Who Said Cafeteria Flex Plans were EASY Nathan
- Slides: 41
Who Said Cafeteria Flex Plans were EASY? Nathan Carlson, MBA, AIF®, QPA, QKA President 24 Hour. Flex
Outline A. B. C. D. Introduction Overview of Cafeteria plans Integration issues: Flex/HSA Integration issues: Flex/COBRA
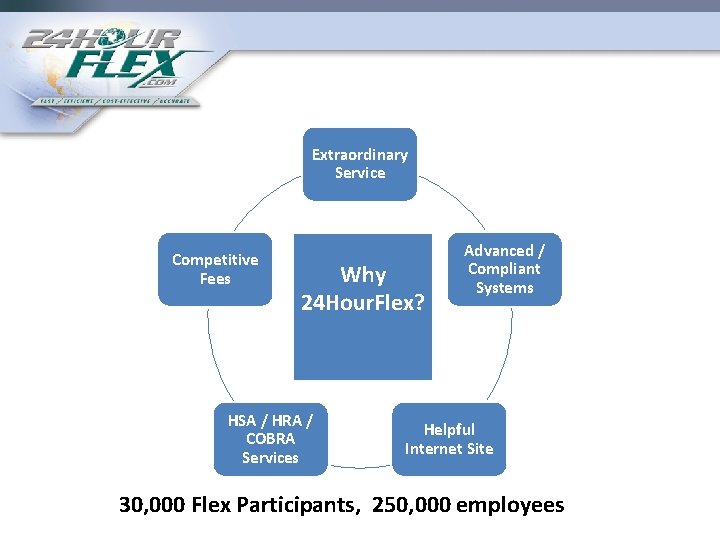
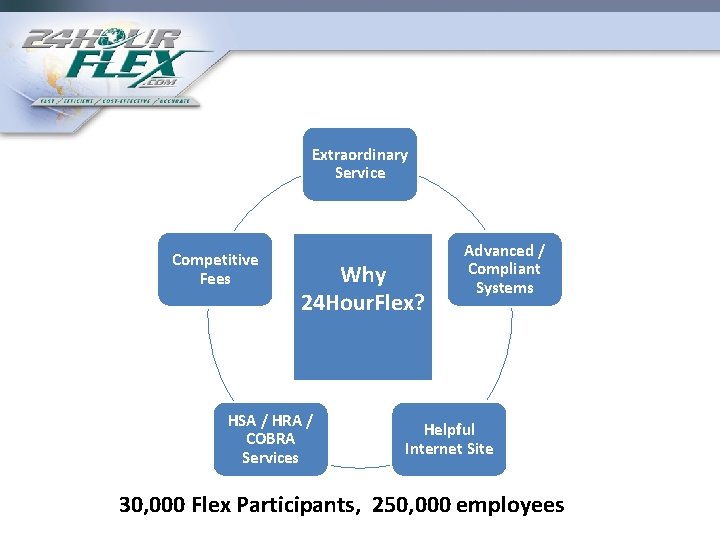
Extraordinary Service Competitive Fees Why 24 Hour. Flex? HSA / HRA / COBRA Services Advanced / Compliant Systems Helpful Internet Site 30, 000 Flex Participants, 250, 000 employees
2011 Statistics 100, 000 Claim Forms 50, 000 Help Center phone calls 600, 000 Debit Card Swipes 30, 000 Flex Participants
Cafeteria Plan Types • Premium-only • Flex Accounts – Medical – Dependent Care – Outside Insurance Premium
Funding • Employee Salary Deferral – Tax savings • FICA (7. 65% employer, 5. 65% employee, wage base $110, 100) • FUTA (6. 2%, wage base $7, 000) • SUTA (varies, wage base $10, 000) • Federal Income Tax • State Income Tax
Funding • Employer contributions – Seed contributions • Example, $25 / month to each employee’s flex account – Matching contributions – Flex credits • Menu of benefits created with associated “cost” • Employees given $X Flex credits to spend on benefits
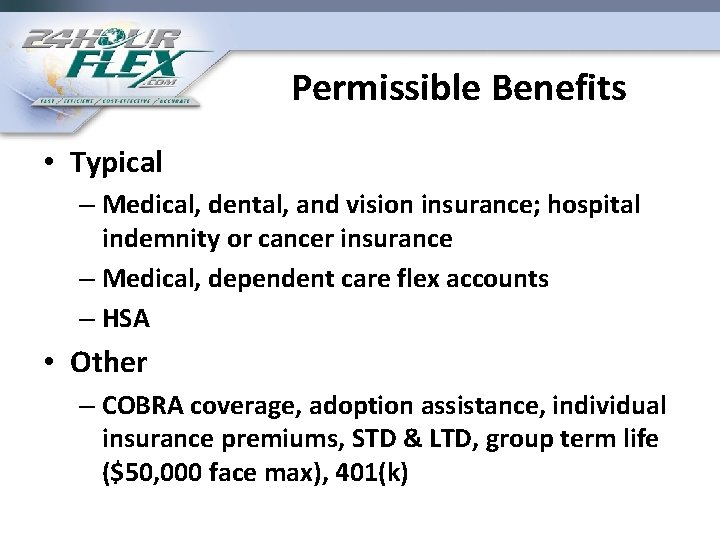
Permissible Benefits • Typical – Medical, dental, and vision insurance; hospital indemnity or cancer insurance – Medical, dependent care flex accounts – HSA • Other – COBRA coverage, adoption assistance, individual insurance premiums, STD & LTD, group term life ($50, 000 face max), 401(k)
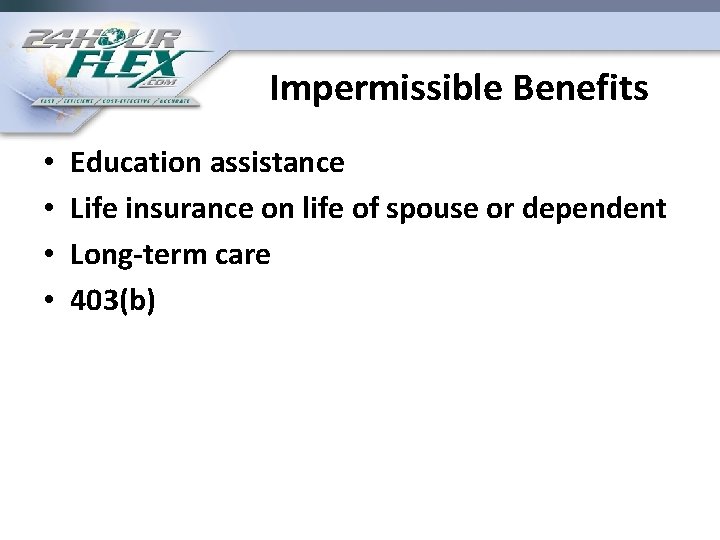
Impermissible Benefits • • Education assistance Life insurance on life of spouse or dependent Long-term care 403(b)
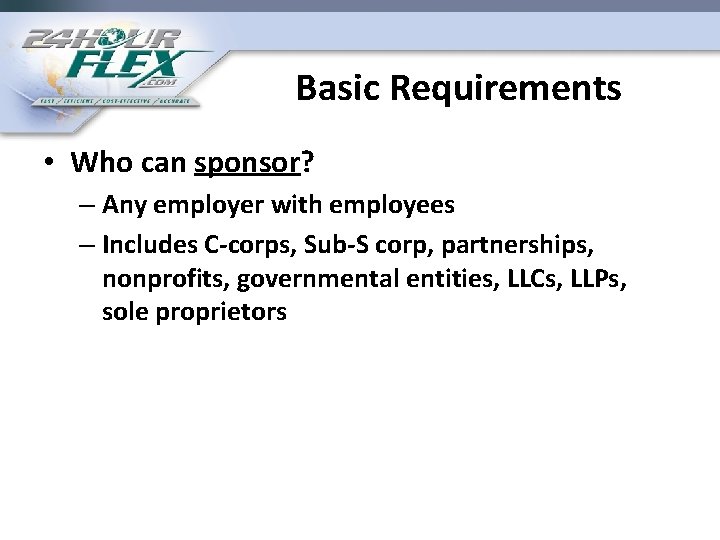
Basic Requirements • Who can sponsor? – Any employer with employees – Includes C-corps, Sub-S corp, partnerships, nonprofits, governmental entities, LLCs, LLPs, sole proprietors
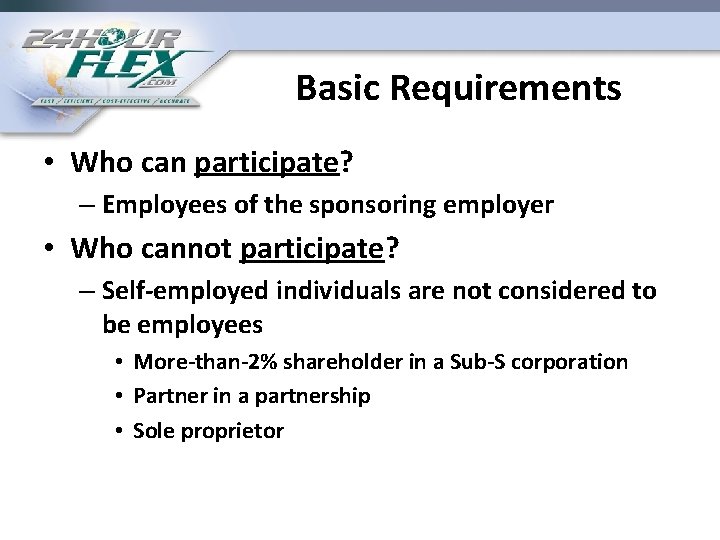
Basic Requirements • Who can participate? – Employees of the sponsoring employer • Who cannot participate? – Self-employed individuals are not considered to be employees • More-than-2% shareholder in a Sub-S corporation • Partner in a partnership • Sole proprietor
Eligibility Rules • Generally tied to group health policy – Ease of administration – Maximize employer FICA savings
Other rules • Written plan document • Written SPD • Must meet annual nondiscrimination testing – All pre-tax benefits; Key <= 25% of total – Daycare: • 5% owners <= 25% of total daycare benefits • NHCE avg >= (HCE avg X 55%) – All ees included in test
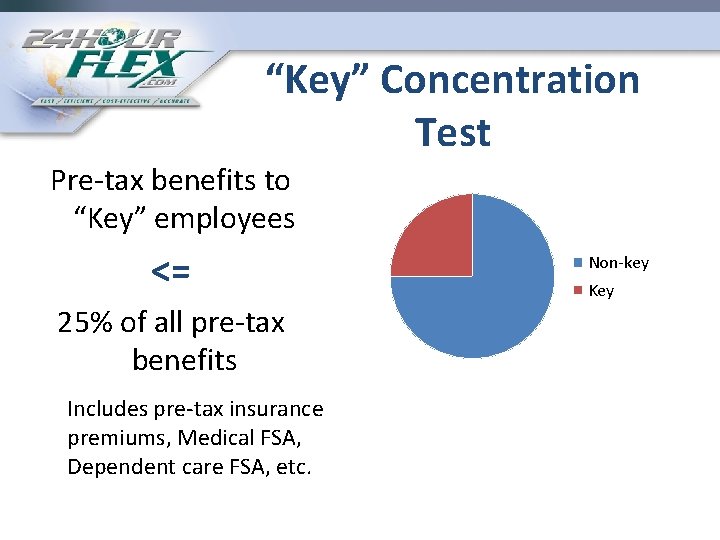
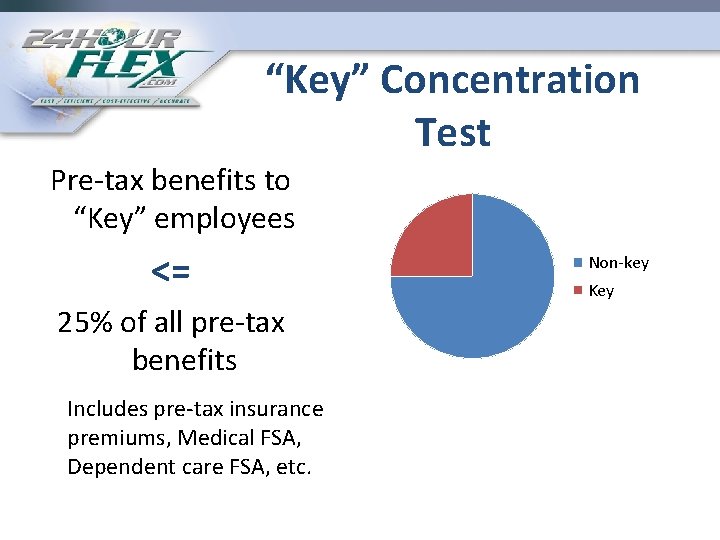
“Key” Concentration Test Pre-tax benefits to “Key” employees <= 25% of all pre-tax benefits Includes pre-tax insurance premiums, Medical FSA, Dependent care FSA, etc. Non-key Key
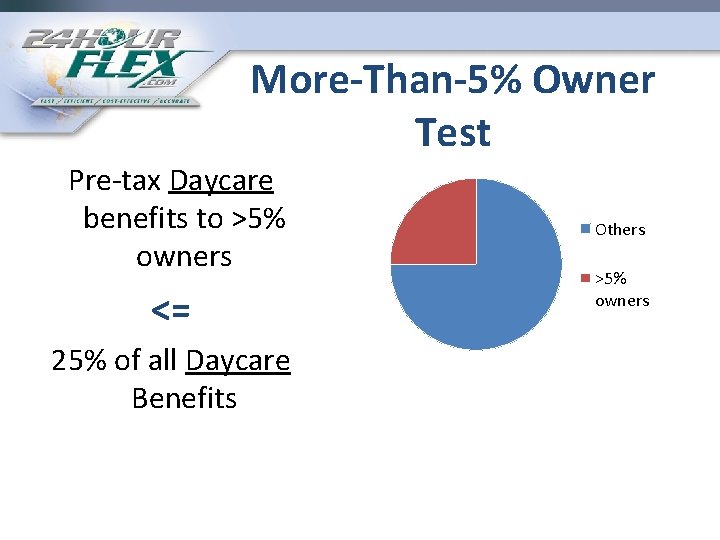
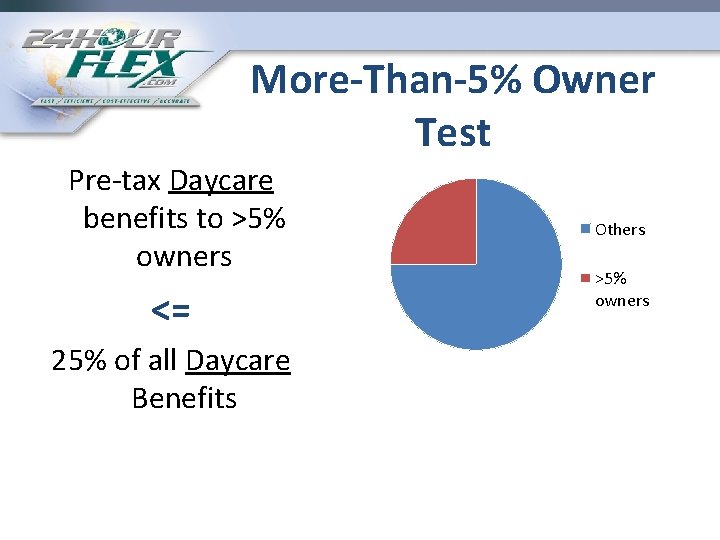
More-Than-5% Owner Test Pre-tax Daycare benefits to >5% owners <= 25% of all Daycare Benefits Others >5% owners
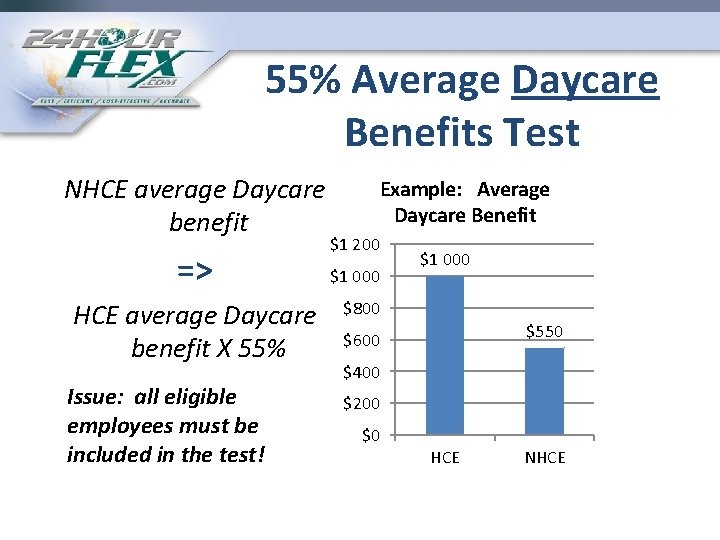
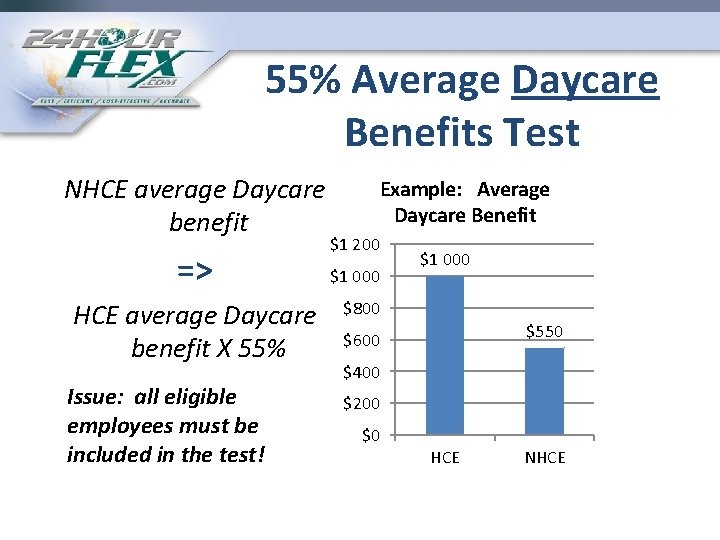
55% Average Daycare Benefits Test NHCE average Daycare benefit => HCE average Daycare benefit X 55% Issue: all eligible employees must be included in the test! Example: Average Daycare Benefit $1 200 $1 000 $800 $550 $600 $400 $200 $0 HCE NHCE
Consequence of Failure • Benefits to “Key”, >5% owners, and/or HCEs are taxable – For the plan year of failure – Requires amending W-2 s, other tax forms
Other rules • Uniform coverage – Annual election available at all times • Election binding unless change of status: – Change of status rules vary with Cafeteria benefit • i. e. , insurance premiums vs. Medical Flex vs. dependent care vs. adoption assistance
FSA Change of Status • Birth, death, or adoption of a child • Change in the employee’s legal status • Termination or commencement of employment by the employee, spouse, or dependent
Change of Status cont. • Change in work schedule (i. e. , reduction of hours) or any other change in employment status that affects eligibility for benefits • Change in eligibility status of a dependent • Change in residence or worksite of employee, spouse, or dependent accompanied by a gain or loss of insurance coverage
Change of Status cont. • For daycare, change in providers resulting in a significant change in daycare cost
Eligible Medical Expense • Amounts paid for the diagnosis, cure, mitigation, treatment, or prevention of disease, or • For the purpose of affecting any structure or function of the body
Eligible Daycare Expense • Expense must enable the employee (and the employee’s spouse) to be gainfully employed • Expense must be for the “care” of one or more “qualifying individuals”. . . – Someone under the age of 13 unless physically or mentally unable to provide self-care
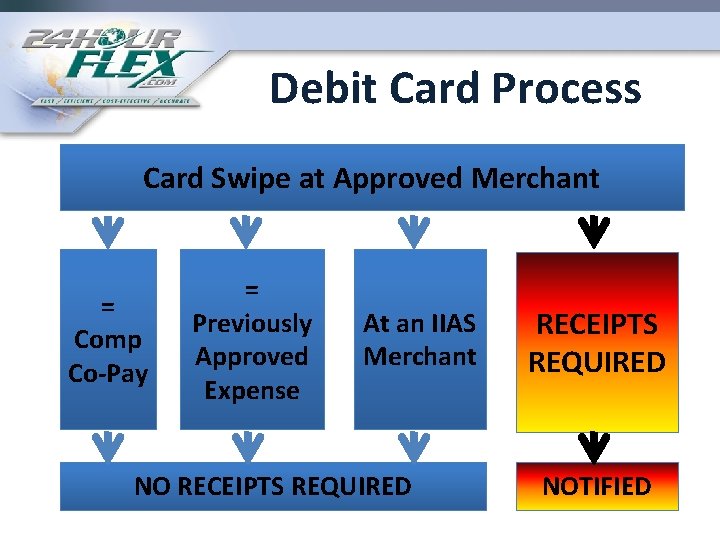
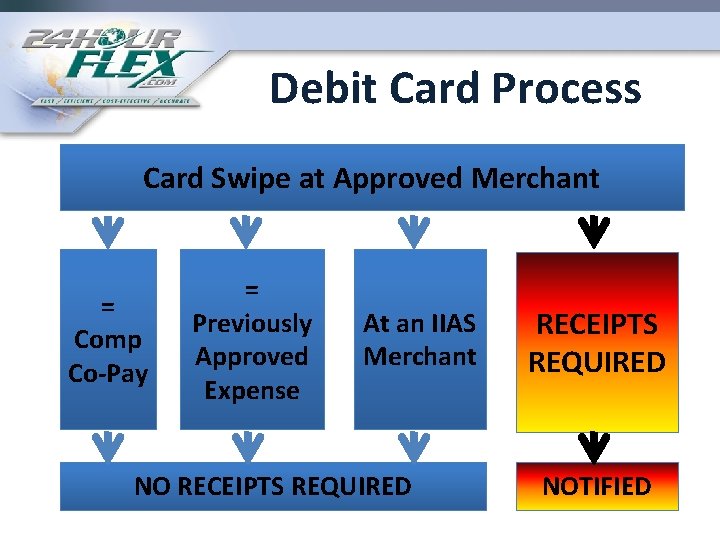
Debit Card Process Card Swipe at Approved Merchant = Comp Co-Pay = Previously Approved Expense At an IIAS Merchant NO RECEIPTS REQUIRED NOTIFIED
Healthcare Flex Changes • OTC – gone as of 1/1/2011 – Unless prescribed by a physician – Does not apply to medical and vision care supplies • Medical FSA cap: $2, 500 – Effective 1/1/2013 – Fiscal year plans: IRS has not instructed us on how this is to be applied
Flex HSA COBRA INTEGRATION QUESTIONS
Q/A 1 • “We have a group that has offered only an HSA-eligible HDHP plan for the last year. At renewal on 8/1 they will offer a non-HSAeligible buy up option. What should we tell employees about their HSA contribution limits for 2011 if they change to the non-HSA-eligible option as of 8/1? ”
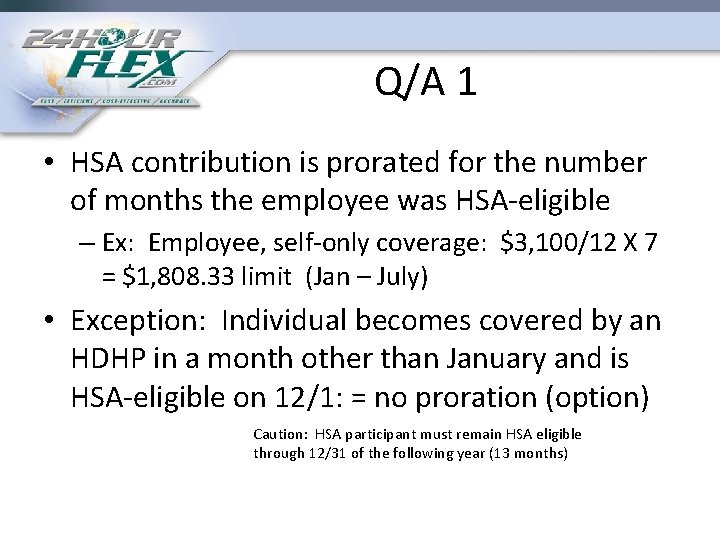
Q/A 1 • HSA contribution is prorated for the number of months the employee was HSA-eligible – Ex: Employee, self-only coverage: $3, 100/12 X 7 = $1, 808. 33 limit (Jan – July) • Exception: Individual becomes covered by an HDHP in a month other than January and is HSA-eligible on 12/1: = no proration (option) Caution: HSA participant must remain HSA eligible through 12/31 of the following year (13 months)
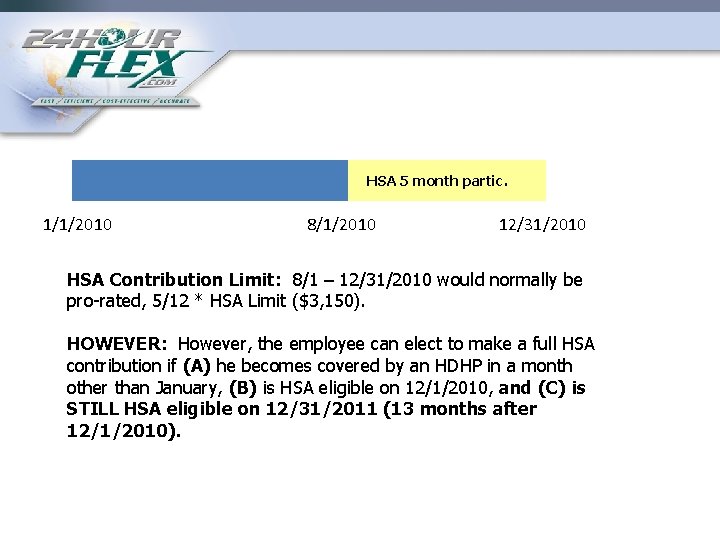
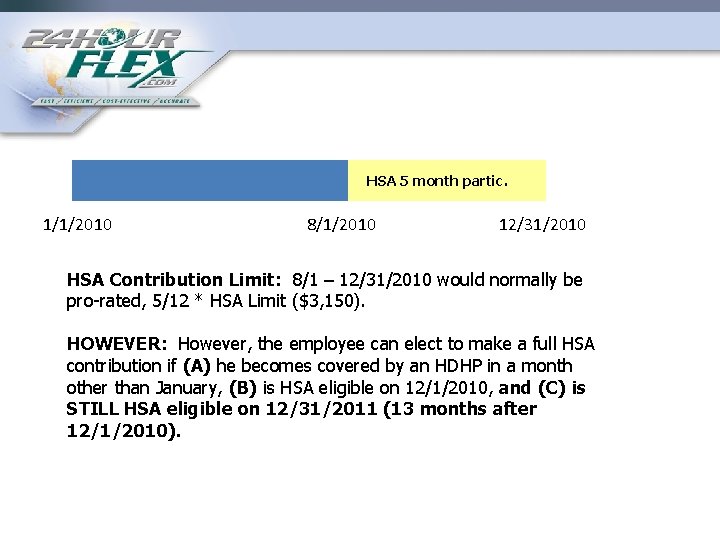
HSA 5 month partic. 1/1/2010 8/1/2010 12/31/2010 HSA Contribution Limit: 8/1 – 12/31/2010 would normally be pro-rated, 5/12 * HSA Limit ($3, 150). HOWEVER: However, the employee can elect to make a full HSA contribution if (A) he becomes covered by an HDHP in a month other than January, (B) is HSA eligible on 12/1/2010, and (C) is STILL HSA eligible on 12/31/2011 (13 months after 12/1/2010).
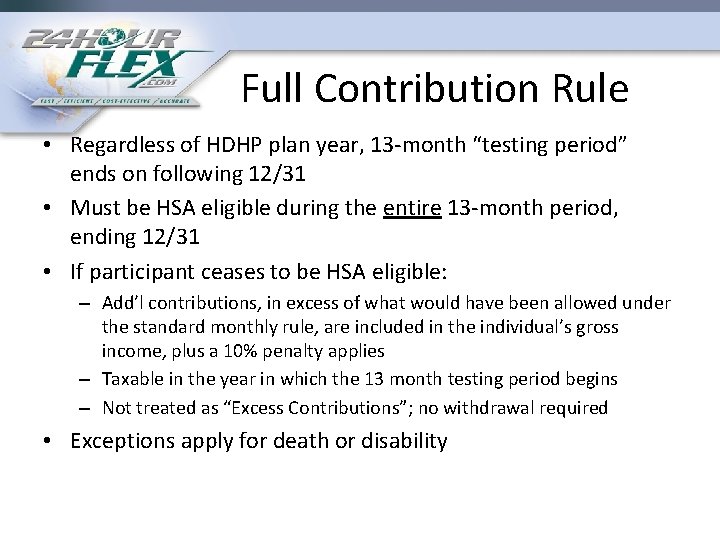
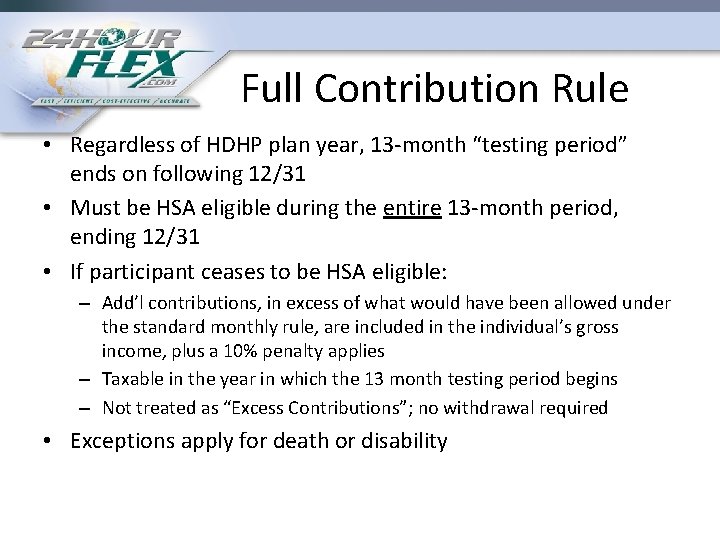
Full Contribution Rule • Regardless of HDHP plan year, 13 -month “testing period” ends on following 12/31 • Must be HSA eligible during the entire 13 -month period, ending 12/31 • If participant ceases to be HSA eligible: – Add’l contributions, in excess of what would have been allowed under the standard monthly rule, are included in the individual’s gross income, plus a 10% penalty applies – Taxable in the year in which the 13 month testing period begins – Not treated as “Excess Contributions”; no withdrawal required • Exceptions apply for death or disability
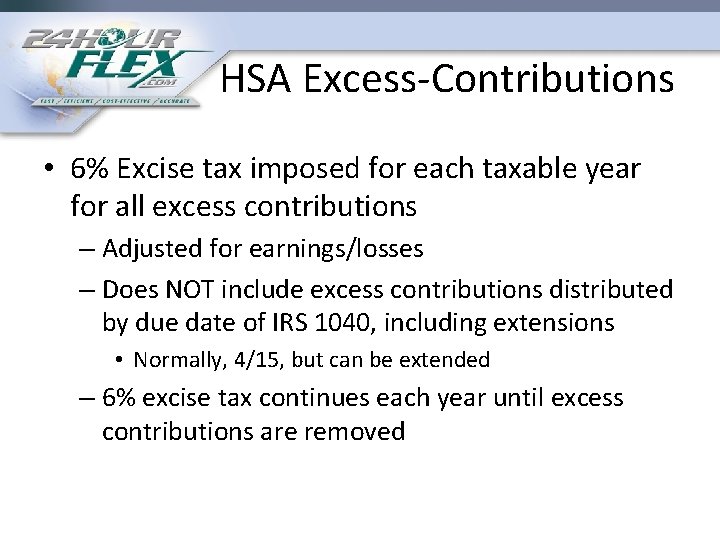
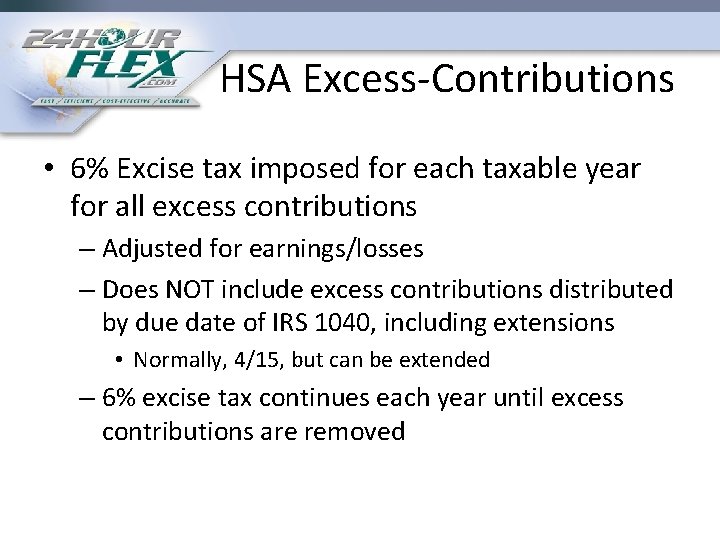
HSA Excess-Contributions • 6% Excise tax imposed for each taxable year for all excess contributions – Adjusted for earnings/losses – Does NOT include excess contributions distributed by due date of IRS 1040, including extensions • Normally, 4/15, but can be extended – 6% excise tax continues each year until excess contributions are removed
Flex HSA DIFFERENT PLAN YEARS COBRA
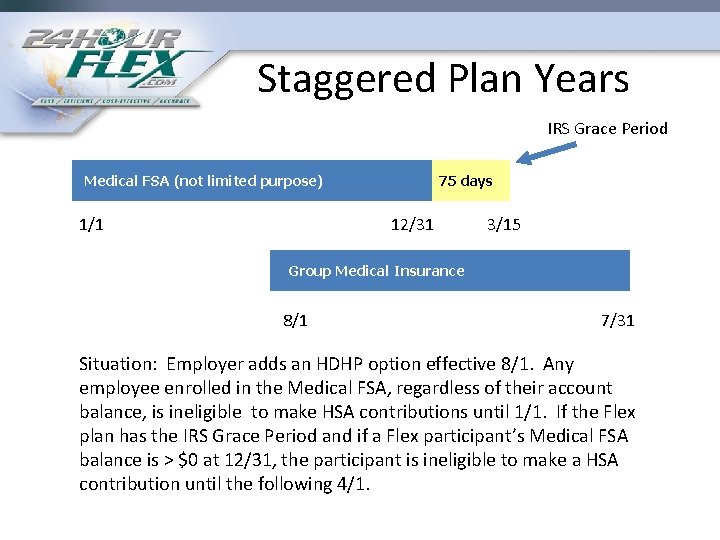
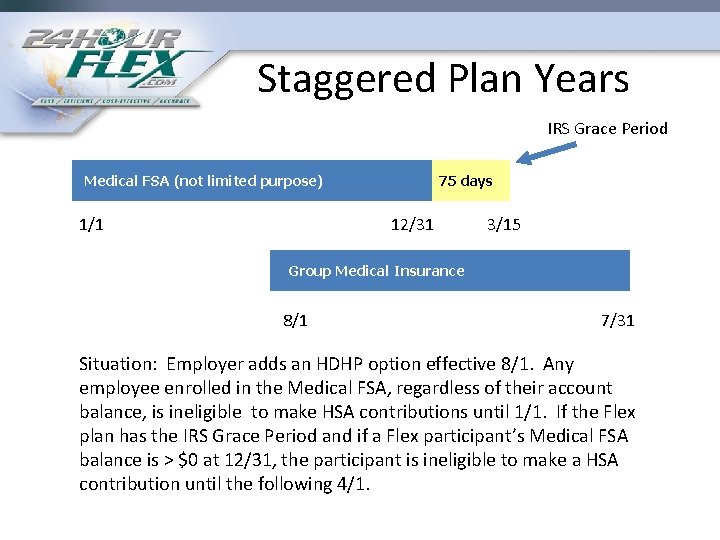
Staggered Plan Years IRS Grace Period Medical FSA (not limited purpose) 1/1 75 days 12/31 3/15 Group Medical Insurance 8/1 7/31 Situation: Employer adds an HDHP option effective 8/1. Any employee enrolled in the Medical FSA, regardless of their account balance, is ineligible to make HSA contributions until 1/1. If the Flex plan has the IRS Grace Period and if a Flex participant’s Medical FSA balance is > $0 at 12/31, the participant is ineligible to make a HSA contribution until the following 4/1.
Flex HSA COBRA INTEGRATION QUESTIONS
Q/A 2 – In 2011 (on a typical day) an employer had 5 medical flex participants, 10 part time employees, 15 full time employees, and individual employeepaid health insurance policies. • Is this medical flex plan subject to COBRA in 2012? – On 12/31/2011, this employer laid off the 10 part time employees, but in 2012 still has 5 medical flex participants and individual health policies. • Is this medical flex plan subject to COBRA in 2012?
Q/A 3 • My flex plan is subject to COBRA. Which participants must be given a medical flex COBRA election, for how long must this election be, what is the COBRA premium, and must all Qualified Beneficiaries be given the option to make a COBRA election with respect to the medical FSA?
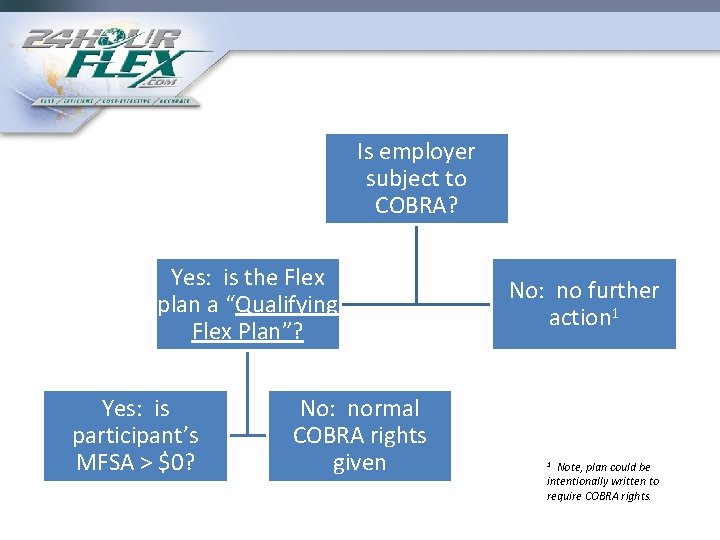
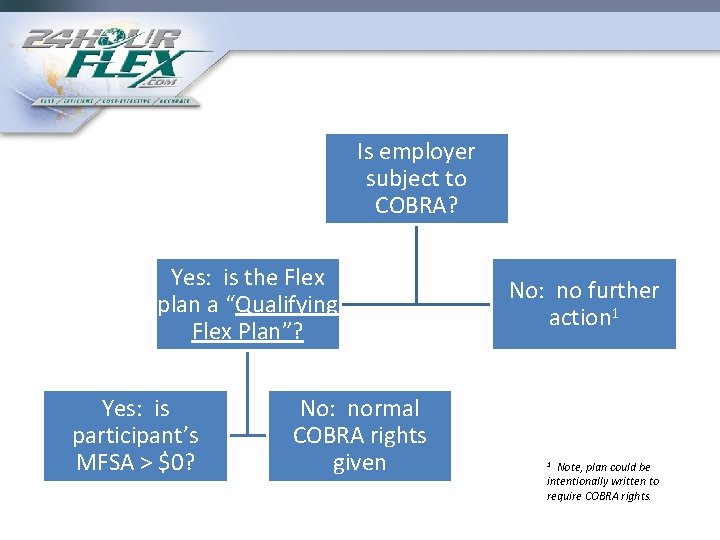
Is employer subject to COBRA? Yes: is the Flex plan a “Qualifying Flex Plan”? Yes: is participant’s MFSA > $0? No: normal COBRA rights given No: no further action 1 Note, plan could be intentionally written to require COBRA rights. 1
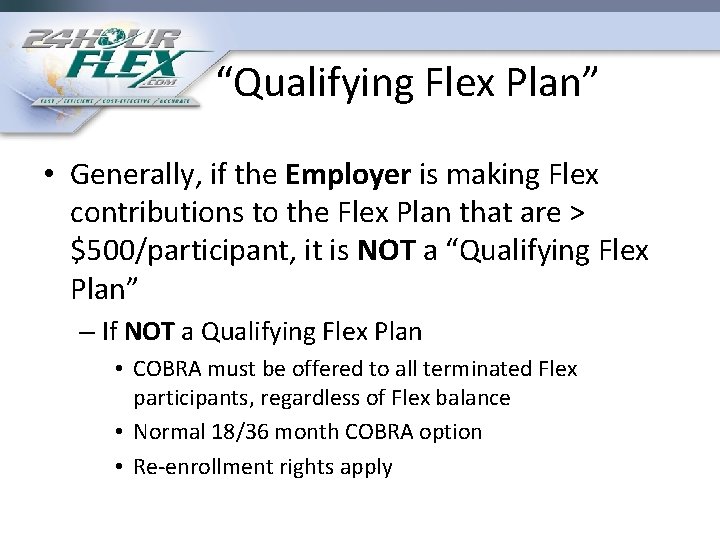
“Qualifying Flex Plan” • Generally, if the Employer is making Flex contributions to the Flex Plan that are > $500/participant, it is NOT a “Qualifying Flex Plan” – If NOT a Qualifying Flex Plan • COBRA must be offered to all terminated Flex participants, regardless of Flex balance • Normal 18/36 month COBRA option • Re-enrollment rights apply
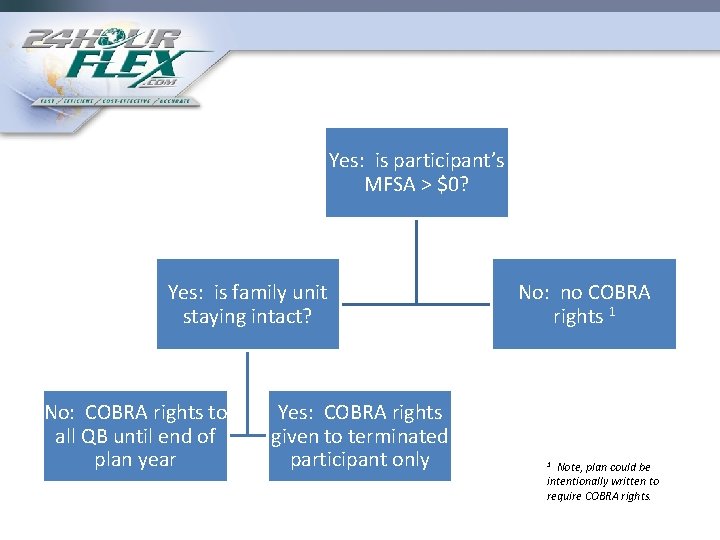
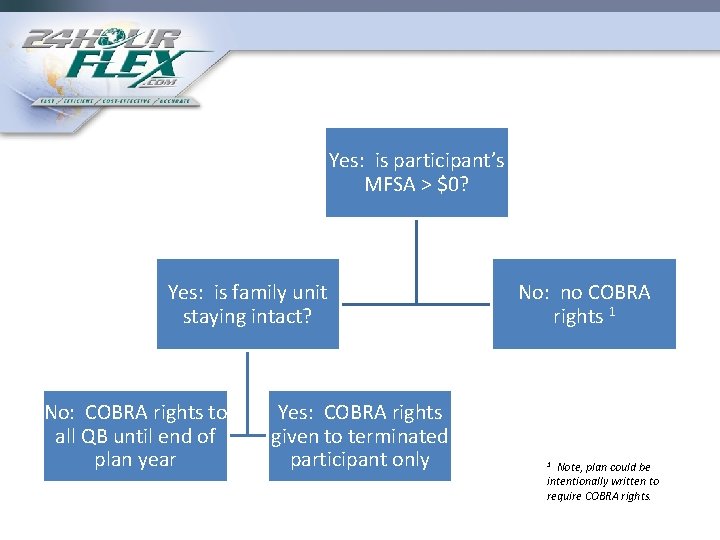
Yes: is participant’s MFSA > $0? Yes: is family unit staying intact? No: COBRA rights to all QB until end of plan year Yes: COBRA rights given to terminated participant only No: no COBRA rights 1 Note, plan could be intentionally written to require COBRA rights. 1
Flex and COBRA • Because of the complexities involved between Flex and COBRA – Good Idea: have same TPA administer both
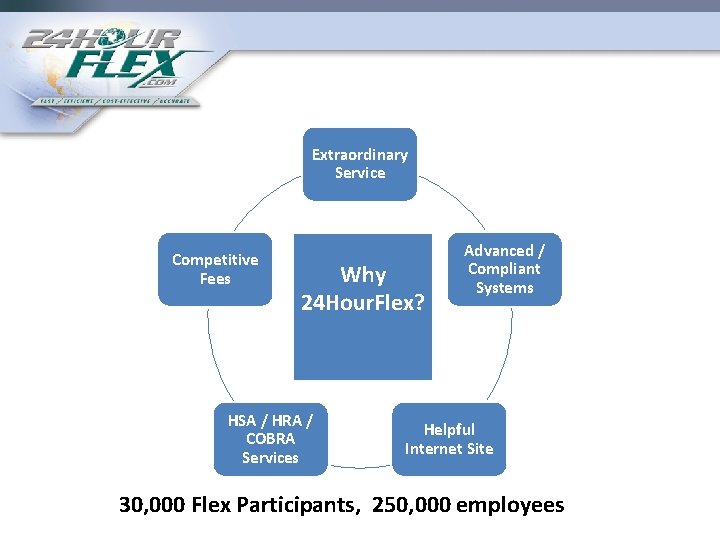
Extraordinary Service Competitive Fees Why 24 Hour. Flex? HSA / HRA / COBRA Services Advanced / Compliant Systems Helpful Internet Site 30, 000 Flex Participants, 250, 000 employees