Whole Health 202 Implementing Whole Health in Clinical




































- Slides: 143
Whole Health 202: Implementing Whole Health in Clinical Care
Introductions for the Journey Together • • Your Name Your Role in VA What brings you joy? In 15 seconds or less! This Photo by Unknown Author is licensed under CC BY-NC-SA 2

Community Agreements for getting on the Rocket Ship üBe Present üBe Healthy üBe Curious üBe Honest üBe Respectful üCulture

Other important matters for getting on the Rocket Ship üSign in for CEUs üRest Rooms üSchedule
Recap What is Whole Health?
Recap What are the parts of the Whole Health System?
Recap What is it like to consider your own Whole Health?
Recap How is health created and supported?
Shift from “What’s the matter? ” to “What matters? ”
Agenda • What • Why – Unintended consequences of the current health care model (102 F) –Evidence • How – 1: 1 (clinician and patient) – With your teams – With your systems This Photo by Unknown Author is licensed under CC BY-SA-NC 10
The Evidence • The Evidence – Patient Centered Care – Whole Person Care – Patient Engagement – Personal Health Planning This Photo by Unknown Author is licensed under CC BY-SA-NC 11

Systematic Review: Patient Experience • 55 studies, >80, 000 pts • Consistent associations – Improved patient safety – Improved adherence – Improved clinical outcomes – Decreased resource utilization Doyle, doi. org/10. 1136/bmjopen-2012 -001570. 12
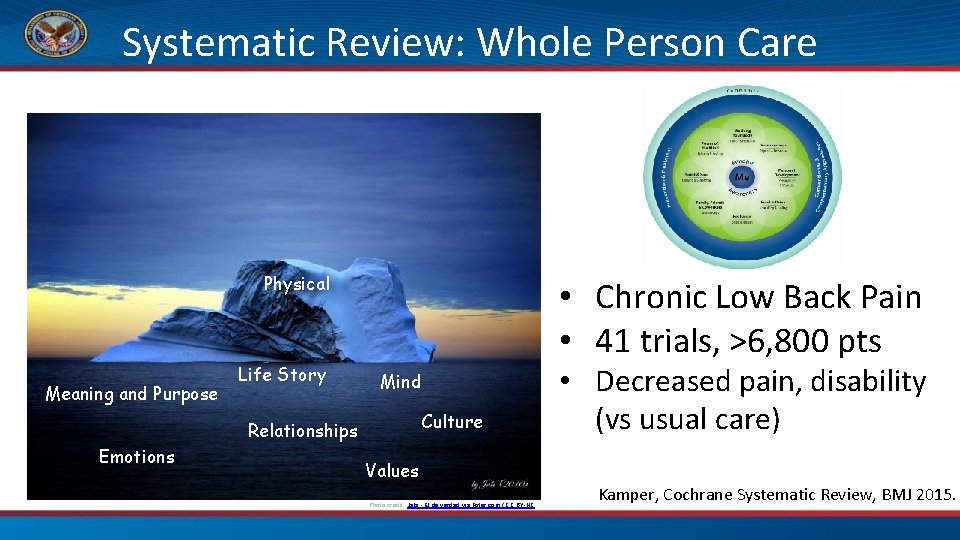
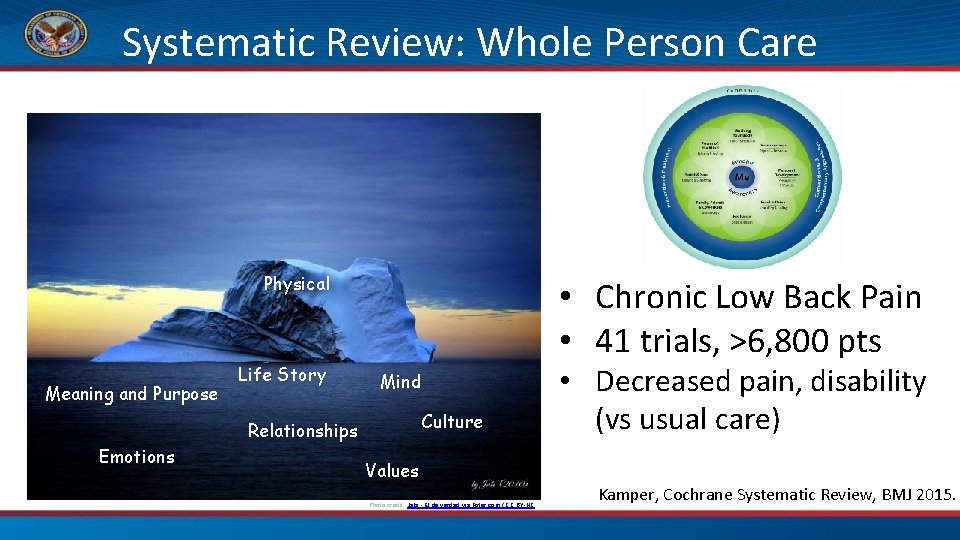
Systematic Review: Whole Person Care Physical Meaning and Purpose Life Story • Chronic Low Back Pain • 41 trials, >6, 800 pts Mind Culture Relationships Emotions • Decreased pain, disability (vs usual care) Values Photo credit: Jabi - El de verdad via Foter. com / CC BY-NC Kamper, Cochrane Systematic Review, BMJ 2015.
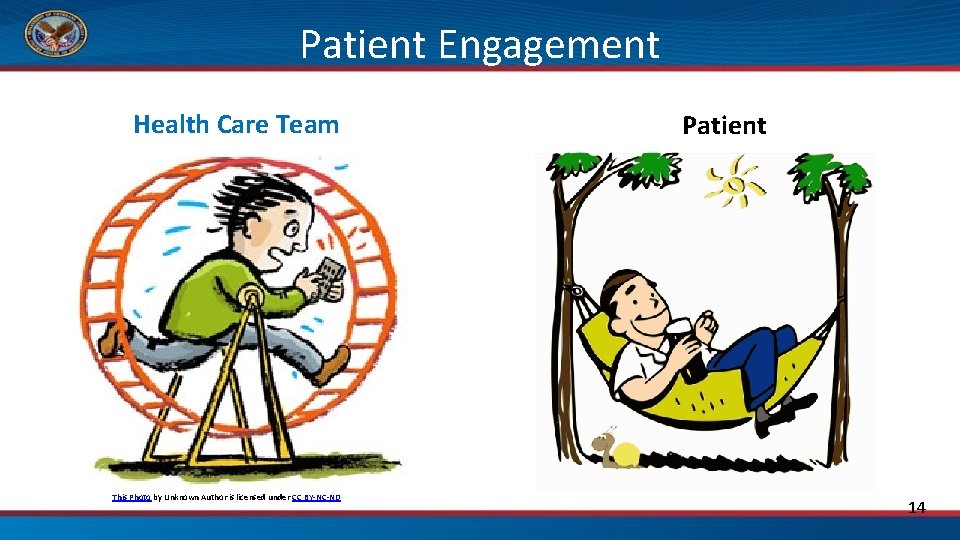
Patient Engagement Health Care Team This Photo by Unknown Author is licensed under CC BY-NC-ND Patient 14
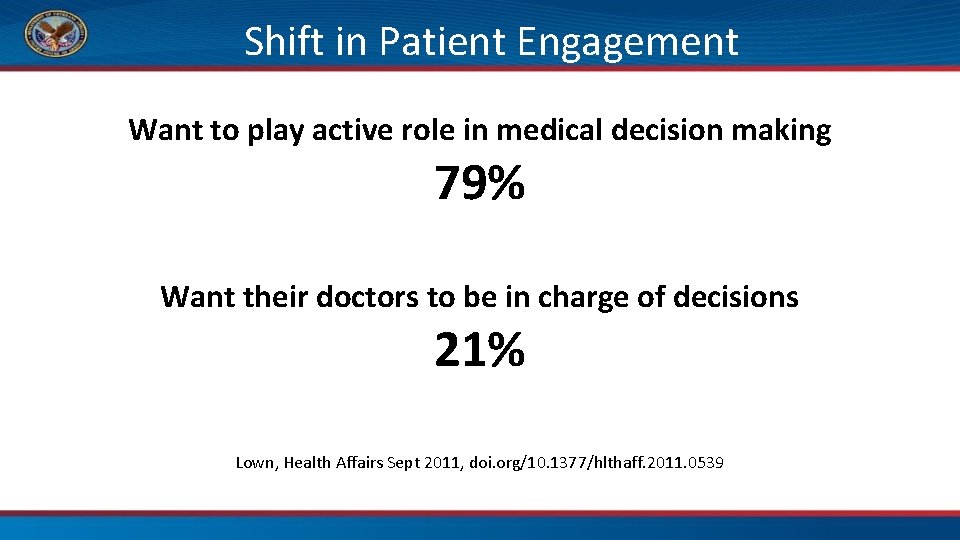
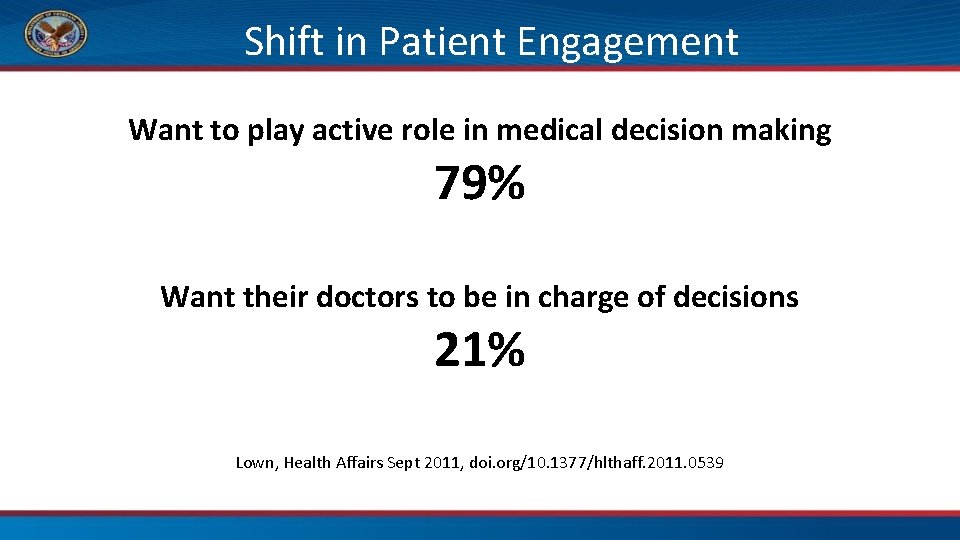
Shift in Patient Engagement Want to play active role in medical decision making 79% Want their doctors to be in charge of decisions 21% Lown, Health Affairs Sept 2011, doi. org/10. 1377/hlthaff. 2011. 0539
Patient Engagement • Understanding the importance of an active role in one’s own healthcare • Knowledge, skills and confidence to manage health • Using these to engage in health-promoting behaviors Simmons, Genome Medicine 2014, doi. org/10. 1186/gm 533. 16.
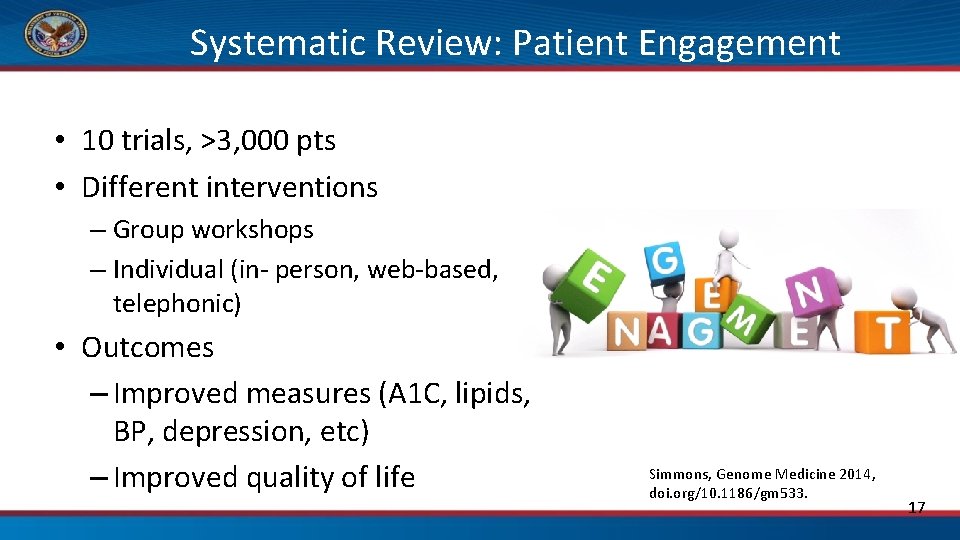
Systematic Review: Patient Engagement • 10 trials, >3, 000 pts • Different interventions – Group workshops – Individual (in- person, web-based, telephonic) • Outcomes – Improved measures (A 1 C, lipids, BP, depression, etc) – Improved quality of life Simmons, Genome Medicine 2014, doi. org/10. 1186/gm 533. 17
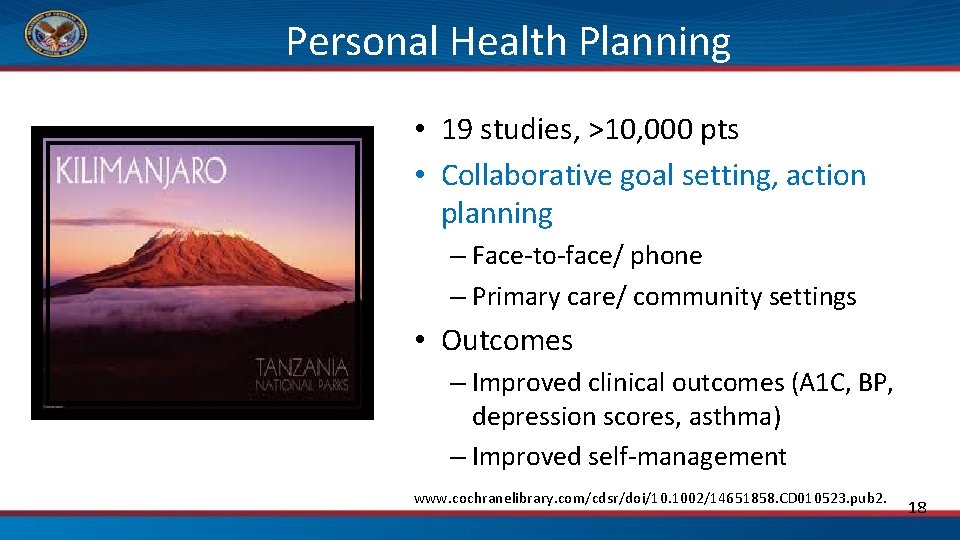
Personal Health Planning • 19 studies, >10, 000 pts • Collaborative goal setting, action planning – Face-to-face/ phone – Primary care/ community settings • Outcomes – Improved clinical outcomes (A 1 C, BP, depression scores, asthma) – Improved self-management www. cochranelibrary. com/cdsr/doi/10. 1002/14651858. CD 010523. pub 2. 18
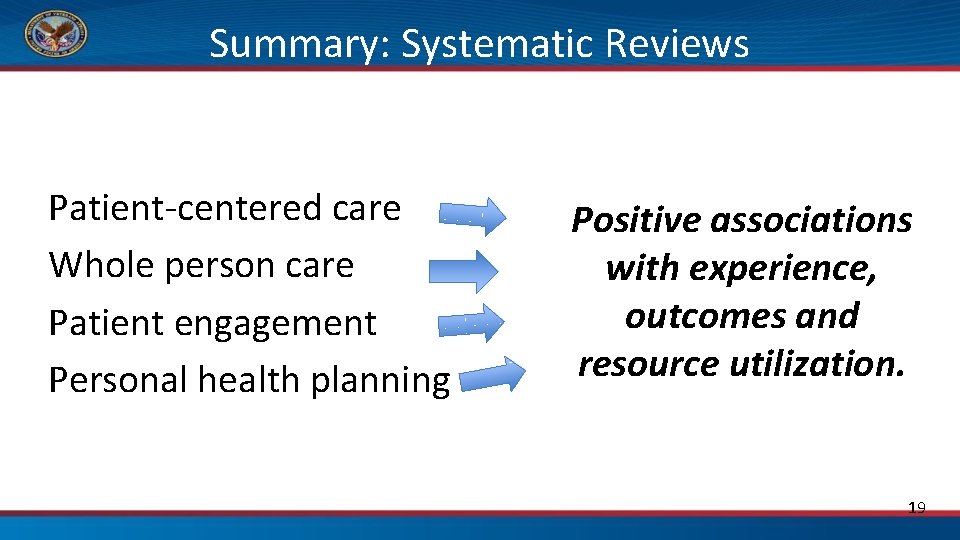
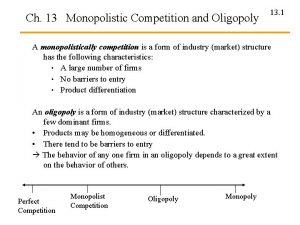
Summary: Systematic Reviews Patient-centered care Whole person care Patient engagement Personal health planning Positive associations with experience, outcomes and resource utilization. 19
What if we put this all together? (Patient-centered care) + (Whole person care) + (Patient engagement) + (Personal health planning) TBD (This is what is being evaluated at Flagships!) 20

Whole Health Education Website http: //wholehealth. wisc. edu
https: //wholehealth. wisc. edu/ Under “Get Started” 22
The Promise of Whole Health in VHA • • • VHA National Strategic Plan PACT Roadmap Chronic conditions Opioid crisis Mental Health/Suicide Prevention Employee Health and Well-being 23
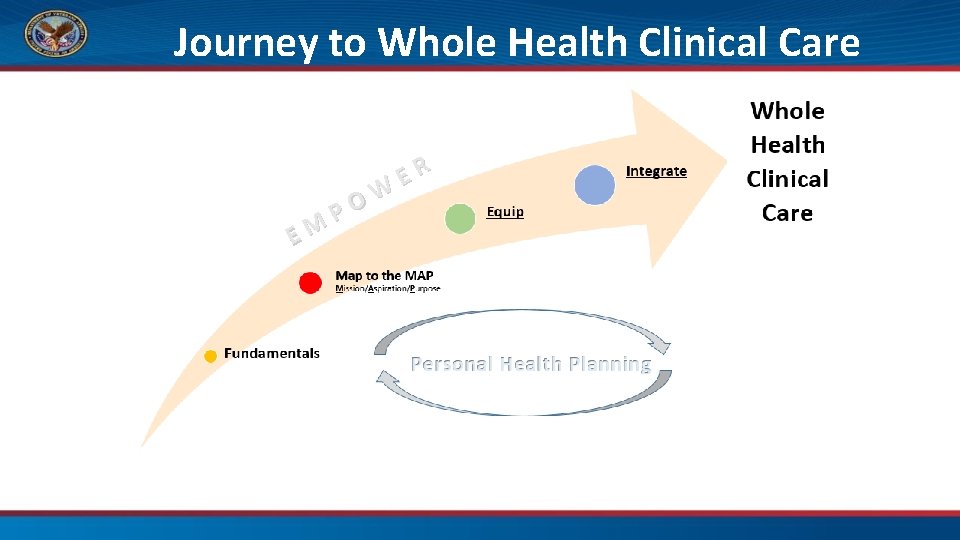
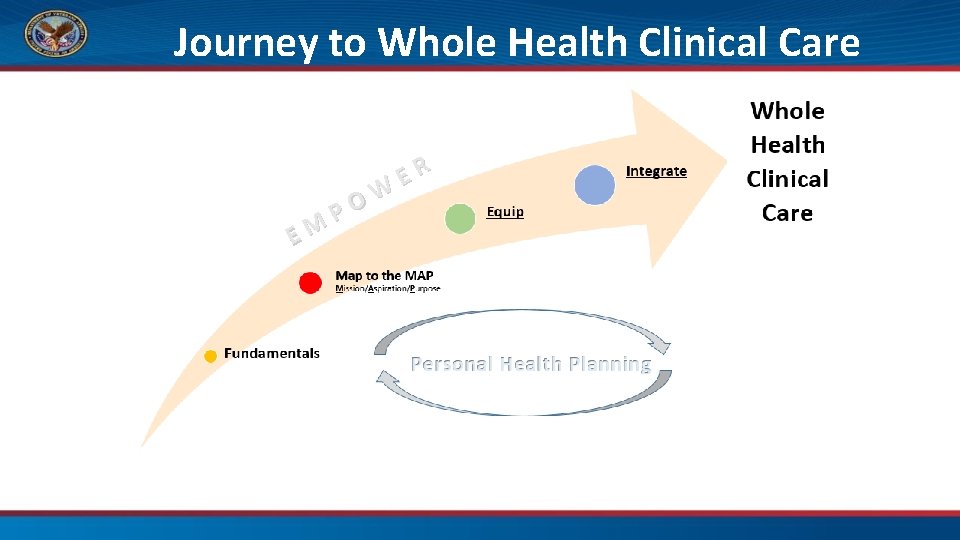
Journey to Whole Health Clinical Care EM W O P ER
WH Clinical Care Implementation • What is happening at our site? • How does this course fit in? • What happens next? 28

Agenda • What • Why – Unintended consequences of the current health care model – Evidence • How – 1: 1 (clinician and patient) – With your teams – With your systems This Photo by Unknown Author is licensed under CC BY-SA-NC 29
Your Patients Yesterday (or Last Week) • Tell your partner (1 minute each) – Who were your patients? – What were their problems? – What did you do for them? Ø What did you really do for them? (15 seconds each) 30
What is it that we do, really? 31

Race, anyone? • Creating time and space • First things first – Dealing with chest pain before asking what matters most! 32
“What Matters Today? ”: Agenda setting • ≈ 30% of Primary Care visits • Potentially increased patient & clinician satisfaction – Fewer “doorknob complaints” • Team-based approach likely best – Involving team members – Using a form or EHR to capture info Patient Educ Couns 2015 May; 99(5): 718 -23. JAMA Jan 1999 Jan 20; 281(3): 283 -7. BMJ 2006; 332: 1238 Annals of Family Medicine March/April 2017; 15 (2) 158 -161.

Agenda Setting: A Quick How-To 1. Solicit patient’s agenda – What are the most important things to you to cover today? 2. Reflect and summarize – Genuine interest (Mindful presence)
Agenda Setting: A Quick How-To 3. Probe further – What else? Anything else? – Is there something else? • SOME vs ANY- eliminated 78% of unmet concerns J Gen Intern Med. 2007 Oct; 22(10): 1429 -33. 4. Identify/communicate your agenda – If necessary, negotiate

What matters most? • For our time together today • In our lives • Negotiated agenda = Shared goals 36

Practice • With a partner, practice agenda-setting – Patient • Think of 3 -4 things you want to talk about. Consider making the last one on your list the “real” issue you are worried about – Clinician • Solicit your patient’s agenda • Reflect and summarize • Probe further • Identify and communicate your agenda to come up with a shared agenda 37
Debrief This Photo by Unknown Author is licensed under CC BY-SA 38
Now what? • Creating time and space to support healing and health – First things first • Power of you This Photo by Unknown Author is licensed under CC BY-NC-ND 39
BREAK 40
The Power of You
1: 1 with a Patient This Photo by Unknown Author is licensed under CC BY-NC-ND 42

Does Clinical Care ever feel like this? Right tool, anyone? This Photo by Unknown Author is licensed under CC BY-NC-ND This Photo by Unknown Author is licensed under CC BY-SA-NC 43
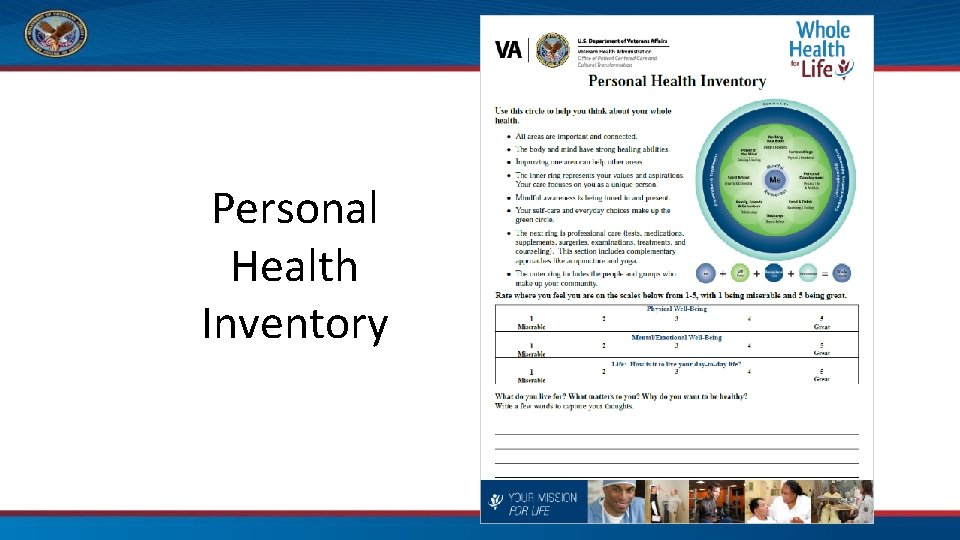
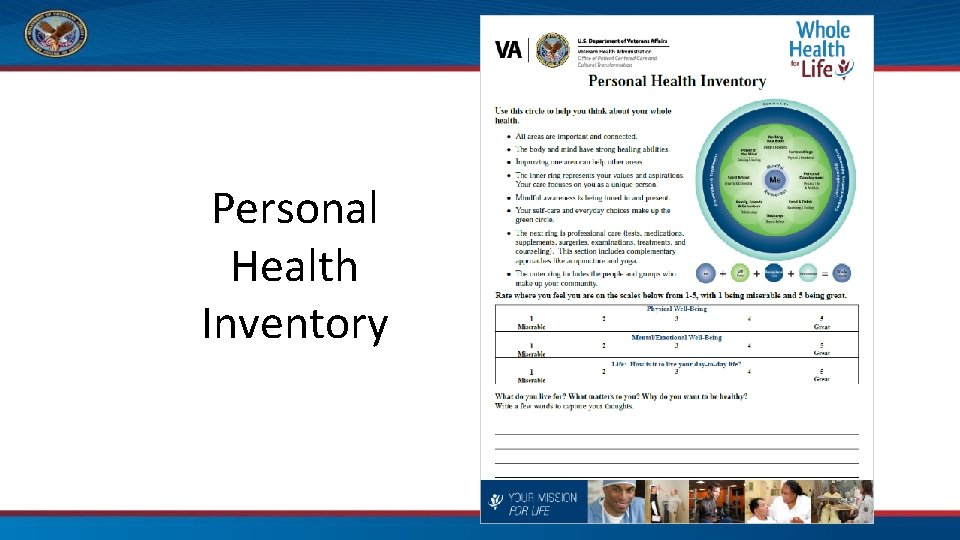
Personal Health Inventory
Whole Health Conversations • Demo (5 min) – Debrief • Your turn! Use the PHI as a “talking map” – In pairs, explore (5 min total each) • What matters most • The Circle- What stands out, Areas of strength, Areas to explore more • Possible next step(s) 45

Debrief • • What went well? What was hard? What surprised you? How might we use this with the “stuck” situations we listed? 46

Which statement gets the best response? Statement A “Your A 1 c is clear up to 10. That means your sugars have been really high for a while. Studies show this will put your heart, retinas, nerves, and kidneys at risk. ” Statement B “I know your goal is to dance at your granddaughter’s wedding. Keeping your sugars in a good place will help your heart, legs, and the rest of your body be up for it! And it will keep that A 1 c number down, too. ”
Developing a Personal Mission and Creating a Vision One Way to Start a Conversation • What’s the matter? A Different Way to Start a Conversation • What matters most? • What concerns you about your health? • What do you want your health for? • What are your problems today? • What is your vision of your best possible health?
Shared Goals “I know your goal is to climb Mt. Kilimanjaro. Keeping your sugars in a good place will help your heart, legs, and the rest of your body be up for it! And it will keep that A 1 c number down, too. ” 49
Shared Goals “I know you are worried about lowering your pain medications. I also know you want to keep doing things you enjoy, like walking outdoors with your wife and your dog. Our goal is to help keep you walking with your family. Let’s talk about how we might do that together. ” 50
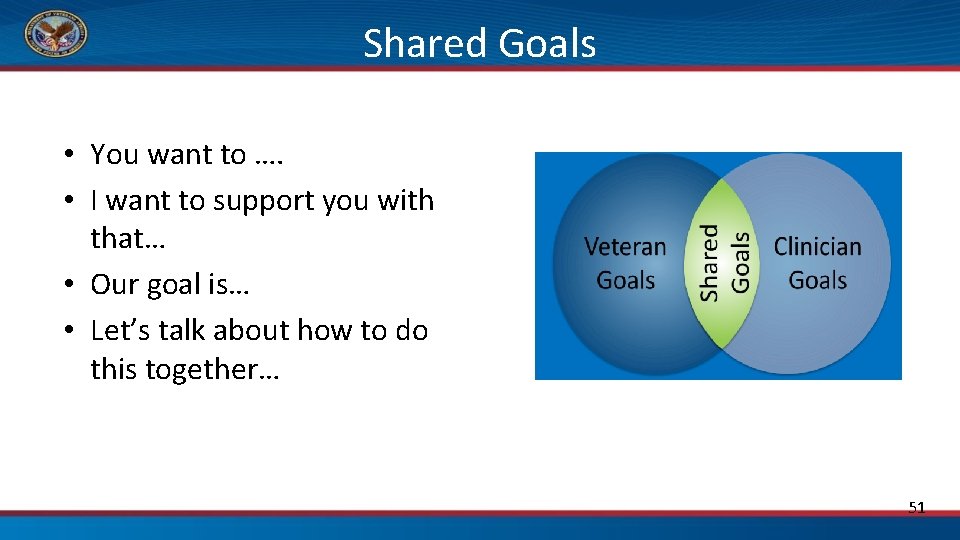
Shared Goals • You want to …. • I want to support you with that… • Our goal is… • Let’s talk about how to do this together… 51
We are on the same team. How else can we convey this? This Photo by Unknown Author is licensed under CC BY-NC-ND
Has this ever happened to you? Your patient has a highly specialized problem outside of your usual area of expertise, and wants your thoughts on how to proceed. Why does this happen? 53
NIH-Funded Empathy Research ü Good Doc ü “Standard” Doc ü No Doc

UW Cold Study: Perception of Perfect Empathy IL-8 No Visit Standard Neutrophils Enhanced No Visit Standard Enhanced Rakel, Hoeft, Barrett, et al. Fam Med. 2009; 41(7): 494 -501. Rakel, Barrett, Zhang, et al. Patient Ed & Counseling, 2011; 85: 390 -7.
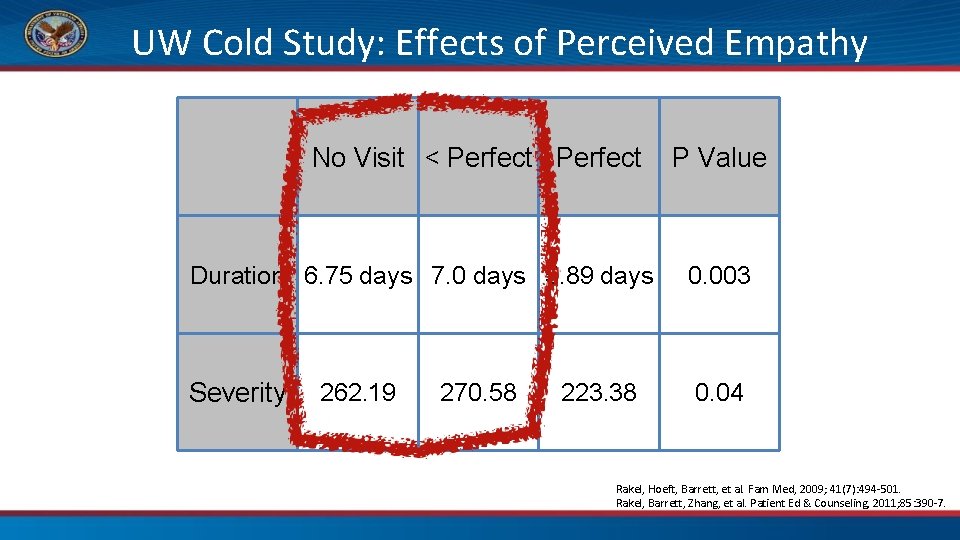
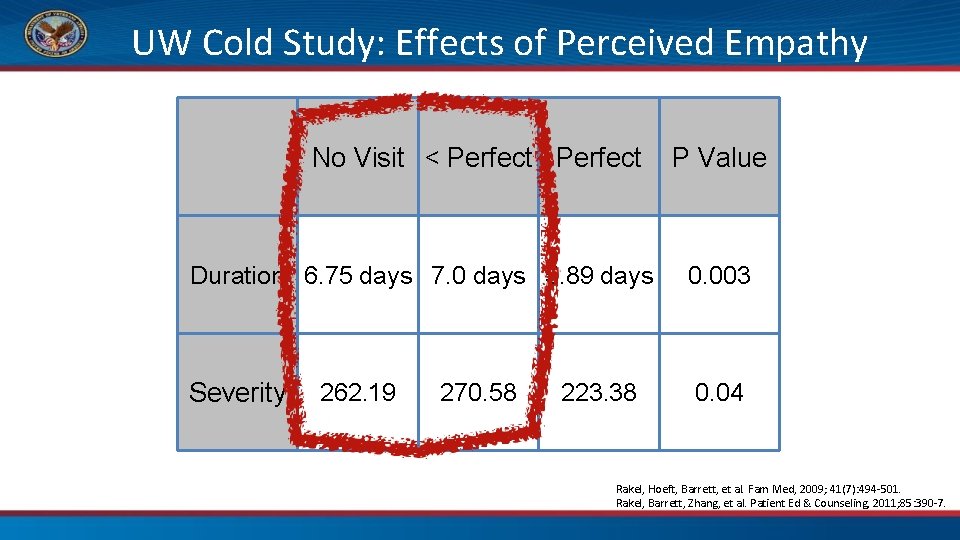
UW Cold Study: Effects of Perceived Empathy No Visit < Perfect P Value Duration 6. 75 days 7. 0 days 5. 89 days 0. 003 Severity 0. 04 262. 19 270. 58 223. 38 Rakel, Hoeft, Barrett, et al. Fam Med, 2009; 41(7): 494 -501. Rakel, Barrett, Zhang, et al. Patient Ed & Counseling, 2011; 85: 390 -7.
Generous Listening Attention is the rarest and purest form of generosity. 58
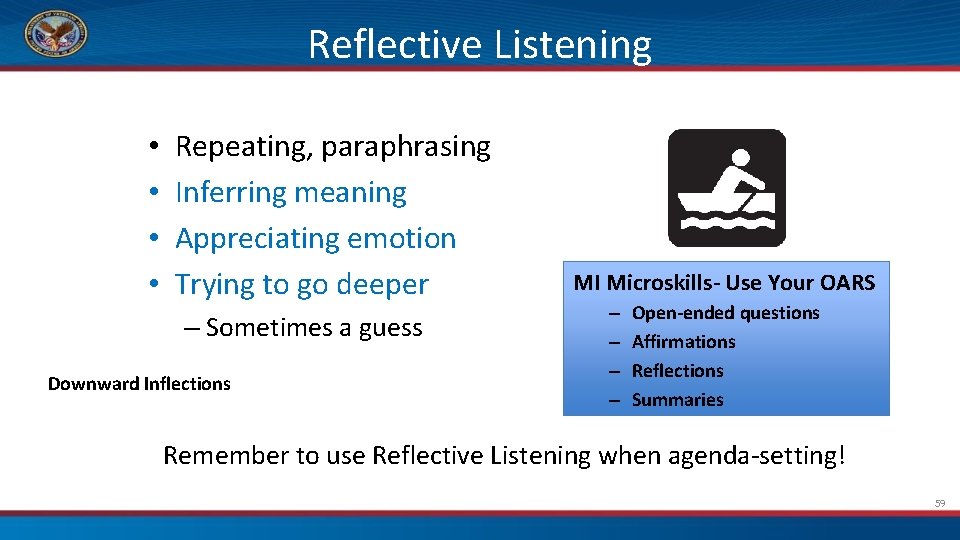
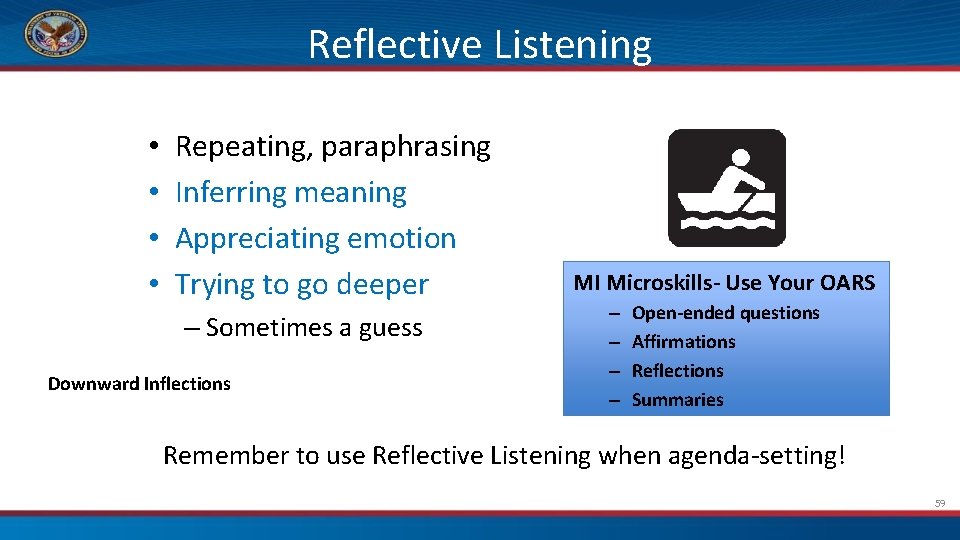
Reflective Listening • • Repeating, paraphrasing Inferring meaning Appreciating emotion Trying to go deeper – Sometimes a guess Downward Inflections MI Microskills- Use Your OARS – – Open-ended questions Affirmations Reflections Summaries Remember to use Reflective Listening when agenda-setting! 59
Reflective Listening • With a partner (1 min each) • Speaker- tell your partner one thing you like about yourself. • Listener- make reflective statements – nothing else – Try to get deeper – Speaker will respond only with one word at a time- “yes”, “no”, “maybe”, or “sometimes”. Downward Inflections 60
Discussion • What was it like to be the person making the reflections? • What was it like to be the person receiving the reflections? 61
Insight
Insight • 53 man with poorly controlled diabetes, depression, chronic pain I don’t have any mental health issues. I guess these might be related. Which of your patients might benefit from this type of “a-ha” moment?
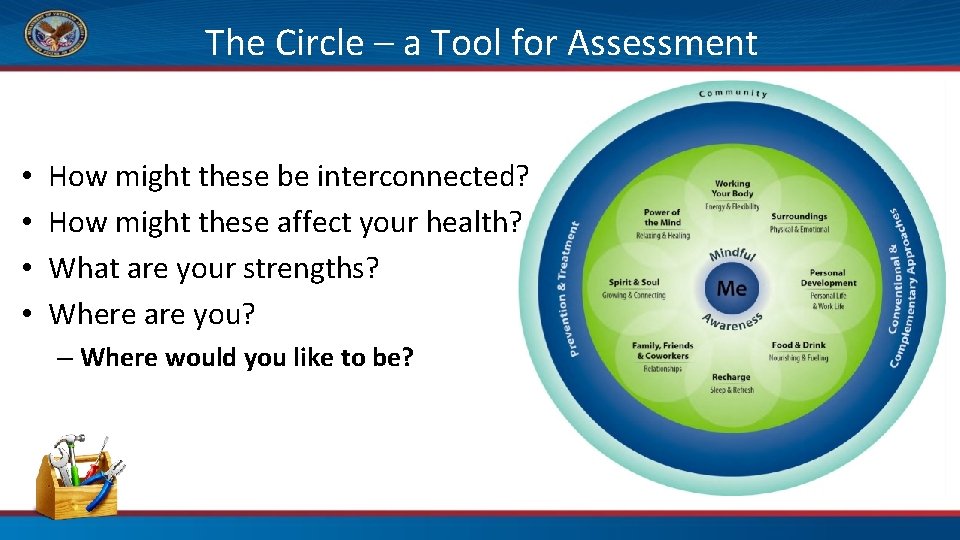
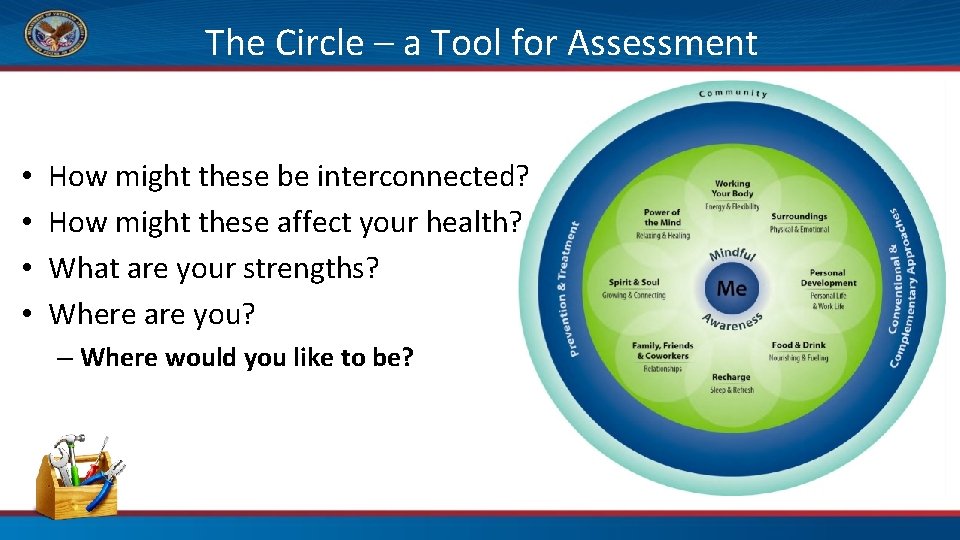
The Circle – a Tool for Assessment • • How might these be interconnected? How might these affect your health? What are your strengths? Where are you? – Where would you like to be?
Vitality Signs 93 yo man with metastatic cancer, recent admission for CHF • How do you rate your physical health (from 1 -5, 5 best)? – “ 4 - I know I have some issues but I still have all my limbs!” • How do you rate your emotional health? – “ 5 - I have a wonderful family!” • How do you rate your day to day life? – “ 4 - I am grateful for each day!” 65
Vitality Signs 34 yo man, former Marine, depressed with PTSD • How do you rate your physical health (from 1 -5, 5 best)? – “ 2 - As a Marine, I was in excellent physical condition. Now I’m not. ” • How do you rate your emotional health? – “ 3 - My PTSD symptoms are bad sometimes. ” • How do you rate your day to day life? – “ 3 –Depends on the day I guess. ” 66
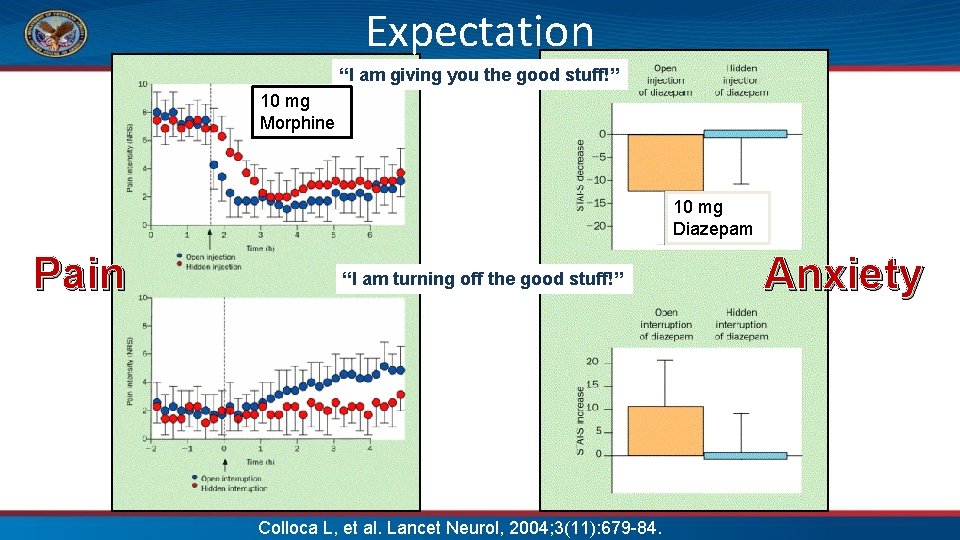
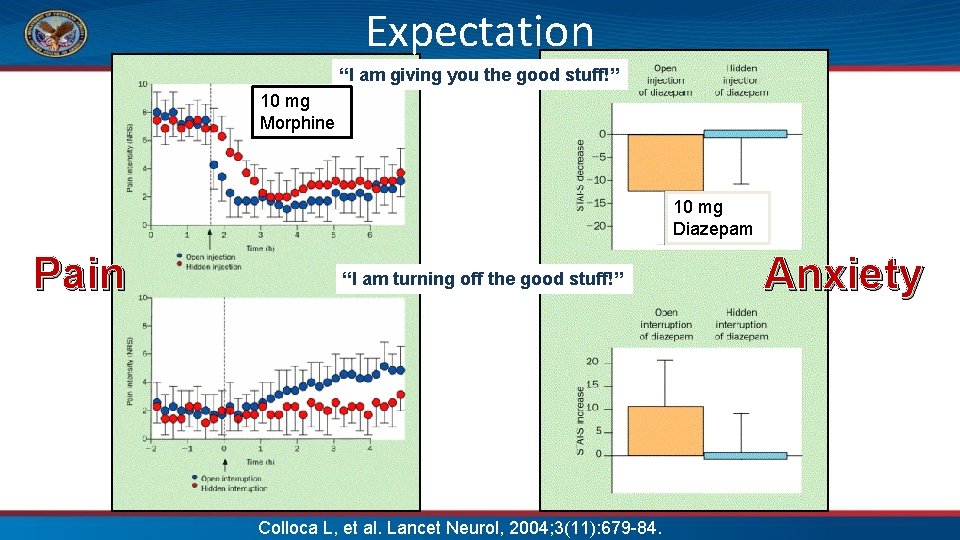
Expectation “I am giving you the good stuff!” 10 mg Morphine 10 mg Diazepam Pain “I am turning off the good stuff!” Colloca L, et al. Lancet Neurol, 2004; 3(11): 679 -84. Anxiety
Lack of Hope • Think of a patient who doesn’t seem to believe they can get better – What is it like to see this patient? – How might their expectations impact the outcome? – How about your expectations? • What about a patient who is hopeful? 68
Hope • 64 woman, morbid obesity, depression, chronic pain I have no areas of strength. I survived my divorce. I guess I’m stronger than I thought.

Empowerment Confidence: Building Hope and Possibility 70
Empowering and Equipping This Photo by Unknown Author is licensed under CC BY-SA-NC 71
Open Ended Questions for Goals • • • Where would you like to start? What is a reasonable next step? What appeals to you the most? What would you commit to? What else might you do? This Photo by Unknown Author is licensed under CC BY-NC-ND Sparkpeople. com
Effective Goals ØSMART Goals q Specific q Measurable q Action-oriented q Realistic q Time-bound This Photo by Unknown Author is licensed under CC BY-NC-ND 74
Assess and Address Barriers What might get in the way? What might help you overcome that barrier? What helped in the past? Would you like to hear some things that have worked for other people? • Now, what is your plan? • •

What else might be helpful? • Ask what might help • Set up for success – Referrals- create a Whole Health team – Resources- handouts, websites, etc – Skill-building • Follow up

Your New Toolbox • • • Engagement/Motivation The Big Picture Insight Hope Moving Forwards • Which is your favorite? • Which do you plan to try first? 77
Having Whole Health Conversations • Best therapeutic presence • PHI – As your Talking Map – Or use “back pocket” mini-tools prn • Explore – What matters most – The Circle- make sure “patient” decides where to focus – Possible next step(s), if ready 78
Never underestimate the power of your therapeutic presence!
BREAK 80

Professional Care: Complementary And Integrative Health (CIH)
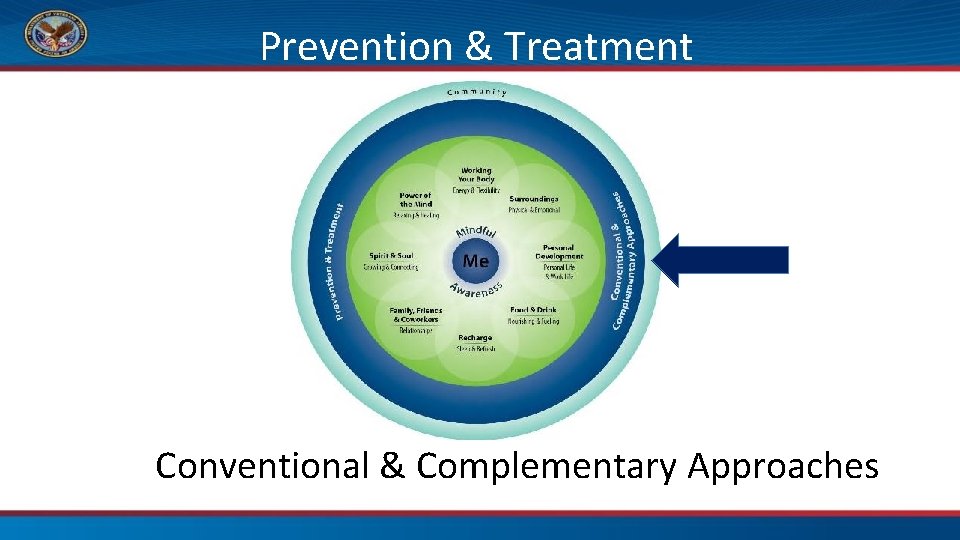
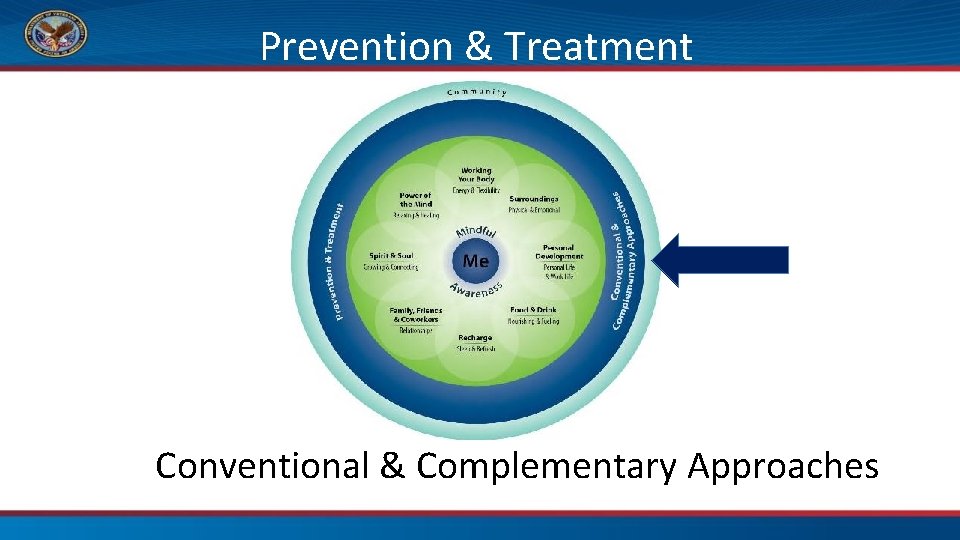
Prevention & Treatment Conventional & Complementary Approaches

Tai Chi & Qigong Na tur op ath y
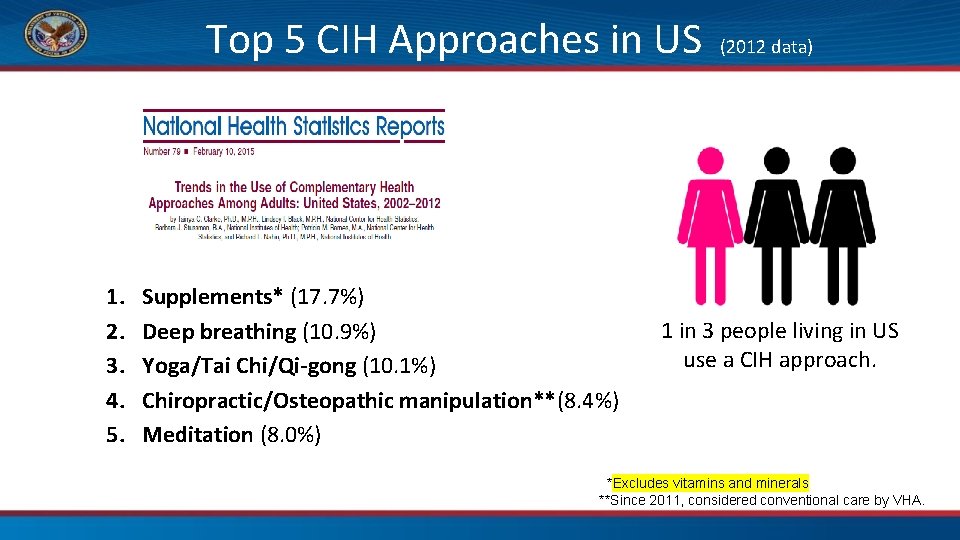
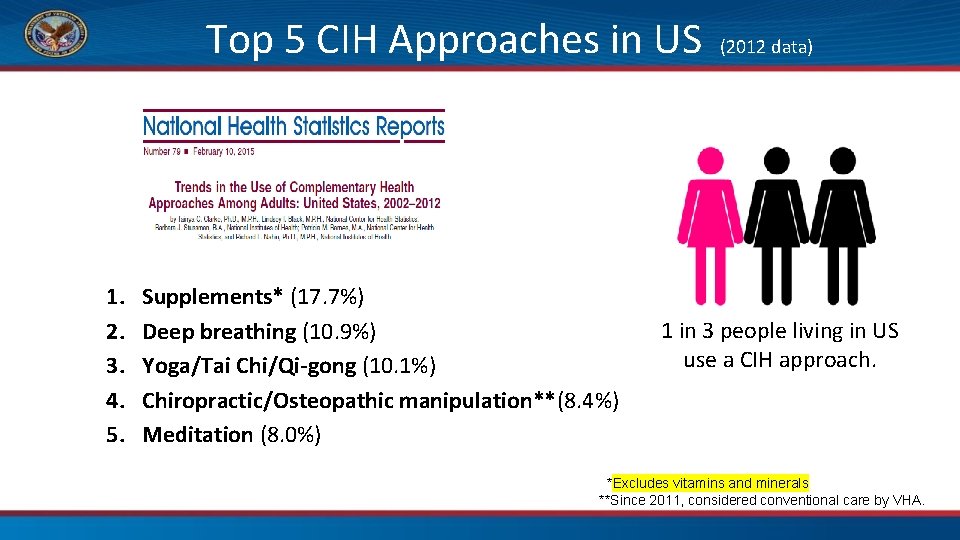
Top 5 CIH Approaches in US 1. 2. 3. 4. 5. Supplements* (17. 7%) Deep breathing (10. 9%) Yoga/Tai Chi/Qi-gong (10. 1%) Chiropractic/Osteopathic manipulation**(8. 4%) Meditation (8. 0%) (2012 data) 1 in 3 people living in US use a CIH approach. *Excludes vitamins and minerals **Since 2011, considered conventional care by VHA.
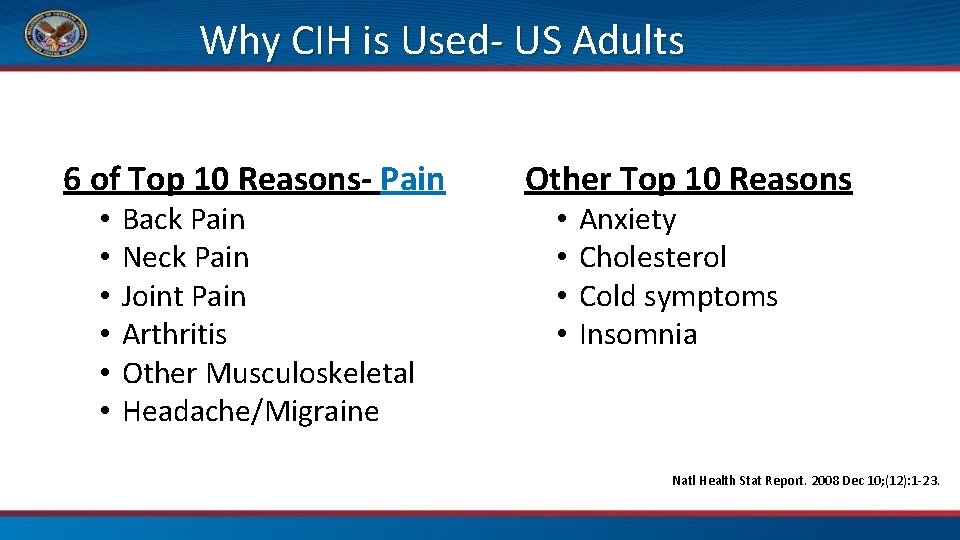
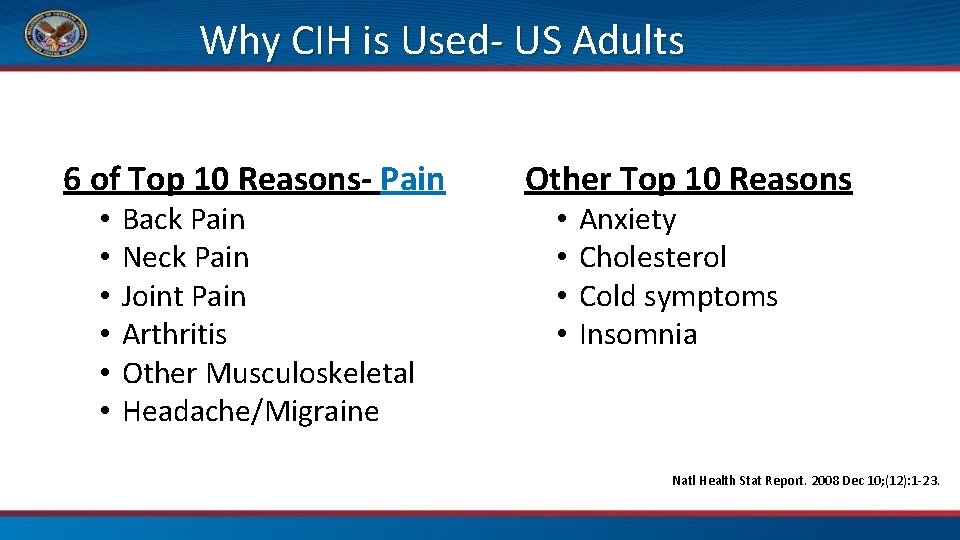
Why CIH is Used- US Adults 6 of Top 10 Reasons- Pain • • • Back Pain Neck Pain Joint Pain Arthritis Other Musculoskeletal Headache/Migraine Other Top 10 Reasons • • Anxiety Cholesterol Cold symptoms Insomnia Natl Health Stat Report. 2008 Dec 10; (12): 1 -23.
Most Common Conditions in VA for CIH Use 1. Stress 2. Anxiety 3. PTSD 4. Depression 5. Pain Healthcare Analysis & Information Group (HAIG) Report A Field Unit of the Office of Strategic Planning & Analysis

Considerations • Efficacy • Co$t • Harms • Opinions
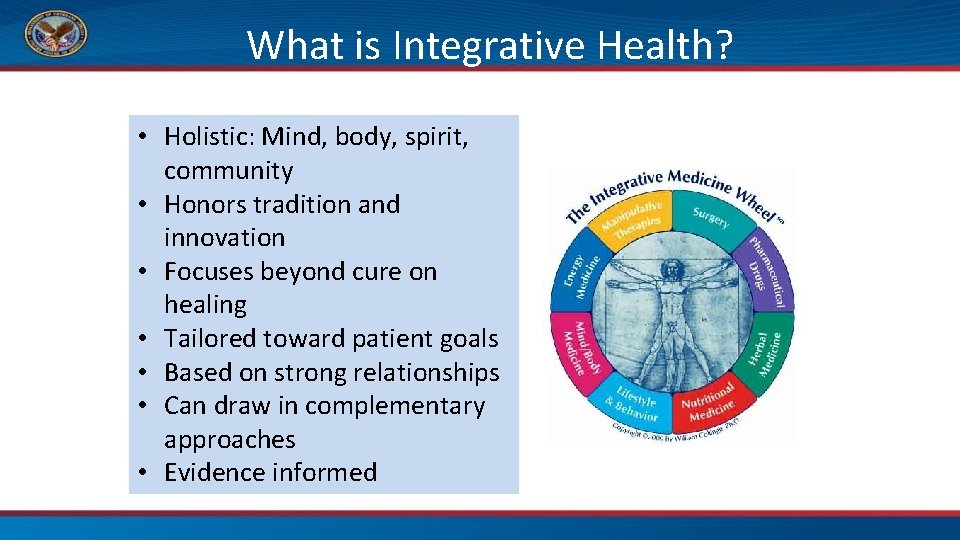
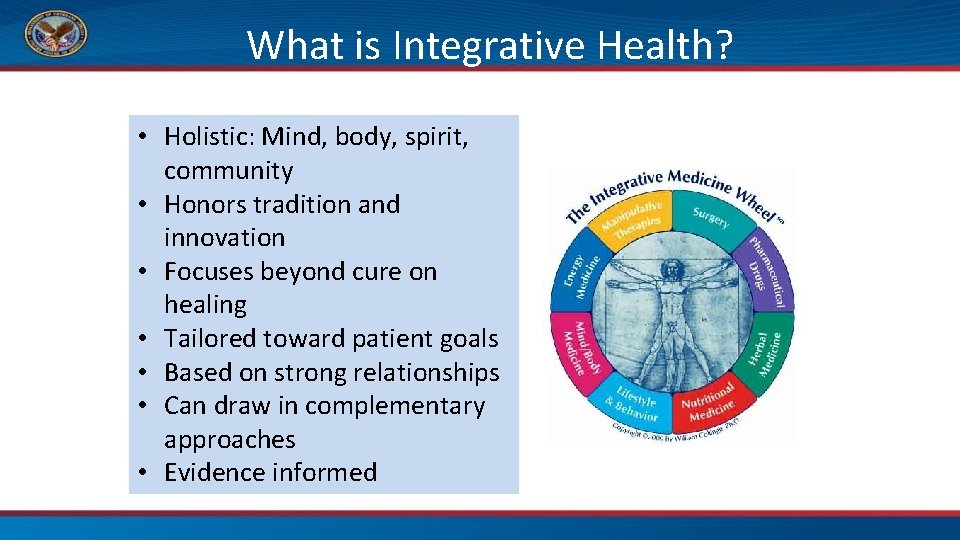
What is Integrative Health? • Holistic: Mind, body, spirit, community • Honors tradition and innovation • Focuses beyond cure on healing • Tailored toward patient goals • Based on strong relationships • Can draw in complementary approaches • Evidence informed
An Important Reminder Whole Health is inclusive of conventional clinical treatment and prevention, self-care strategies, and complementary practices.
“Find it, Fix it” and CIH therapies

Approved CIH Approaches- List 1 Promising/Potential benefit, Standard Benefits Package • • Acupuncture Meditation Tai Chi Yoga • • Massage for treatment Guided imagery Biofeedback Clinical hypnosis Note: Chiropractic care considered conventional in VA http: //vaww. infoshare. va. gov/sites/OPCC/Site. Pages/IHCC-Approved-CIH. aspx
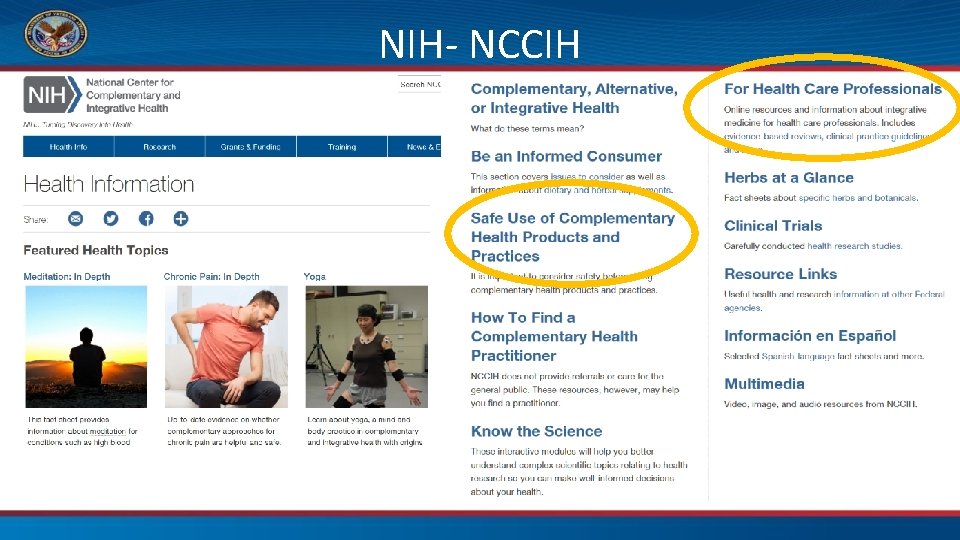
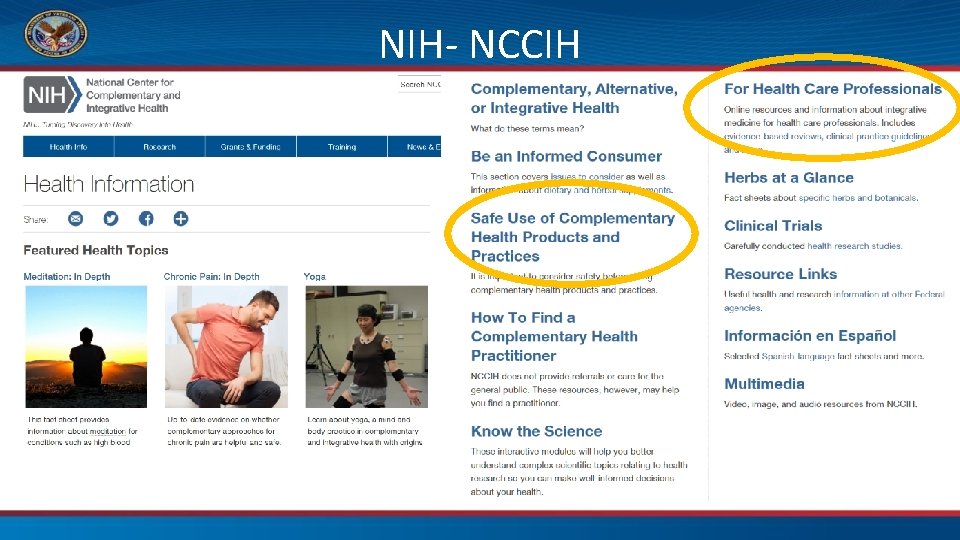
NIH- NCCIH

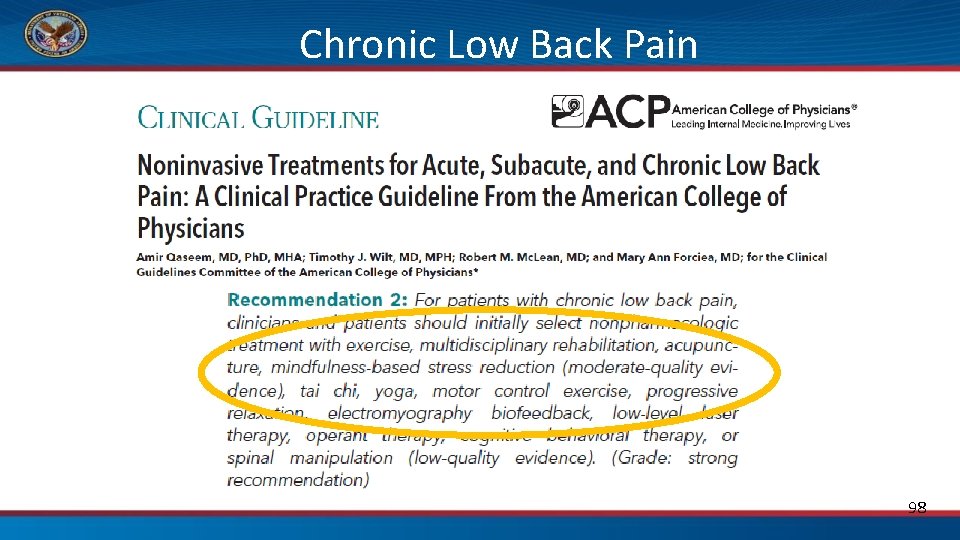
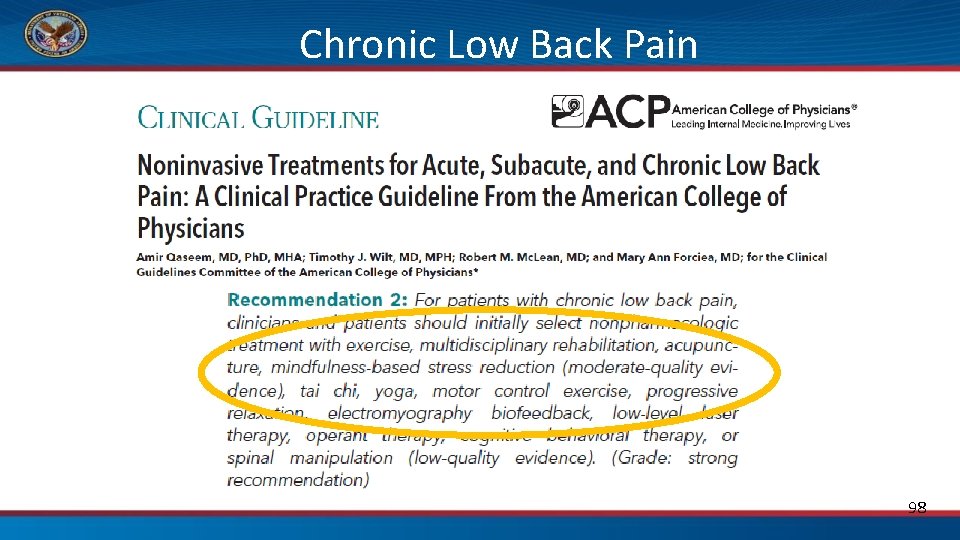
Chronic Low Back Pain 98
Talking with patients about CIH referrals • Collaboration with the care team • Framing in terms of self-care role – “Active” vs. “Passive” therapies • Managing expectations – National Guidance – Local considerations Supply Demand 99
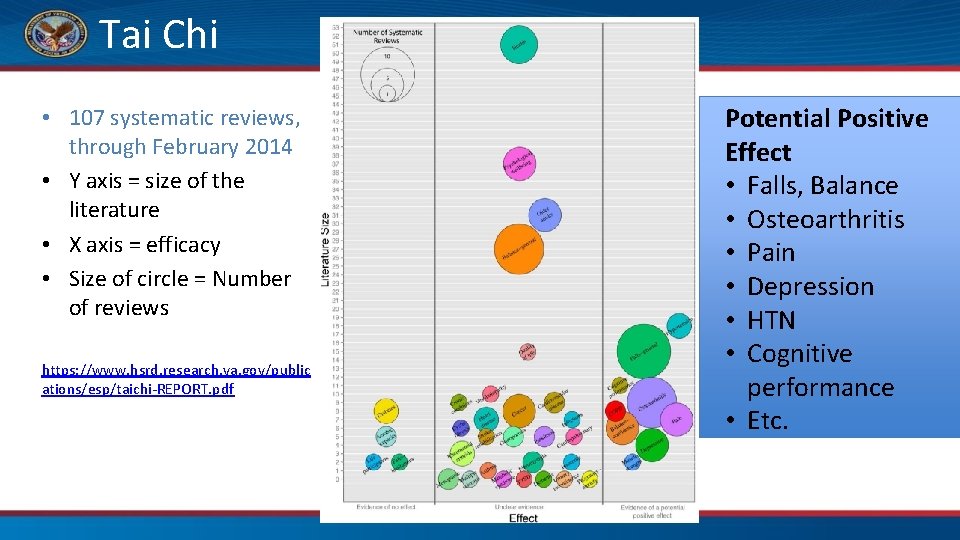
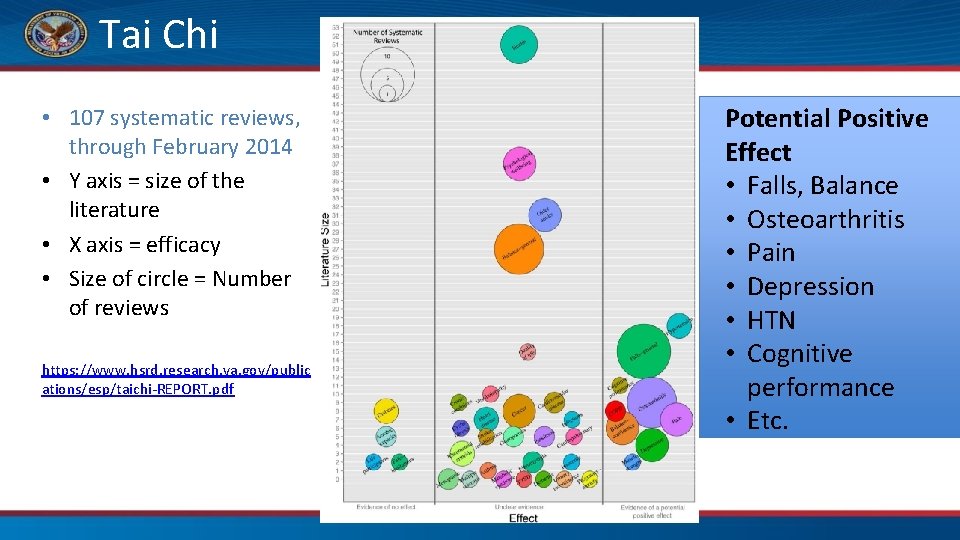
Tai Chi • 107 systematic reviews, through February 2014 • Y axis = size of the literature • X axis = efficacy • Size of circle = Number of reviews https: //www. hsrd. research. va. gov/public ations/esp/taichi-REPORT. pdf Potential Positive Effect • Falls, Balance • Osteoarthritis • Pain • Depression • HTN • Cognitive performance • Etc.
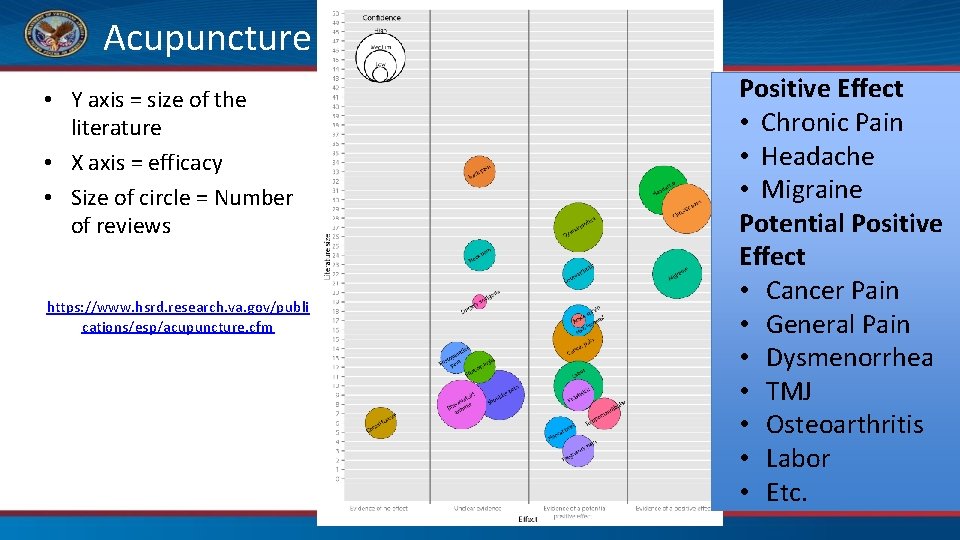
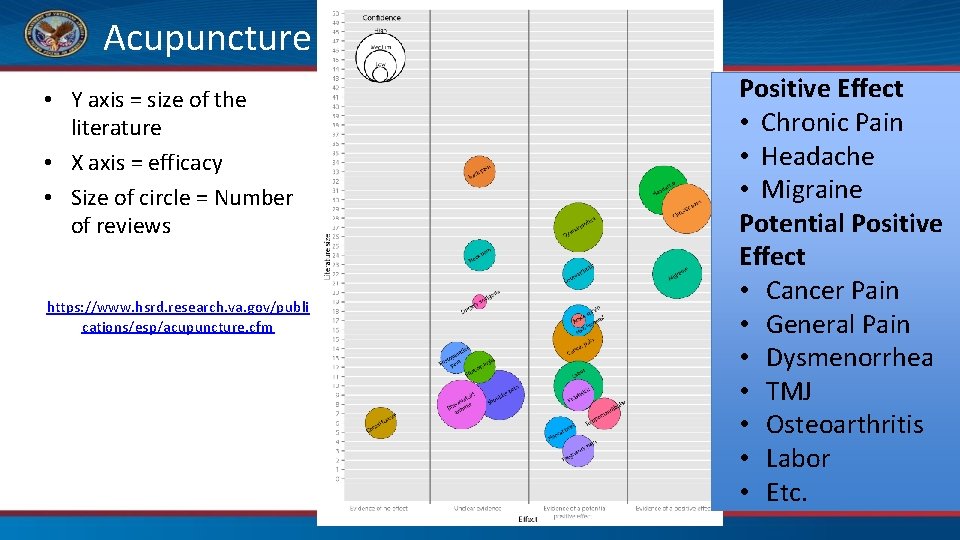
Acupuncture • Y axis = size of the literature • X axis = efficacy • Size of circle = Number of reviews https: //www. hsrd. research. va. gov/publi cations/esp/acupuncture. cfm Positive Effect • Chronic Pain • Headache • Migraine Potential Positive Effect • Cancer Pain • General Pain • Dysmenorrhea • TMJ • Osteoarthritis • Labor • Etc.

Auricular Acupuncture • Battlefield Acupuncture one example – Now called “Protocolized Needling” • Used for pain management sushiphotos via Foter. com / CC BY

The Passport has a chapter on each group of therapies • Chapter 14 – Intro to CIH • 12, Power of the Mind (covers mind-body therapies) • 15 – Biologically Based • 16 – Manipulative and Body. Based • 17 – Energy Medicine • 18 – Whole Systems of Medicine https: //wholehealth. wisc. edu/ Under “Get Started”
In Summary. . . • Many CIH approaches out there – Veterans use them and want them – Research variable, but promising for some • Know about them, know how you feel about them. – Perhaps try them yourself. How might they fit into your self-care? • The VA is covering List 1 CIH therapies now!

Mindful Movement Break Tai Chi and Qigong Dolfin. Dans via Foter. com / CC BY
Whole Health Clinical Care: Working with Teams and Systems
1: 1 with a Patient This Photo by Unknown Author is licensed under CC BY-NC-ND 109
Agenda • What • Why – Unintended consequences of the current health care model – Evidence • How – 1: 1 (clinician and patient) – With your teams – With your systems This Photo by Unknown Author is licensed under CC BY-SA-NC 110
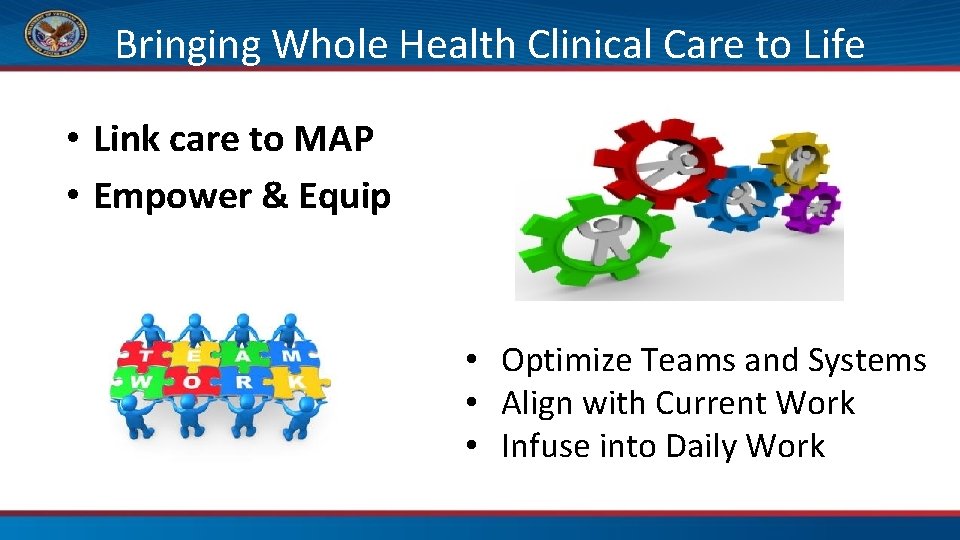
Bringing Whole Health Clinical Care to Life • Link care to MAP • Empower & Equip • Optimize Teams and Systems • Align with Current Work • Infuse into Daily Work
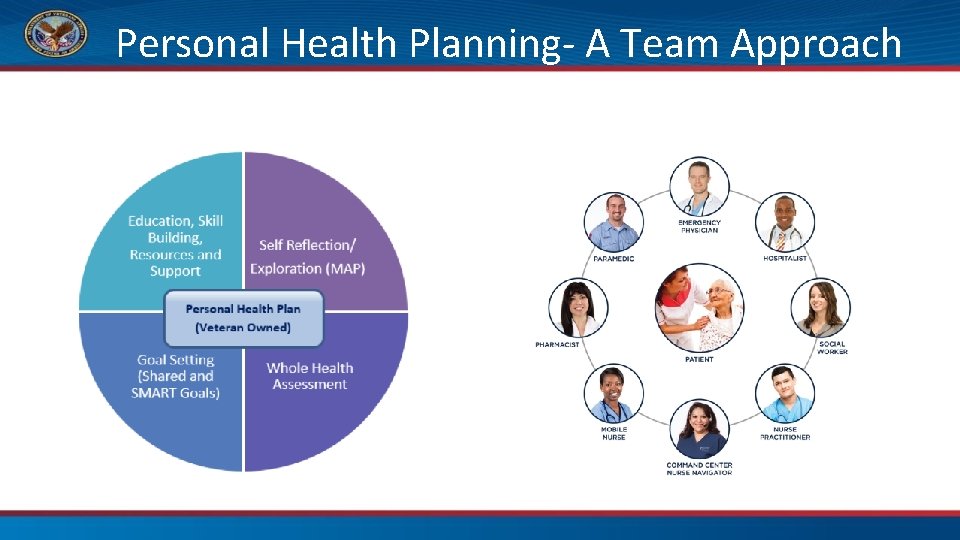
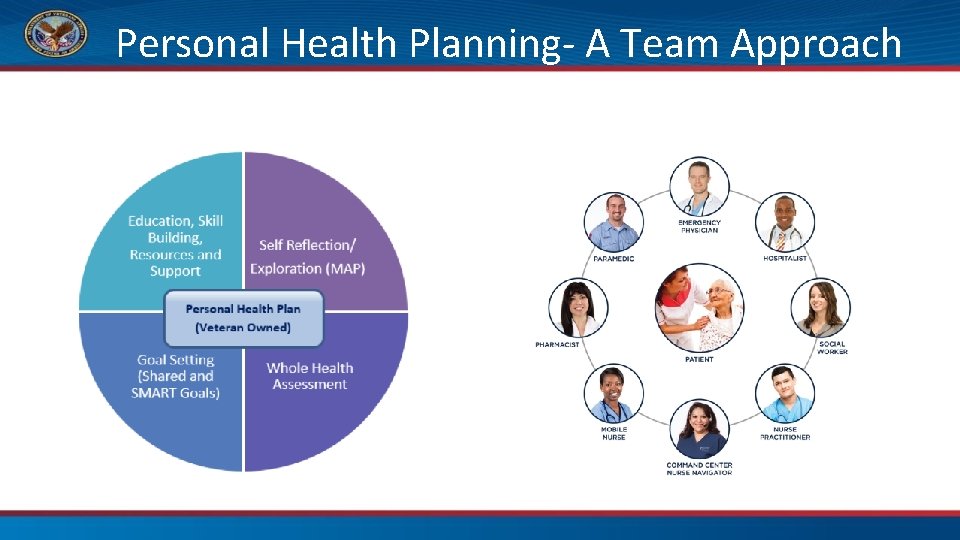
Personal Health Planning- A Team Approach
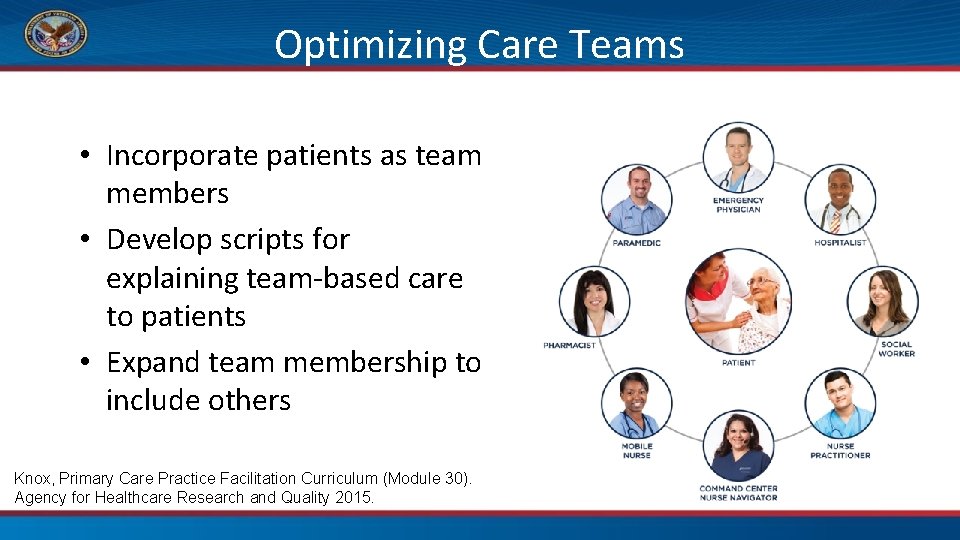
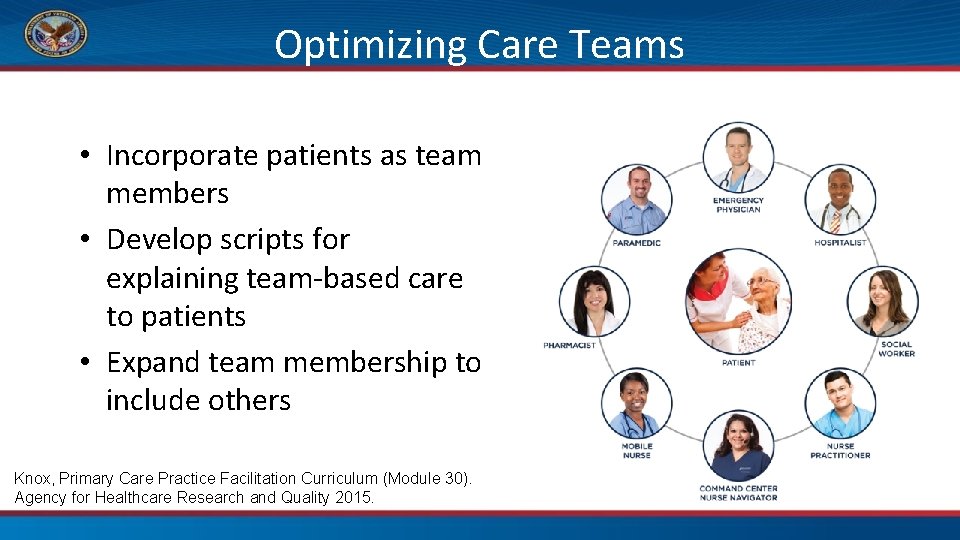
Optimizing Care Teams • Incorporate patients as team members • Develop scripts for explaining team-based care to patients • Expand team membership to include others Knox, Primary Care Practice Facilitation Curriculum (Module 30). Agency for Healthcare Research and Quality 2015.

Letting Our Patients Know • Setting the Stage – Helpful to hear this from different team members – Relatively brief interventions • What happens over time when a patient starts to understand they have a central role in caring for their own whole person? • Practice (30 seconds each) – Patient as a Core Team Member Script – Whole Health Elevator Speech 114
Force Multipliers This Photo by Unknown Author is licensed under CC BY-SA-NC This Photo by Unknown Author is licensed under CC BY-NC 115
Systems 116
Scheduling Systems- Working with Groups • • • Health Coaching groups Shared Medical Appointments Peer groups Access Efficiency Teams This Photo by Unknown Author is licensed under CC BY-SA-NC 117
Technological Systems: Tele-Health • • • Peer groups Mindfulness Yoga Skill-building Etc. This Photo by Unknown Author is licensed under CC BY-NC-ND 119

Data Systems: Population Management • Pre- and post-clinical visit work • Registry work • Whom to target first? – Consider • Importance of “easy wins” as people are learning • “Patient profiling” This Photo by Unknown Author is licensed under CC BY 120
Whole Health in CPRS-examples • PHI using patient data objects • Chronic Low Back Pain order menu • Whole Health-infused Clinical Reminders 121
Infusing into Daily Work • • • Patient letters/Lab results letters Discharge Instructions/After Visit Summaries My. Healthe. Vet Waiting Rooms Etc. 125
Getting it Done • • Bits and pieces Over time Different places Different team members 126

Health Care Teams 127
1 2 8 Best Team Ever • Consider the best team you have ever been on. • What made it so good? This Photo by Unknown Author is licensed under CC BY-NC
1 2 9 Whole Health Teams
Your Team Resource or Demand? This Photo by Unknown Author is licensed under CC BY
1 3 1 Good Teams, Bad Teams • Not the team, it’s the behaviors • Behaviors can be changed, developed, improved This Photo by Unknown Author is licensed under CC BY-SA

Principles of High-Functioning Teams • • • Shared goals Clear roles Mutual trust Effective communication Measurable processes/outcomes Smith, et al. Implementing Optimal Team-Based Care Reduce Clinician Burnout. National Academy of Medicine, Sept 2018. 132
1 3 3 Exercise 1 • 90 seconds to do This Photo by Unknown Author is licensed under CC BY-NC-ND
Debrief • What team behaviors helped you? • What made it hard?
1 3 5 Exercise 2 • 30 seconds to plan/huddle • 90 seconds to do
Debrief • What team behaviors helped you? • What made it hard?
Way to go, Team! This Photo by Unknown Author is licensed under CC BY-NC-ND 137

Personal Health Planning- A Team Approach Possible Team Members • Patient • Family • Community • Peers • Health Coaches • CIH Team Members
Exercise 1 • Introduce and reinforce the idea that your patients are key members of your team. Introduce Whole Health to your patients. • Who on your team will do what? • Consider systems changes your team (or other teams) might work on to support this. 139
Exercise 2 • Begin using PHI’s or PHI content with patients. – Think about where patients can enter the system. • Who on your team will do what? • Consider systems changes your team (or other teams) might work on to support this. *Note: Peer and Health Coach may not always be available to you (not every patient will engage with these folks). Then what? 140
Exercise 3 • Map to the MAP. – Routinely align Clinical Care with individual’s Mission/Aspiration/Purpose. • Who on your team will do what? • Consider systems changes your team (or other teams) might work on to support this. 141

Exercise 4 • Decrease the number of patients readmitted with heart failure after discharge (or improve another clinical metric of your choice) through more effectively empowering and equipping patients. • Who on your team will do what? • Consider systems changes your team (or other teams) might work on to support this. 142
Way to go, Team! 143
Continuous Process Improvement Plan Do Act Study 144
Bringing Whole Health Clinical Care to Life • Link care to MAP • Empower & Equip • • 1: 1 with patients Optimize Teams and Systems Align with Current Work Infuse into Daily Work
Ideal State • Infrastructure supports a Whole Health approach as standard work and the default option. This Photo by Unknown Author is licensed under CC BY-SA 146

Ideal State: Patient/Staff Experience • • • Healing environment Relationship, connection Communication Coordination Aligned Empowered 147
Are we so different than our patients? • We don’t always make choices consistent with our values. • We know what we want to do, but not always how. • We also want the quick fix. • We get discouraged and give up. 148
Just as with our Veterans… We may not always have total control over everything… But what might we have some control over? 149

This Photo by Unknown Author is licensed under CC BY-NC-ND
The Way Forward • Focus on what really matters – Link to MAP • Work smarter, not harder – Empower and Equip – Force multipliers- our teams and systems • Celebrate successes This Photo by Unknown Author is licensed under CC BY 151
Teamwork This Photo by Unknown Author is licensed under CC BY-NC-ND 152

What will you try this week? 153


Now, we can help them be mission ready for their lives, optimizing their health in service of what matters to them. How Will We Identify Success? When Veterans achieve outcomes they never even imagined. VETERANS HEALTH ADMINISTRATION

Thank you! 156
To Learn More About Whole Health VA Patient Centered Care (External–OPCC&CT resources for Veterans & family members) http: //www. va. gov/patientcenteredcare/ OPCC&CT Share. Point Hub (Internal–OPCC&CT Share. Point) https: //vaww. infoshare. va. gov/sites/OPCC/Pages/Default. aspx Whole Health Education Website https: //wholehealth. wisc. edu/ Field Implementation Team Consultant Insert your FIT Consultant email here
 Cdc whole school whole community whole child
Cdc whole school whole community whole child Whole health clinical group
Whole health clinical group Whole health circle of health
Whole health circle of health Massed practice
Massed practice Implementation of hrd program
Implementation of hrd program Implementing strategies management and operations issues
Implementing strategies management and operations issues Mis issues in strategy implementation
Mis issues in strategy implementation Chapter 7 strategic management
Chapter 7 strategic management Tripod pricing strategy
Tripod pricing strategy Implementing merchandise plans
Implementing merchandise plans Designing and implementing branding strategies
Designing and implementing branding strategies Designing and implementing brand architecture strategies
Designing and implementing brand architecture strategies Features of portfolio assessment
Features of portfolio assessment Crm vision statement examples
Crm vision statement examples Qsen core competencies
Qsen core competencies Challenges of implementing predictive analytics
Challenges of implementing predictive analytics Implementing organizational change spector
Implementing organizational change spector Implementing strategies marketing finance/accounting
Implementing strategies marketing finance/accounting Is the traditional method of implementing access control
Is the traditional method of implementing access control Problems in implementing portfolio management
Problems in implementing portfolio management Matching structure with strategy
Matching structure with strategy Brand hierarchy
Brand hierarchy Nfpa 1600 standard
Nfpa 1600 standard Implementing organizational change theory into practice
Implementing organizational change theory into practice Ubmta
Ubmta Nfpa business continuity
Nfpa business continuity Stateful firewall
Stateful firewall Implementing strategies management and operations issues
Implementing strategies management and operations issues Clinical and administrative health information system
Clinical and administrative health information system Bp form 204
Bp form 204 Oblique cutting example
Oblique cutting example Ta 202
Ta 202 Difference between mt103 and mt202
Difference between mt103 and mt202 Linia kolejowa 202
Linia kolejowa 202 Mt 202
Mt 202 202 accepted
202 accepted Sfu library surrey
Sfu library surrey Cve 202
Cve 202 Coe 202 kfupm
Coe 202 kfupm Coe 202
Coe 202 Consensus theorem
Consensus theorem Umbc cmsc 202
Umbc cmsc 202 Xxxxxxxv
Xxxxxxxv Cvsp 202 aub
Cvsp 202 aub Ashrae standard 202 pdf
Ashrae standard 202 pdf B d ribofuranosa
B d ribofuranosa Cse 202
Cse 202 Cse 202
Cse 202 Cpcs 202
Cpcs 202 Coe 202
Coe 202 Coe 202
Coe 202 Coe202
Coe202 05/11/202
05/11/202 Cs 202
Cs 202 Contilube 2
Contilube 2 Application of lcm and hcf in daily life ppt
Application of lcm and hcf in daily life ppt Mt manager inventia download
Mt manager inventia download 202
202 Bio 202
Bio 202 Ie 202
Ie 202 Tolga girici ele 202
Tolga girici ele 202 Cpcs 202
Cpcs 202 202
202 Coe 202
Coe 202 Leadership in medical education
Leadership in medical education Aud-202
Aud-202 A+202:2=800
A+202:2=800 Coe 202
Coe 202 Provision of unrealised profit
Provision of unrealised profit Acf 202
Acf 202 Acf 202
Acf 202 What does 202 mean
What does 202 mean Chn 202
Chn 202 Coe 202
Coe 202 A+202:2=800
A+202:2=800 Win 202
Win 202 Emma watson 202
Emma watson 202 Myanmar 202/5
Myanmar 202/5 Coe 202
Coe 202 Plasa
Plasa Watson emma
Watson emma 192,168,0,202
192,168,0,202 192,168,0,202
192,168,0,202 Cv 202
Cv 202 Coe 202 unlv
Coe 202 unlv Enve 202
Enve 202 2016/c 202/02
2016/c 202/02 Cse 202
Cse 202 Cse 202
Cse 202 Cse 202
Cse 202 Cse 202
Cse 202 Penjir
Penjir Cpcs 202
Cpcs 202 Eee202
Eee202 Coe 202
Coe 202 Bbkfupm
Bbkfupm Cmsc 341 umbc
Cmsc 341 umbc Elec 202
Elec 202 Live your whole life trinity
Live your whole life trinity Whole health library
Whole health library Passport to whole health
Passport to whole health Dacbn meaning
Dacbn meaning Clinical equipoise
Clinical equipoise Uric acid clinical significance
Uric acid clinical significance University clinical center tuzla
University clinical center tuzla Astenopy
Astenopy Clinical scales of mmpi
Clinical scales of mmpi Managing clinical risk
Managing clinical risk Fsfd clinical trial
Fsfd clinical trial Nature of clinical psychology
Nature of clinical psychology Clinical value compass
Clinical value compass Good clinical governance adalah
Good clinical governance adalah Socra clinical research
Socra clinical research Clinical significance of albumin
Clinical significance of albumin Dr charlotte lemech
Dr charlotte lemech Introduction to clinical laboratory
Introduction to clinical laboratory Dicompi
Dicompi Clinical risk management in dentistry
Clinical risk management in dentistry Undertaking clinical fieldwork
Undertaking clinical fieldwork Research design in clinical psychology
Research design in clinical psychology Remounting procedure
Remounting procedure Importance of refraction
Importance of refraction Pi clinical research consultancy
Pi clinical research consultancy Schistocytes in dic
Schistocytes in dic Cholecystitis pathogenesis
Cholecystitis pathogenesis Outpatient clinical documentation improvement
Outpatient clinical documentation improvement Clinical comprehensive assessment
Clinical comprehensive assessment Nsw education
Nsw education Triad of normal pressure hydrocephalus
Triad of normal pressure hydrocephalus Nida clinical trials network
Nida clinical trials network Ncsbn clinical judgment measurement model
Ncsbn clinical judgment measurement model Bedside clinical guidelines partnership
Bedside clinical guidelines partnership Www.myclinicalexchange.com
Www.myclinicalexchange.com Dr bernard lo's clinical model
Dr bernard lo's clinical model Clinical audit example
Clinical audit example Clinical value compass
Clinical value compass Clinical pathology definition
Clinical pathology definition Site initiation visit
Site initiation visit Ctopci
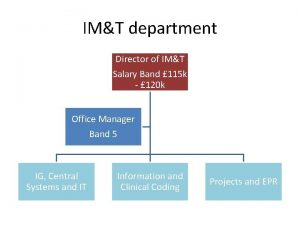
Ctopci Clinical coder salary
Clinical coder salary Clubfoot clinical features
Clubfoot clinical features Clinical presentation of hodgkin's lymphoma
Clinical presentation of hodgkin's lymphoma Good documentation practices error correction
Good documentation practices error correction Dr ayling sanjaya
Dr ayling sanjaya