Why Vitamin D is important for Bone health

Why Vitamin D is important for Bone health? Basel Masri, MD Consultant Rheumatologist Jordan Osteoporosis Center Jordan Hospital J O P S Jordanian Osteoporosis Prevention Society Al-Najah University 9 October 2009 Nablus - Palestine
Vitamin D fat soluble prohormone necessary for bone health, it controls absorption of calcium from the intestines and its use in bone mineralization J O P S two important representatives: Vitamin D 2 found in plants considerably less potent than Vitamin D 3 naturally occurring form in humans
Sources of Vitamin D (1) Known as the Sunshine Vitamin ØSunlight Exposure provides 90% of vitamin D for the body’s daily requirement ØVitamin D production is affected by: v season J v duration and body-surface of exposure O v sunscreen use P v and skin pigmentation S *Sold in the United States, Canada, Argentina (optional), Brazil, Guatemala, Honduras, Mexico, Philippines (optional), and Venezuela Adapted from Holick MF; Allain TJ, Dhesi J; Webb AR et al; Reid IR et al; Matsuoka LY et al; Holick MF; Lips P; Macleod CC et al; Omdahl JL et al; Chen TC et al; Holick MF et al; Heaney RP; Segal E et al; Webb AR et al; Faulkner H et al; Roche Vitamins Europe Ltd.
Sources of Vitamin D (2) Endogenous production J O P S Ability of skin, liver and kidneys to form and process vitamin D *Sold in the United States, Canada, Argentina (optional), Brazil, Guatemala, Honduras, Mexico, Philippines (optional), and Venezuela Adapted from Holick MF; Allain TJ, Dhesi J; Webb AR et al; Reid IR et al; Matsuoka LY et al; Holick MF; Lips P; Macleod CC et al; Omdahl JL et al; Chen TC et al; Holick MF et al; Heaney RP; Segal E et al; Webb AR et al; Faulkner H et al; Roche Vitamins Europe Ltd.
Sources of Vitamin D (3) Dietary intake 10% only ØMinor source of vitamin D, providing 100 IU/day ØVitamin D is rare in foods other than fatty fish, eggs, and supplemented dairy products* ØEven vitamin D–fortified dairy products may not contain level indicated on label ØVitamin D can be supplied by multivitamins and J supplements O ØSupplements containing vitamin D alone are not readily available P ØPatient compliance with supplementation therapy is S inconsistent *Sold in the United States, Canada, Argentina (optional), Brazil, Guatemala, Honduras, Mexico, Philippines (optional), and Venezuela Adapted from Holick MF; Allain TJ, Dhesi J; Webb AR et al; Reid IR et al; Matsuoka LY et al; Holick MF; Lips P; Macleod CC et al; Omdahl JL et al; Chen TC et al; Holick MF et al; Heaney RP; Segal E et al; Webb AR et al; Faulkner H et al; Roche Vitamins Europe Ltd.
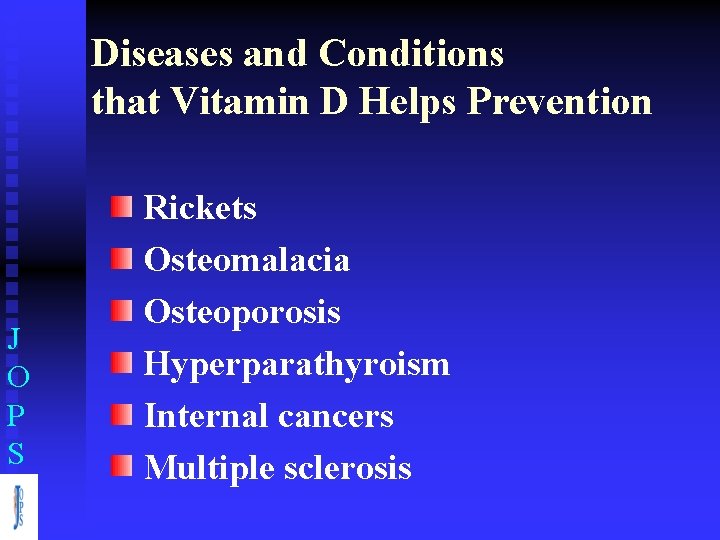
Diseases and Conditions that Vitamin D Helps Prevention J O P S Rickets Osteomalacia Osteoporosis Hyperparathyroism Internal cancers Multiple sclerosis
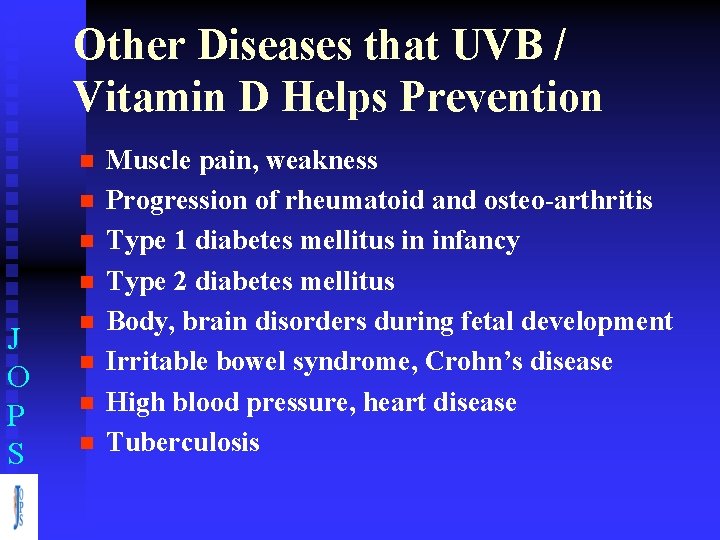
Other Diseases that UVB / Vitamin D Helps Prevention n n J O P S n n Muscle pain, weakness Progression of rheumatoid and osteo-arthritis Type 1 diabetes mellitus in infancy Type 2 diabetes mellitus Body, brain disorders during fetal development Irritable bowel syndrome, Crohn’s disease High blood pressure, heart disease Tuberculosis
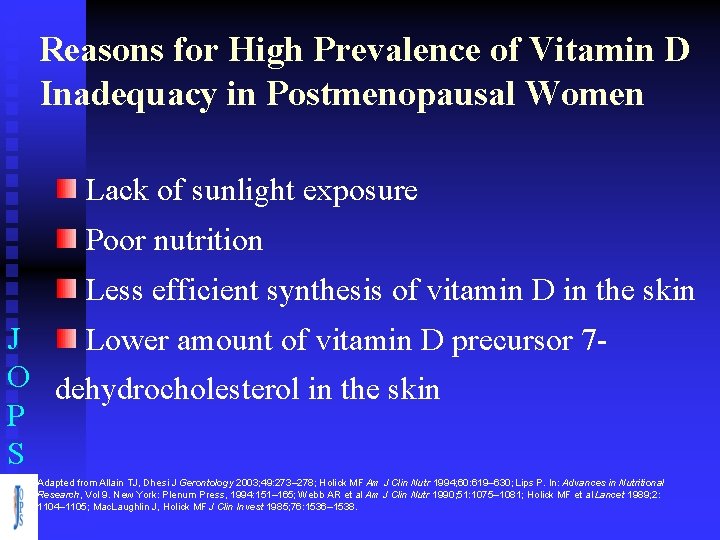
Reasons for High Prevalence of Vitamin D Inadequacy in Postmenopausal Women Lack of sunlight exposure Poor nutrition Less efficient synthesis of vitamin D in the skin J Lower amount of vitamin D precursor 7 O dehydrocholesterol in the skin P S Adapted from Allain TJ, Dhesi J Gerontology 2003; 49: 273– 278; Holick MF Am J Clin Nutr 1994; 60: 619– 630; Lips P. In: Advances in Nutritional Research, Vol 9. New York: Plenum Press, 1994: 151– 165; Webb AR et al Am J Clin Nutr 1990; 51: 1075– 1081; Holick MF et al Lancet 1989; 2: 1104– 1105; Mac. Laughlin J, Holick MF J Clin Invest 1985; 76: 1536– 1538.
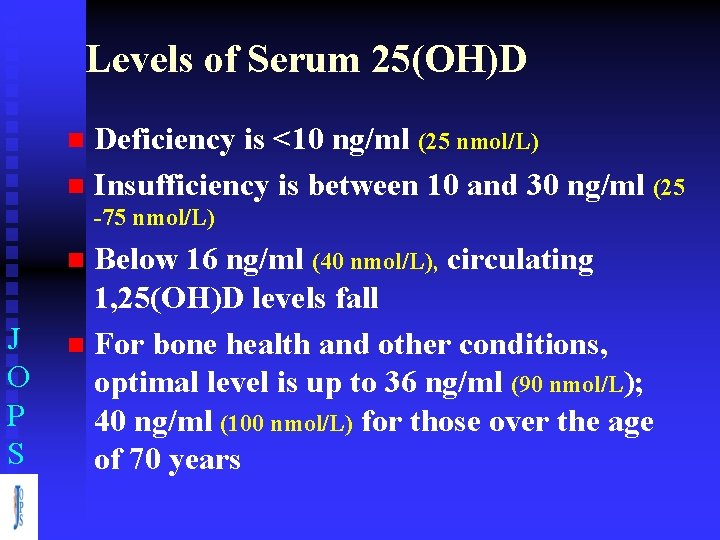
Levels of Serum 25(OH)D Deficiency is <10 ng/ml (25 nmol/L) n Insufficiency is between 10 and 30 ng/ml (25 n -75 nmol/L) Below 16 ng/ml (40 nmol/L), circulating 1, 25(OH)D levels fall n For bone health and other conditions, optimal level is up to 36 ng/ml (90 nmol/L); 40 ng/ml (100 nmol/L) for those over the age of 70 years n J O P S
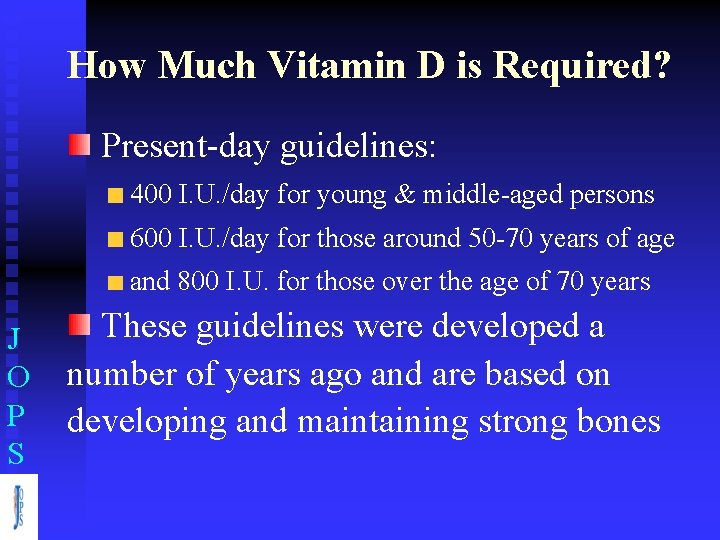
How Much Vitamin D is Required? Present-day guidelines: 400 I. U. /day for young & middle-aged persons 600 I. U. /day for those around 50 -70 years of age and 800 I. U. for those over the age of 70 years J O P S These guidelines were developed a number of years ago and are based on developing and maintaining strong bones
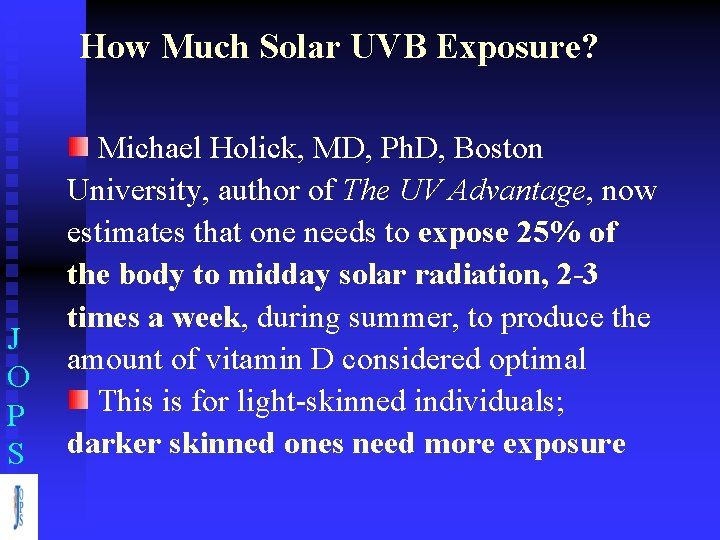
How Much Solar UVB Exposure? J O P S Michael Holick, MD, Ph. D, Boston University, author of The UV Advantage, now estimates that one needs to expose 25% of the body to midday solar radiation, 2 -3 times a week, during summer, to produce the amount of vitamin D considered optimal This is for light-skinned individuals; darker skinned ones need more exposure
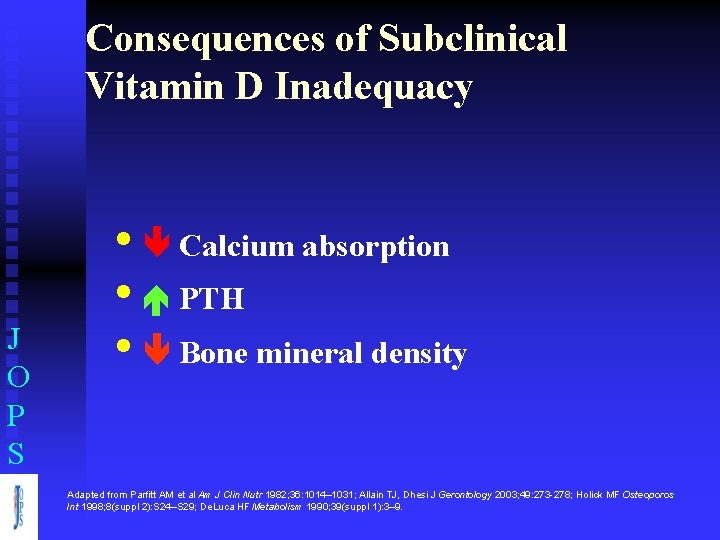
Consequences of Subclinical Vitamin D Inadequacy J O P S • Calcium absorption • PTH • Bone mineral density Adapted from Parfitt AM et al Am J Clin Nutr 1982; 36: 1014– 1031; Allain TJ, Dhesi J Gerontology 2003; 49: 273 -278; Holick MF Osteoporos Int 1998; 8(suppl 2): S 24–S 29; De. Luca HF Metabolism 1990; 39(suppl 1): 3– 9.
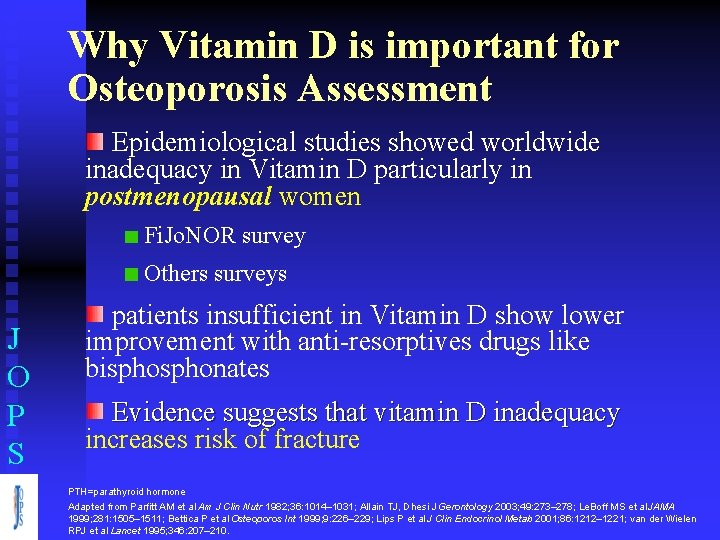
Why Vitamin D is important for Osteoporosis Assessment Epidemiological studies showed worldwide inadequacy in Vitamin D particularly in postmenopausal women Fi. Jo. NOR survey Others surveys J O P S patients insufficient in Vitamin D show lower improvement with anti-resorptives drugs like bisphonates Evidence suggests that vitamin D inadequacy increases risk of fracture PTH=parathyroid hormone Adapted from Parfitt AM et al Am J Clin Nutr 1982; 36: 1014– 1031; Allain TJ, Dhesi J Gerontology 2003; 49: 273– 278; Le. Boff MS et al JAMA 1999; 281: 1505– 1511; Bettica P et al Osteoporos Int 1999; 9: 226– 229; Lips P et al J Clin Endocrinol Metab 2001; 86: 1212– 1221; van der Wielen RPJ et al Lancet 1995; 346: 207– 210.
First Jordanian National Osteoporosis Record Fi. Jo. NOR J O P S Vitamin D Data Fi. Jo. NOR B. Masri, E. Azar, A. Faqih (JOPS)
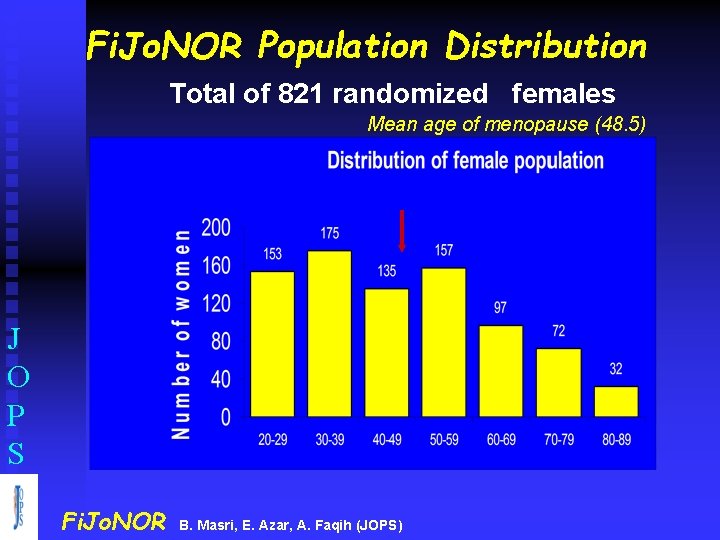
Fi. Jo. NOR Population Distribution Total of 821 randomized females Mean age of menopause (48. 5) J O P S Fi. Jo. NOR B. Masri, E. Azar, A. Faqih (JOPS)
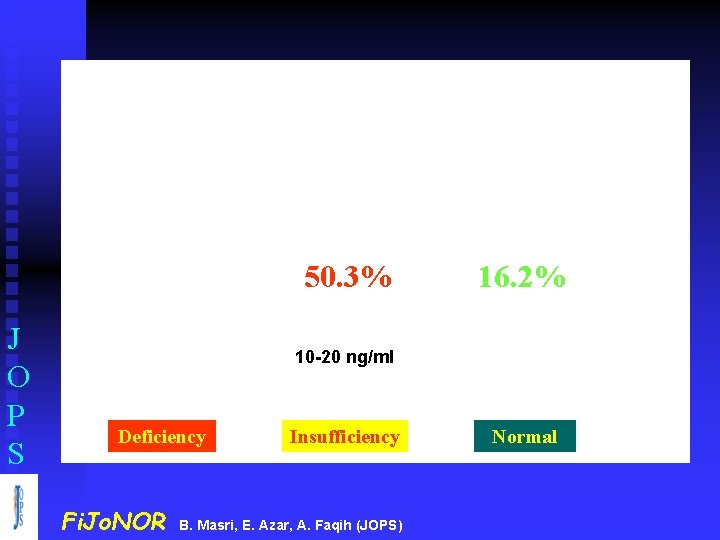
J O P S 33. 5% 50. 3% 16. 2% < 10 ng/ml 10 -20 ng/ml > 20 ng/ml Deficiency Insufficiency Normal Fi. Jo. NOR B. Masri, E. Azar, A. Faqih (JOPS)
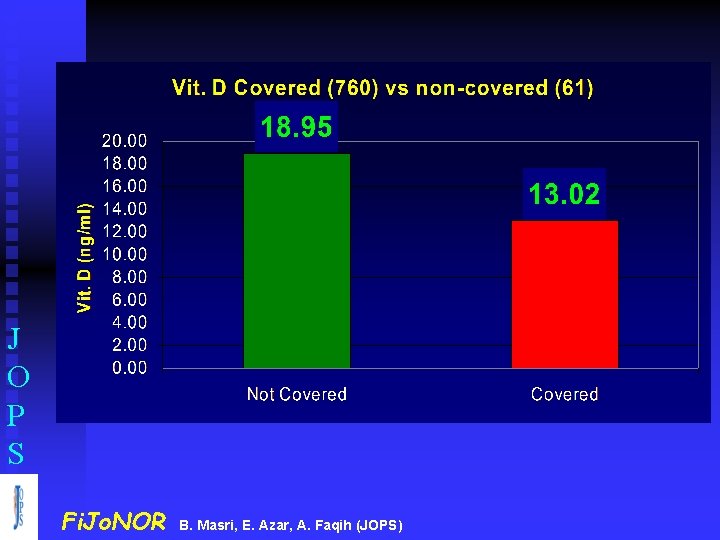
J O P S Fi. Jo. NOR B. Masri, E. Azar, A. Faqih (JOPS)
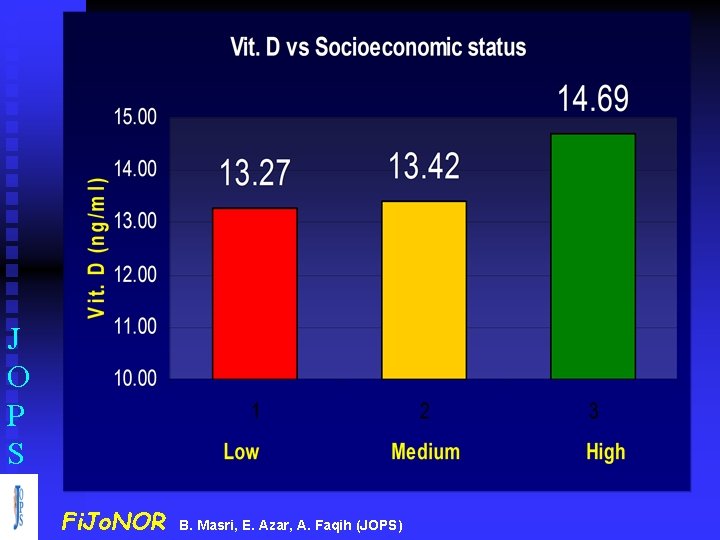
J O P S Fi. Jo. NOR B. Masri, E. Azar, A. Faqih (JOPS)
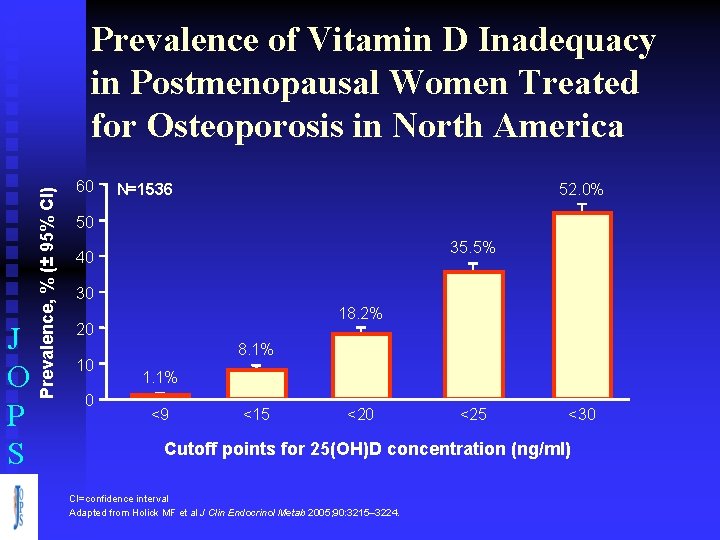
J O P S Prevalence, % (± 95% CI) Prevalence of Vitamin D Inadequacy in Postmenopausal Women Treated for Osteoporosis in North America 60 52. 0% N=1536 50 35. 5% 40 30 18. 2% 20 10 0 8. 1% 1. 1% <9 <15 <20 <25 <30 Cutoff points for 25(OH)D concentration (ng/ml) CI=confidence interval Adapted from Holick MF et al J Clin Endocrinol Metab 2005; 90: 3215– 3224.
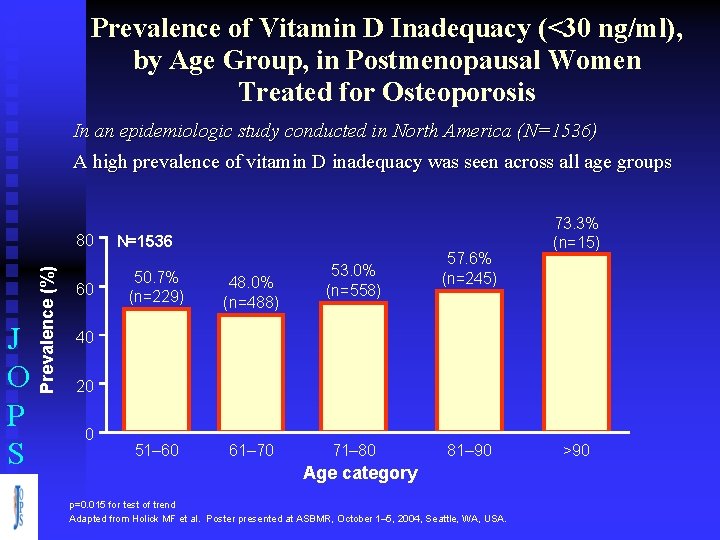
Prevalence of Vitamin D Inadequacy (<30 ng/ml), by Age Group, in Postmenopausal Women Treated for Osteoporosis In an epidemiologic study conducted in North America (N=1536) A high prevalence of vitamin D inadequacy was seen across all age groups J O P S Prevalence (%) 80 60 N=1536 50. 7% (n=229) 48. 0% (n=488) 51– 60 61– 70 53. 0% (n=558) 57. 6% (n=245) 73. 3% (n=15) 40 20 0 71– 80 81– 90 Age category p=0. 015 for test of trend Adapted from Holick MF et al. Poster presented at ASBMR, October 1– 5, 2004, Seattle, WA, USA. >90
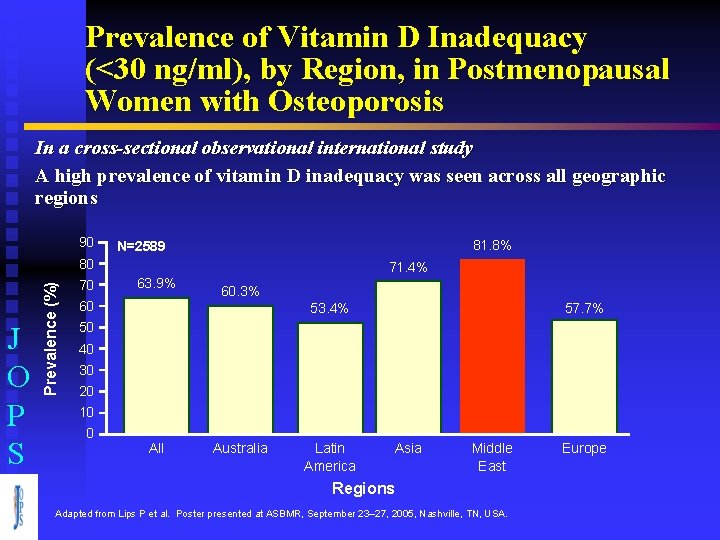
Prevalence of Vitamin D Inadequacy (<30 ng/ml), by Region, in Postmenopausal Women with Osteoporosis In a cross-sectional observational international study A high prevalence of vitamin D inadequacy was seen across all geographic regions 90 81. 8% N=2589 J O P S Prevalence (%) 80 70 71. 4% 63. 9% 60 60. 3% 53. 4% 57. 7% 50 40 30 20 10 0 All Australia Latin America Asia Middle East Regions Adapted from Lips P et al. Poster presented at ASBMR, September 23– 27, 2005, Nashville, TN, USA. Europe
Vitamin D Supplementation Decreases Fracture Risk J O P S
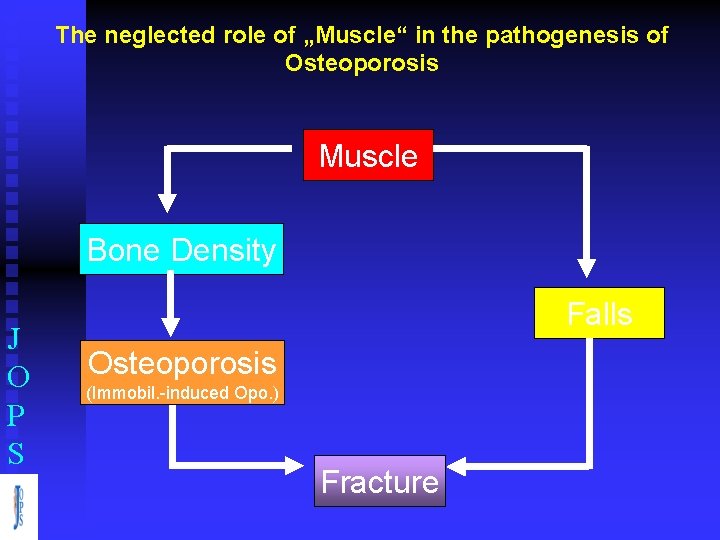
The neglected role of „Muscle“ in the pathogenesis of Osteoporosis Muscle Bone Density J O P S Falls Osteoporosis (Immobil. -induced Opo. ) Fracture
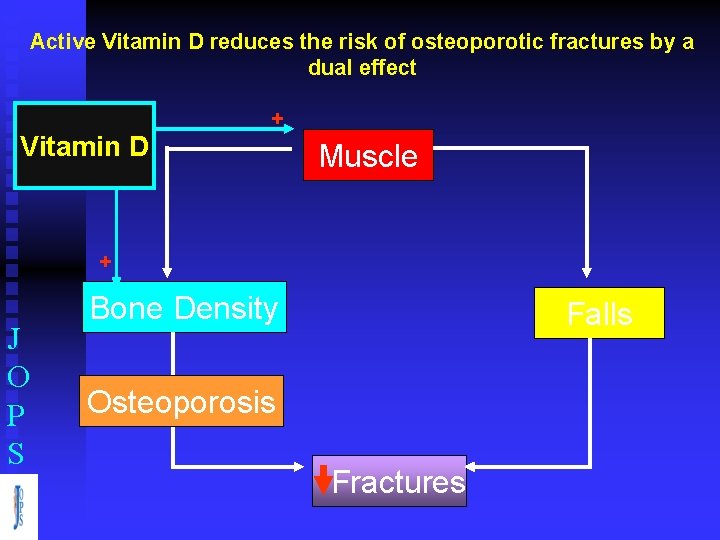
Active Vitamin D reduces the risk of osteoporotic fractures by a dual effect Vitamin D + Muscle + J O P S Bone Density Falls Osteoporosis Fractures
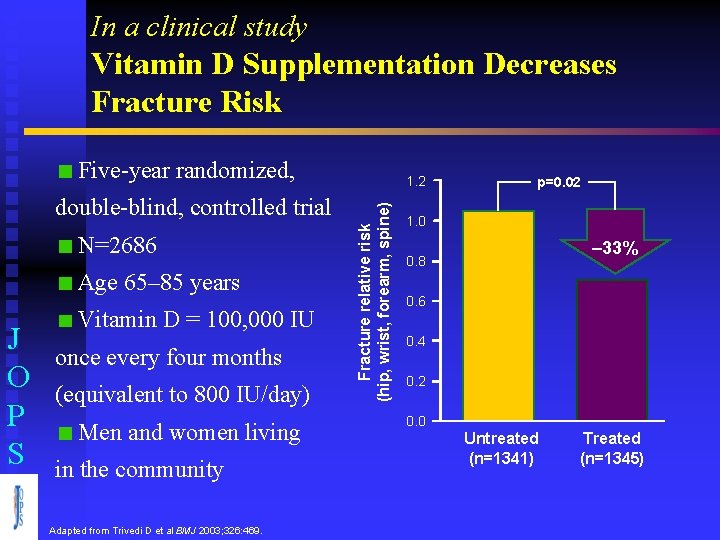
In a clinical study Vitamin D Supplementation Decreases Fracture Risk Five-year randomized, N=2686 Age 65– 85 years J O P S Vitamin D = 100, 000 IU once every four months (equivalent to 800 IU/day) Men and women living in the community Adapted from Trivedi D et al BMJ 2003; 326: 469. Fracture relative risk (hip, wrist, forearm, spine) double-blind, controlled trial 1. 2 p=0. 02 1. 0 – 33% 0. 8 0. 6 0. 4 0. 2 0. 0 Untreated (n=1341) Treated (n=1345)
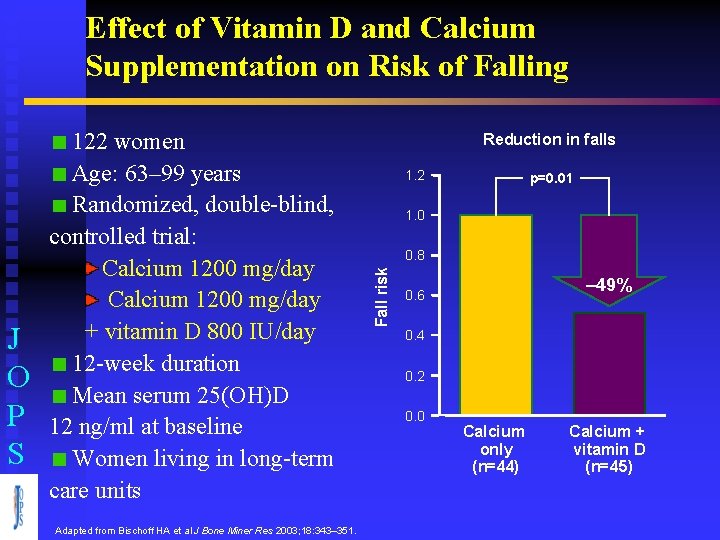
Effect of Vitamin D and Calcium Supplementation on Risk of Falling Adapted from Bischoff HA et al J Bone Miner Res 2003; 18: 343– 351. Reduction in falls 1. 2 p=0. 01 1. 0 0. 8 Fall risk J O P S 122 women Age: 63– 99 years Randomized, double-blind, controlled trial: Calcium 1200 mg/day + vitamin D 800 IU/day 12 -week duration Mean serum 25(OH)D 12 ng/ml at baseline Women living in long-term care units – 49% 0. 6 0. 4 0. 2 0. 0 Calcium only (n=44) Calcium + vitamin D (n=45)
Summary I J O P S Vitamin D inadequacy is widespread in postmenopausal women Postmenopausal women have difficulty getting enough Vitamin D: Ø Formation and processing of vitamin D may be impaired Ø Exposure to sunlight may be limited Ø Dietary sources provide little vitamin D Ø Patient compliance with vitamin D supplementation is inconsistent
Summary II J O P S Vitamin D is essential for calcium absorption. Adequate calcium absorption prevents secondary hyperparathyroidism and limits bone resorption Vitamin D supplementation has been shown to reduce the risk of fracture and falls and improves lower extremity function in the elderly Vitamin optimize antiresorptive drugs efficacy specially Bisphonates
- Slides: 28