Why when How to add Prandial insulin after

- Slides: 38
Why, when & How to add Prandial insulin after Basal Optimization FOCUS OF PROFILE GLULISINE
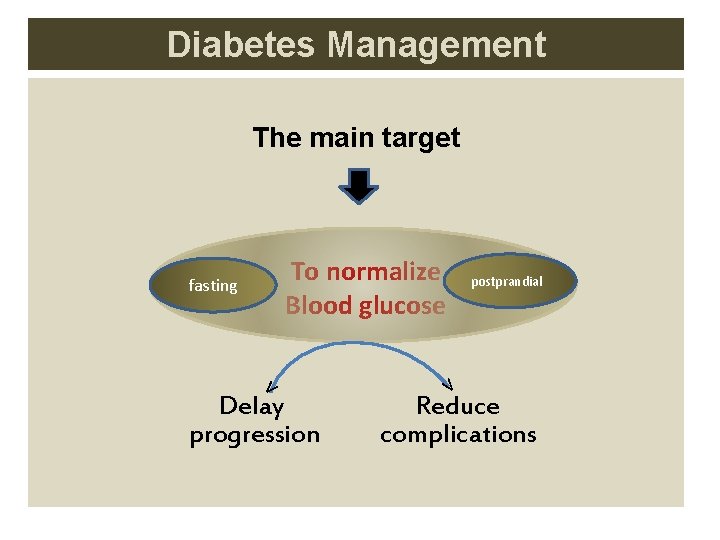
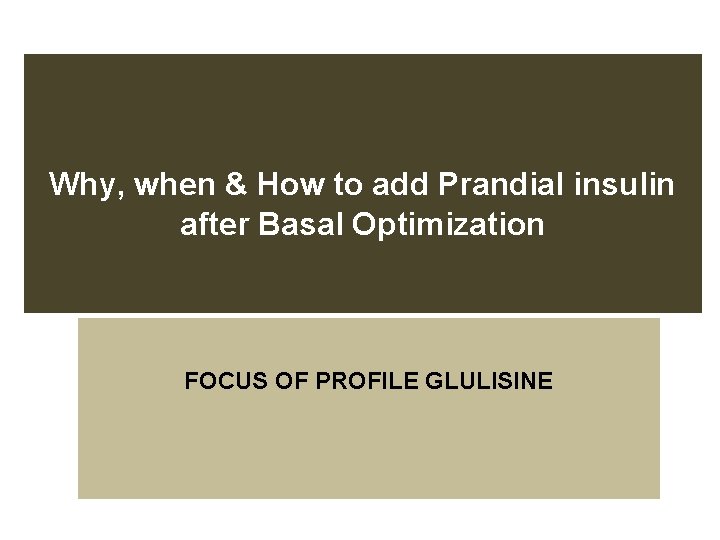
Diabetes Management The main target To normalize Blood glucose fasting ᵛ Delay progression postprandial ᵛ Reduce complications
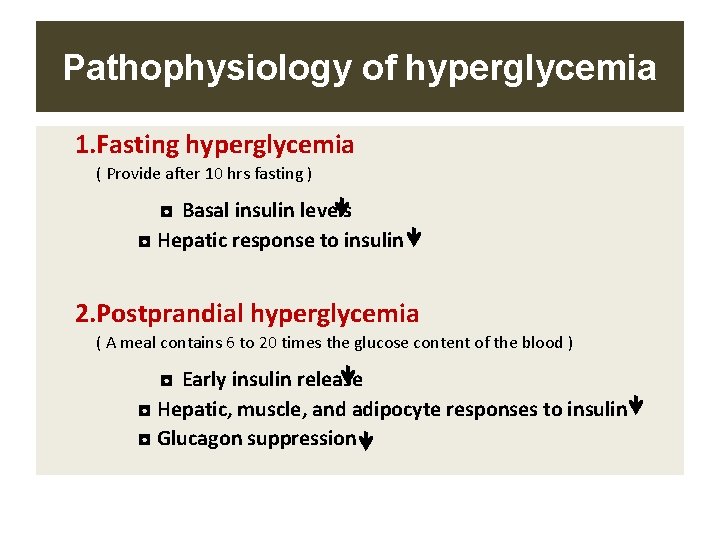
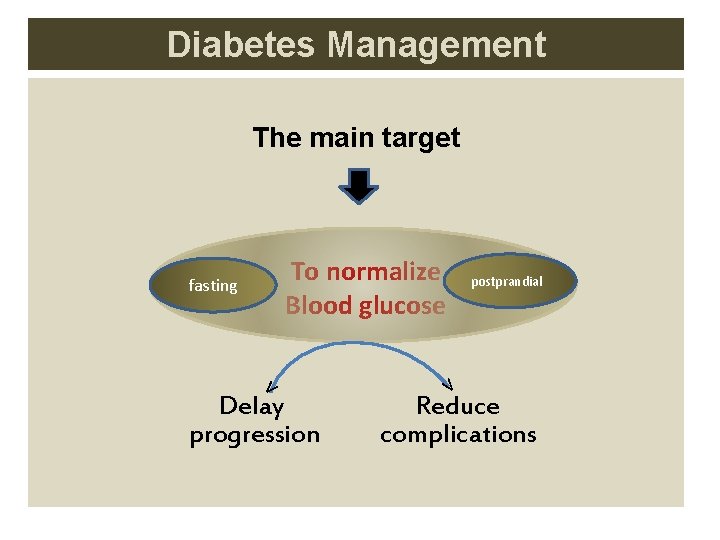
Pathophysiology of hyperglycemia 1. Fasting hyperglycemia ( Provide after 10 hrs fasting ) ◘ Basal insulin levels ◘ Hepatic response to insulin 2. Postprandial hyperglycemia ( A meal contains 6 to 20 times the glucose content of the blood ) ◘ Early insulin release ◘ Hepatic, muscle, and adipocyte responses to insulin ◘ Glucagon suppression
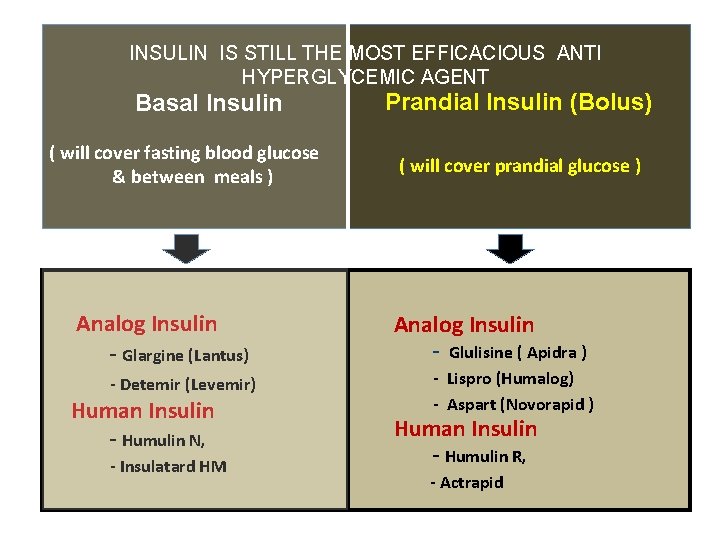
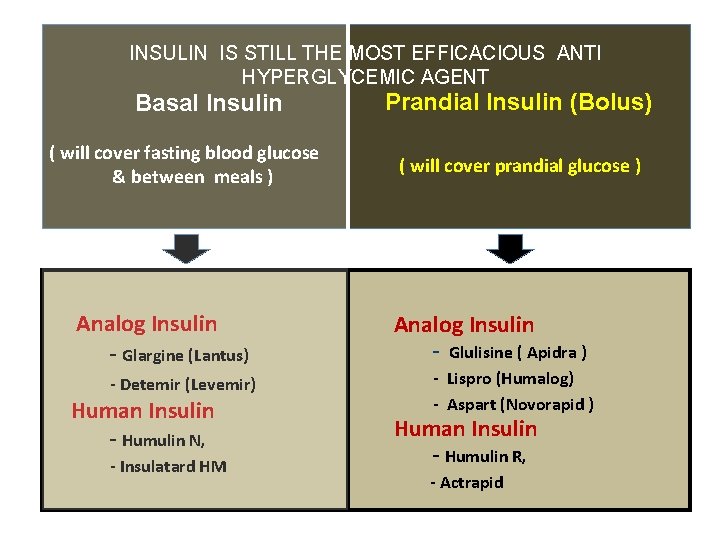
INSULIN IS STILL THE MOST EFFICACIOUS ANTI HYPERGLYCEMIC AGENT Basal Insulin ( will cover fasting blood glucose & between meals ) Analog Insulin - Glargine (Lantus) - Detemir (Levemir) Human Insulin - Humulin N, - Insulatard HM Prandial Insulin (Bolus) ( will cover prandial glucose ) Analog Insulin - Glulisine ( Apidra ) - Lispro (Humalog) - Aspart (Novorapid ) Human Insulin - Humulin R, - Actrapid
Adding Prandial Insulin Why
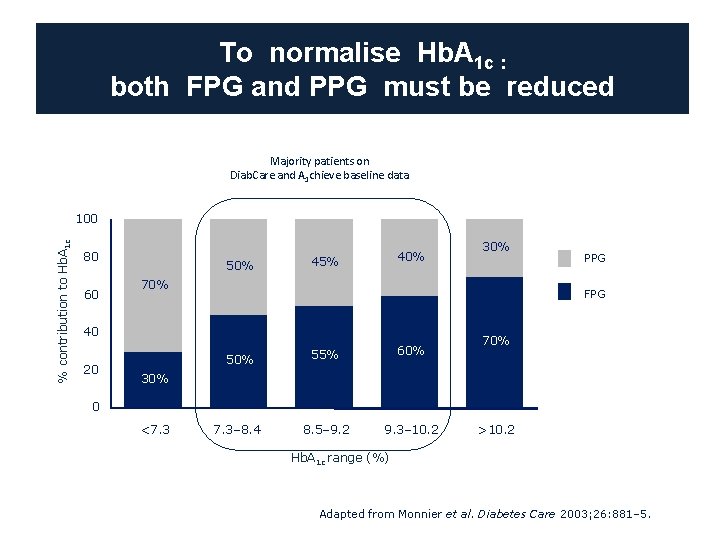
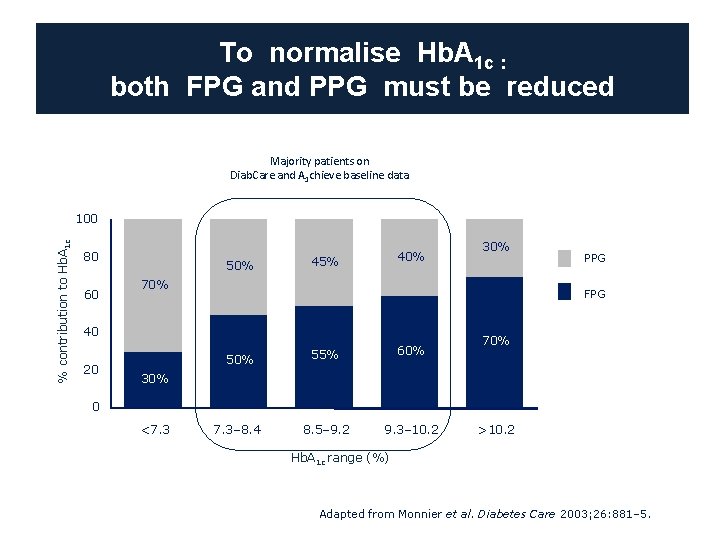
To normalise Hb. A 1 c : both FPG and PPG must be reduced Majority patients on Diab. Care and A 1 chieve baseline data % contribution to Hb. A 1 c 100 80 60 50% 45% 70% PPG FPG 40 20 30% 55% 60% 7. 3– 8. 4 8. 5– 9. 2 9. 3– 10. 2 70% 30% 0 <7. 3 >10. 2 Hb. A 1 c range (%) Adapted from Monnier et al. Diabetes Care 2003; 26: 881– 5.
Why do we need to intensify from basal insulin? Within 1 year, the majority of basal insulin patients will need another insulin to reach their glycaemic target 1. Holman et al. N Engl J Med 2007; 357: 1716– 30; 2 Garber AJ, et al. Diabetes, Obesity and Metabolism, 8, 2006, 58– 66.
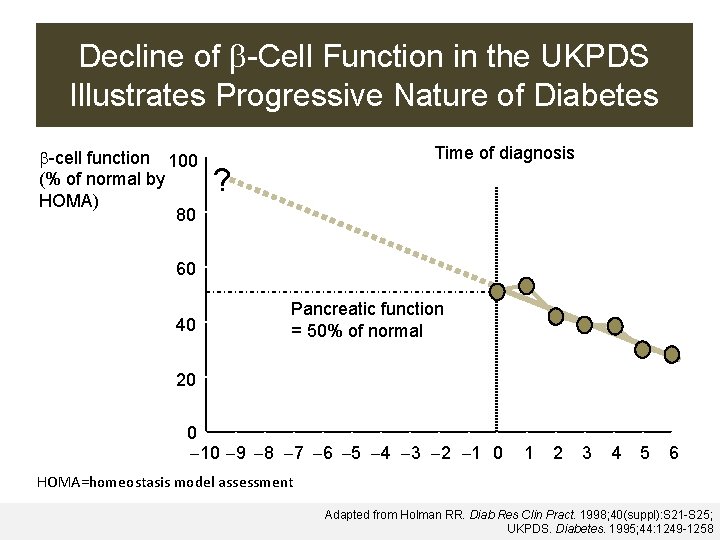
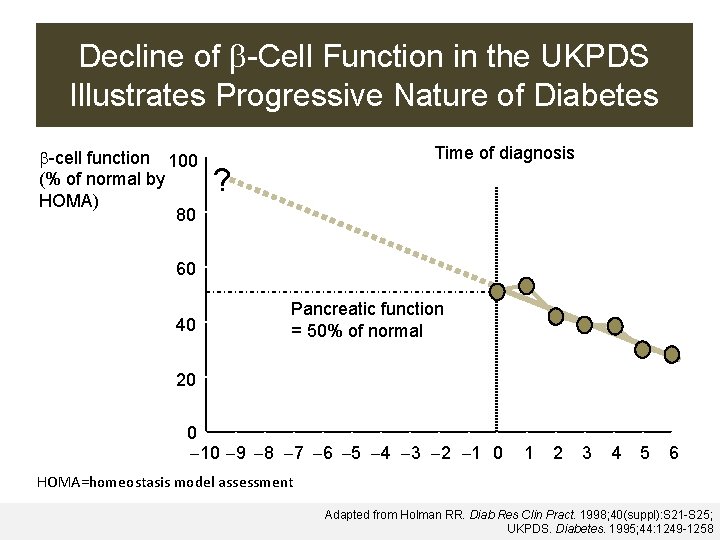
Decline of -Cell Function in the UKPDS Illustrates Progressive Nature of Diabetes -cell function 100 (% of normal by HOMA) 80 ? Time of diagnosis 60 40 Pancreatic function = 50% of normal 20 0 10 9 8 7 6 5 4 3 2 1 0 HOMA=homeostasis model. Years assessment 1 2 3 4 5 6 Adapted from Holman RR. Diab Res Clin Pract. 1998; 40(suppl): S 21 -S 25; UKPDS. Diabetes. 1995; 44: 1249 -1258
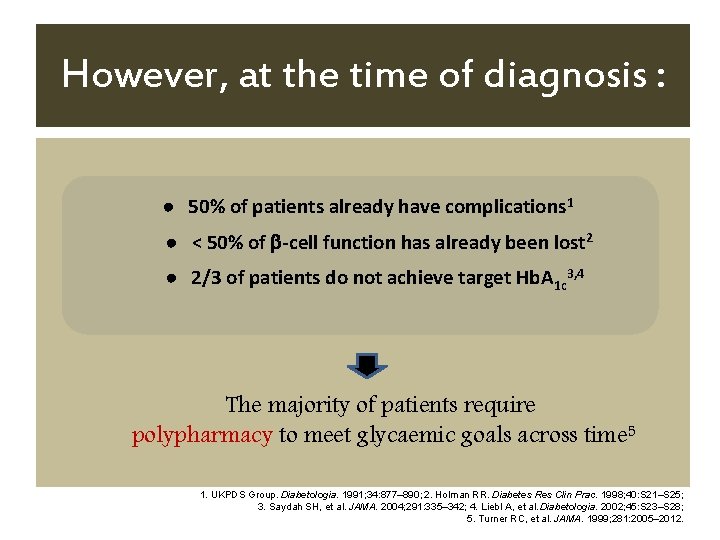
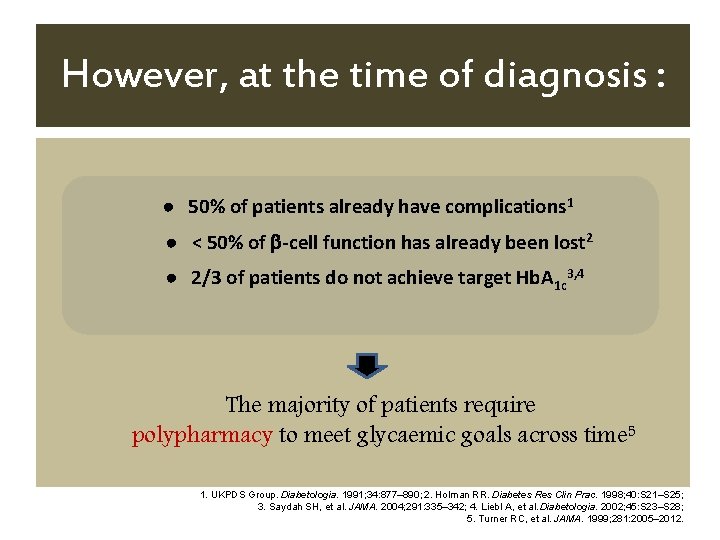
However, at the time of diagnosis : ● 50% of patients already have complications 1 ● < 50% of -cell function has already been lost 2 ● 2/3 of patients do not achieve target Hb. A 1 c 3, 4 The majority of patients require polypharmacy to meet glycaemic goals across time 5 1. UKPDS Group. Diabetologia. 1991; 34: 877– 890; 2. Holman RR. Diabetes Res Clin Prac. 1998; 40: S 21–S 25; 3. Saydah SH, et al. JAMA. 2004; 291: 335– 342; 4. Liebl A, et al. Diabetologia. 2002; 45: S 23–S 28; 5. Turner RC, et al. JAMA. 1999; 281: 2005– 2012.
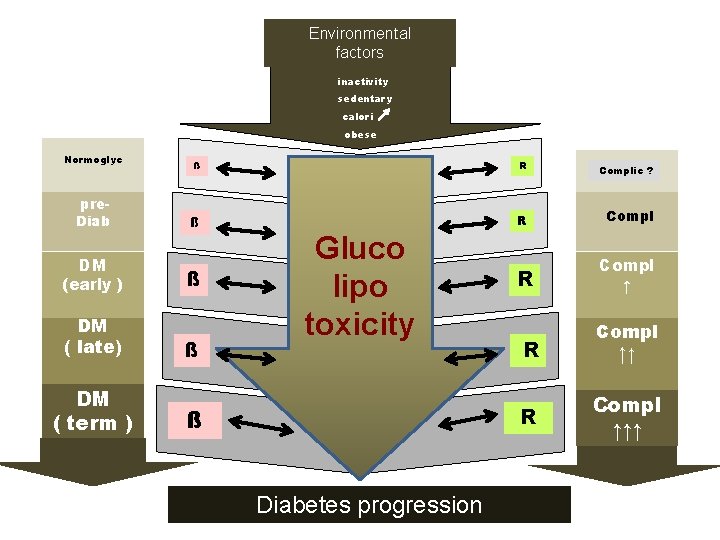
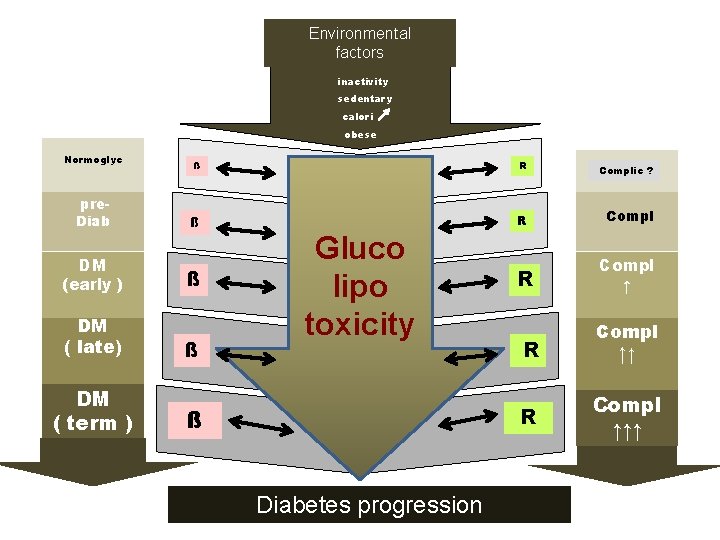
Environmental factors inactivity sedentary calori obese Normoglyc pre. Diab DM (early ) DM ( late) DM ( term ) ß R Complic ? ß R Compl Gluco Hyper lipo glycemia toxicity ß ß R R Diabetes progression Compl ↑ ↑ R Compl ↑↑↑
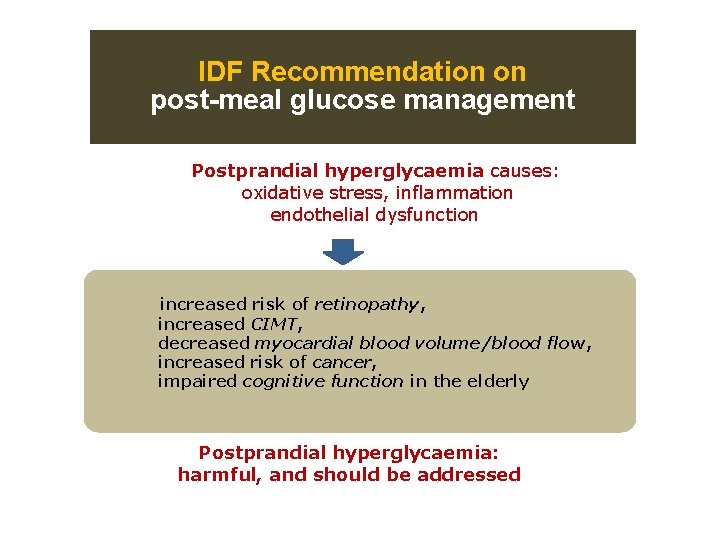
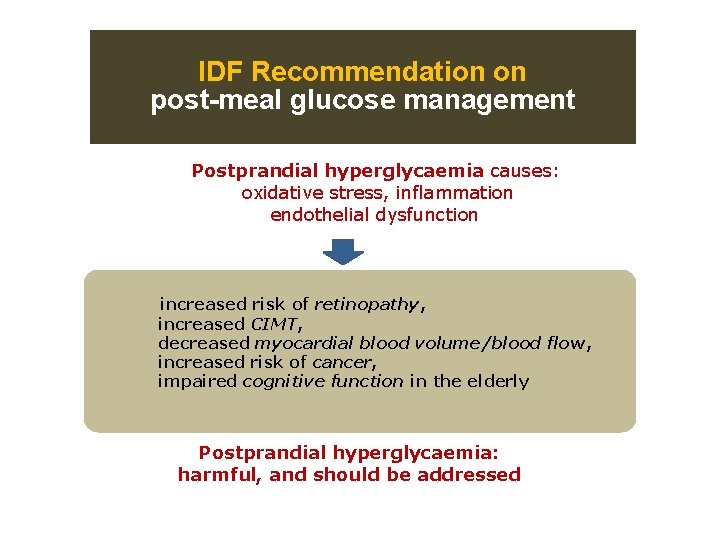
IDF Recommendation on post-meal glucose management Postprandial hyperglycaemia causes: oxidative stress, inflammation endothelial dysfunction increased risk of retinopathy, increased CIMT, decreased myocardial blood volume/blood flow, increased risk of cancer, impaired cognitive function in the elderly Postprandial hyperglycaemia: harmful, and should be addressed
Adding Prandial Insulin When
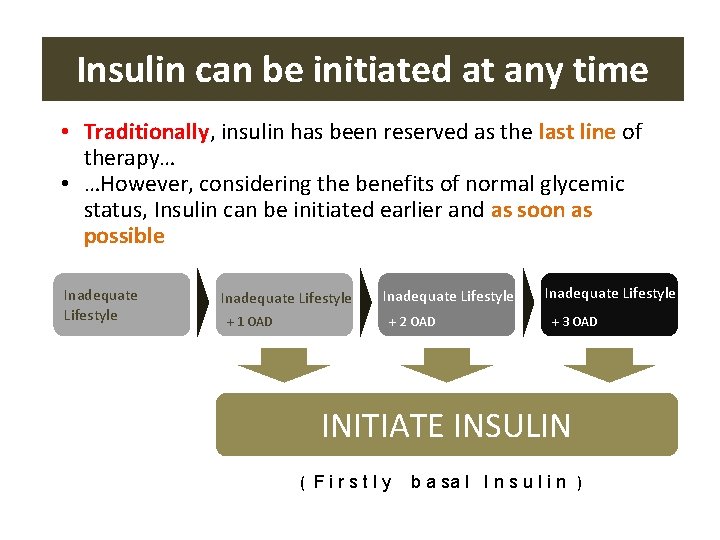
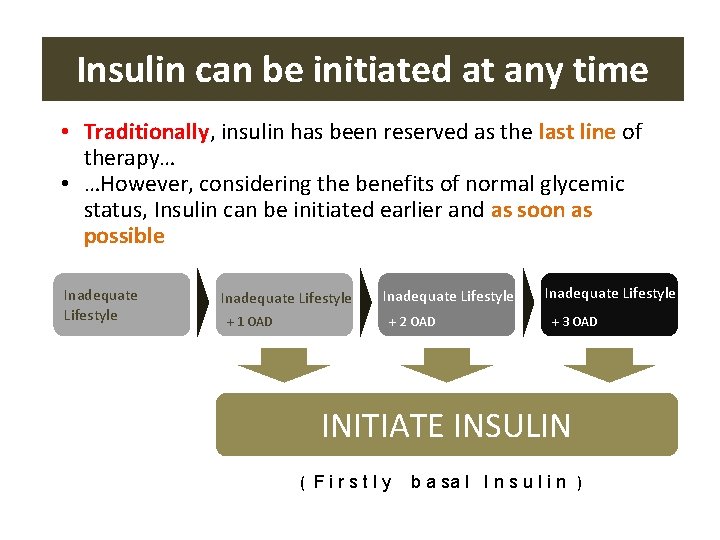
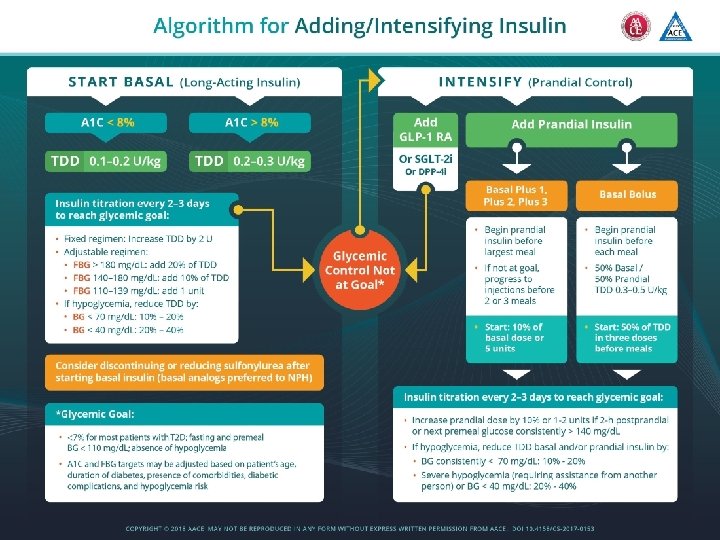
Insulin can be initiated at any time • Traditionally, insulin has been reserved as the last line of therapy… • …However, considering the benefits of normal glycemic status, Insulin can be initiated earlier and as soon as possible Inadequate Lifestyle + 1 OAD Inadequate Lifestyle + 2 OAD Inadequate Lifestyle + 3 OAD INITIATE INSULIN ( Firstly b a sa l I n s u l i n )
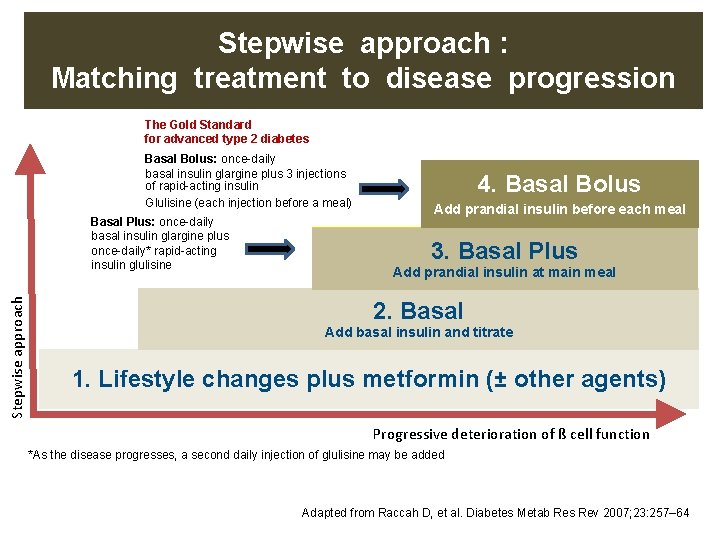
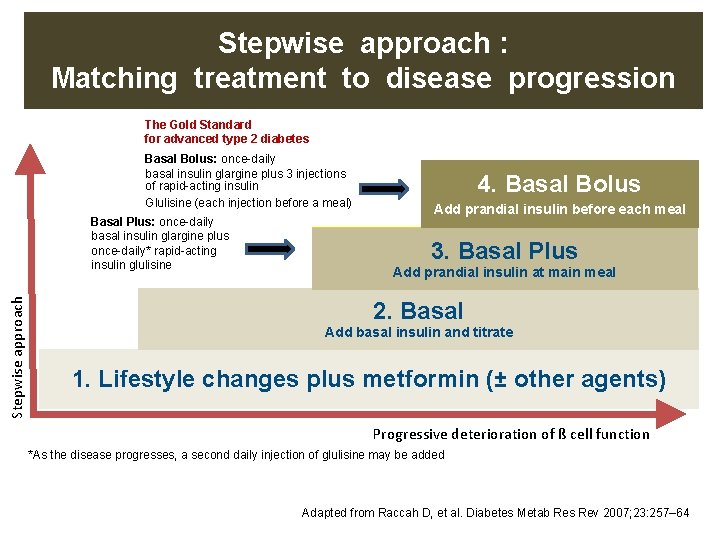
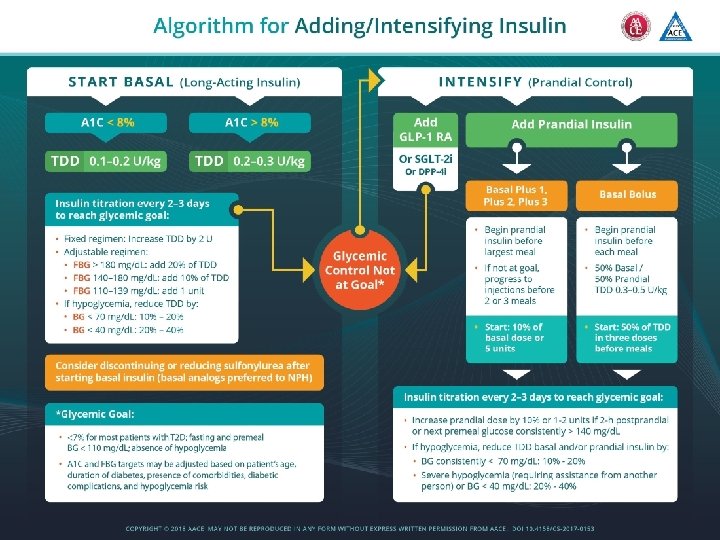
Stepwise approach : Matching treatment to disease progression The Gold Standard for advanced type 2 diabetes Basal Bolus: once-daily basal insulin glargine plus 3 injections of rapid-acting insulin Glulisine (each injection before a meal) Stepwise approach Basal Plus: once-daily basal insulin glargine plus once-daily* rapid-acting insulin glulisine 4. Basal Bolus Add prandial insulin before each meal 3. Basal. Plus Add prandial insulin at main meal 2. Basal Add basal insulin and titrate 1. Lifestyle changes plus metformin (± other agents) Progressive deterioration of ß cell function *As the disease progresses, a second daily injection of glulisine may be added Adapted from Raccah D, et al. Diabetes Metab Res Rev 2007; 23: 257– 64
Adding Prandial Insulin How
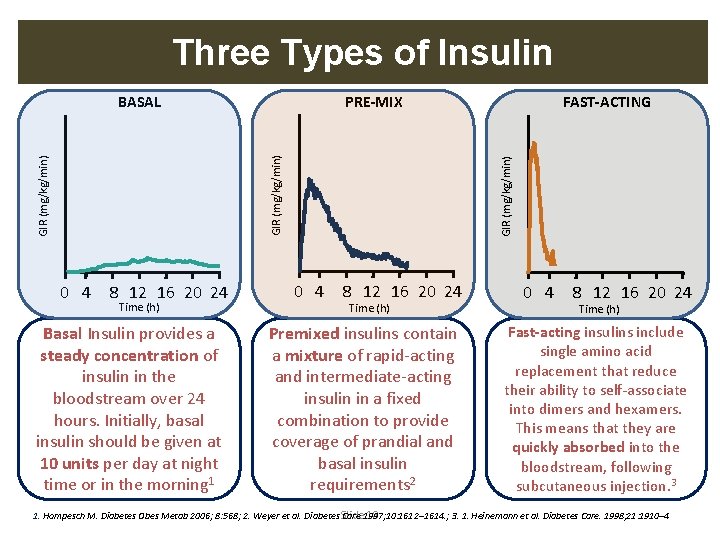
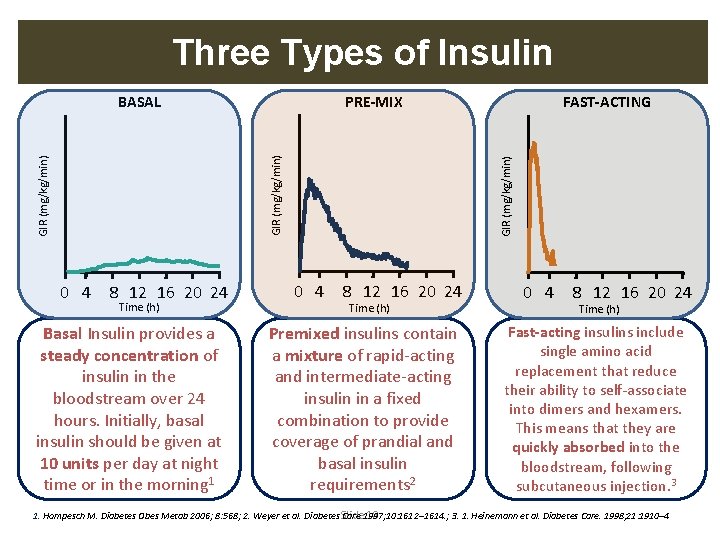
Three Types of Insulin PRE-MIX 0 4 8 12 16 20 24 Time (h) Basal Insulin provides a steady concentration of insulin in the bloodstream over 24 hours. Initially, basal insulin should be given at 10 units per day at night time or in the morning 1 FAST-ACTING GIR (mg/kg/min) BASAL 0 4 8 12 16 20 24 Time (h) Premixed insulins contain a mixture of rapid-acting and intermediate-acting insulin in a fixed combination to provide coverage of prandial and basal insulin requirements 2 0 4 8 12 16 20 24 Time (h) Fast-acting insulins include single amino acid replacement that reduce their ability to self-associate into dimers and hexamers. This means that they are quickly absorbed into the bloodstream, following subcutaneous injection. 3 1. Hompesch M. Diabetes Obes Metab 2006; 8: 568; 2. Weyer et al. Diabetes Slide Care 1997; 10: 1612– 1614. ; 3. 1. Heinemann et al. Diabetes Care. 1998; 21: 1910– 4 18
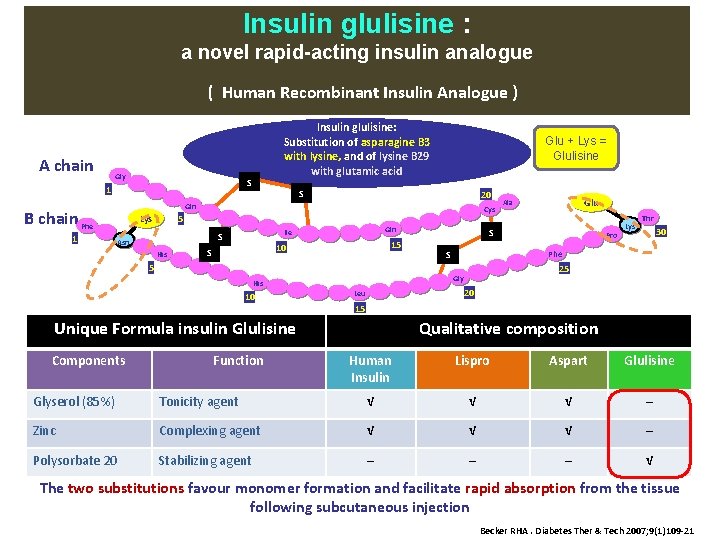
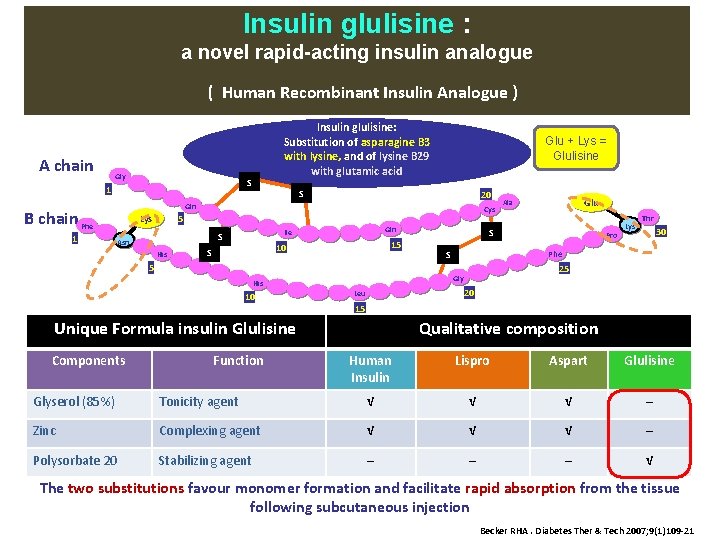
Insulin glulisine : a novel rapid-acting insulin analogue ( Human Recombinant Insulin Analogue ) A chain Gly S 1 Glu + Lys = Glulisine S 20 Gln B chain Phe 1 Insulin glulisine: Substitution of asparagine B 3 with lysine, and of lysine B 29 with glutamic acid Lys Cys 5 S Asn His Gln Ile 15 10 S 5 10 Function Pro Lys Thr 30 Phe S 25 20 Leu 15 Unique Formula insulin Glulisine Components S Gly His Glu Ala Qualitative composition Human Insulin Lispro Aspart Glulisine Glyserol (85%) Tonicity agent √ √ √ ─ Zinc Complexing agent √ √ √ ─ Polysorbate 20 Stabilizing agent ─ ─ ─ √ The two substitutions favour monomer formation and facilitate rapid absorption from the tissue following subcutaneous injection Becker RHA. Diabetes Ther & Tech 2007; 9(1)109 -21
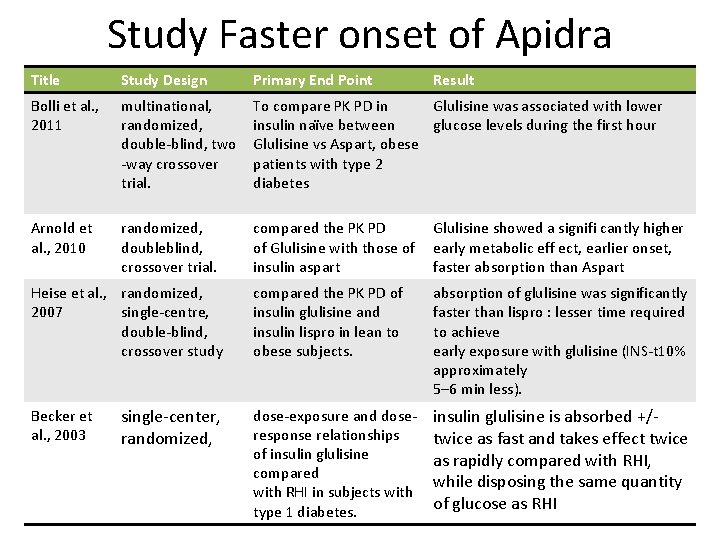
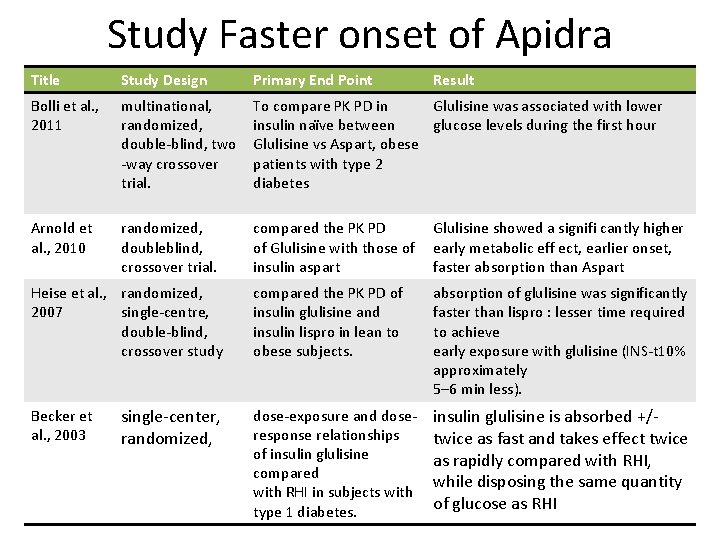
Study Faster onset of Apidra Title Study Design Primary End Point Bolli et al. , 2011 multinational, randomized, double-blind, two -way crossover trial. To compare PK PD in Glulisine was associated with lower insulin naïve between glucose levels during the first hour Glulisine vs Aspart, obese patients with type 2 diabetes Arnold et al. , 2010 randomized, doubleblind, crossover trial. compared the PK PD of Glulisine with those of insulin aspart Glulisine showed a signifi cantly higher early metabolic eff ect, earlier onset, faster absorption than Aspart compared the PK PD of insulin glulisine and insulin lispro in lean to obese subjects. absorption of glulisine was significantly faster than lispro : lesser time required to achieve early exposure with glulisine (INS-t 10% approximately 5– 6 min less). dose-exposure and doseresponse relationships of insulin glulisine compared with RHI in subjects with type 1 diabetes. insulin glulisine is absorbed +/twice as fast and takes effect twice as rapidly compared with RHI, while disposing the same quantity of glucose as RHI Heise et al. , randomized, 2007 single-centre, double-blind, crossover study Becker et al. , 2003 single-center, randomized, Result
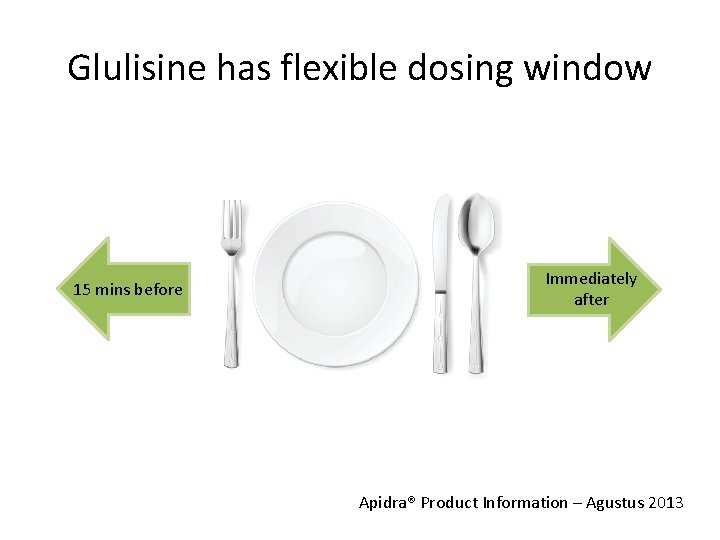
Glulisine has flexible dosing window 15 mins before Immediately after Apidra® Product Information – Agustus 2013
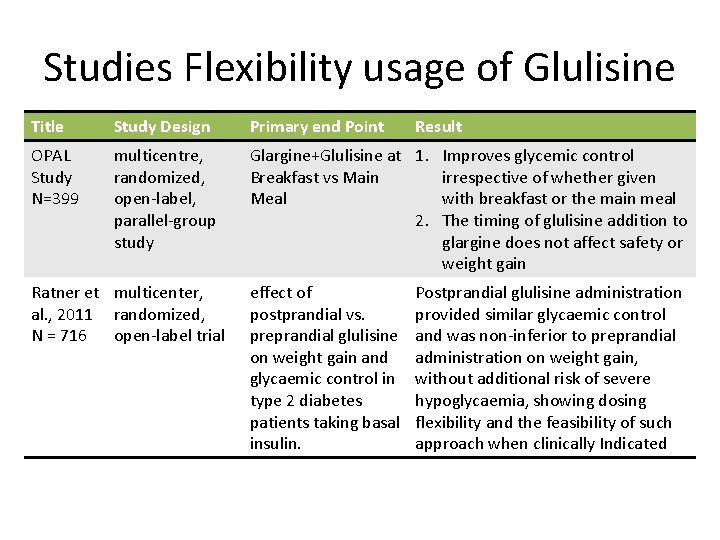
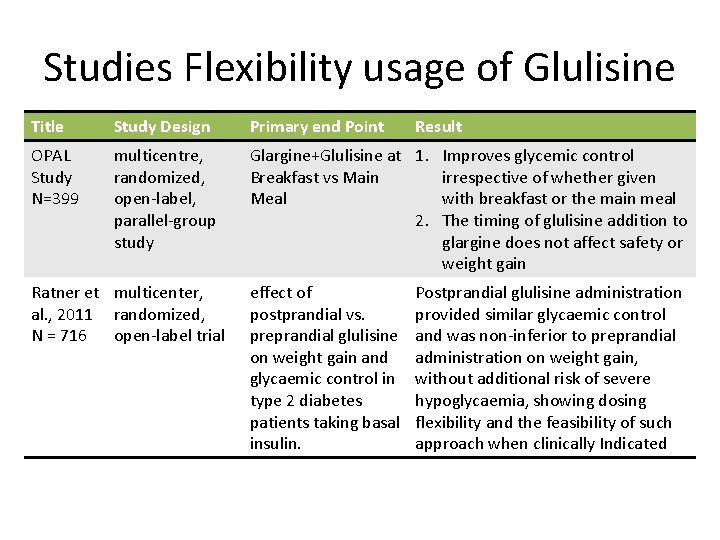
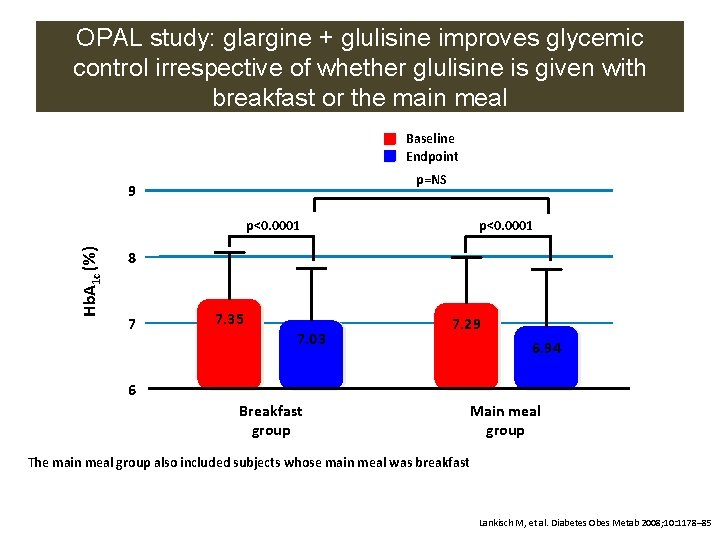
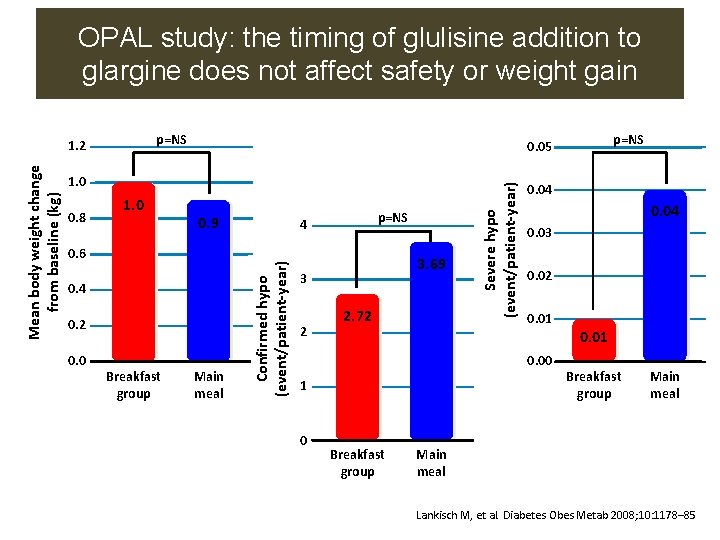
Studies Flexibility usage of Glulisine Title Study Design Primary end Point OPAL Study N=399 multicentre, randomized, open-label, parallel-group study Glargine+Glulisine at 1. Improves glycemic control Breakfast vs Main irrespective of whether given Meal with breakfast or the main meal 2. The timing of glulisine addition to glargine does not affect safety or weight gain Ratner et multicenter, al. , 2011 randomized, N = 716 open-label trial effect of postprandial vs. preprandial glulisine on weight gain and glycaemic control in type 2 diabetes patients taking basal insulin. Result Postprandial glulisine administration provided similar glycaemic control and was non-inferior to preprandial administration on weight gain, without additional risk of severe hypoglycaemia, showing dosing flexibility and the feasibility of such approach when clinically Indicated
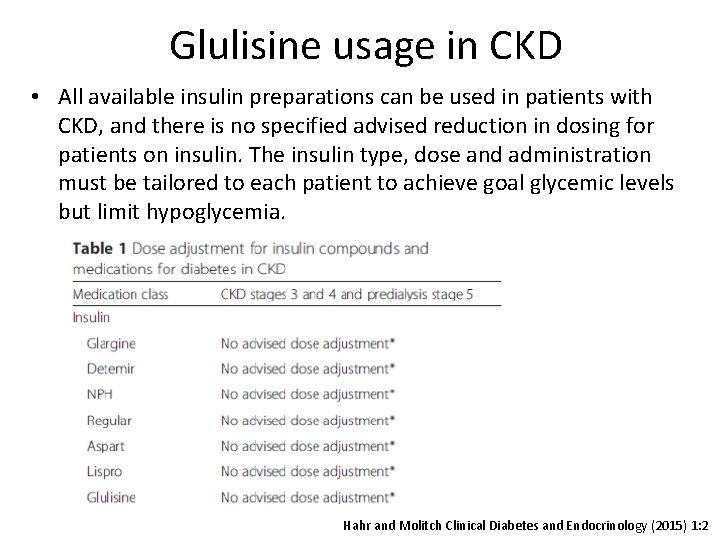
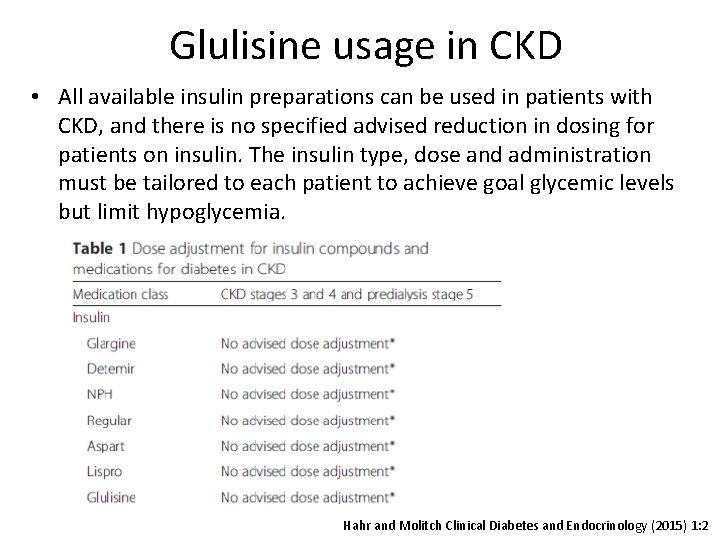
Glulisine usage in CKD • All available insulin preparations can be used in patients with CKD, and there is no specified advised reduction in dosing for patients on insulin. The insulin type, dose and administration must be tailored to each patient to achieve goal glycemic levels but limit hypoglycemia. Hahr and Molitch Clinical Diabetes and Endocrinology (2015) 1: 2
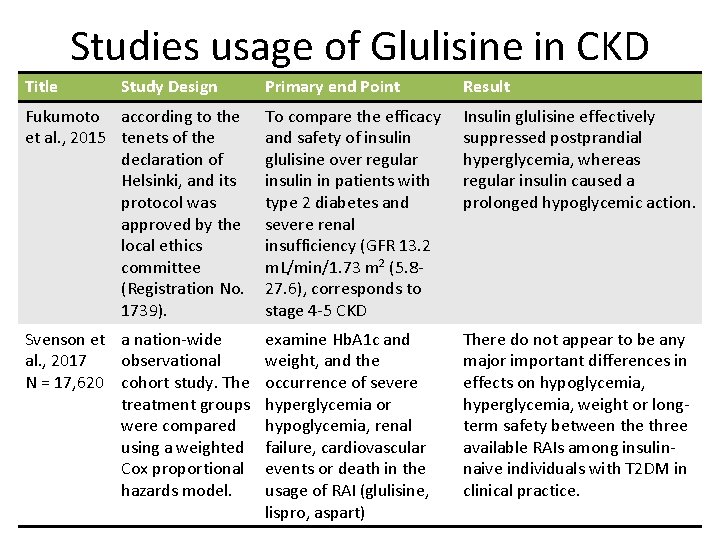
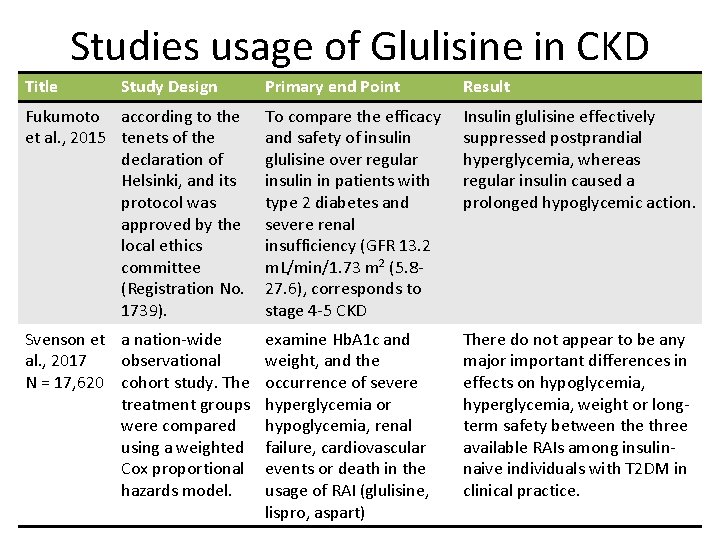
Studies usage of Glulisine in CKD Title Study Design Primary end Point Result Fukumoto according to the et al. , 2015 tenets of the declaration of Helsinki, and its protocol was approved by the local ethics committee (Registration No. 1739). To compare the efficacy and safety of insulin glulisine over regular insulin in patients with type 2 diabetes and severe renal insufficiency (GFR 13. 2 m. L/min/1. 73 m 2 (5. 827. 6), corresponds to stage 4 -5 CKD Insulin glulisine effectively suppressed postprandial hyperglycemia, whereas regular insulin caused a prolonged hypoglycemic action. Svenson et a nation-wide al. , 2017 observational N = 17, 620 cohort study. The treatment groups were compared using a weighted Cox proportional hazards model. examine Hb. A 1 c and weight, and the occurrence of severe hyperglycemia or hypoglycemia, renal failure, cardiovascular events or death in the usage of RAI (glulisine, lispro, aspart) There do not appear to be any major important differences in effects on hypoglycemia, hyperglycemia, weight or longterm safety between the three available RAIs among insulinnaive individuals with T 2 DM in clinical practice.
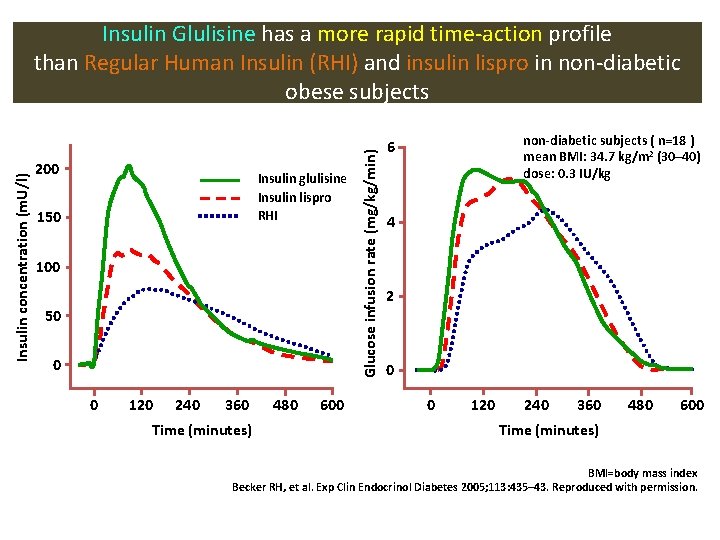
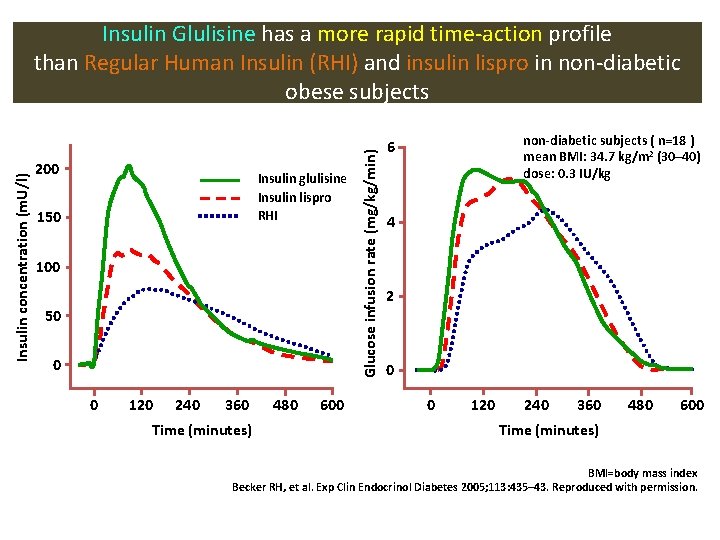
200 Insulin glulisine Insulin lispro RHI 150 100 50 0 0 120 240 360 Time (minutes) 480 600 Glucose infusion rate (mg/kg/min) Insulin concentration (m. U/l) Insulin Glulisine has a more rapid time-action profile than Regular Human Insulin (RHI) and insulin lispro in non-diabetic obese subjects non-diabetic subjects ( n=18 ) mean BMI: 34. 7 kg/m 2 (30– 40) dose: 0. 3 IU/kg 6 4 2 0 0 120 240 360 480 600 Time (minutes) BMI=body mass index Becker RH, et al. Exp Clin Endocrinol Diabetes 2005; 113: 435– 43. Reproduced with permission.
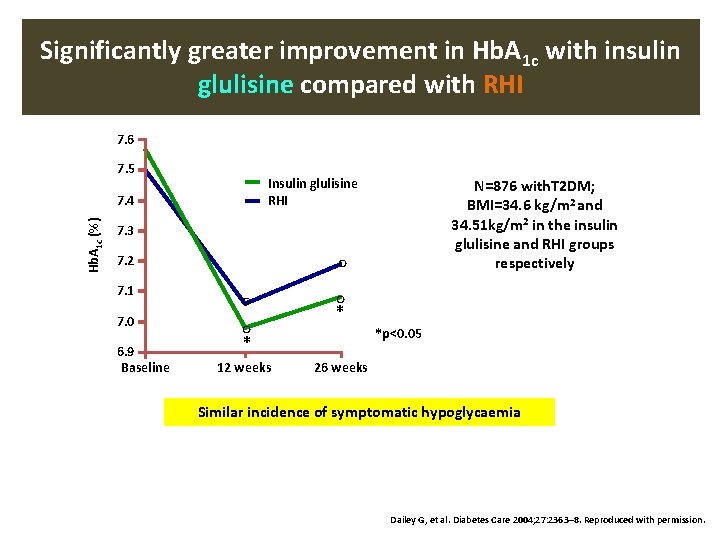
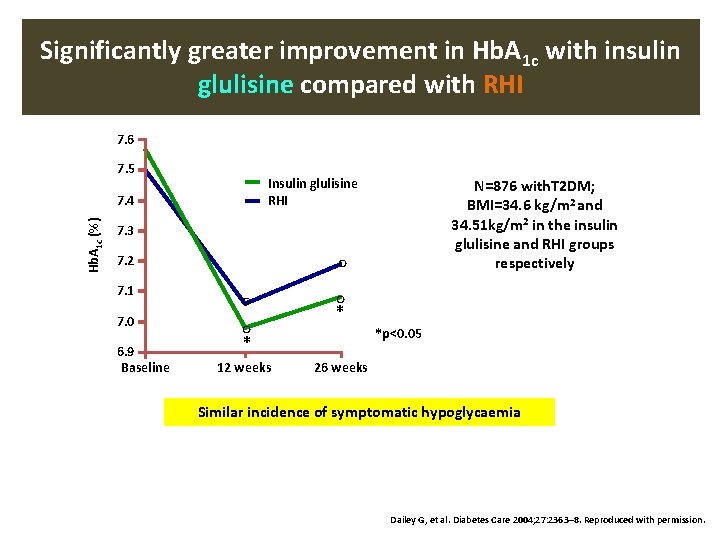
Significantly greater improvement in Hb. A 1 c with insulin glulisine compared with RHI 7. 6 7. 5 Insulin glulisine RHI Hb. A 1 c (%) 7. 4 N=876 with. T 2 DM; BMI=34. 6 kg/m 2 and 34. 51 kg/m 2 in the insulin glulisine and RHI groups respectively 7. 3 7. 2 7. 1 7. 0 6. 9 Baseline ◦ ◦* 12 weeks ◦ ◦* *p<0. 05 26 weeks Similar incidence of symptomatic hypoglycaemia Dailey G, et al. Diabetes Care 2004; 27: 2363– 8. Reproduced with permission.
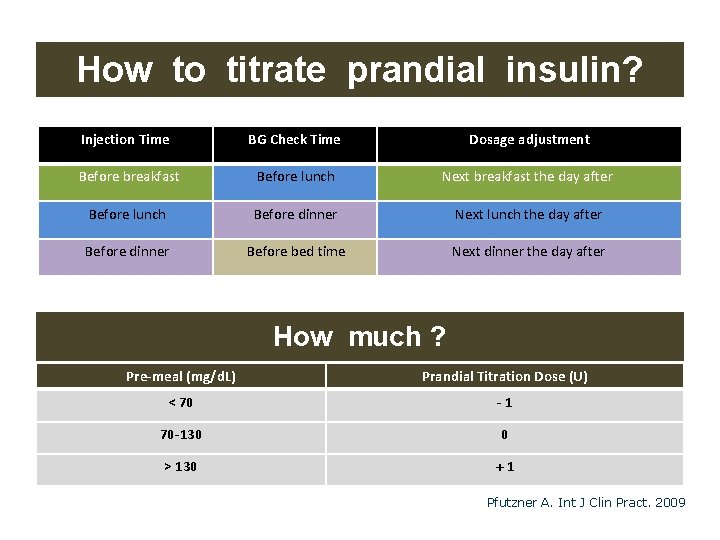
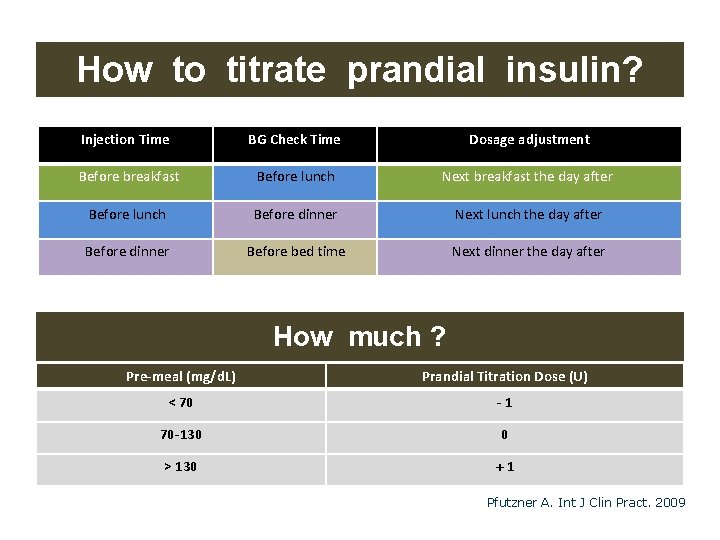
How to titrate prandial insulin? Injection Time BG Check Time Dosage adjustment Before breakfast Before lunch Next breakfast the day after Before lunch Before dinner Next lunch the day after Before dinner Before bed time Next dinner the day after How much ? Pre-meal (mg/d. L) Prandial Titration Dose (U) < 70 -1 70 -130 0 > 130 +1 Pfutzner A. Int J Clin Pract. 2009
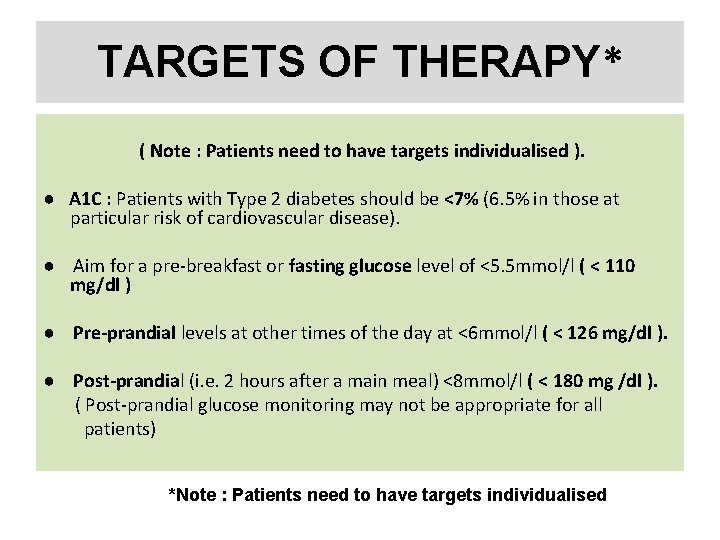
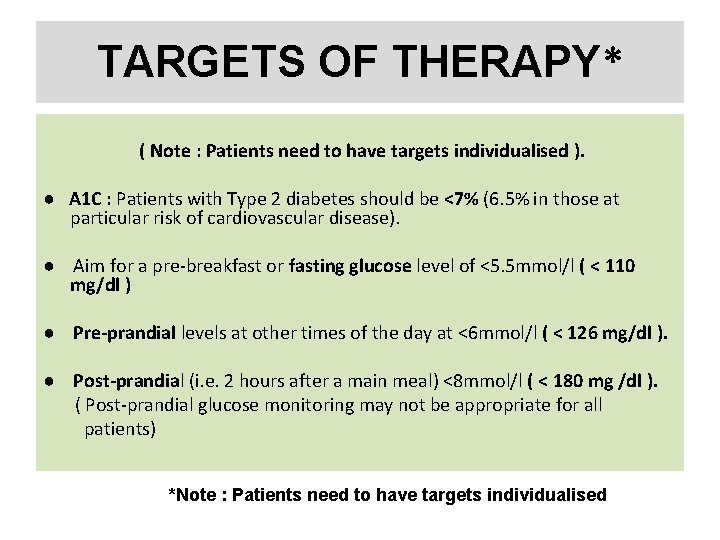
TARGETS OF THERAPY* ( Note : Patients need to have targets individualised ). ● A 1 C : Patients with Type 2 diabetes should be <7% (6. 5% in those at particular risk of cardiovascular disease). ● Aim for a pre-breakfast or fasting glucose level of <5. 5 mmol/l ( < 110 mg/dl ) ● Pre-prandial levels at other times of the day at <6 mmol/l ( < 126 mg/dl ). ● Post-prandial (i. e. 2 hours after a main meal) <8 mmol/l ( < 180 mg /dl ). ( Post-prandial glucose monitoring may not be appropriate for all patients) *Note : Patients need to have targets individualised
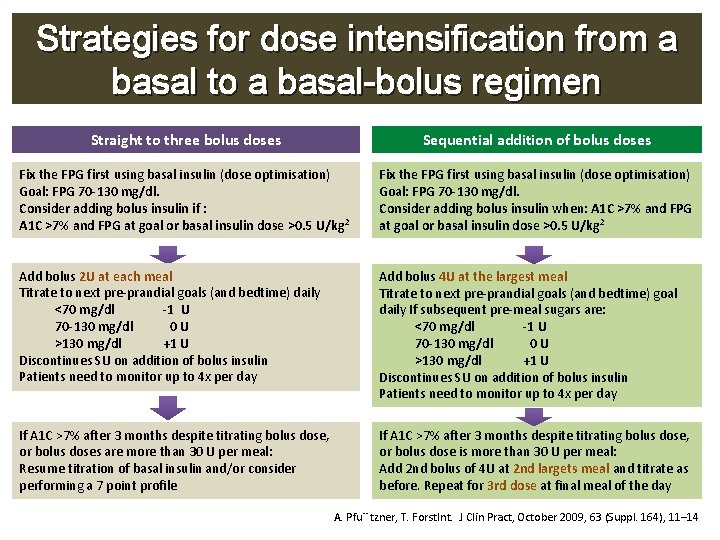
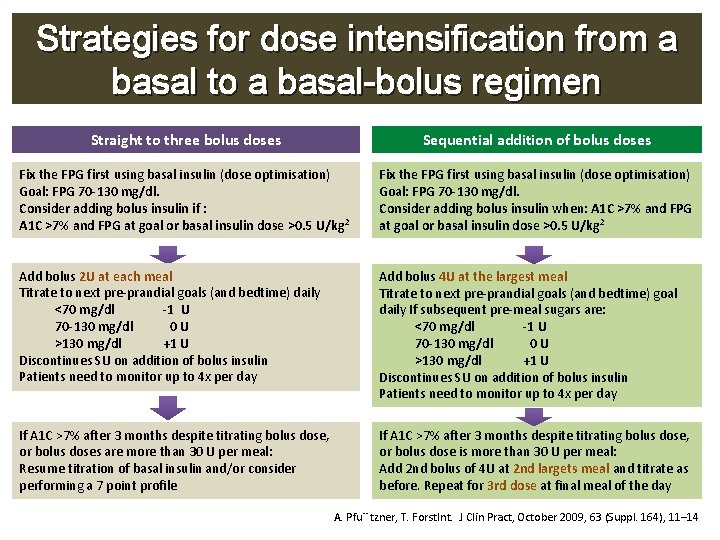
Strategies for dose intensification from a basal to a basal-bolus regimen Straight to three bolus doses Sequential addition of bolus doses Fix the FPG first using basal insulin (dose optimisation) Goal: FPG 70 -130 mg/dl. Consider adding bolus insulin if : A 1 C >7% and FPG at goal or basal insulin dose >0. 5 U/kg 2 Fix the FPG first using basal insulin (dose optimisation) Goal: FPG 70 -130 mg/dl. Consider adding bolus insulin when: A 1 C >7% and FPG at goal or basal insulin dose >0. 5 U/kg 2 Add bolus 2 U at each meal Titrate to next pre-prandial goals (and bedtime) daily <70 mg/dl -1 U 70 -130 mg/dl 0 U >130 mg/dl +1 U Discontinues SU on addition of bolus insulin Patients need to monitor up to 4 x per day Add bolus 4 U at the largest meal Titrate to next pre-prandial goals (and bedtime) goal daily If subsequent pre-meal sugars are: <70 mg/dl -1 U 70 -130 mg/dl 0 U >130 mg/dl +1 U Discontinues SU on addition of bolus insulin Patients need to monitor up to 4 x per day If A 1 C >7% after 3 months despite titrating bolus dose, or bolus doses are more than 30 U per meal: Resume titration of basal insulin and/or consider performing a 7 point profile If A 1 C >7% after 3 months despite titrating bolus dose, or bolus dose is more than 30 U per meal: Add 2 nd bolus of 4 U at 2 nd largets meal and titrate as before. Repeat for 3 rd dose at final meal of the day A. Pfu¨ tzner, T. Forst. Int. J Clin Pract, October 2009, 63 (Suppl. 164), 11– 14

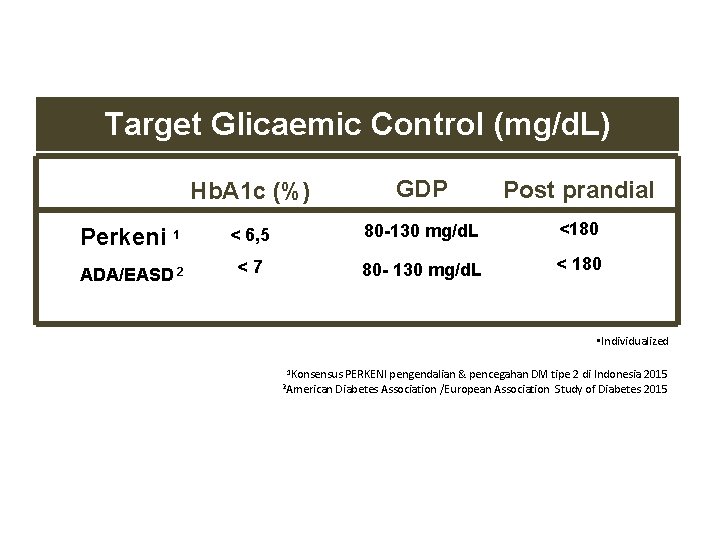
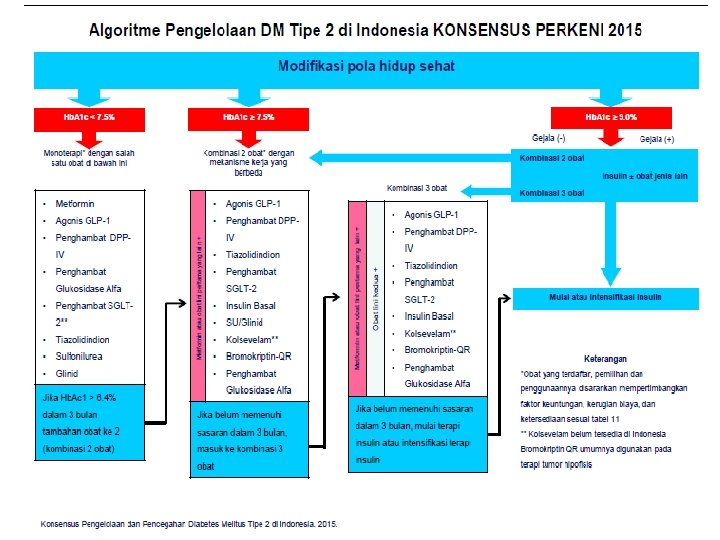
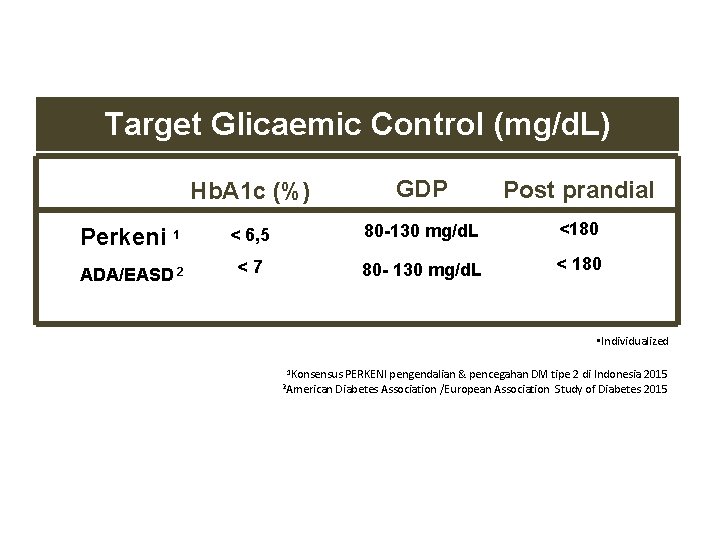
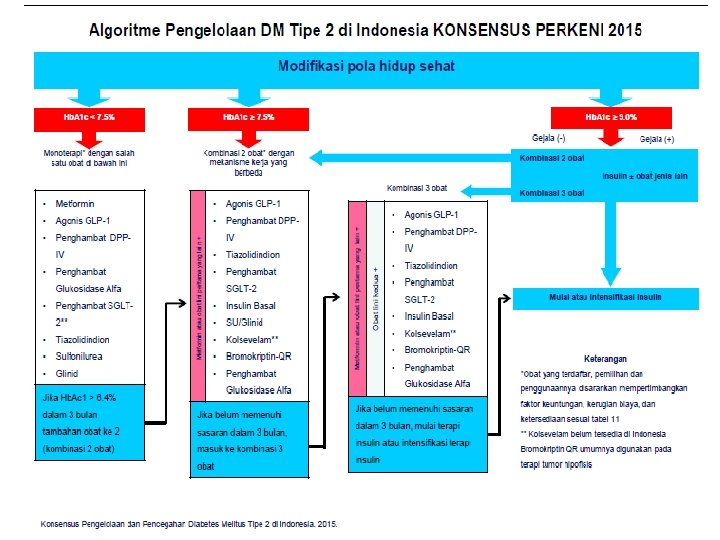
Target Glicaemic Control (mg/d. L) Hb. A 1 c (%) GDP Post prandial Perkeni 1 < 6, 5 80 -130 mg/d. L <180 ADA/EASD 2 <7 80 - 130 mg/d. L < 180 • Individualized 1 Konsensus 2 American PERKENI pengendalian & pencegahan DM tipe 2 di Indonesia 2015 Diabetes Association /European Association Study of Diabetes 2015
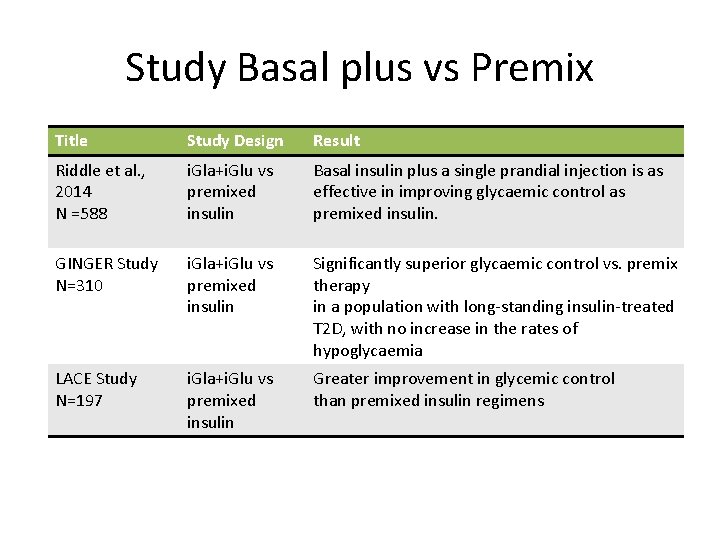
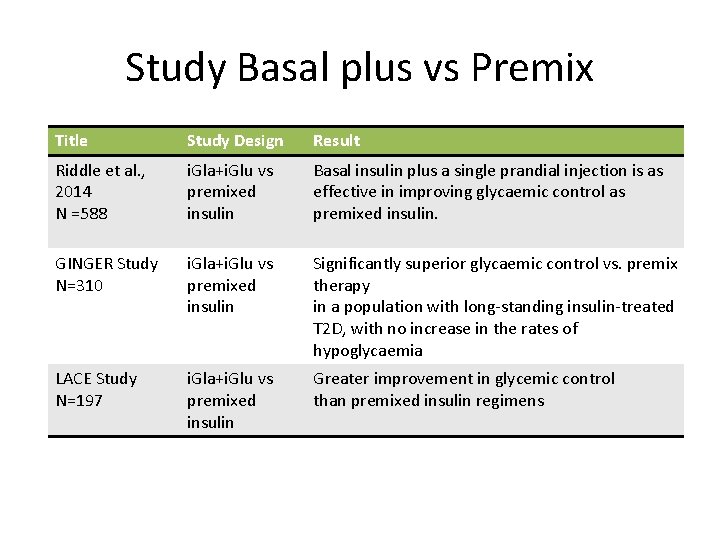
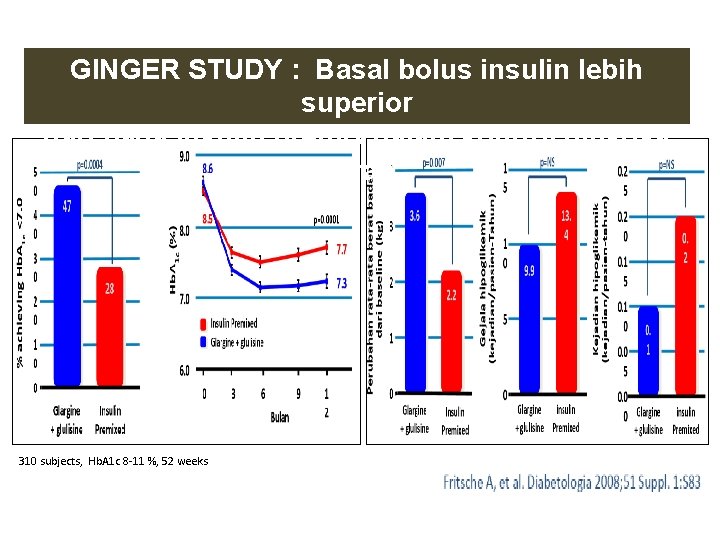
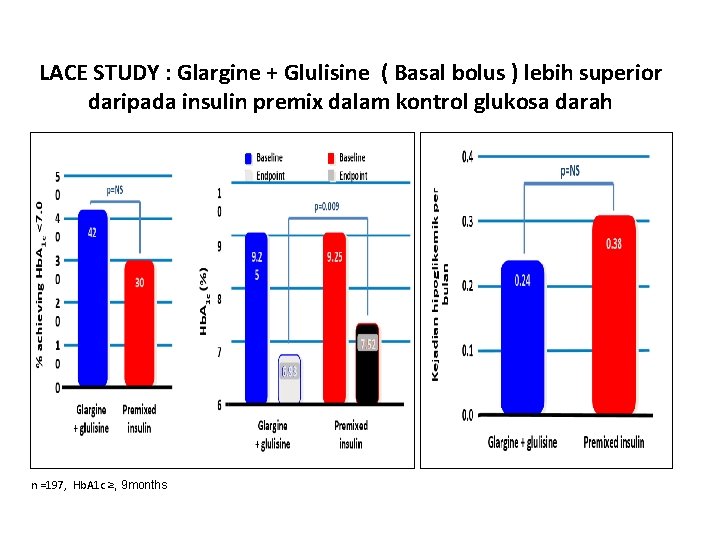
Study Basal plus vs Premix Title Study Design Result Riddle et al. , 2014 N =588 i. Gla+i. Glu vs premixed insulin Basal insulin plus a single prandial injection is as effective in improving glycaemic control as premixed insulin. GINGER Study N=310 i. Gla+i. Glu vs premixed insulin Significantly superior glycaemic control vs. premix therapy in a population with long-standing insulin-treated T 2 D, with no increase in the rates of hypoglycaemia LACE Study N=197 i. Gla+i. Glu vs premixed insulin Greater improvement in glycemic control than premixed insulin regimens
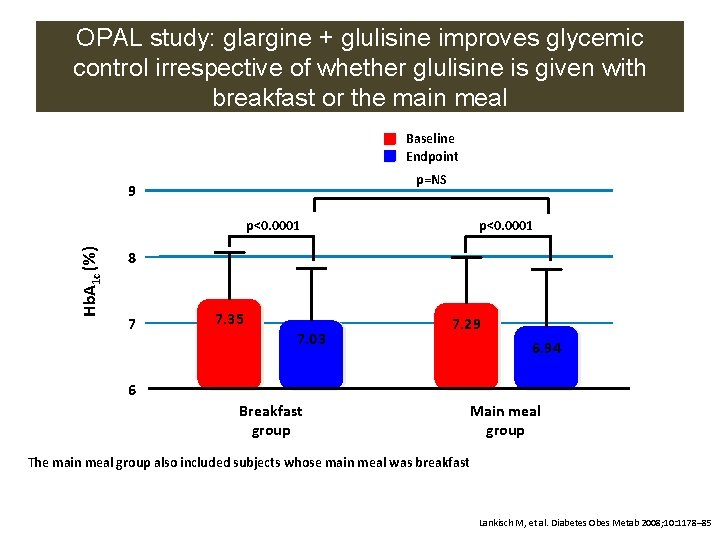
OPAL study: glargine + glulisine improves glycemic control irrespective of whether glulisine is given with breakfast or the main meal Baseline Endpoint p=NS 9 Hb. A 1 c (%) p<0. 0001 8 7 7. 35 7. 03 7. 29 6. 94 6 Breakfast group Main meal group The main meal group also included subjects whose main meal was breakfast Lankisch M, et al. Diabetes Obes Metab 2008; 10: 1178– 85
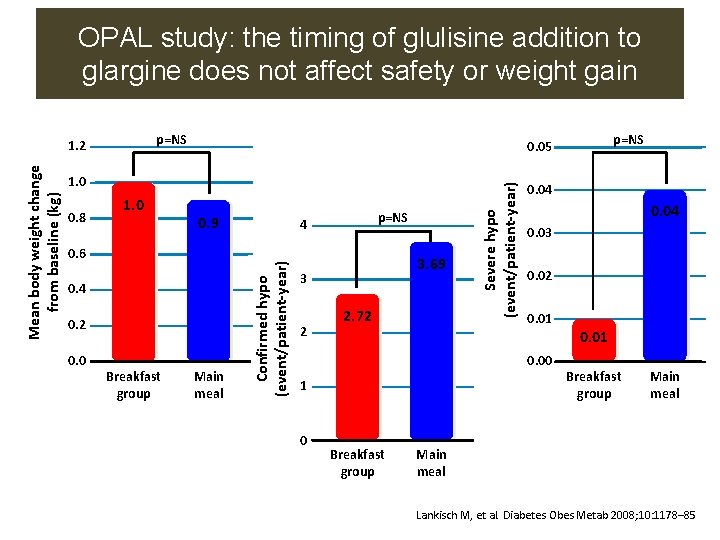
OPAL study: the timing of glulisine addition to glargine does not affect safety or weight gain p=NS 1. 0 0. 9 0. 6 0. 4 0. 2 0. 0 Breakfast group Main meal p=NS 4 3. 69 3 2 2. 72 Severe hypo (event/patient-year) 1. 0 0. 8 p=NS 0. 05 Confirmed hypo (event/patient-year) Mean body weight change from baseline (kg) 1. 2 0. 04 0. 03 0. 02 0. 01 0. 00 1 0 Breakfast group Main meal Lankisch M, et al. Diabetes Obes Metab 2008; 10: 1178– 85
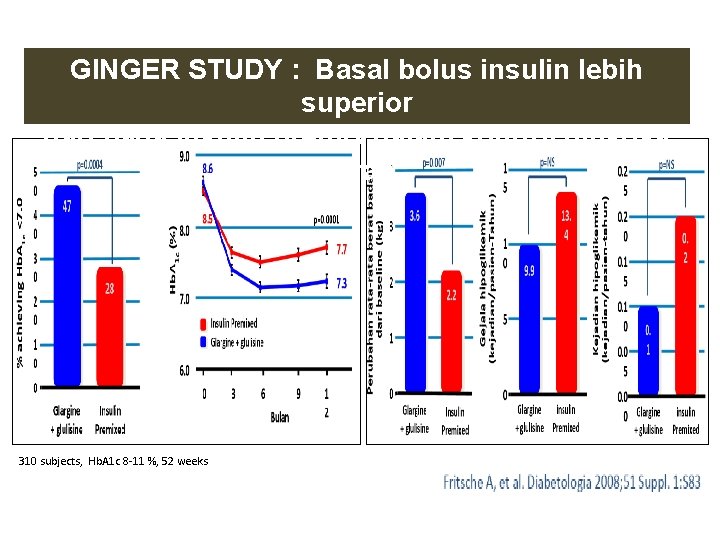
GINGER STUDY : Basal bolus insulin lebih superior dari pada insulin premix dalam kontrol glukosa darah 310 subjects, Hb. A 1 c 8 -11 %, 52 weeks
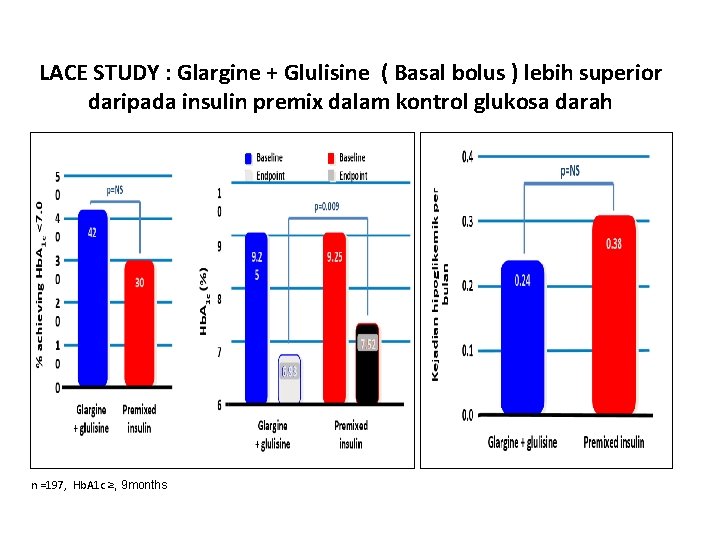
LACE STUDY : Glargine + Glulisine ( Basal bolus ) lebih superior LACE STUDY : Glargine + Glulisine ( Basal bolus ) lebihdarah superior daripada insulin premix dalam kontrol glukosa darah n =197, Hb. A 1 c ≥, 9 months
Conclusion • Blood glucose control, fasting and postprandial, is the main target in DM management for delaying progressivity and complication of disease • Early initiation of insulin addresses the issues of glucotoxicity, lipotoxicity, inflammation, first phase insulin response, insulin resistance and many other factors • Basal insulin will be the best of choice in starting diabetes treatment in which fasting blood glucose is considered as the first step to be controlled • Prandial insulin such as glulisine, should be added as combination treatment with basal insulin in order to get comprehensive blood glucose control, after fasting blood glucose is controlled. • There is evidences from studies that glulisine is superior to other prandial insulin, either human or insulin analogue, in efficacies and adverse events.