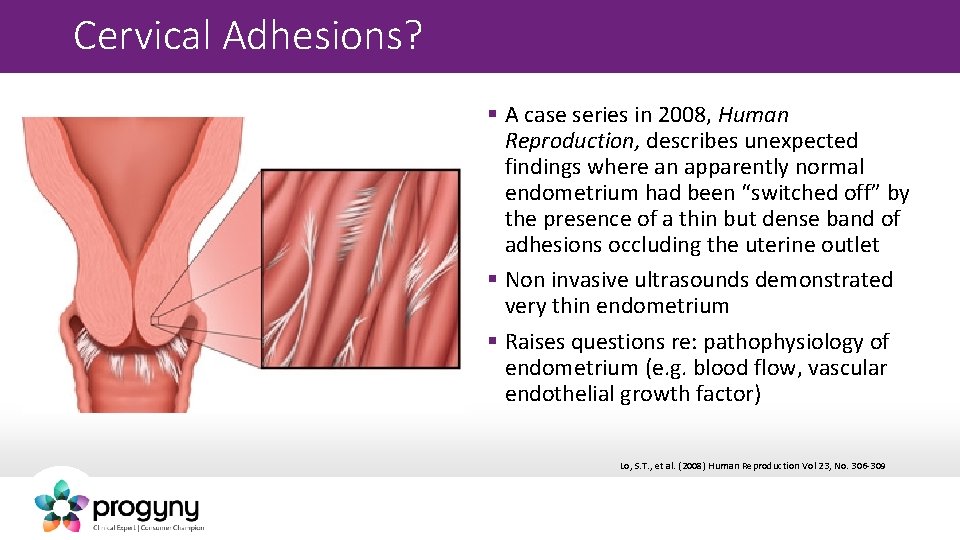
Cervical Adhesions? § A case series in 2008, Human Reproduction, describes unexpected findings where an apparently normal endometrium had been “switched off” by the presence of a thin but dense band of adhesions occluding the uterine outlet § Non invasive ultrasounds demonstrated very thin endometrium § Raises questions re: pathophysiology of endometrium (e. g. blood flow, vascular endothelial growth factor) Lo, S. T. , et al. (2008) Human Reproduction Vol 23, No. 306 -309
Primary Goal in Treatment § Restore normal volume and shape to the uterine cavity
Secondary Goals in Treatment § Associated with symptoms (pain, infertility, abnormal menses) § Prevention of the recurrence of adhesions
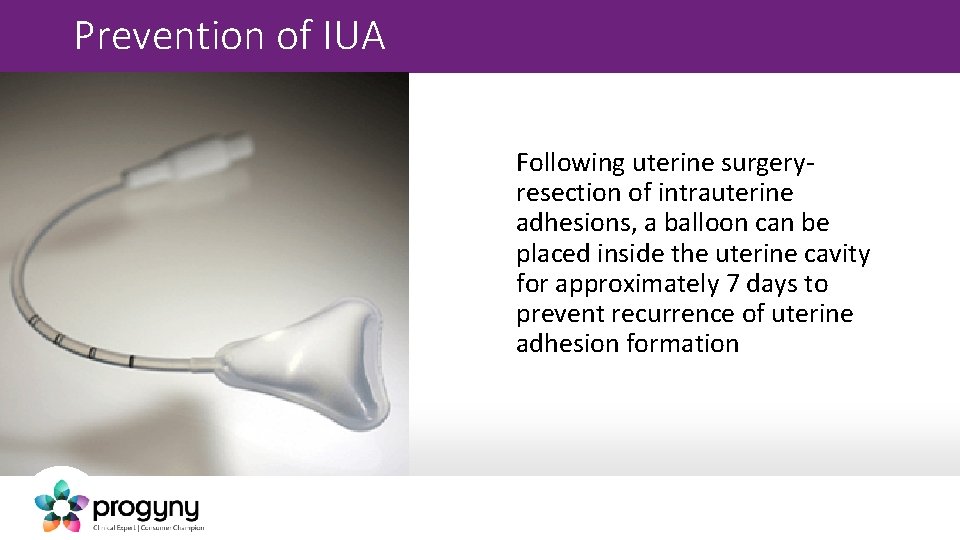
Prevention of IUA Following uterine surgeryresection of intrauterine adhesions, a balloon can be placed inside the uterine cavity for approximately 7 days to prevent recurrence of uterine adhesion formation
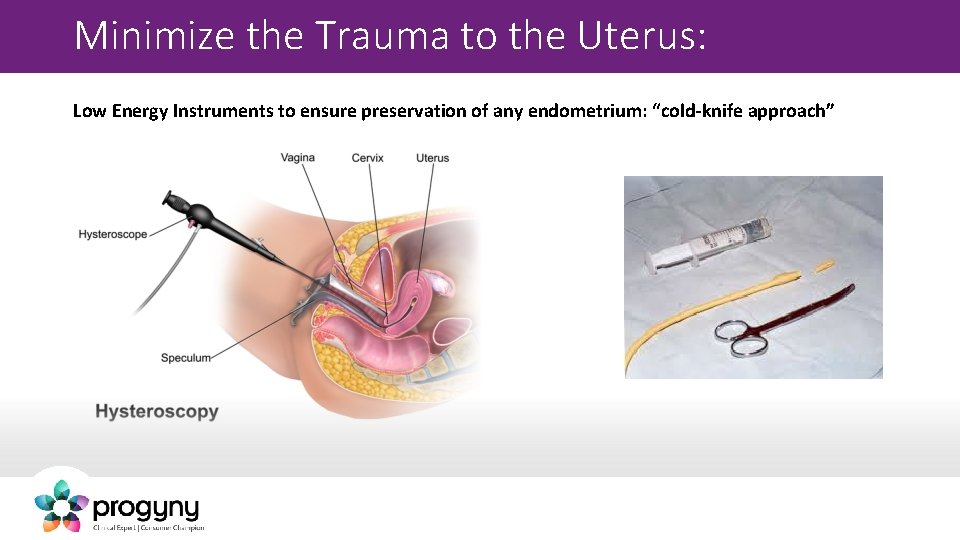
Minimize the Trauma to the Uterus: Low Energy Instruments to ensure preservation of any endometrium: “cold-knife approach”
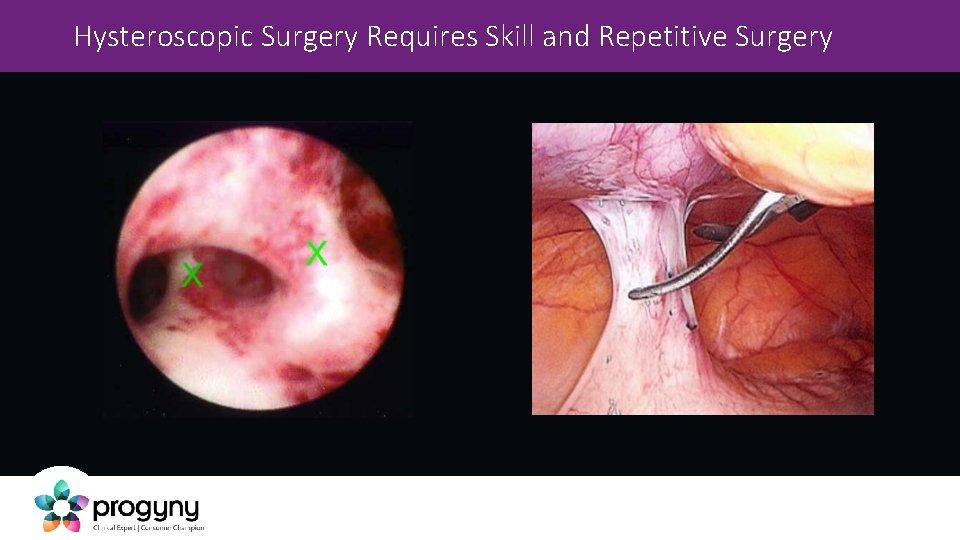
Hysteroscopic Surgery Requires Skill and Repetitive Surgery
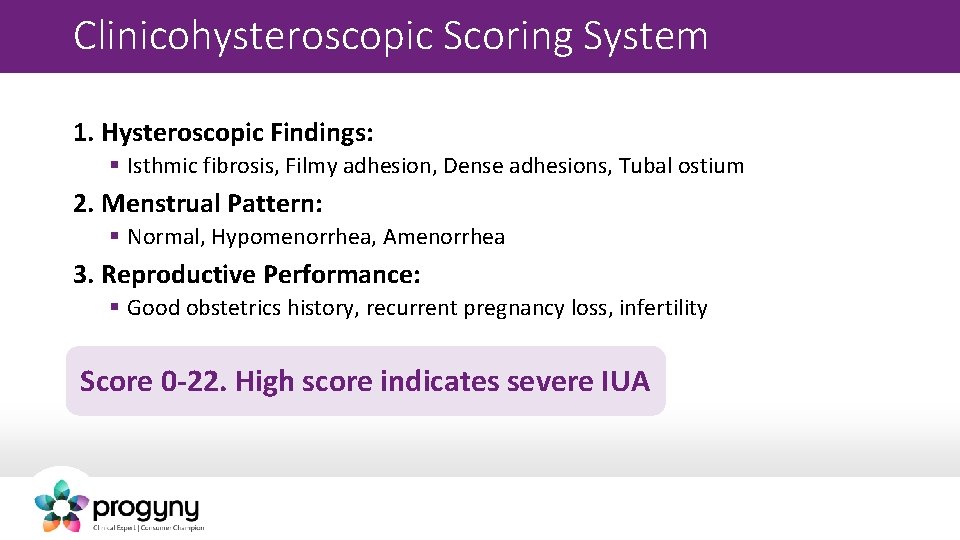
Clinicohysteroscopic Scoring System 1. Hysteroscopic Findings: § Isthmic fibrosis, Filmy adhesion, Dense adhesions, Tubal ostium 2. Menstrual Pattern: § Normal, Hypomenorrhea, Amenorrhea 3. Reproductive Performance: § Good obstetrics history, recurrent pregnancy loss, infertility Score 0 -22. High score indicates severe IUA
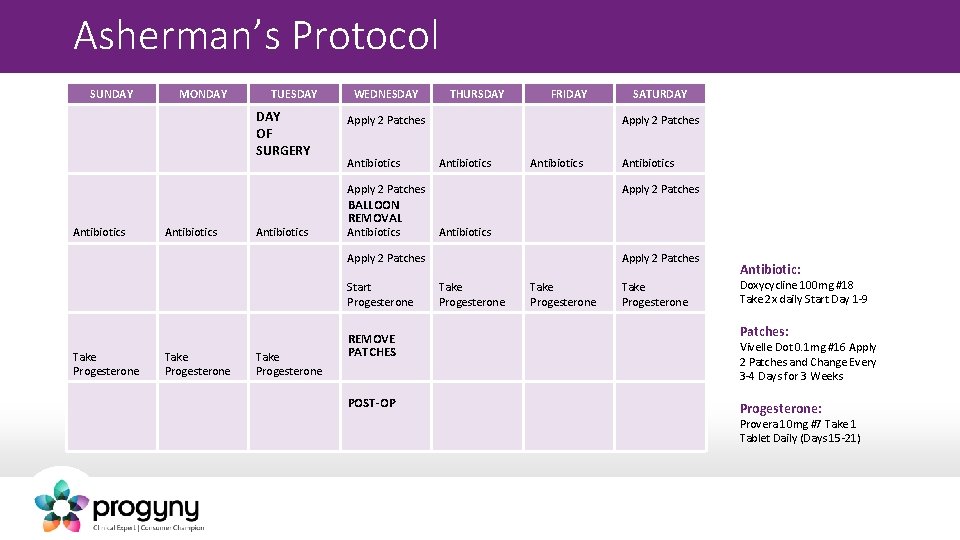
Asherman’s Protocol SUNDAY MONDAY TUESDAY OF SURGERY WEDNESDAY THURSDAY FRIDAY Apply 2 Patches Antibiotics Antibiotics BALLOON REMOVAL Antibiotics Take Progesterone REMOVE PATCHES POST-OP Antibiotics Apply 2 Patches Start Progesterone SATURDAY Apply 2 Patches Take Progesterone Antibiotic: Doxycycline 100 mg #18 Take 2 x daily Start Day 1 -9 Patches: Vivelle Dot 0. 1 mg #16 Apply 2 Patches and Change Every 3 -4 Days for 3 Weeks Progesterone: Provera 10 mg #7 Take 1 Tablet Daily (Days 15 -21)
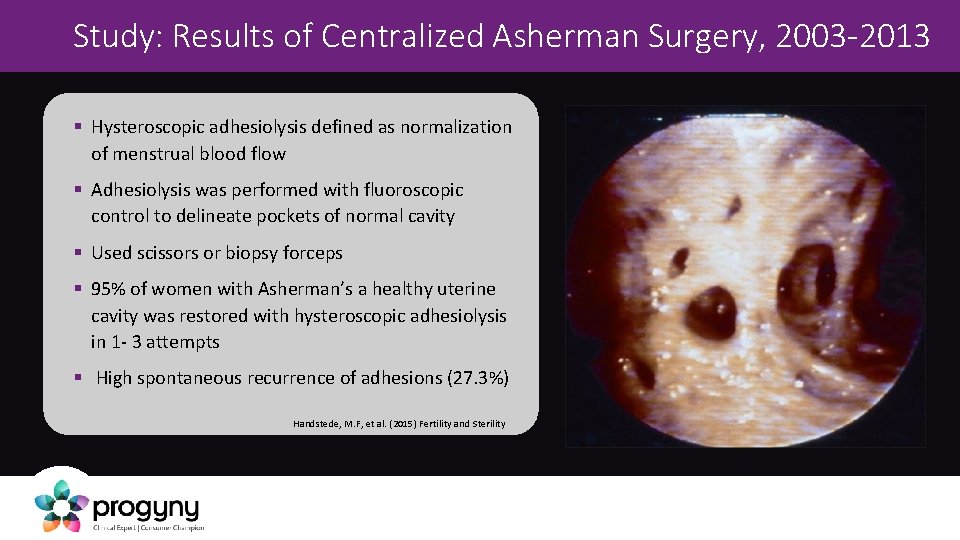
Study: Results of Centralized Asherman Surgery, 2003 -2013 § Hysteroscopic adhesiolysis defined as normalization of menstrual blood flow § Adhesiolysis was performed with fluoroscopic control to delineate pockets of normal cavity § Used scissors or biopsy forceps § 95% of women with Asherman’s a healthy uterine cavity was restored with hysteroscopic adhesiolysis in 1 - 3 attempts § High spontaneous recurrence of adhesions (27. 3%) Handstede, M. F, et al. (2015) Fertility and Sterility
Treatment: Comprehensive Management Study by Meyers & Bradley (2012) Comprehensive Management of Severe Asherman: 12 women § Combination of preoperative, intraoperative and postoperative measures § The use of estrogen before surgery promotes endometrial growth and allows surgery to be performed in proliferative phase § Hysteroscopic repair (mechanical adhesiolysis) under ultrasound guidance to improve visualization § Mechanical separation of uterine cavity- post operative triangle balloon catheterremoved after 1 week § Copper IUD immediately placed after balloon removal § Oral E 2 4 -6 mg daily continued until removal of IUD 4 -10 weeks Results: all women resumed menses. 6 of 9 <39 yrs achieved pregnancy (67%) Meyers, E. M. & Hurst, B. S. (2012) Fertility and Sterility
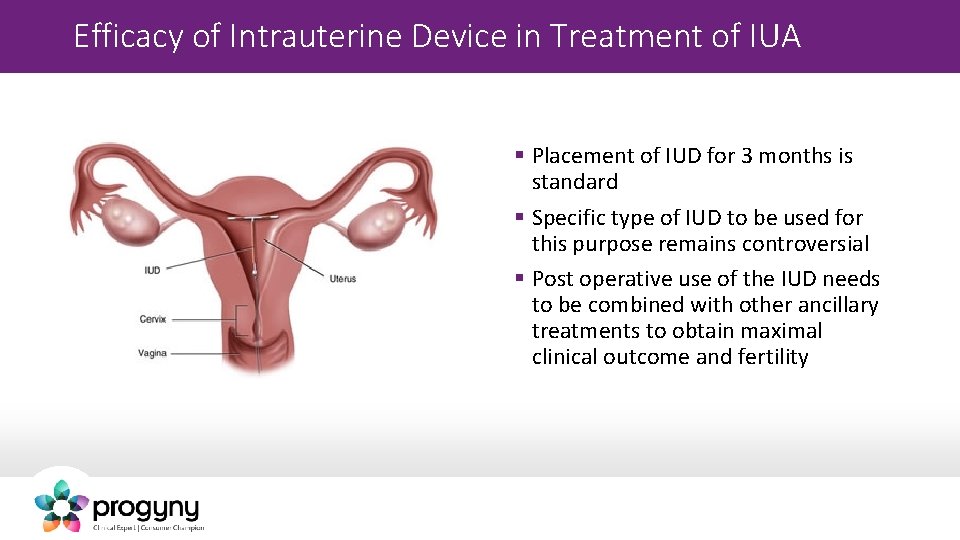
Efficacy of Intrauterine Device in Treatment of IUA § Placement of IUD for 3 months is standard § Specific type of IUD to be used for this purpose remains controversial § Post operative use of the IUD needs to be combined with other ancillary treatments to obtain maximal clinical outcome and fertility
IUD Types § Types of recommended IUDs: Y shaped, Lippes loop, and uterine shaped § T shaped and those impregnated with progestin are not recommended (suppress endometrial proliferation) § Uterine shaped IUD consists of stainless steel coiled wire with copper inside release antiinflammatory agent- widely used in China with good result Salma, U. , Xue, M, et al. (2014) Bio. Med Research International
Hyaluronic Acid and other Anti-adhesion Barriers § Hyaluronic acid is a widespread component in human tissue § Involved in biologic functions such as mechanical support, cell migration and proliferation § Used to prevent intrauterine adhesions- (only temporary barrier) § Hyaluronic based products removed from market due to its toxicity in 2003 § Use chemically modified hyaluronic barriers (sodium hyaluronate, alginate carboxymethylcellulose hyaluronic acid)
Viagara (Slidenfil) for Improving Endometrial Thickness: Review of the Literature: Slidenafil use for improving endometrial thickness remains controversial: § Zinger, M. , Thomas, M. & Liu. (2001) University of Cincinnati- Vaginal sildenafil improves endometrium in Asherman’s syndrome. Fertility and Sterility, 76(3), S 255. (2 patients University of Cincinnati) § Black, S. , Bergman, S. , et al. (2002) Viagara did not normalize controlled endometrial development in poor prognosis patients. Fertility and Sterility, 78, 3(1), S 236. (10 patients: Genetics and IVF Institute Fairfax, Va. ) § Grunfeld, L. , Sandler, B. et al. , (2005). Vaginal Viagara is not effective on improving endometrial adequacy. Fertility and Sterility, 84, S 240. (23 patients RMA of New York) § Eid, M. (2015). Sildenafil improves implantation rate in women with thin endometrium secondary to improvement of uterine blood flow: pilot study. Fertility and Sterility, 104(3), e 342. (22 patients Cairo University United Arab Emirates)
Pregnancy outcome after treatment Correlation between the extent of adhesions and pregnancy outcome after surgical treatment § Valle and Sciarra Mild- 81. 3% Moderate- 66. 0% Severe- 31. 9% Endometrial Sclerosis: little or no functioning endometrium Valle & Sciarra (1988) Am J Obstet Gynecol
Post Operative Assessment § Evaluation of uterine cavity after adhesiolysis is an important step in management § Complete resolution of IUA is not always possible with a single procedure § 50% recurrence rate of IUA in severe cases § 21. 6% recurrence rate of IUA in moderate cases § Timely recognition of any recurrence is essential to provide the best prognosis § May be necessary to repeat surgery Valle & Sciarra (1988) Am J Obstet Gynecol
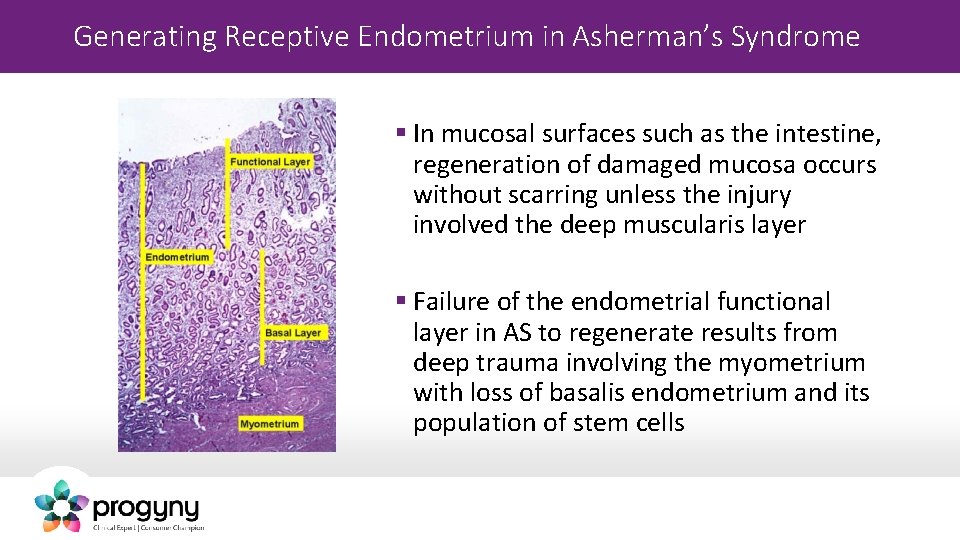
Generating Receptive Endometrium in Asherman’s Syndrome § In mucosal surfaces such as the intestine, regeneration of damaged mucosa occurs without scarring unless the injury involved the deep muscularis layer § Failure of the endometrial functional layer in AS to regenerate results from deep trauma involving the myometrium with loss of basalis endometrium and its population of stem cells
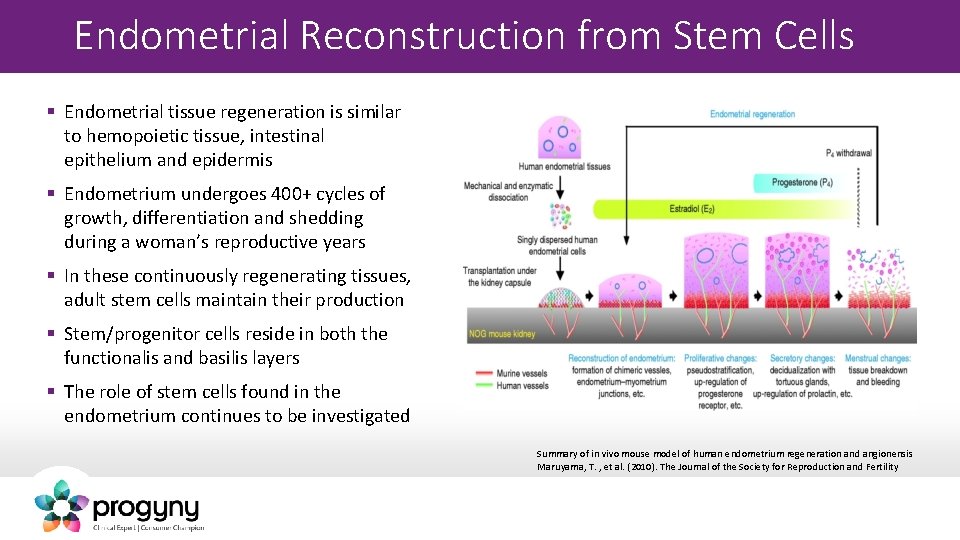
Endometrial Reconstruction from Stem Cells § Endometrial tissue regeneration is similar to hemopoietic tissue, intestinal epithelium and epidermis § Endometrium undergoes 400+ cycles of growth, differentiation and shedding during a woman’s reproductive years § In these continuously regenerating tissues, adult stem cells maintain their production § Stem/progenitor cells reside in both the functionalis and basilis layers § The role of stem cells found in the endometrium continues to be investigated Summary of in vivo mouse model of human endometrium regeneration and angionensis Maruyama, T. , et al. (2010). The Journal of the Society for Reproduction and Fertility
Case Report: § Endometrial regeneration using autologous adult stem cells followed by conception by in vitro fertilization in a patient with severe Asherman’s § Innovative treatment of a 33 year old woman with AS using autologous bone marrow § Derived stem cell populations regenerated the endometrium sufficiently to enable implantation of a donor oocyte IVF embryo § Case report highlights the potential role of invoking tissue damage to promote endometrial regeneration Gargett, C. E. & Healy, D. L. (2011). J Hum Repro Sci, 4(1), 49 -52.
Clinical Trial: § Human CD 133+ bone marrow derived stem cells to promote endometrial proliferation in a murine model of Asherman syndrome (Cervello, et al. (2015) Fertility and Sterility § Animal model aims to illustrate the engraftment, localization, and mechanisms to induce endometrial proliferation § Clinical application of this strategy as an autologous cell therapy for AS in humans Cerevell, I. , et al. , (2015) Fertility and Sterility, 104 (6), 1552 -1560.
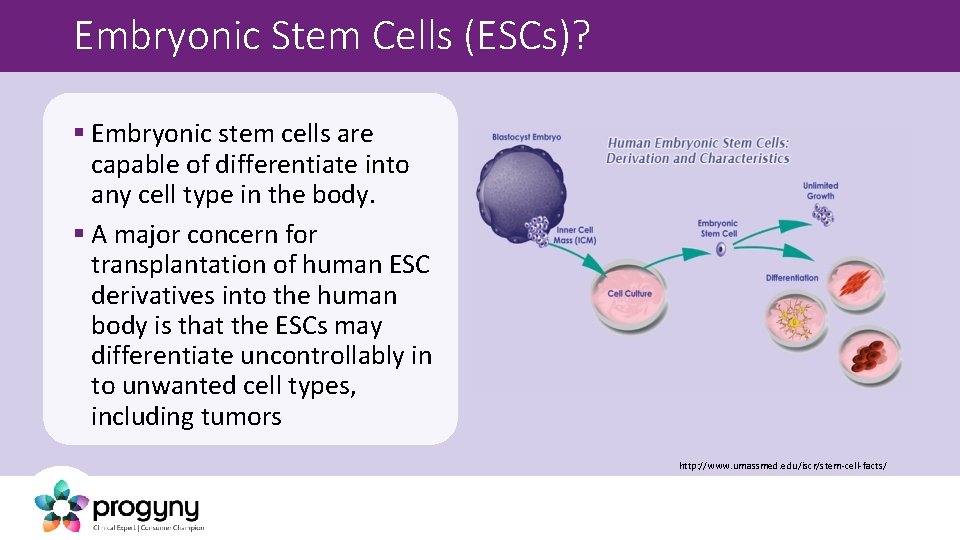
Embryonic Stem Cells (ESCs)? § Embryonic stem cells are capable of differentiate into any cell type in the body. § A major concern for transplantation of human ESC derivatives into the human body is that the ESCs may differentiate uncontrollably in to unwanted cell types, including tumors http: //www. umassmed. edu/iscr/stem-cell-facts/
Conclusion § A comprehensive approach provides the best possible outcome in poor-prognosis women with severe Asherman’s § Early diagnosis § Meticulous surgery § Modalities to reduce scar formation § IUD, uterine stent, adhesion barriers and hormonal treatment have proven efficient, yet more comparative trials are needed § Adult stem cells can reconstruct endometrial tissue in vivo suggesting their possible use in treating disorders with inadequate endometrium
Thank You!
- Slides: 35