WHO Multimodal Hand Hygiene Improvement Strategy Education Session

- Slides: 56
WHO Multimodal Hand Hygiene Improvement Strategy Education Session on Health Care-associated Infections and Hygiene for Trainers, Observers and Health-care Workers ANNEX 16
Objectives 1. Definition, impact and burden of health care-associated infection 2. Major patterns of transmission of health care-associated germs with a particular focus on hand transmission 3. Prevention of health care-associated infection and hygiene 4. The WHO Guidelines on Hand Hygiene in Health Care (Advanced Draft) and their implementation strategy and tools 5. Why, when and how to perform hand hygiene in health care 6. How to observe hand hygiene practices among health-care workers
WHO Multimodal Hand Hygiene Improvement Strategy Part 1 Definition, impact and burden of health care-associated infection
Definition of health care- associated infection (also referred to as “nosocomial” or “hospital” infection) “An infection occurring in a patient during the process of care in a hospital or other health-care facility which was not present or incubating at the time of admission. This includes infections acquired in the hospital but appearing after discharge, and also occupational infections among staff of the facility” Ducel G et al. Prevention of hospital-acquired infections. A practical guide. WHO 2002
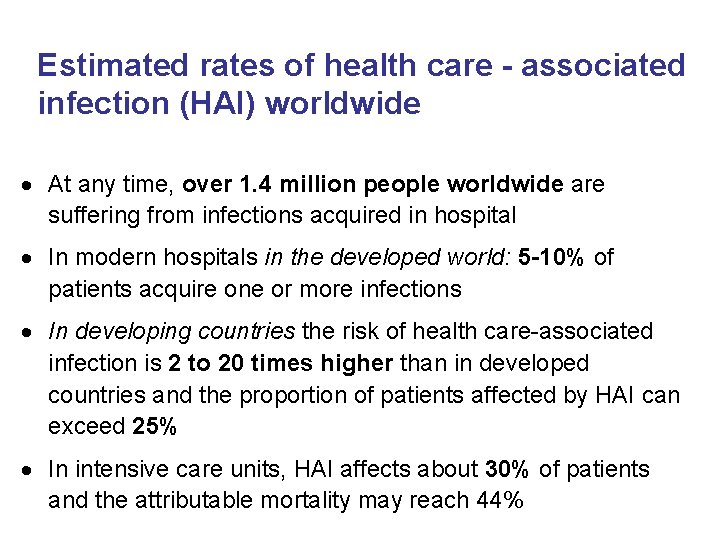
Estimated rates of health care - associated infection (HAI) worldwide At any time, over 1. 4 million people worldwide are suffering from infections acquired in hospital In modern hospitals in the developed world: 5 -10% of patients acquire one or more infections In developing countries the risk of health care-associated infection is 2 to 20 times higher than in developed countries and the proportion of patients affected by HAI can exceed 25% In intensive care units, HAI affects about 30% of patients and the attributable mortality may reach 44%
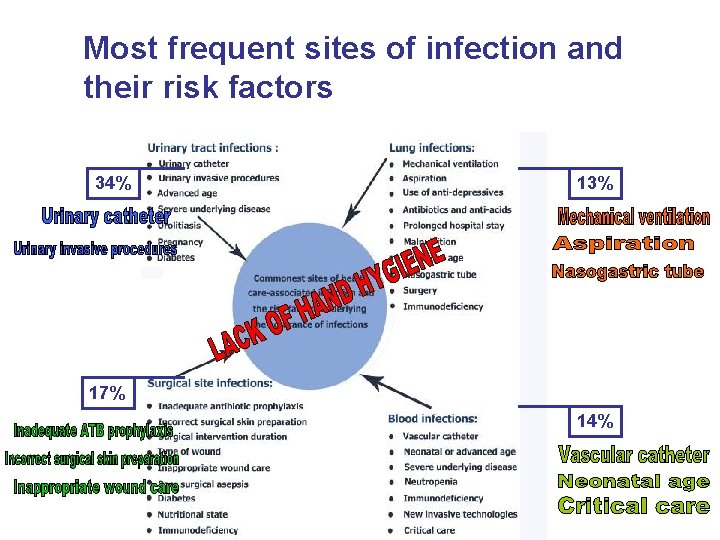
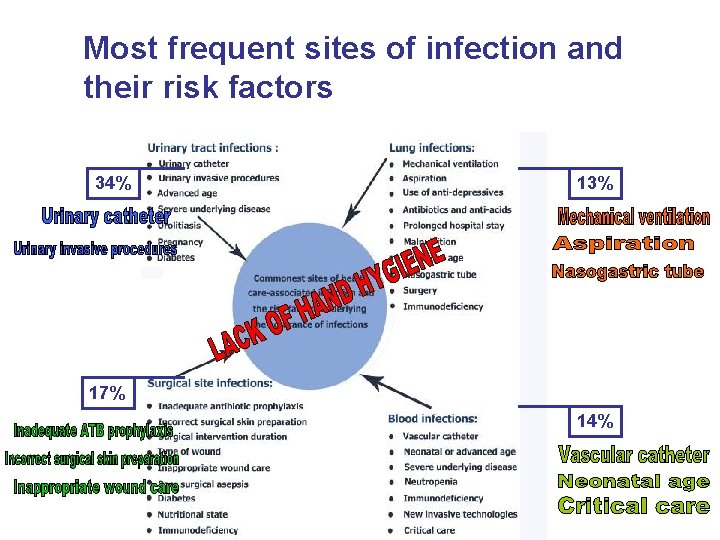
Most frequent sites of infection and their risk factors 34% 13% 17% 14%
Part 2 Major patterns of transmission of health care-associated germs with a particular focus on hand transmission
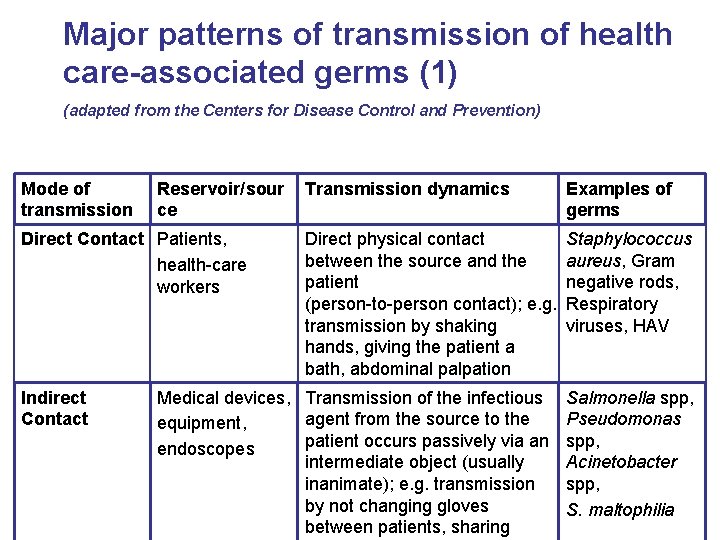
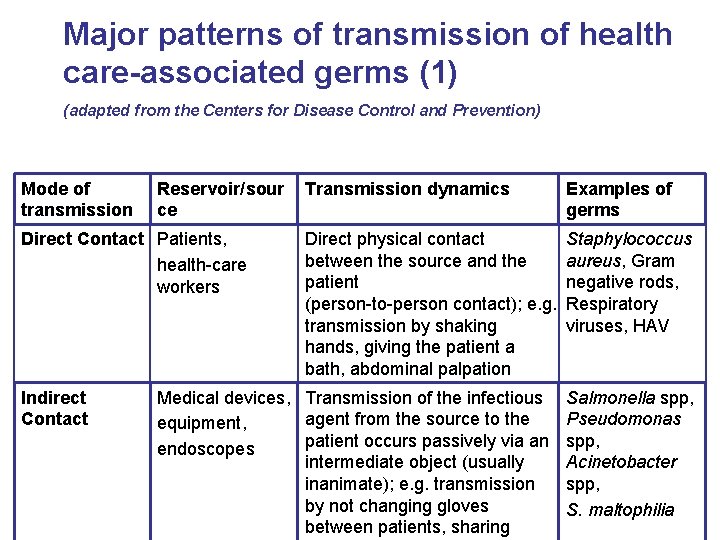
Major patterns of transmission of health care-associated germs (1) (adapted from the Centers for Disease Control and Prevention) Mode of transmission Reservoir/sour ce Direct Contact Patients, health-care workers Indirect Contact Transmission dynamics Examples of germs Direct physical contact between the source and the patient (person-to-person contact); e. g. transmission by shaking hands, giving the patient a bath, abdominal palpation Staphylococcus aureus, Gram negative rods, Respiratory viruses, HAV Medical devices, Transmission of the infectious agent from the source to the equipment, patient occurs passively via an endoscopes intermediate object (usually inanimate); e. g. transmission by not changing gloves between patients, sharing Salmonella spp, Pseudomonas spp, Acinetobacter spp, S. maltophilia
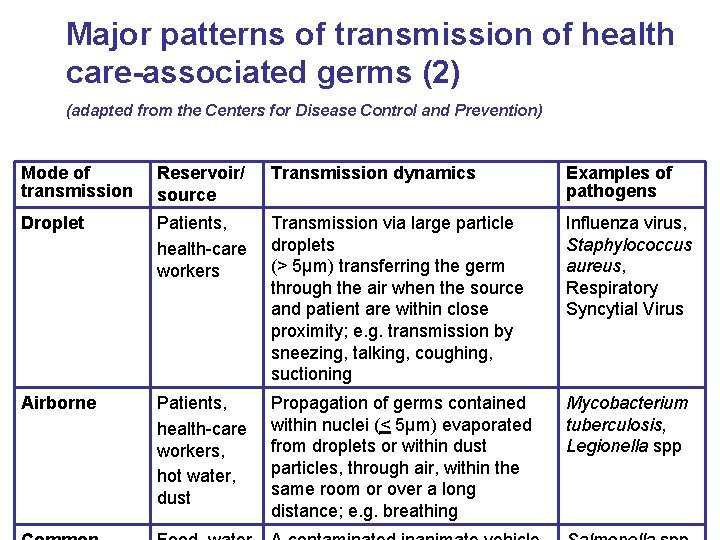
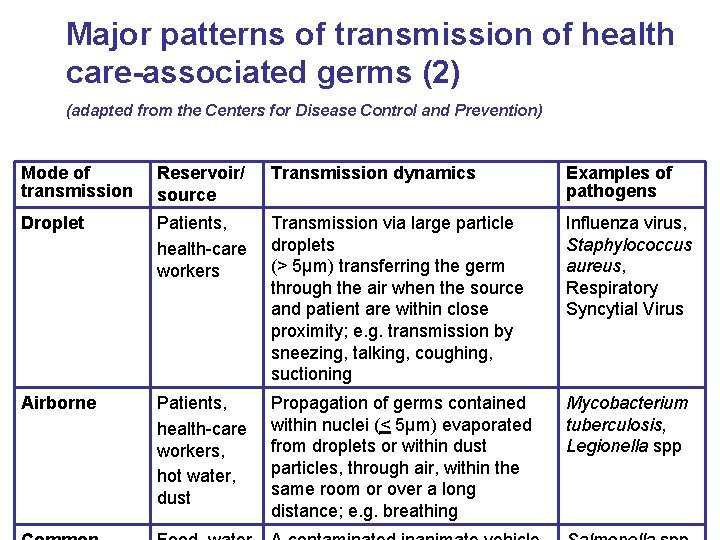
Major patterns of transmission of health care-associated germs (2) (adapted from the Centers for Disease Control and Prevention) Mode of transmission Reservoir/ source Transmission dynamics Examples of pathogens Droplet Patients, health-care workers Transmission via large particle droplets (> 5µm) transferring the germ through the air when the source and patient are within close proximity; e. g. transmission by sneezing, talking, coughing, suctioning Influenza virus, Staphylococcus aureus, Respiratory Syncytial Virus Airborne Patients, health-care workers, hot water, dust Propagation of germs contained within nuclei (< 5µm) evaporated from droplets or within dust particles, through air, within the same room or over a long distance; e. g. breathing Mycobacterium tuberculosis, Legionella spp
Hand transmission • Hands are the most common vehicle to transmit health careassociated pathogens • Transmission of health care-associated pathogens from one patient to another via healthcare workers’ hands requires 5 sequential steps
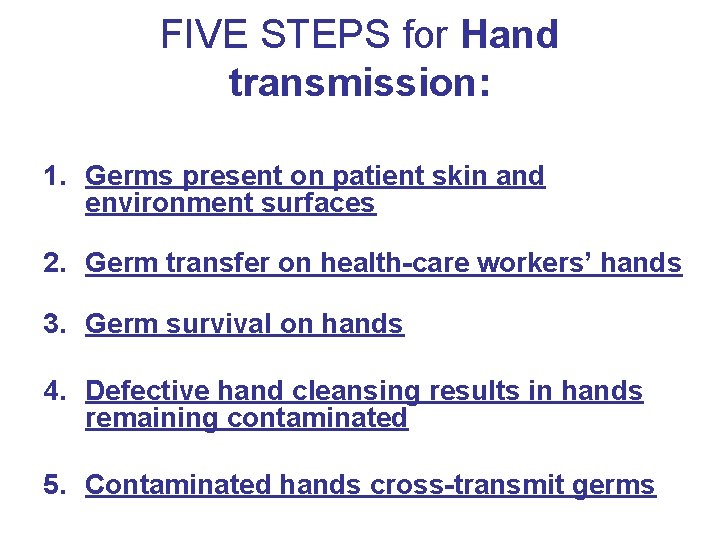
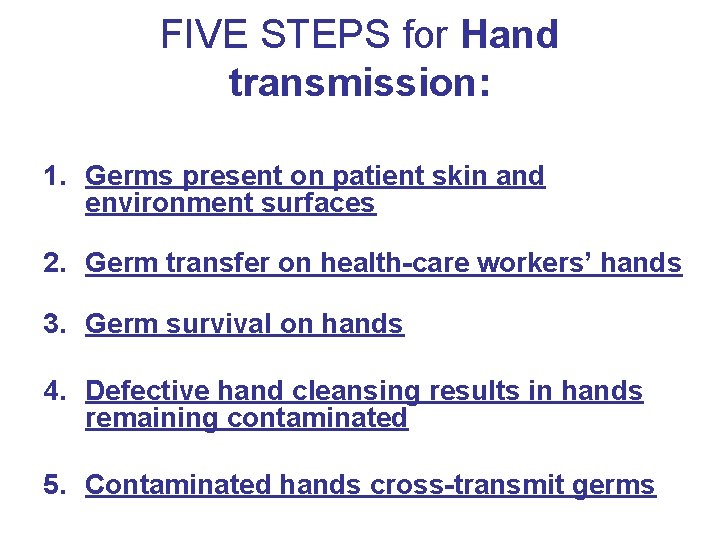
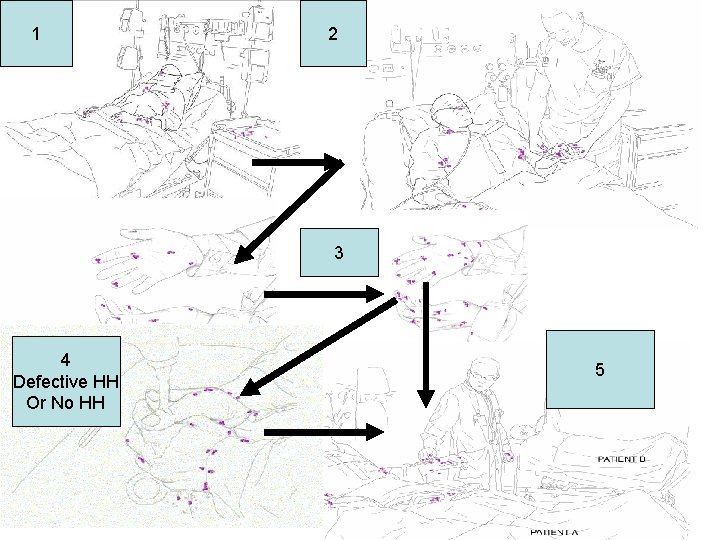
FIVE STEPS for Hand transmission: 1. Germs present on patient skin and environment surfaces 2. Germ transfer on health-care workers’ hands 3. Germ survival on hands 4. Defective hand cleansing results in hands remaining contaminated 5. Contaminated hands cross-transmit germs
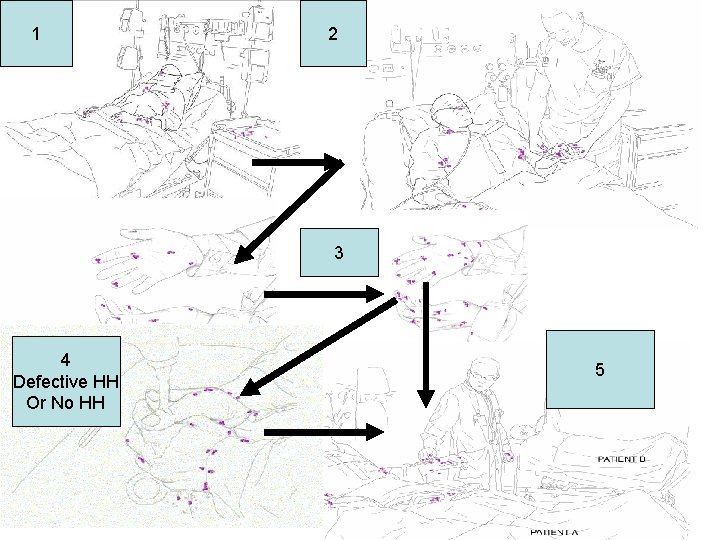
1 2 3 4 Defective HH Or No HH 5
Part 3 Prevention of health care-associated infection and hygiene
Strategies for infection control General measures Surveillance Standard precautions Transmission-based precautions Antibiotic control Specific measures Specifically targeted against: - Urinary tract infections - Surgical site infections - Respiratory infections - Bloodstream infections
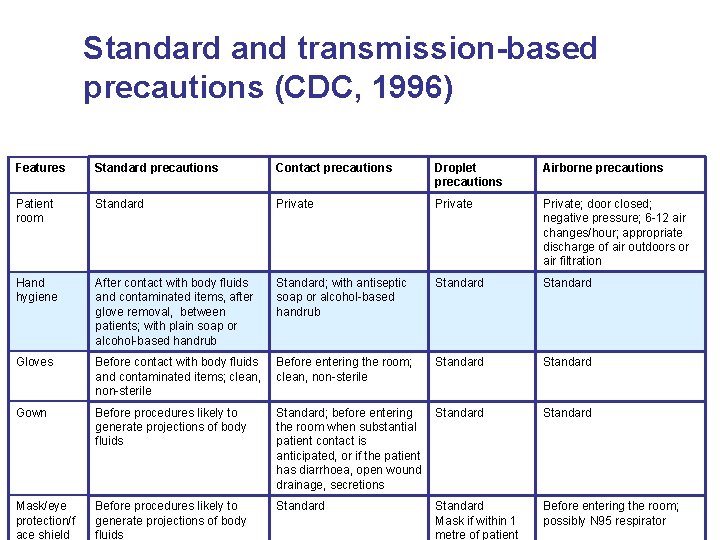
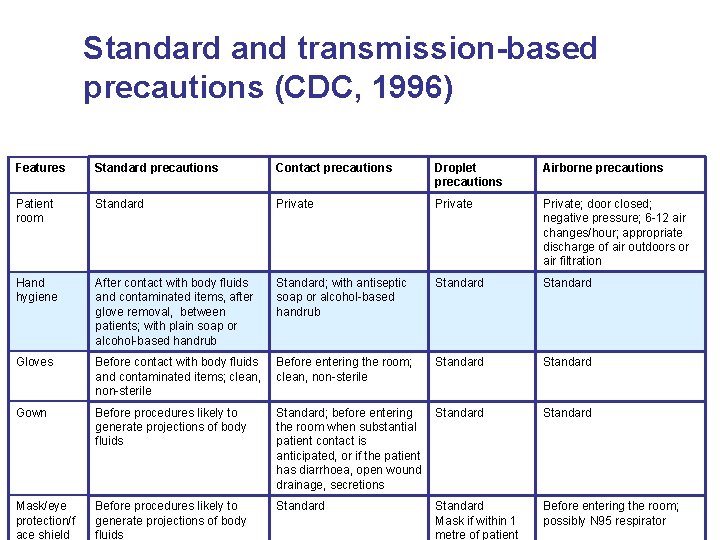
Standard and transmission-based precautions (CDC, 1996) Features Standard precautions Contact precautions Droplet precautions Airborne precautions Patient room Standard Private; door closed; negative pressure; 6 -12 air changes/hour; appropriate discharge of air outdoors or air filtration Hand hygiene After contact with body fluids and contaminated items, after glove removal, between patients; with plain soap or alcohol-based handrub Standard; with antiseptic soap or alcohol-based handrub Standard Gloves Before contact with body fluids and contaminated items; clean, non-sterile Before entering the room; clean, non-sterile Standard Gown Before procedures likely to generate projections of body fluids Standard; before entering the room when substantial patient contact is anticipated, or if the patient has diarrhoea, open wound drainage, secretions Standard Mask/eye protection/f ace shield Before procedures likely to generate projections of body fluids Standard Mask if within 1 metre of patient Before entering the room; possibly N 95 respirator
Simple evidence… Hand hygiene is the single most effective measure to reduce health care-associated infections
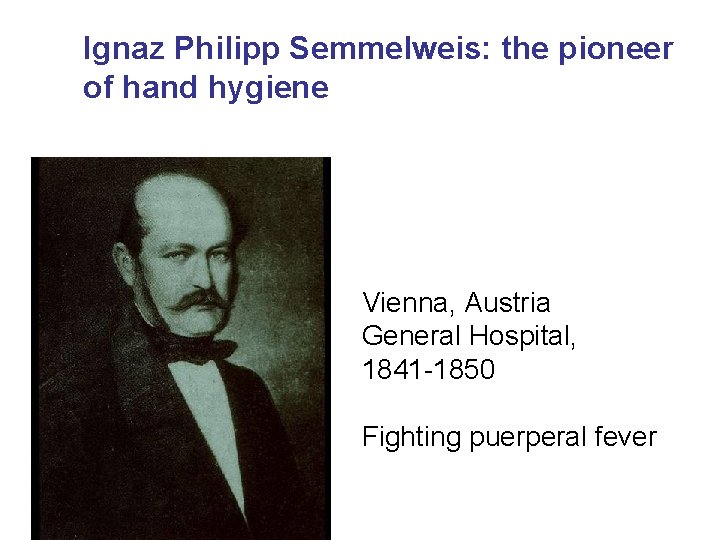
Ignaz Philipp Semmelweis: the pioneer of hand hygiene Vienna, Austria General Hospital, 1841 -1850 Fighting puerperal fever
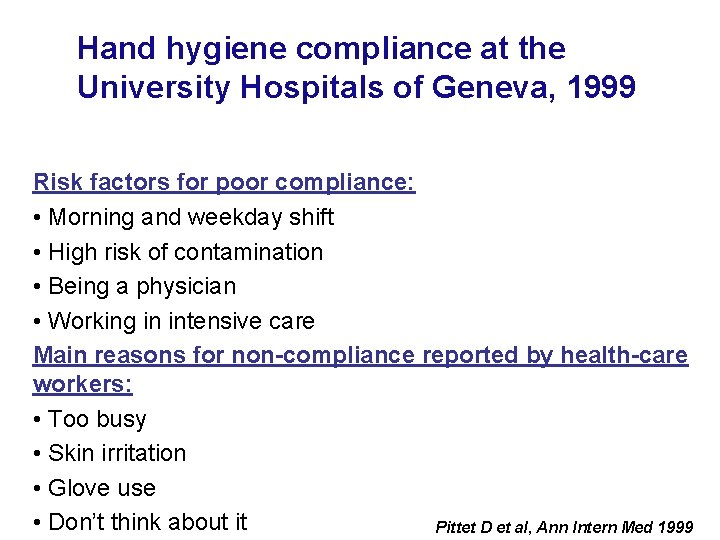
Hand hygiene compliance at the University Hospitals of Geneva, 1999 Risk factors for poor compliance: • Morning and weekday shift • High risk of contamination • Being a physician • Working in intensive care Main reasons for non-compliance reported by health-care workers: • Too busy • Skin irritation • Glove use • Don’t think about it Pittet D et al, Ann Intern Med 1999
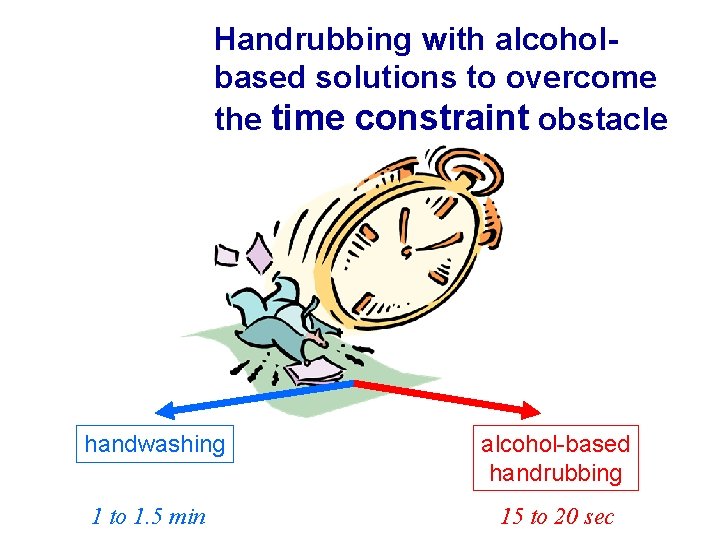
Time constraint = major obstacle for hand hygiene Adequate handwashing with water and soap requires: 1 to 1. 5 minutes Averages time usually adopted by health-care workers: < 10 secs
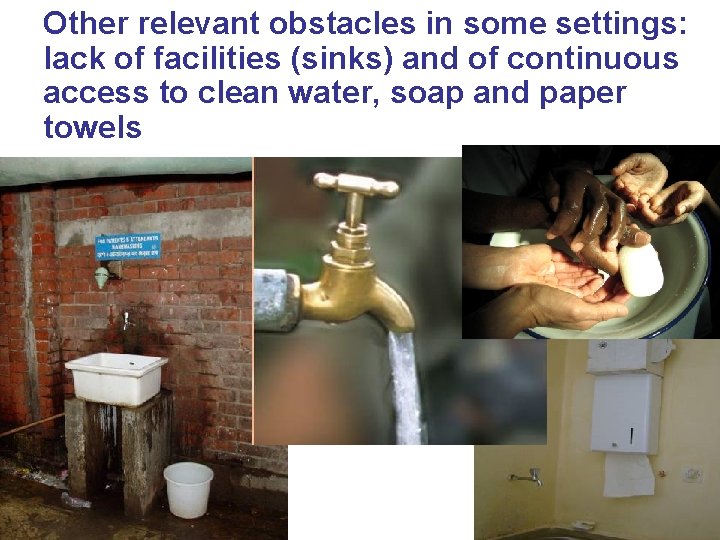
Other relevant obstacles in some settings: lack of facilities (sinks) and of continuous access to clean water, soap and paper towels
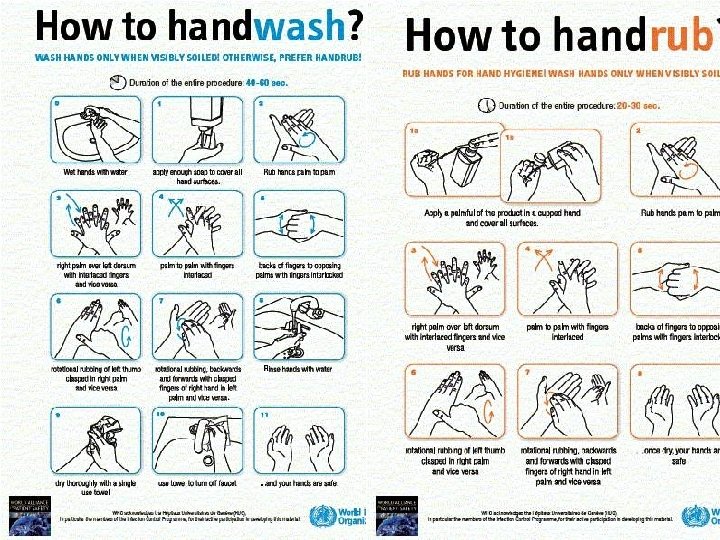
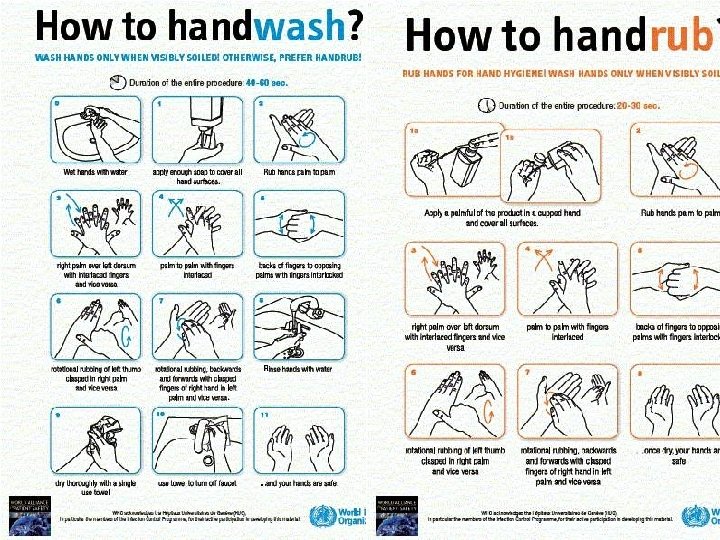
Handrubbing is the solution to obstacles to improve hand hygiene compliance • Handwashing with soap and water only when hands are visibly dirty or following visible exposure to body fluids • Adoption of alcoholbased handrub is the gold standard in all other clinical situations
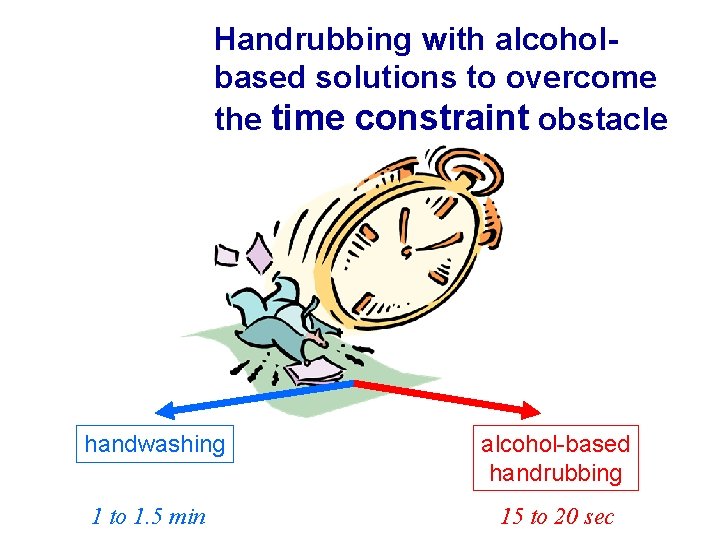
Handrubbing with alcoholbased solutions to overcome the time constraint obstacle handwashing alcohol-based handrubbing 1 to 1. 5 min 15 to 20 sec
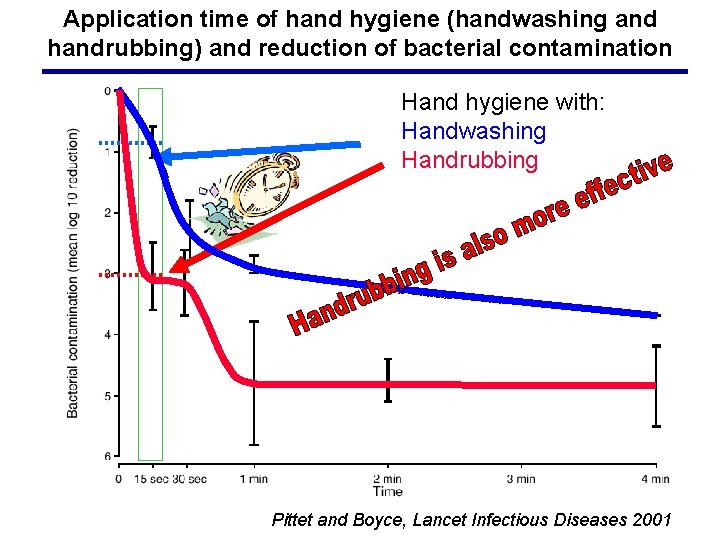
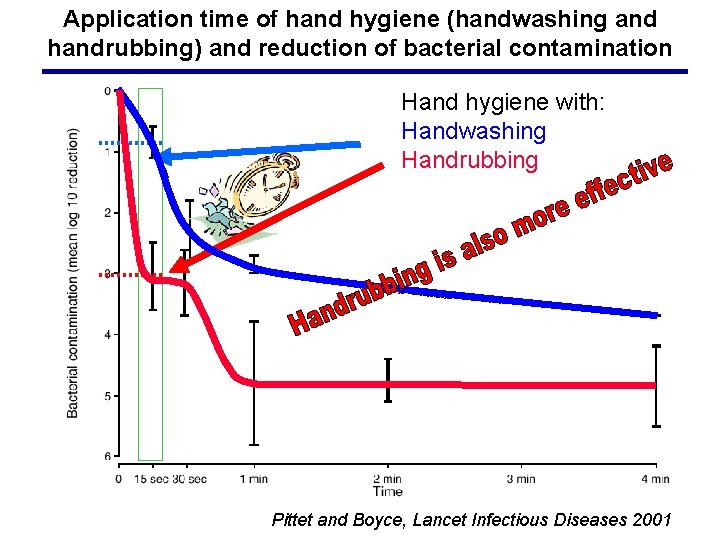
Application time of hand hygiene (handwashing and handrubbing) and reduction of bacterial contamination Hand hygiene with: Handwashing Handrubbing Pittet and Boyce, Lancet Infectious Diseases 2001
Part 4 The WHO Guidelines on Hand Hygiene in Health Care (Advanced Draft) and their implementation strategy and tools
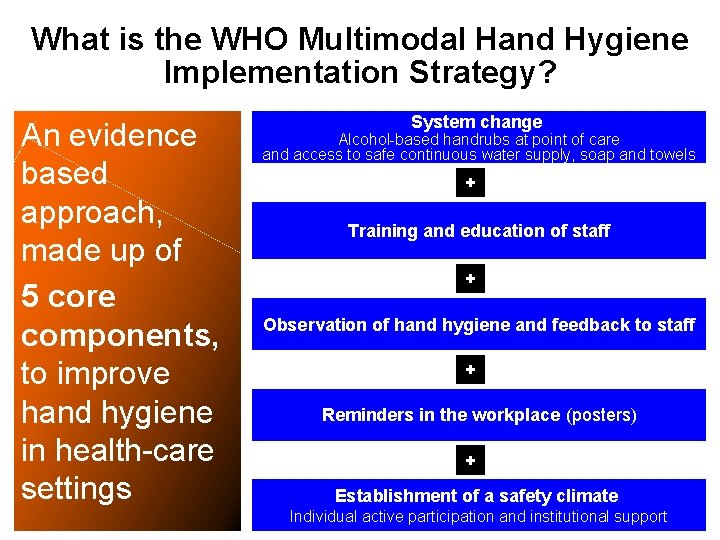
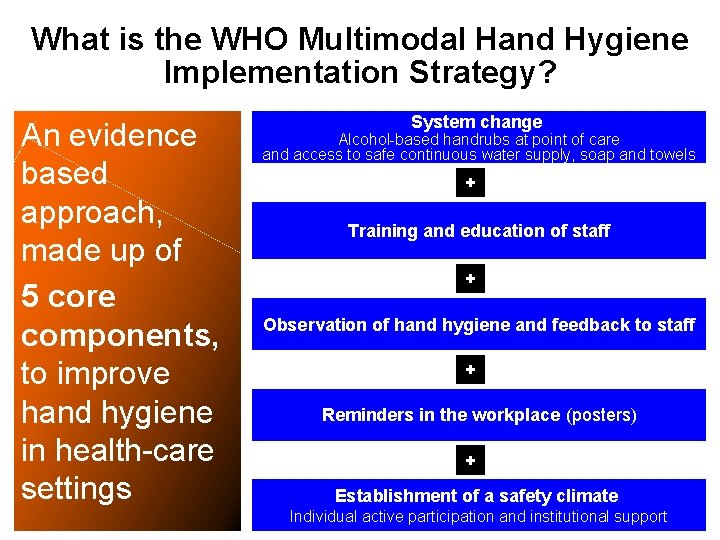
What is the WHO Multimodal Hand Hygiene Implementation Strategy? An evidence based approach, made up of 5 core components, to improve hand hygiene in health-care settings System change Alcohol-based handrubs at point of care and access to safe continuous water supply, soap and towels + Training and education of staff + Observation of hand hygiene and feedback to staff + Reminders in the workplace (posters) + Establishment of a safety climate Individual active participation and institutional support
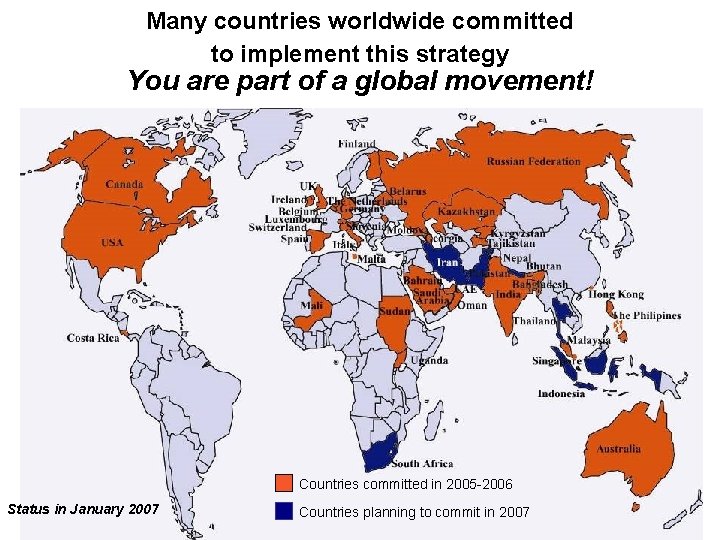
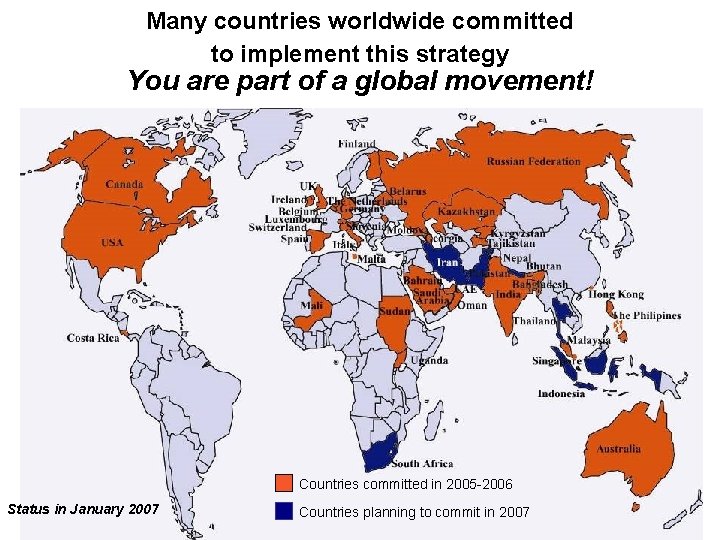
Many countries worldwide committed to implement this strategy You are part of a global movement! Countries committed in 2005 -2006 Status in January 2007 Countries planning to commit in 2007
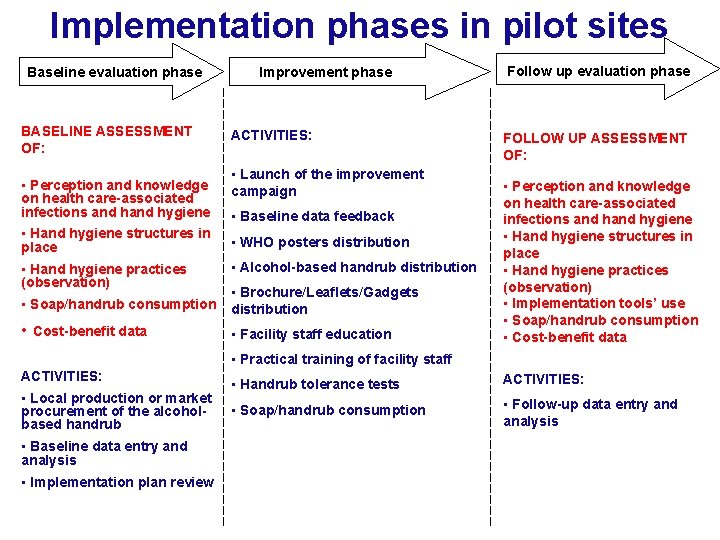
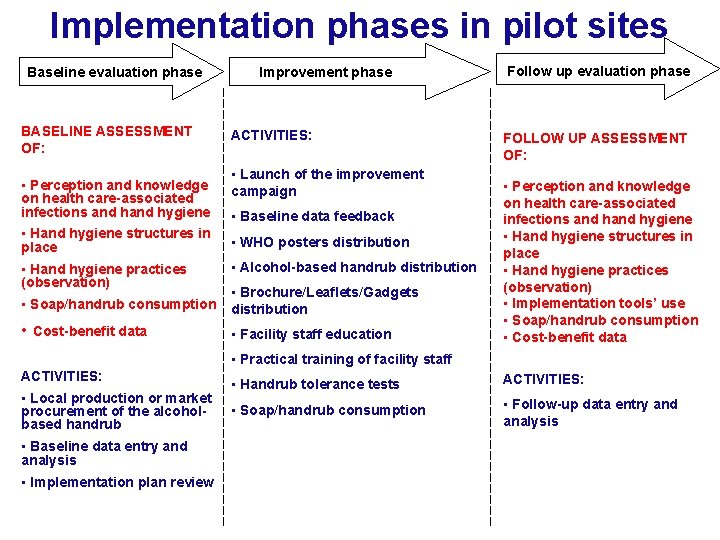
Implementation phases in pilot sites Baseline evaluation phase BASELINE ASSESSMENT OF: • Perception and knowledge on health care-associated infections and hygiene • Hand hygiene structures in place • Hand hygiene practices (observation) Improvement phase ACTIVITIES: • Launch of the improvement campaign • Baseline data feedback • WHO posters distribution • Alcohol-based handrub distribution • Soap/handrub consumption • Brochure/Leaflets/Gadgets distribution • Cost-benefit data • Facility staff education Follow up evaluation phase FOLLOW UP ASSESSMENT OF: • Perception and knowledge on health care-associated infections and hygiene • Hand hygiene structures in place • Hand hygiene practices (observation) • Implementation tools’ use • Soap/handrub consumption • Cost-benefit data • Practical training of facility staff ACTIVITIES: • Local production or market procurement of the alcoholbased handrub • Baseline data entry and analysis • Implementation plan review • Handrub tolerance tests ACTIVITIES: • Soap/handrub consumption • Follow-up data entry and analysis
Part 5 Why, when and how you should perform hand hygiene in health care
Why should you clean your hands? • Any health-care worker, caregiver or person involved in patient care needs to be concerned about hand hygiene • Therefore hand hygiene does concern you! • You must perform hand hygiene: 1) to protect the patient against harmful germs carried on your hands or present on his/her own skin 2) to protect yourself and the health-care environment from harmful germs
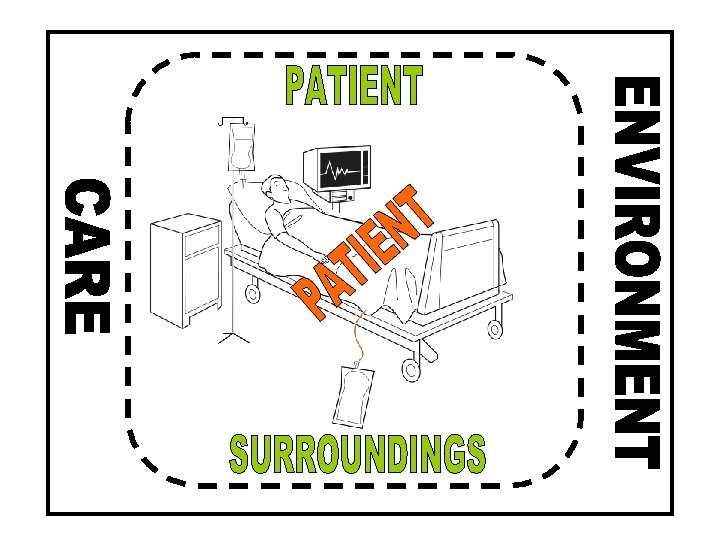
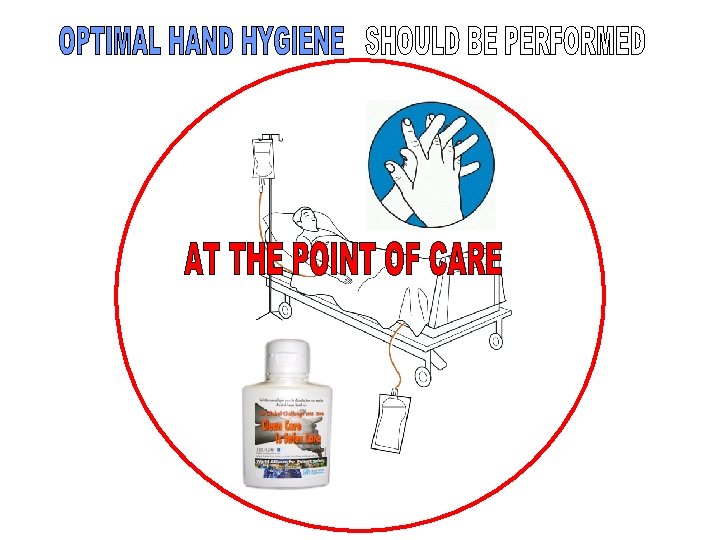
The golden rules for hand hygiene • Hand hygiene must be performed exactly where you are delivering health care to patients (at the point of care) • During health-care delivery, there are 5 moments when it is essential that you perform hand hygiene • To clean your hands, you should prefer handrubbing with an alcohol-based formulation, if available. Why? Because it is possible right at the point of care, it is faster, and it is more effective, and better tolerated. You should wash your hands with soap and water only when visibly soiled • You must perform hand hygiene using the appropriate technique and time duration
THE 5 STEPS OF HAND TRANSMISSION Pittet D et al, Lancet Infect Dis, Oct 2006
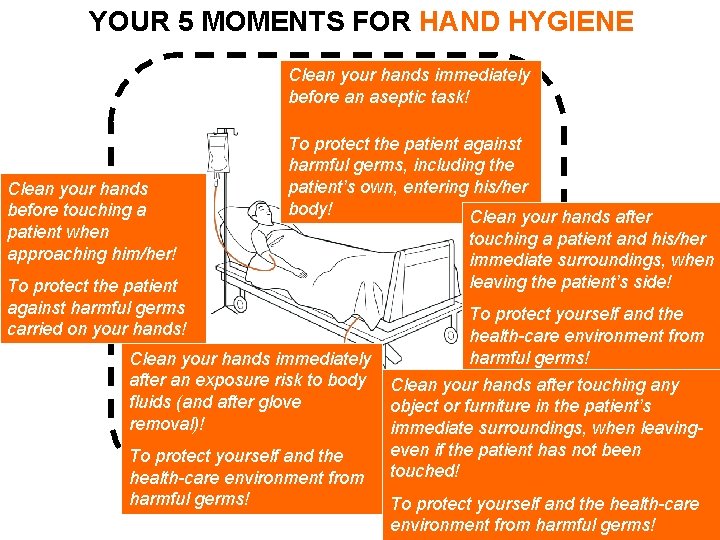
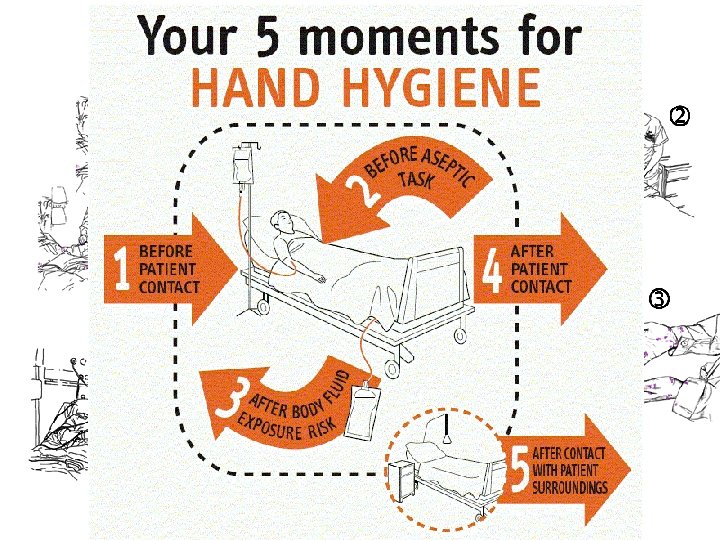
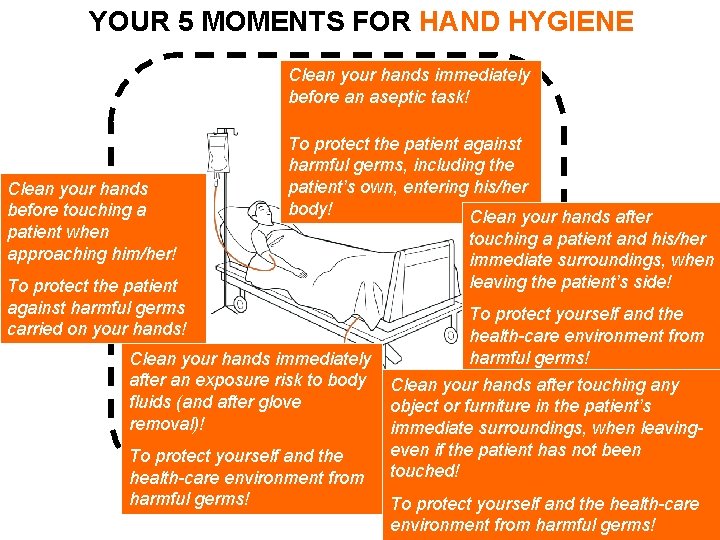
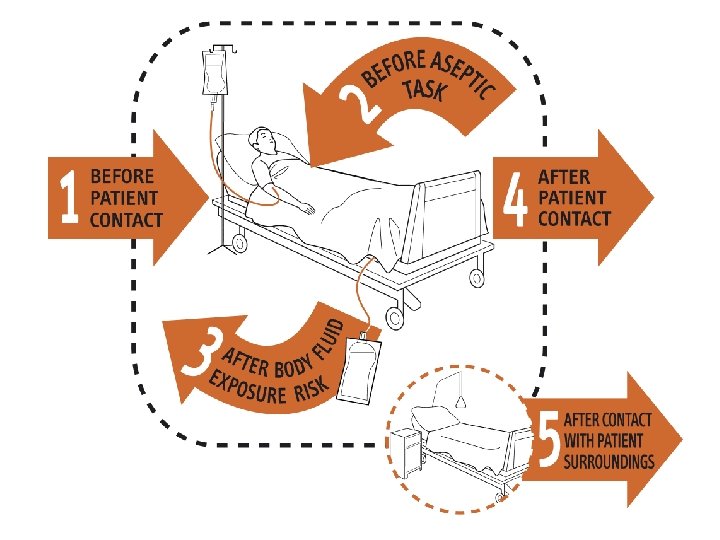
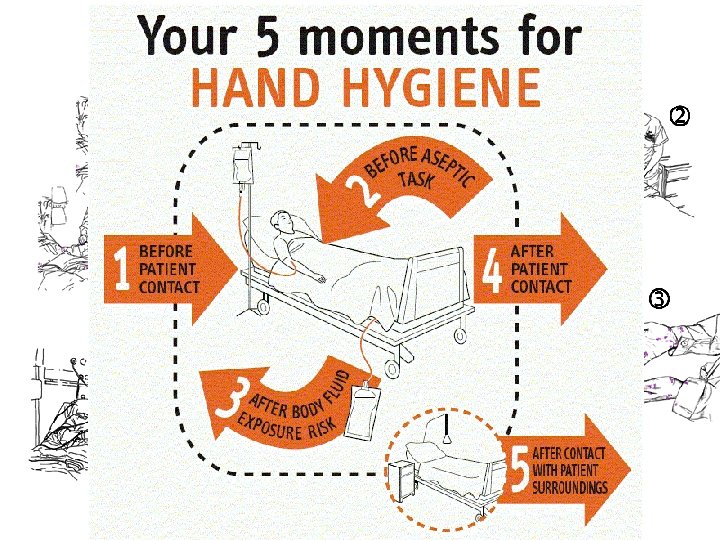
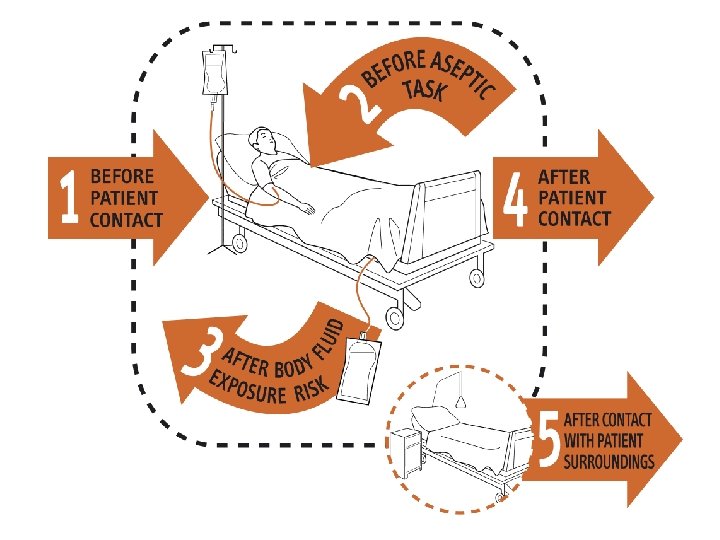
YOUR 5 MOMENTS FOR HAND HYGIENE Clean your hands immediately before an aseptic task! Clean your hands before touching a patient when approaching him/her! To protect the patient against harmful germs, including the patient’s own, entering his/her body! Clean your hands after To protect the patient against harmful germs carried on your hands! Clean your hands immediately after an exposure risk to body fluids (and after glove removal)! To protect yourself and the health-care environment from harmful germs! touching a patient and his/her immediate surroundings, when leaving the patient’s side! To protect yourself and the health-care environment from harmful germs! Clean your hands after touching any object or furniture in the patient’s immediate surroundings, when leavingeven if the patient has not been touched! To protect yourself and the health-care environment from harmful germs!
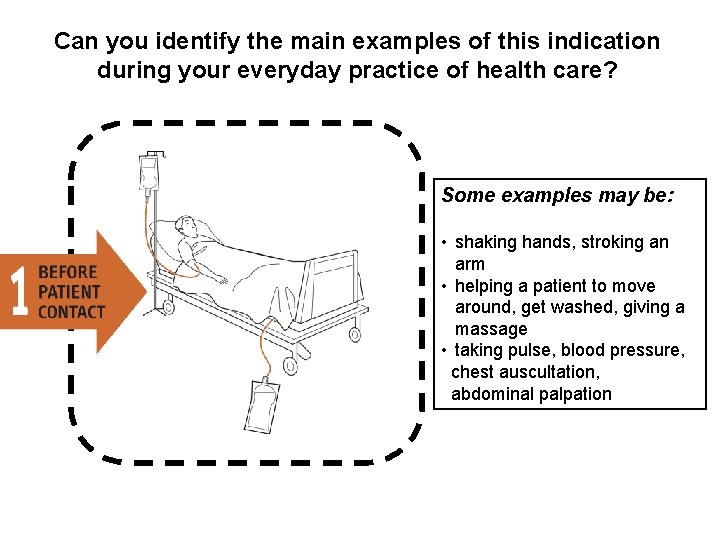
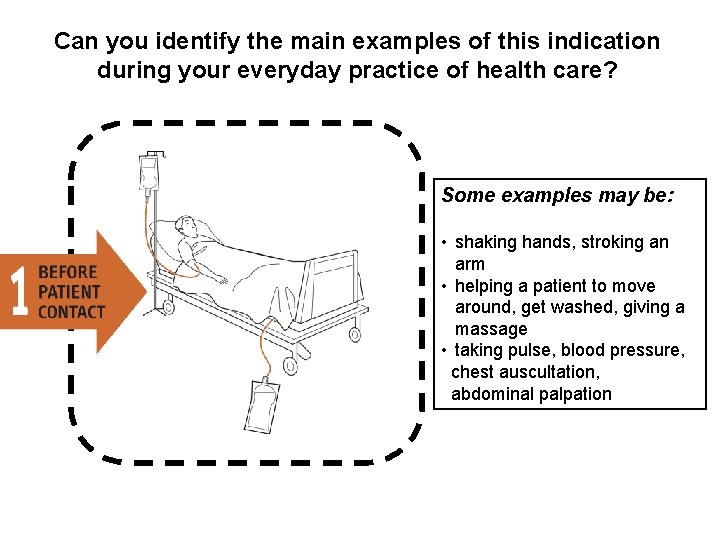
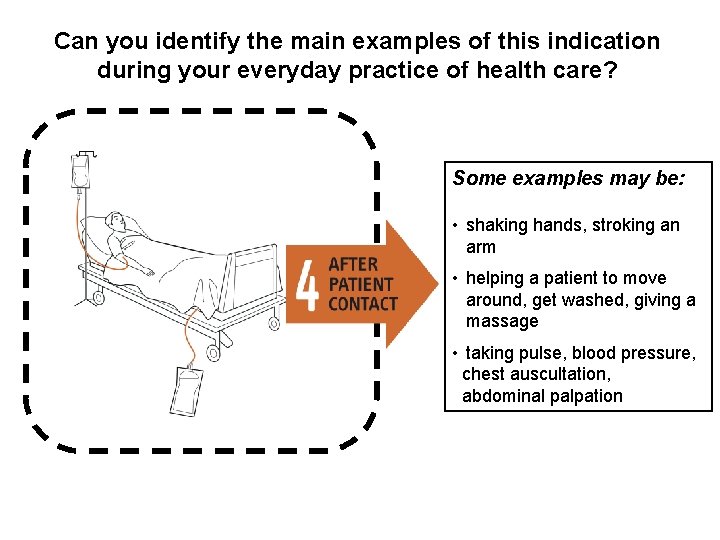
Can you identify the main examples of this indication during your everyday practice of health care? Some examples may be: • shaking hands, stroking an arm • helping a patient to move around, get washed, giving a massage • taking pulse, blood pressure, chest auscultation, abdominal palpation
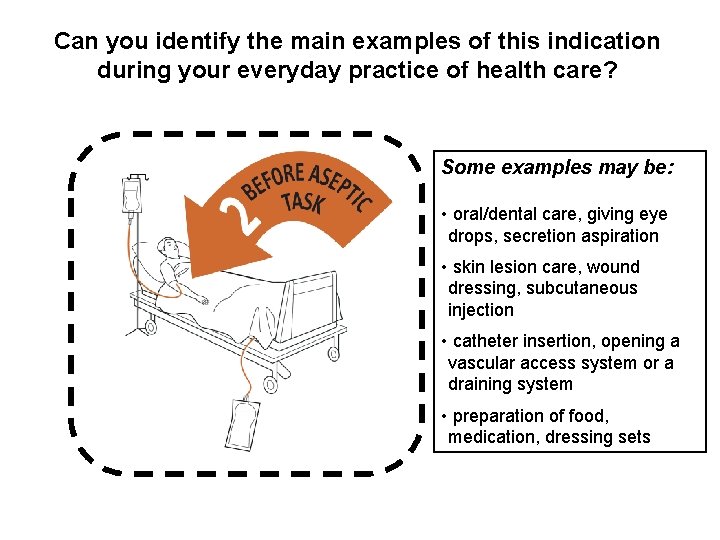
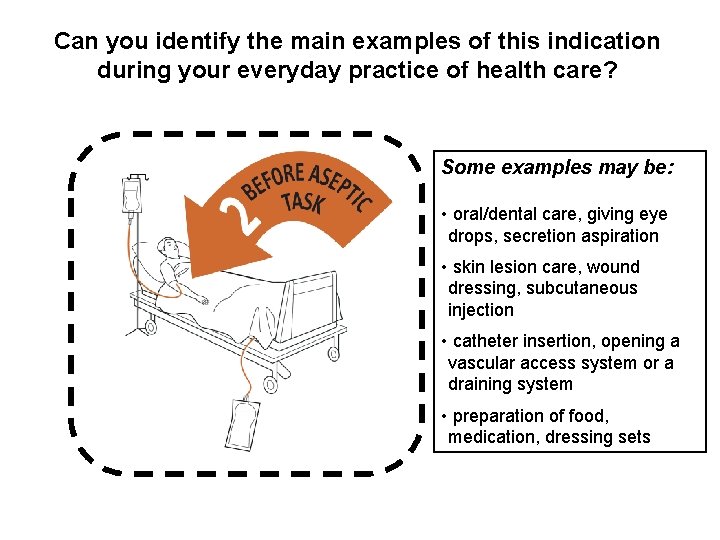
Can you identify the main examples of this indication during your everyday practice of health care? Some examples may be: • oral/dental care, giving eye drops, secretion aspiration • skin lesion care, wound dressing, subcutaneous injection • catheter insertion, opening a vascular access system or a draining system • preparation of food, medication, dressing sets
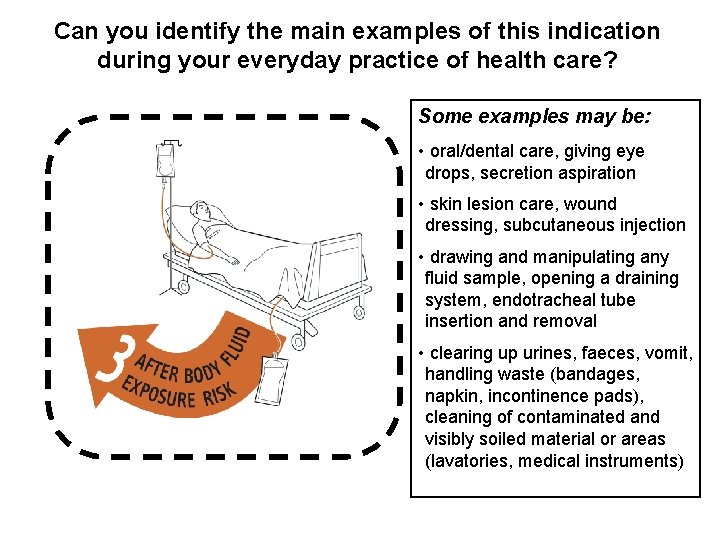
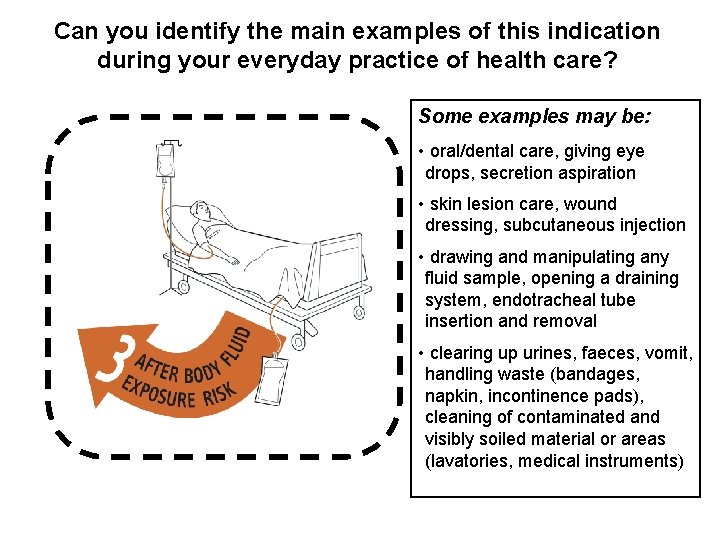
Can you identify the main examples of this indication during your everyday practice of health care? Some examples may be: • oral/dental care, giving eye drops, secretion aspiration • skin lesion care, wound dressing, subcutaneous injection • drawing and manipulating any fluid sample, opening a draining system, endotracheal tube insertion and removal • clearing up urines, faeces, vomit, handling waste (bandages, napkin, incontinence pads), cleaning of contaminated and visibly soiled material or areas (lavatories, medical instruments)
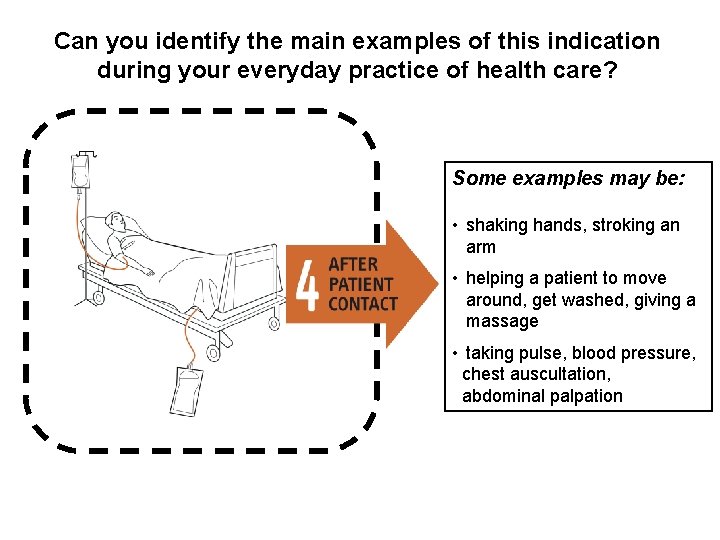
Can you identify the main examples of this indication during your everyday practice of health care? Some examples may be: • shaking hands, stroking an arm • helping a patient to move around, get washed, giving a massage • taking pulse, blood pressure, chest auscultation, abdominal palpation
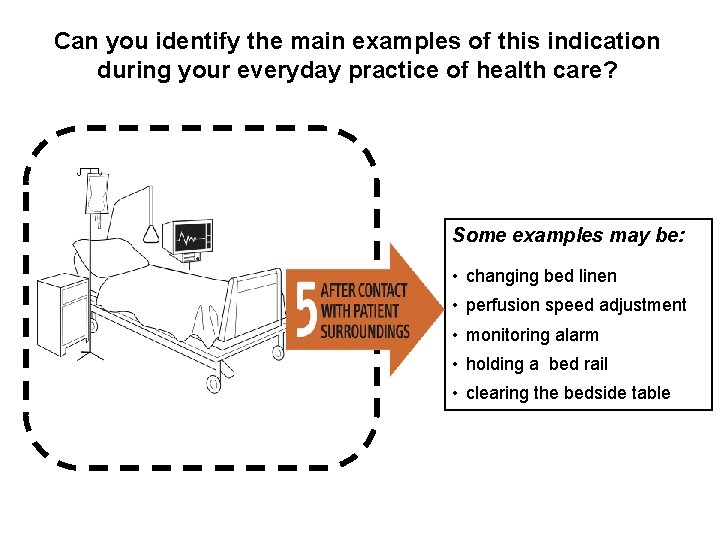
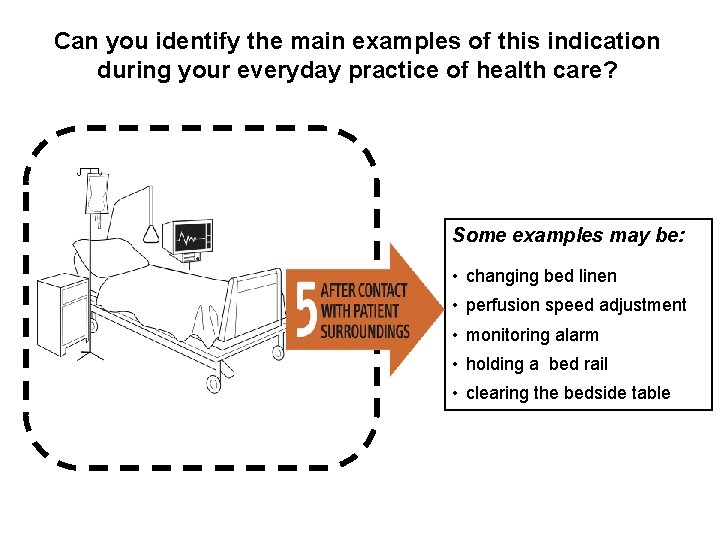
Can you identify the main examples of this indication during your everyday practice of health care? Some examples may be: • changing bed linen • perfusion speed adjustment • monitoring alarm • holding a bed rail • clearing the bedside table
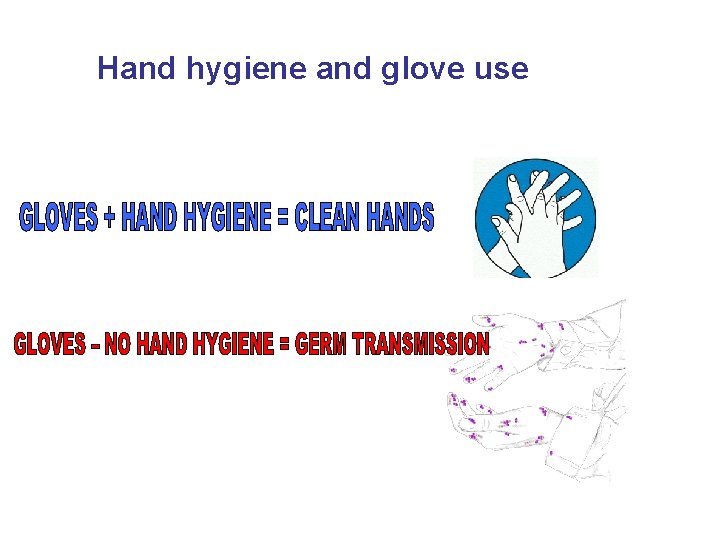
Hand hygiene and glove use
Hand Hygiene should some times be supplemented with gloves: Gloves must be worn according to STANDARD and CONTACT - STERILE GLOVES INDICATED - CLEAN GLOVES INDICATED IN CLINICAL SITUATIONS
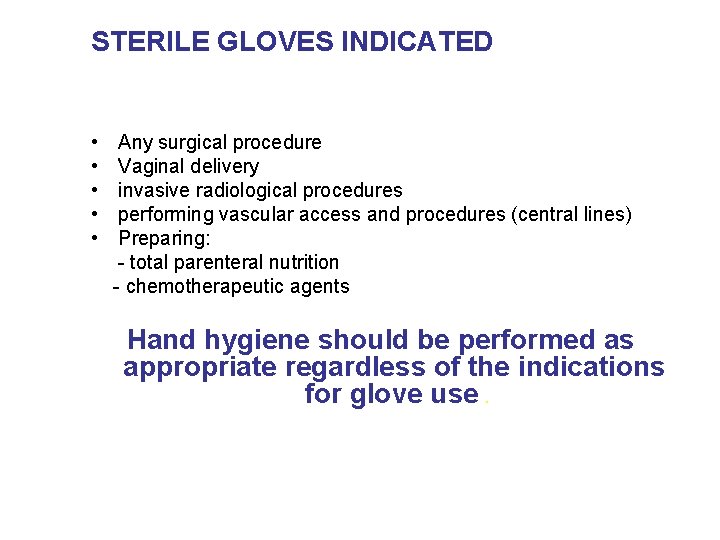
STERILE GLOVES INDICATED • • • Any surgical procedure Vaginal delivery invasive radiological procedures performing vascular access and procedures (central lines) Preparing: - total parenteral nutrition - chemotherapeutic agents Hand hygiene should be performed as appropriate regardless of the indications for glove use.
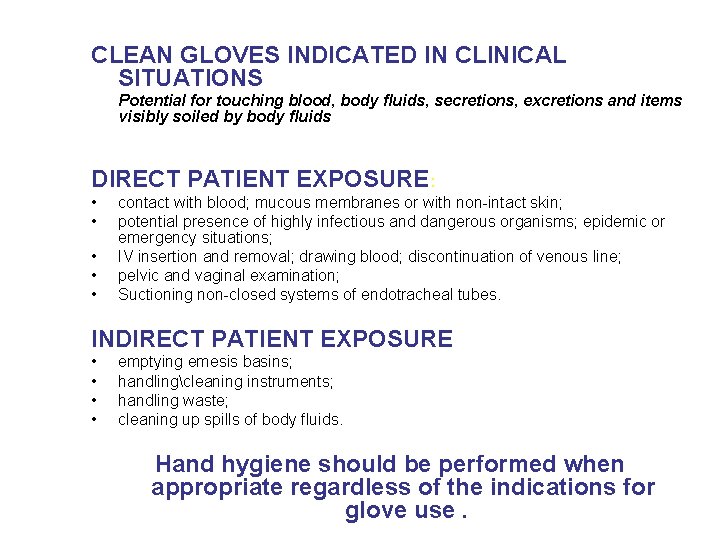
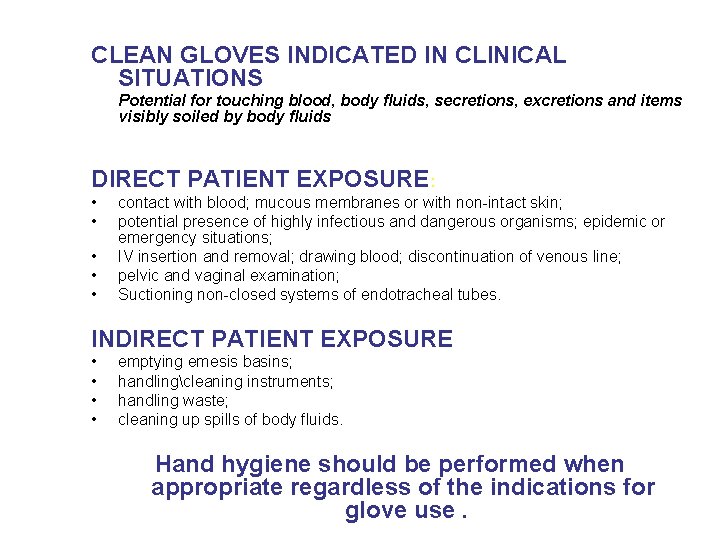
CLEAN GLOVES INDICATED IN CLINICAL SITUATIONS Potential for touching blood, body fluids, secretions, excretions and items visibly soiled by body fluids DIRECT PATIENT EXPOSURE: • • • contact with blood; mucous membranes or with non-intact skin; potential presence of highly infectious and dangerous organisms; epidemic or emergency situations; IV insertion and removal; drawing blood; discontinuation of venous line; pelvic and vaginal examination; Suctioning non-closed systems of endotracheal tubes. INDIRECT PATIENT EXPOSURE • • emptying emesis basins; handlingcleaning instruments; handling waste; cleaning up spills of body fluids. Hand hygiene should be performed when appropriate regardless of the indications for glove use.
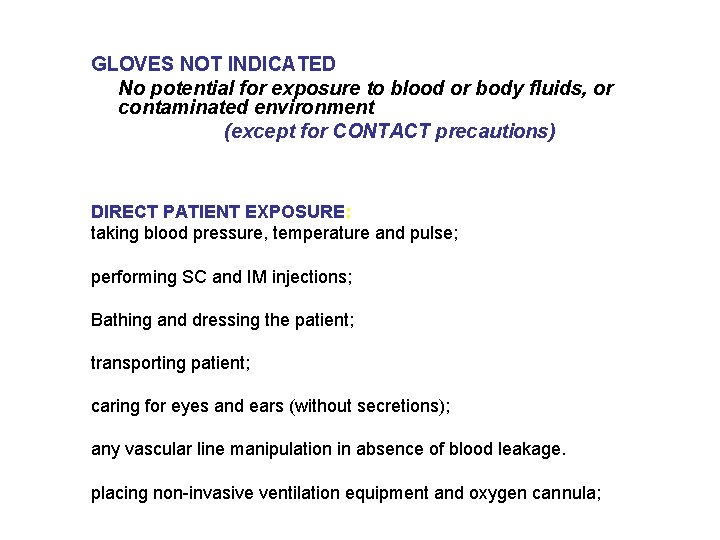
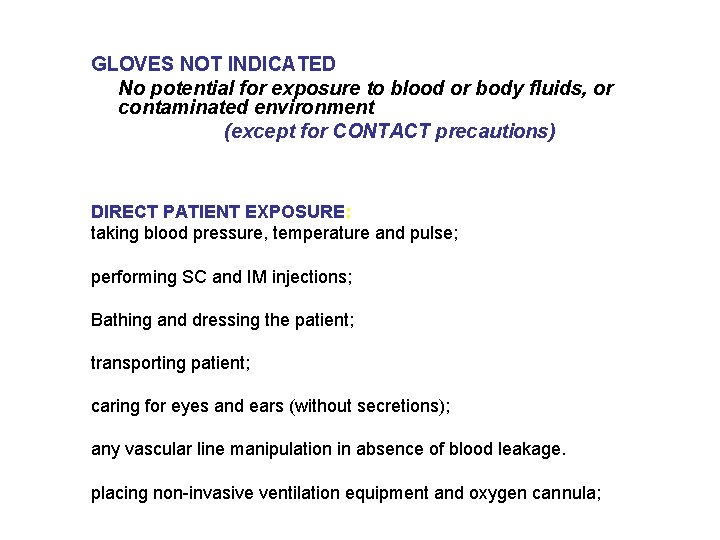
GLOVES NOT INDICATED No potential for exposure to blood or body fluids, or contaminated environment (except for CONTACT precautions) DIRECT PATIENT EXPOSURE: taking blood pressure, temperature and pulse; performing SC and IM injections; Bathing and dressing the patient; transporting patient; caring for eyes and ears (without secretions); any vascular line manipulation in absence of blood leakage. placing non-invasive ventilation equipment and oxygen cannula;
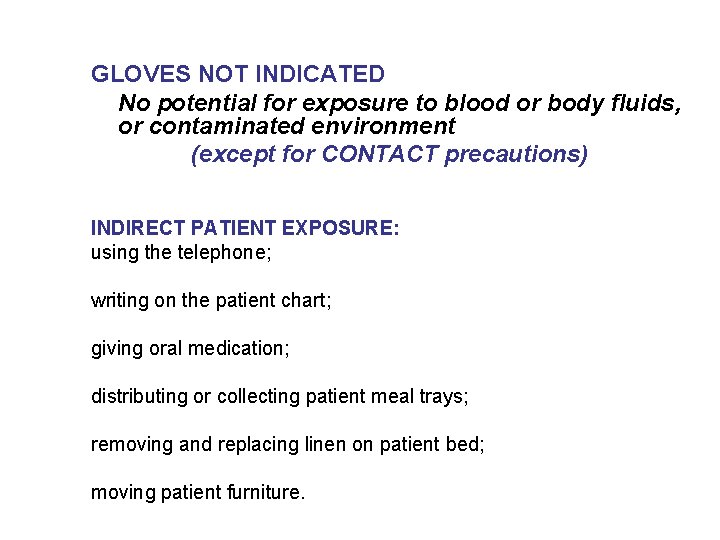
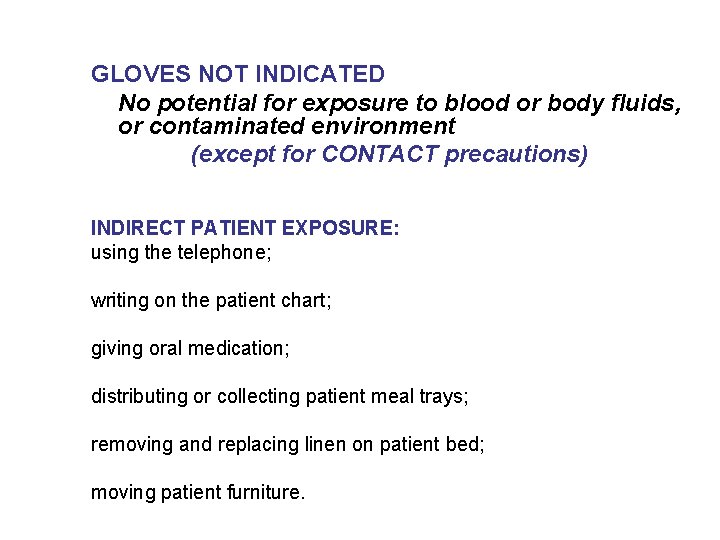
GLOVES NOT INDICATED No potential for exposure to blood or body fluids, or contaminated environment (except for CONTACT precautions) INDIRECT PATIENT EXPOSURE: using the telephone; writing on the patient chart; giving oral medication; distributing or collecting patient meal trays; removing and replacing linen on patient bed; moving patient furniture.
Hand hygiene and glove use • The use of gloves does not replace the need of cleaning your hands! • You should remove gloves to perform hand hygiene, when an indication occurs while wearing gloves • You should wear gloves only when indicated otherwise they become a major risk for germ transmission

It is now possible to improve hand hygiene in your facility! It’s your duty, to protect patients and yourself! You can make a change! Easy infection control for everyone… simple measures save lives!
Part 6 How to observe hand hygiene practices among health-care workers Observers should carefully read the "Manual for Observers" before undergoing this training session
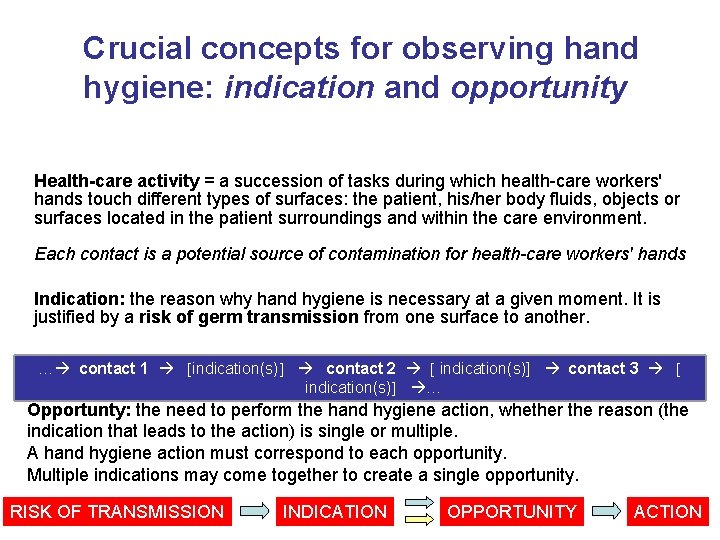
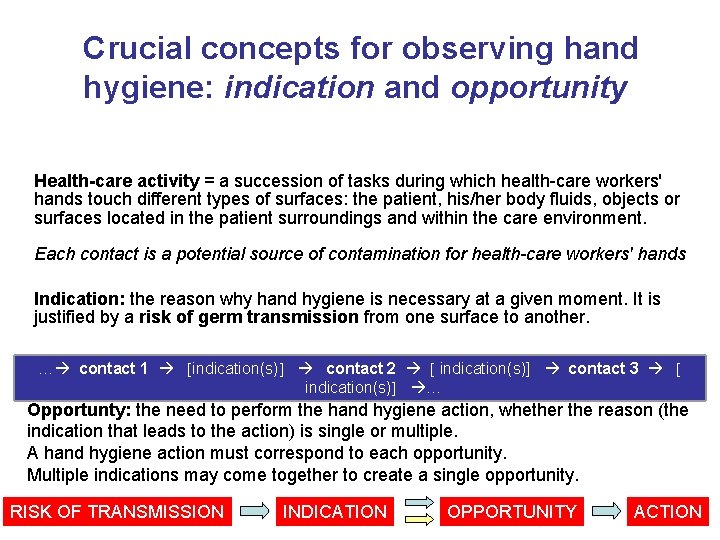
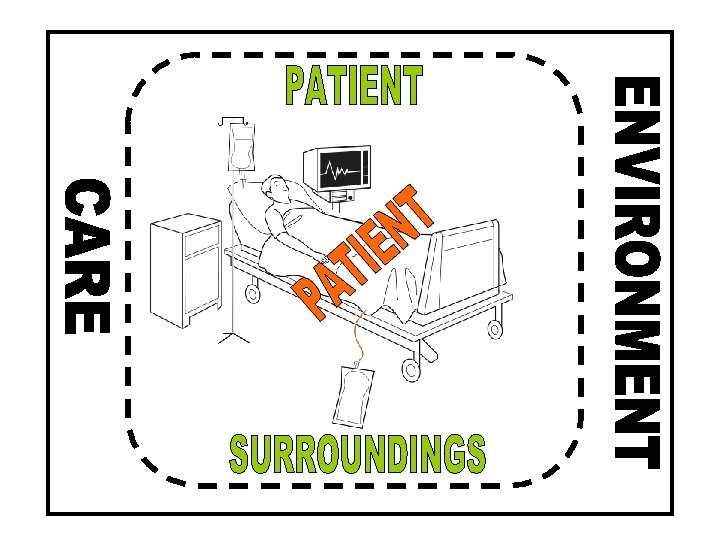
Crucial concepts for observing hand hygiene: indication and opportunity Health-care activity = a succession of tasks during which health-care workers' hands touch different types of surfaces: the patient, his/her body fluids, objects or surfaces located in the patient surroundings and within the care environment. Each contact is a potential source of contamination for health-care workers' hands Indication: the reason why hand hygiene is necessary at a given moment. It is justified by a risk of germ transmission from one surface to another. … contact 1 indication(s) contact 2 indication(s)] contact 3 indication(s) … Opportunty: the need to perform the hand hygiene action, whether the reason (the indication that leads to the action) is single or multiple. A hand hygiene action must correspond to each opportunity. Multiple indications may come together to create a single opportunity. RISK OF TRANSMISSION INDICATION OPPORTUNITY ACTION
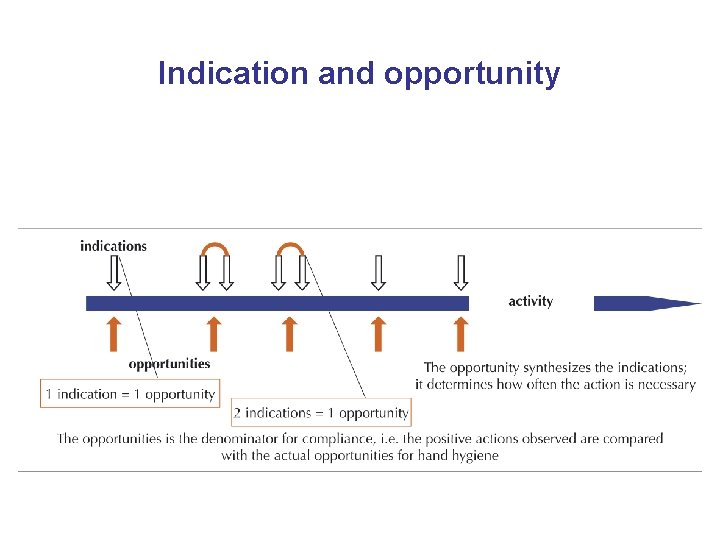
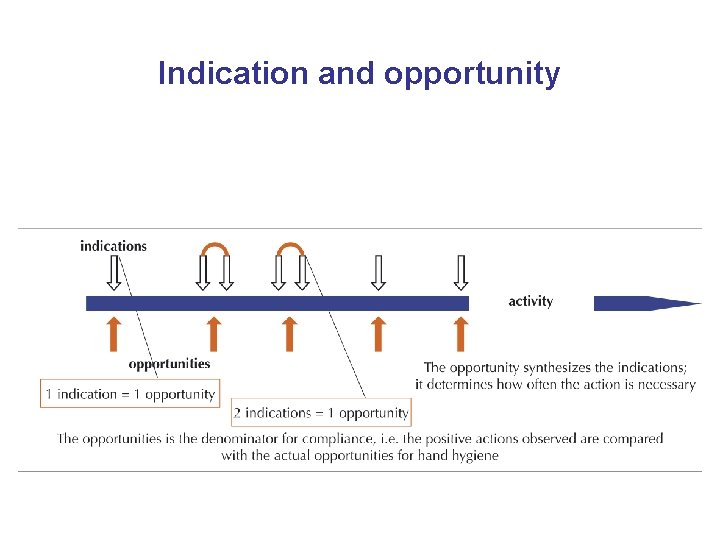
Indication and opportunity
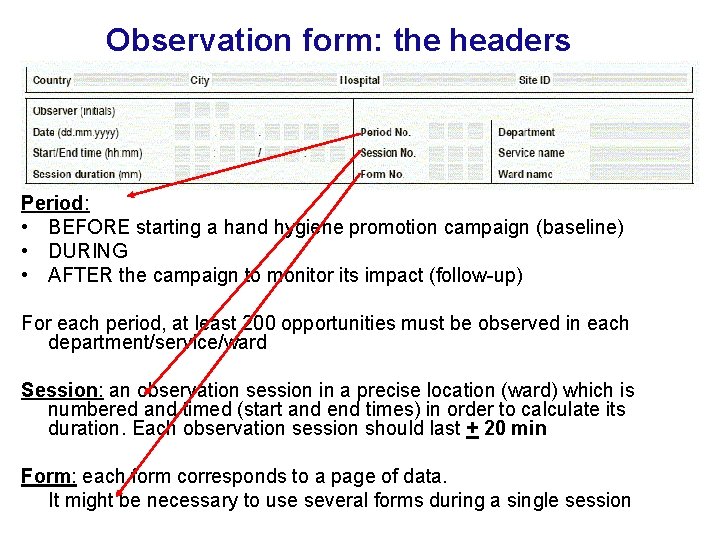
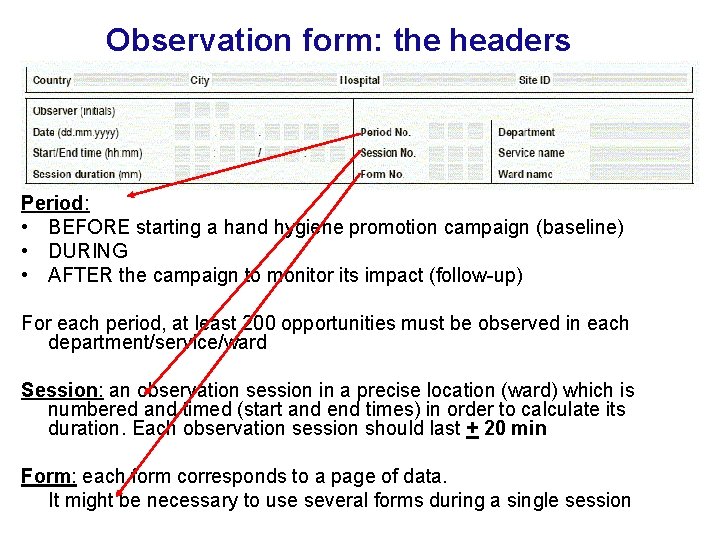
Observation form: the headers Period: • BEFORE starting a hand hygiene promotion campaign (baseline) • DURING • AFTER the campaign to monitor its impact (follow-up) For each period, at least 200 opportunities must be observed in each department/service/ward Session: an observation session in a precise location (ward) which is numbered and timed (start and end times) in order to calculate its duration. Each observation session should last + 20 min Form: each form corresponds to a page of data. It might be necessary to use several forms during a single session
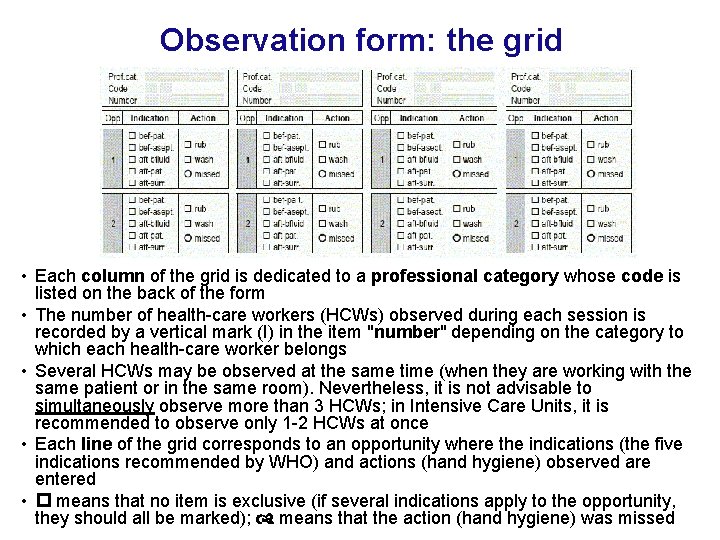
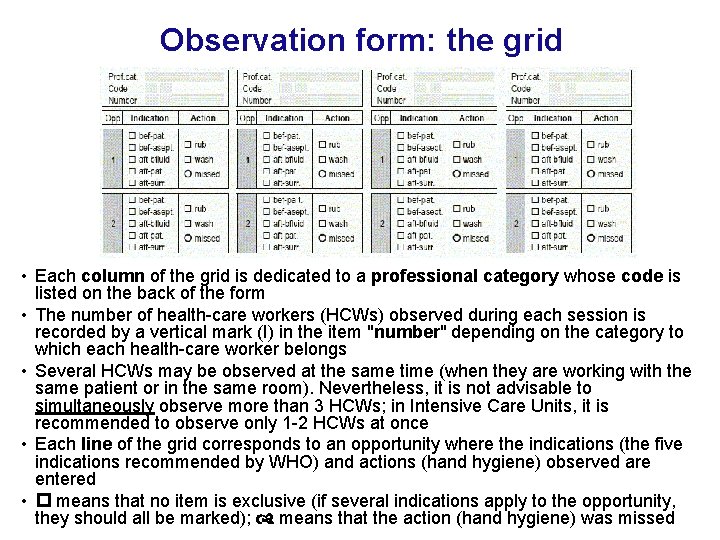
Observation form: the grid • Each column of the grid is dedicated to a professional category whose code is listed on the back of the form • The number of health-care workers (HCWs) observed during each session is recorded by a vertical mark (I) in the item "number" depending on the category to which each health-care worker belongs • Several HCWs may be observed at the same time (when they are working with the same patient or in the same room). Nevertheless, it is not advisable to simultaneously observe more than 3 HCWs; in Intensive Care Units, it is recommended to observe only 1 -2 HCWs at once • Each line of the grid corresponds to an opportunity where the indications (the five indications recommended by WHO) and actions (hand hygiene) observed are entered • means that no item is exclusive (if several indications apply to the opportunity, they should all be marked); means that the action (hand hygiene) was missed