Why Not Home Decreasing SNF Utilization and Optimizing
- Slides: 29
“Why Not Home? ” Decreasing SNF Utilization and Optimizing Patient-Centric Care DOUGLAS HIRT, ATC, SPT
Presentation Objectives Identify the “WHY” for “Why Not Home” Implications for therapy team Describe the process of identifying appropriate patients Application: case scenarios (discussion) Discuss how to incorporate Why Not Home into workflow
Why Not Home? Goal: Get appropriate patients home instead of a skilled nursing facility Why? ◦ Over utilization of skilled nursing facilities ◦ Increased spending has not led to improved outcomes for patients ◦ Institutional goal: Decrease SNF utilization by 8% ◦ Benefits to the Patient ◦ Comfort of home ◦ Potential lower out-of-pocket costs ◦ Safety ◦ Inconsistent levels of care, increased risk of infection associated with skilled nursing facilities ◦ Transition to home without readmission
Implications for the Therapy Team Thorough Evaluation Identify “WNH” patients Daily treatment sessions for patients identified as WNH Caregiver training Communication with medical team
It Starts with the Evaluation! Identifying barriers ◦ PLOF ◦ What was it? ◦ How close is the patient to their baseline? ◦ When was it? ◦ Home environment ◦ Barriers/facilitators ◦ Modification possible? ◦ Social Support ◦ Ability and availability
It Starts with the Evaluation! Can barriers be bridged with…? ◦ ◦ Focused treatment sessions on limitations Utilization of caregiver training Safe return home with continued services at home or in the outpatient setting Resources/DME recommendations
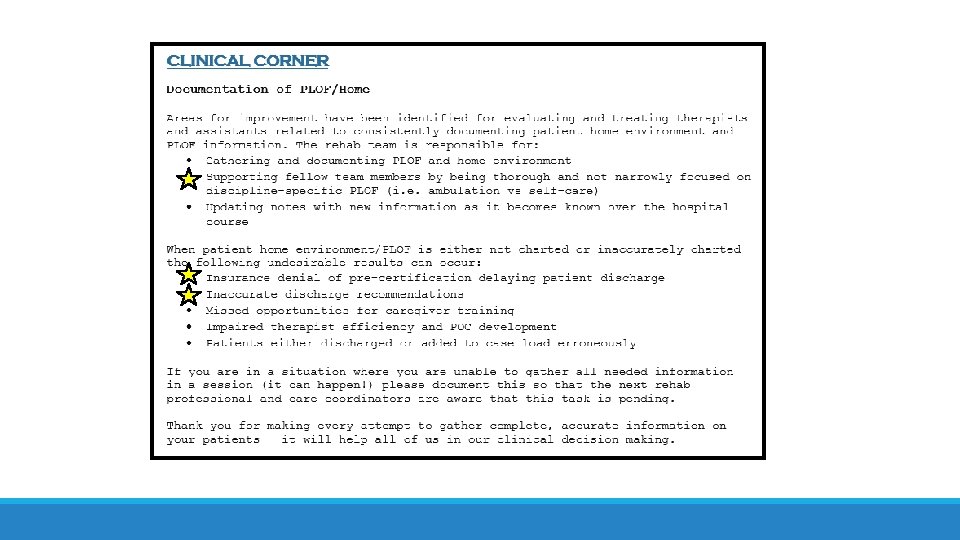
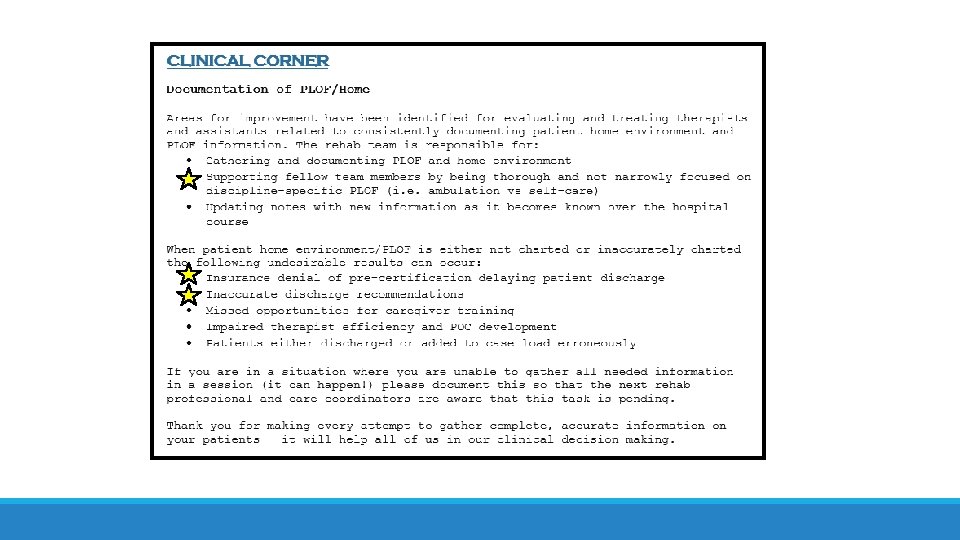
It Starts with the Evaluation! Thorough evaluation Supported by management: Gigi’s email – “October IP Rehab Newsletter” ◦ See next slide
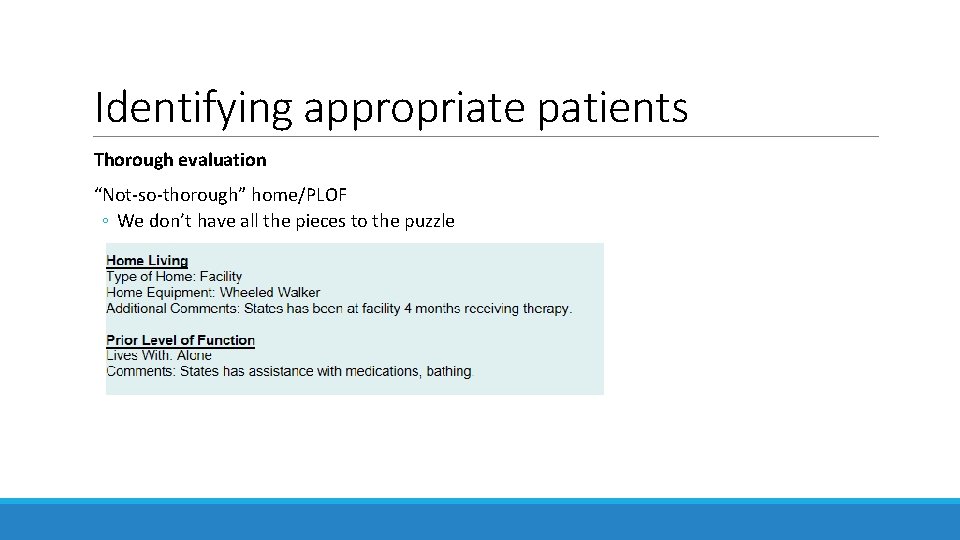
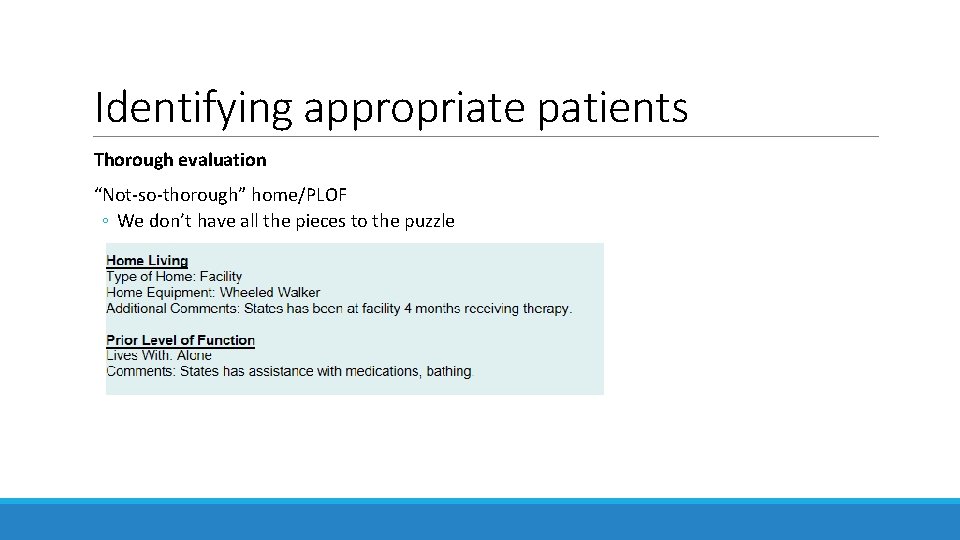
Identifying appropriate patients Thorough evaluation “Not-so-thorough” home/PLOF ◦ We don’t have all the pieces to the puzzle
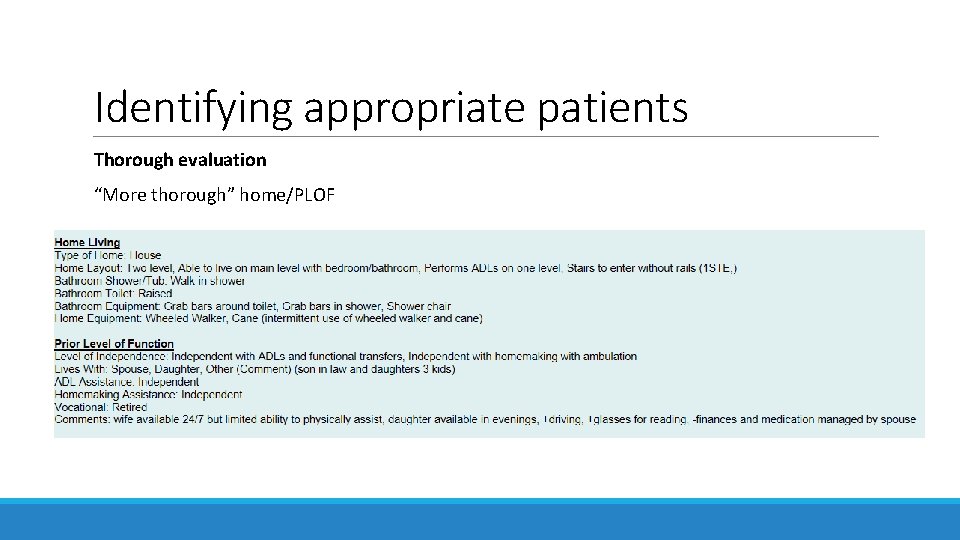
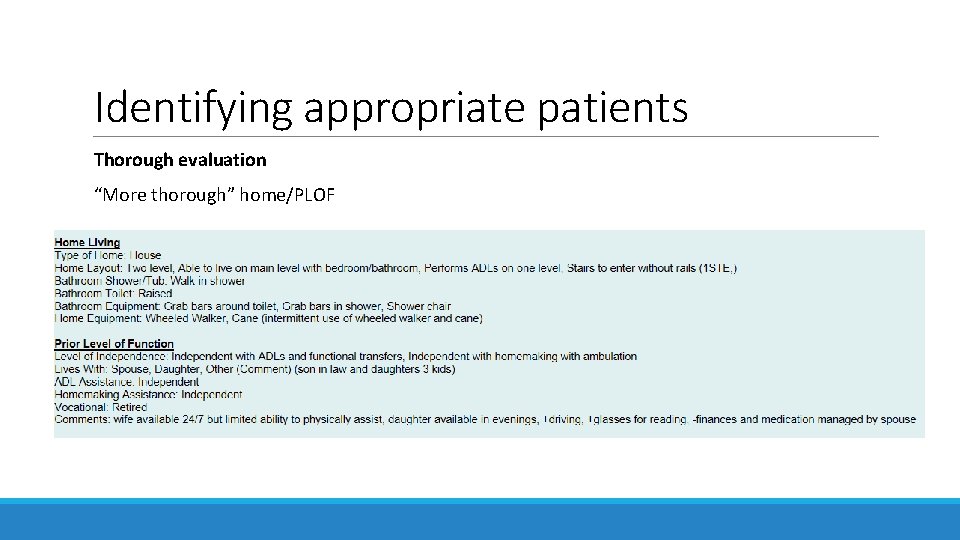
Identifying appropriate patients Thorough evaluation “More thorough” home/PLOF
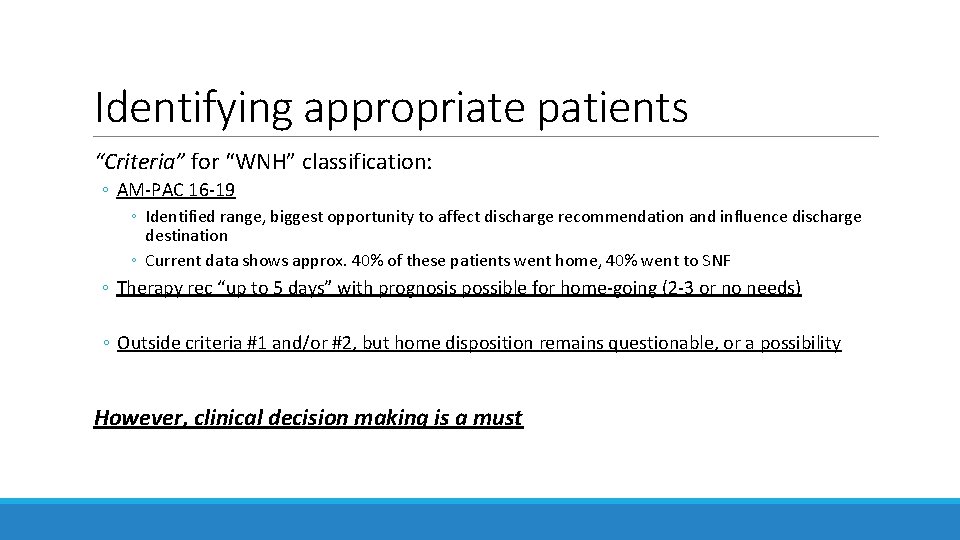
Identifying appropriate patients “Criteria” for “WNH” classification: ◦ AM-PAC 16 -19 ◦ Identified range, biggest opportunity to affect discharge recommendation and influence discharge destination ◦ Current data shows approx. 40% of these patients went home, 40% went to SNF ◦ Therapy rec “up to 5 days” with prognosis possible for home-going (2 -3 or no needs) ◦ Outside criteria #1 and/or #2, but home disposition remains questionable, or a possibility However, clinical decision making is a must
Identifying appropriate patients Other factors to consider for “WNH” classification include: Patients outside AM-PAC 16 -19 ◦ Does not automatically exclude patients from WNH Patient has need for SNF, but patient refuses or pre-certification is denied Presence of a caregiver ◦ Very helpful, but not essential
Identifying appropriate patients Patients who are NOT “WNH”: ◦ AM-PAC 16 -19 but… ◦ Therapy rec home-going, patient agreeable, no overt safety concerns (or concerns have been addressed) ◦ Therapy rec consistent for SNF/IPR, patient agreeable, patient not safe/appropriate for home-going ◦ In both scenarios there is plan and discharge is not questionable ◦ AM-PAC outside 16 -19 and patient not appropriate for home-going, and/or from facility ◦ Patient to return to facility ◦ Facility placement certainty ◦ Patients who were identified as “WNH”, but no longer meet criteria ◦ Remove from “WNH” ◦ If home going is no longer uncertain and does not meet criteria, remove them from the list!
Daily Treatment Sessions Increased frequency of interventions ◦ QD frequency ◦ Potentially BID if appropriate (i. e. D/C plans change mid-day, now patient going home) ◦ If at some point patient no longer meets “WNH” criteria → change their acute frequency Increased attention on patient-specific needs, functional barriers, safety ◦ Extended session if needed ◦ Education for home-going (strategies, energy conservation, timing of daily activities, etc. ) ◦ WNH is to cause change that will allow patients to go home
Caregiver Training EARLY AND OFTEN ◦ Upon evaluation if possible Areas to address determined based on patient needs/environmental barriers Communication with patient and medical team ◦ “Who is in charge of scheduling this? ” – more to come on this!
Communication with Medical Team Services after discharge DME needs Change in status ◦ Progress/decline Unified message/target ◦ Patient-centric, patient/caregiver must be involved ◦ Therapy, UMCC, attending ◦ Physician to reinforce message/plan to patient Everyone must be on the same page ◦ Not necessarily same rec, but unified awareness and efforts
Case Scenario #1 70 year old male, encephalopathy after leaving SNF (“AMA”), presented back to hospital Evaluation: ◦ ◦ Questionable historian Complex environment/support Prior AM-PAC (24)*; Current AM-PAC (17) Initial rec “Up to 5” What do we need to clarify? ◦ Environment ◦ PLOF Contact family (daughter) in order to clarify
Case Scenario #1 Patient questionable historian. Student PT called daughter for home info/PLOF. ◦ Determined to be complex home environment/support, "not safe" ◦ Daughter states patient to move in with her, new home info gathered per D/C plan ◦ Stairs primary safety barrier Interventions: ◦ Patient seen 3 days in a row, BID on last day with caregiver training (CGT) for transfers, gait, stairs ◦ During CGT identified 1+1 STE, with opportunity to educate/perform on-the-spot training for navigation with wheeled walker Outcome: Patient went home with daughter who felt more confident in ability to provide assistance for patient
Case Scenario #2 72 yo female; admit for increased fatigue, SOB, cough, chronic supplemental O 2 Evaluation: ◦ Lives with spouse ◦ Spouse physically able to assist ◦ Available 24/7 ◦ Assisted living, receives assist from facility staff, personal care assistant each morning ◦ 1 level ◦ 0 STE, accessible via DME has wheeled walker and manual wheelchair Prior AM-PAC (16); Current AM-PAC (15) Initial PT Rec: “Up to 5 (with hopeful progression)”
Case Scenario #2 Identified potential for home-going Setup caregiver training next day ◦ Physical caregiver training with spouse (1 session) ◦ Patient-specific session last day to address barriers: home setup, safety, energy conservation, strategies for increased daily activity Direct conversation with patient about current status
Case Scenario #2 In summary: Patient therapy rec "Up to 5" short duration ◦ Identified caregiver opportunity through thorough evaluation of support system and home-going barriers ◦ Engaged charge nurse on Friday to set up caregiver training for Saturday Safety issues/barriers thoroughly (intentionally) addressed; patient discharged home!
Case Scenario #3 69 year old male; admitted for R knee pain s/p fall Thorough Evaluation: ◦ Lives with spouse and daughter + son-in-law ◦ Digging deeper… spouse unable to physically assist ◦ Daughter only there in evenings and having surgery the following week ◦ 2 level home, able to live on main level, wheeled walker and cane ◦ How many steps to enter? ◦ One without a rail ◦ Prior AM-PAC (24); Current AM-PAC (15) Initial PT rec: “Up to 5 (with hopeful progression)”
Case Scenario #3 Identified potential for home-going after conversation with patient Primary barriers: bed mobility from flat bed, 1 STE (curb step) ◦ What can we do to potentially bridge this gap? ◦ Contacted UMCC as soon as possible to evaluate possibility of rent/obtaining a hospital bed for patient at home
Case Scenario #3 In summary: Thorough evaluation leading to determination of WNH, identify barriers, home-going potential, focused sessions on barriers and discussion with patient throughout session ◦ Early identification caregiver training opportunity ◦ Engaging charge nurse to setup caregiver training (care team all on board) Identified bed mobility as impeding barrier ◦ Problem solve through discussion with UMCC and attending physician ◦ Vouching for extra day and face-to-face for increased support/resources (hospital bed) Patient/family discussion, agreeable, patient to go home with HH services ◦ Engaging the family and patient, including them in decision making process
How to integrate WNH into your caseload Treatments: Focusing on patient limitations and caregiver training when applicable ◦ Communication with staff, scheduling caregiver training ◦ Education is billable time! Adding and removing patients after evaluation ◦ Have therapy recommendations changed? ◦ Caregiver training completed, patient improvement ◦ Is D/C home questionable? Is there a plan? ◦ If there is a plan, then patient is no longer WNH ◦ If there is not a plan or D/C is still questionable, still WNH Use of handoff (. rmhgenmedpthandoff, . rmhgenmedothandoff) ◦ Needs for caregiver training? ◦ Focus of sessions?
How to integrate WNH into your caseload Use of Standard Work flowsheet ◦ Coming soon! Percentage of WNH patients ◦ Last 2. 5 weeks: 20% of patients, highest daily percentage 44%
Conclusion ØWhy Not Home is a tool to decrease SNF utilization and increase positive outcomes for patients ØWe are responsible for identifying appropriate patients and communicating with the medical team ØThis begins with a thorough evaluation and continues with focused treatment sessions and caregiver training (when applicable) ØWhile Why Not Home patients are a focus, they are not the majority
References 1. Belagaje SR, Zander K, Thackeray L, et al. Disposition to home or acute rehabilitation is associated with a favorable clinical outcome. Journal of Neuro. Interventional Surgery 2015; 7: 322 -325. 2. Hakkarainen TW, Arbabi S, Willis MM, Davidson GH, Flum DR. Outcomes of patients discharged to skilled nursing facilities after acute care hospitizations. Amer Surg. 2014; 263(2): 280 -285. 3. Zhu JM, Patel V, Shea JA, Neuman MD, Werner RM. Hospitals using bundled payment report reducing skilled nursing facility use and improving care integration. Health Affairs. 2018; 37(8): 1282 -1289. 4. Jette DU, Stilphen M, Ranganathan VK, Passek SD, Frost FS, Jette AM. AM-PAC “ 6 -Clicks” functional assessment scores predict acute care hospital discharge destination. Amer Phys Ther Assoc Journal. 2014; 94(9): 1252 -1261. 5. Peiris CL, Taylor NF, Shields N. Extra physical therapy reduces patient length of stay and improves functional outcomes. Arch Phys Med Rehabil. 2011; 92: 1490 -1500. 6. Johnson JK, Pierson J, Noren CS, La. Stayo PC, Marcus RL. AM-PAC “ 6 -Clicks”: Implementation and potention usefulness in a university health system. Acute Care Critical Edge Phys Ther. Post num: 1027.
Questions? “BE THE BAR that others strive towards”