Withdrawing and withholding treatment at the end of





- Slides: 39
Withdrawing and withholding treatment at the end of life The ethics and practice of treatment withdrawal
Some guiding principles • • Beneficence (doing good) Non-maleficence (avoiding harm) Autonomy (respecting the person) Justice (ensuring fairness to all)
Is it ethical to take away treatments that are sustaining life? Yes, provided that it is • Consistent with patient’s wishes as expressed or documented and • In the patient’s best interest Beneficence Non-maleficence Autonomy Justice
Is withdrawing different from withholding treatment? • Ethically no • If treatment not beneficial, ethical to stop it • If treatment not beneficial, ethical to not start it Beneficence Non-maleficence Autonomy Justice
Are we asking the wrong question? • Instead of “can it be in the best interest of the person that treatment is withdrawn? ” • Ask “can it be in the best interest of the patient that life should be prolonged by this treatment? ” Beneficence Non-maleficence Autonomy Justice
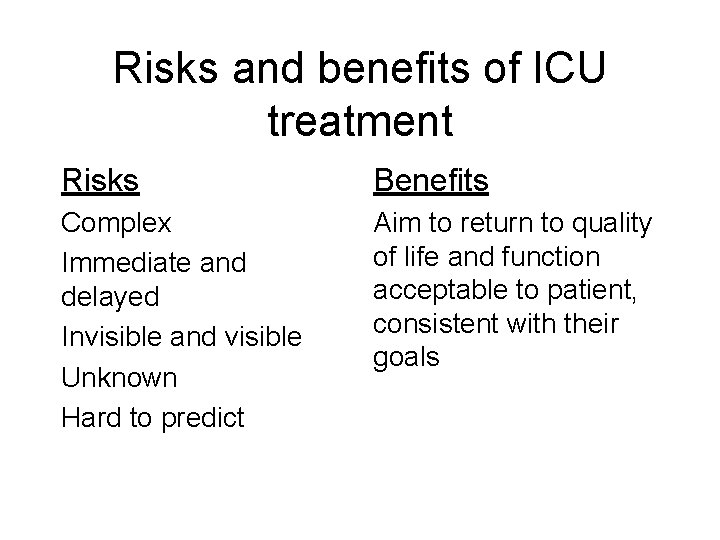
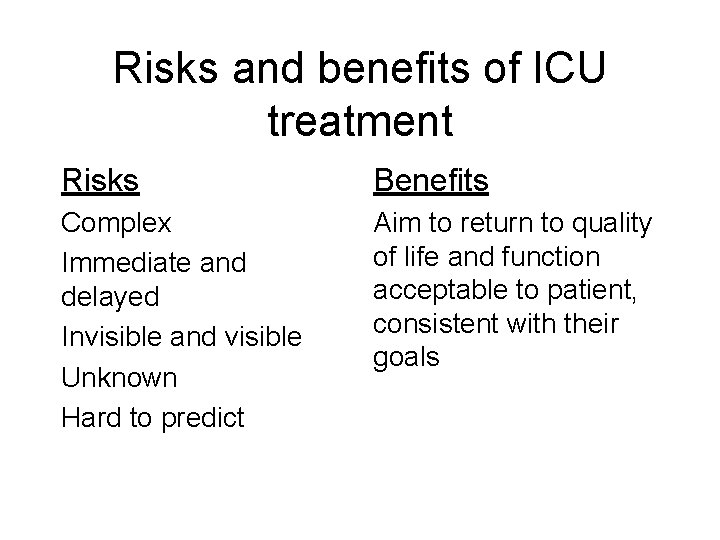
Risks and benefits of ICU treatment Risks Benefits Complex Immediate and delayed Invisible and visible Unknown Hard to predict Aim to return to quality of life and function acceptable to patient, consistent with their goals
Reasons for admission to ICU • • • Reversible illness Uncertain reversibility (trial of therapy) Difficult symptom management Family issues Consideration for donation

Responsibility of the intensivist Communication Accountability Reassessment of progress Determination of patient wishes Goal setting Maintaining physiological stability Maintaining team integrity Building relationship with family Realistic chance of good Is this a potential donor?
Sources of conflict • Duty to current patients • Duty to provide care to those who could benefit from it • Duty to use limited resource wisely to avoid compromising healthcare elsewhere in the system • Decisions must be reasonable & accountable Beneficence Non-maleficence Autonomy Justice
An aside on cognitive dissonance Balance between confidence in decision making/diagnosis/treatment and humility to accept might be wrong Only time will tell: trial of therapy
Withdrawal or withholding requires • • Reflection on and within practice Goal setting Knowledge of what is possible Knowledge of patient wishes Reassessment of patient and response Consensus Communication and relationship Courage and accountability
Effects • Takes a toll on staff: decision-makers, contributors, observers • Not quick process (though effects may be) • Not an easy option • Effect on family can be immediate/delayed
Language • • Clear Honest Respectful Takes into account understanding and emotions
Language • Incredibly important • Want: family then focus on treatments rather than goals • Futile or worth • Doing everything where the alternative is doing nothing
An aside on futility • Subjective • Cannot easily be argued with by family • Negative connotation about the person rather than condition/treatment • Ambiguous
Language • What would he say if he were in the room with us? • Switch focus from trying to cure, to trying to make him comfortable • We need to allow death to happen: our treatments are getting in the way • It’s becoming more obvious that we are doing isn’t helping him: the treatments are not working • He is showing us that he isn’t getting better • We will continue doing the things that keep him comfortable and stop doing the things that are not helping or are causing him discomfort
• • Do you want us to do everything? There is nothing more we can do This is futile Value judgments: it’s not worth carrying on in his case because of who he is • We want your permission to turn off the machines

This is looking futile ✖

✖ We need to stop treatment: ICU is a valuable resource and someone else needs the bed more

✖ It’s not worth carrying on

✔ It’s time to stop doing those treatments that aren’t helping any more and focus on those that are keeping Bob comfortable
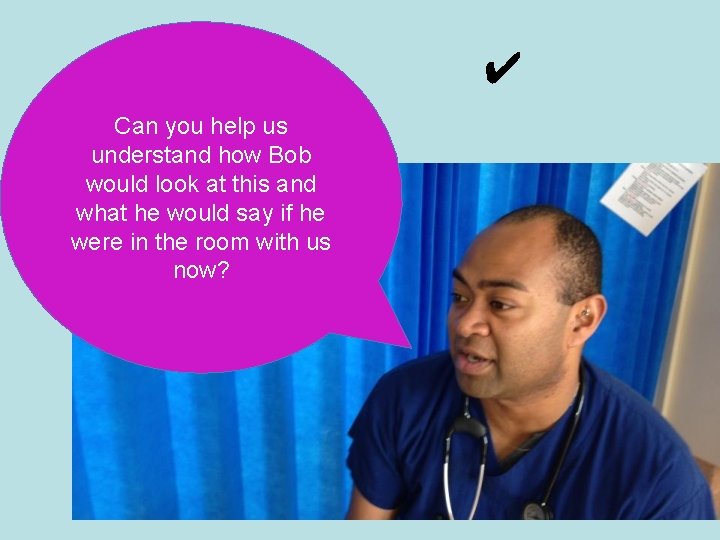
✔ Can you help us understand how Bob would look at this and what he would say if he were in the room with us now?
Non-critical care experience • Renal: withdrawal of dialysis • Respiratory: withdrawal of O 2 or NIV • Incorporating existing AD or Goals of Treatment/Care document
What is Advance Care Planning? • Process by which healthcare preferences can be planned and recorded in case • Includes choosing substitute decision maker who can speak for patient in that event
How do we withdraw? • Planned • Comfort a priority • Location in ICU/hospital/home or other
Other considerations • Cultural differences • Children (patients or family members)
Pitfalls of withdrawing • Might make things worse: create a person who survives in condition inconsistent with their wishes • Or disability might be inconsistent with predictions, e. g. post-intended DCD
Essentials • • Consensus that it is the right thing to do Understanding of what it means Clarity around method Clearly understood by patient and/or family • Communication Beneficence Non-maleficence Autonomy Justice
Consensus and shared decision-making • Decision making is shared between those involved • Consensus: everyone supports the decision that has been made, although it might not be what they would prefer Beneficence Non-maleficence Autonomy Justice
Sources of conflict
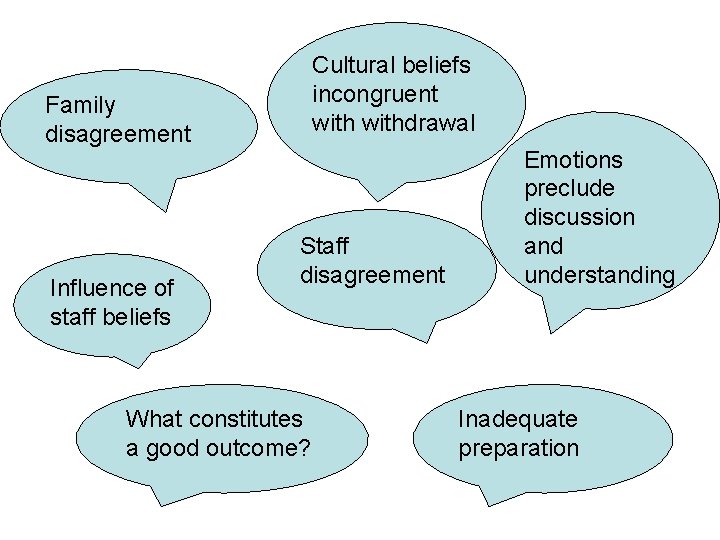
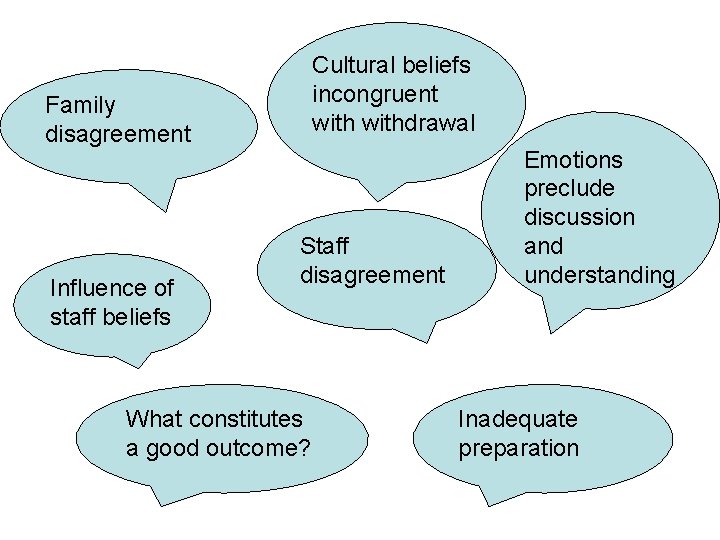
Cultural beliefs incongruent withdrawal Family disagreement Influence of staff beliefs Staff disagreement What constitutes a good outcome? Emotions preclude discussion and understanding Inadequate preparation
Support and advice • • Cultural support Clinical colleagues Second opinion Legal advice (organisation)
Do we really do what we say we do? Psirides & Sturland Crit Care Resus 2009 Staff response to anonymous WD scenario Retrospective audit 40 patients who had WD
• Difference between belief and practice (IV fluid, ECG, pulse oximetry) • Documentation incomplete • Inconsistencies around communication of clear rationale • Reflects challenges of ICU EOLC: symptom assessment in non-verbal, belief that IV fluid beneficial
Conclusion (mine) • Increasing the dialogue around EOLC in ICU is essential: role for Palliative Care • Contributions from all members of the team involved in the process • Communication: could do better
Developments • Introduction of a guiding tool for EOL improved cessation of treatments and monitoring, documentation • Impact on patient and family experience unknown
Are we doing the right thing? • Patient and family perspective: bereavement data • Consistent with professional guidelines and code of ethics • Reflection on practice Beneficence Non-maleficence Autonomy Justice
It’s complicated “EOL decisions are difficult, unsettling and sometimes distressing. Professionals have different views and sometimes reach different conclusions. This is not necessarily a sign we are on the wrong track, and should not be taken to preclude withholding or withdrawing treatment if that is consistent with the patients wishes” Wilkinson et al Bioethics 2016 Beneficence Non-maleficence Autonomy Justice
Questions?