WHO evidence and guidance for salt iodization salt
- Slides: 19
WHO evidence and guidance for salt iodization & salt reduction Dr Lisa M. Rogers Technical officer, Evidence and Programme Guidance Unit Department of Nutrition for Health and Development WHO Geneva Achieving Universal Salt Iodisation for Optimal Iodine Nutrition in the East Asia and Pacific Region 12 -14 October 2015, Bangkok, Thailand
Outline • World Health Assembly (WHA) resolutions • Systematic review on salt iodization • WHO guidance on salt iodization • Compatibility of salt reduction and salt iodization strategies
WHA resolutions • In 1990, the 43 rd WHA adopted the goal of eliminating iodine deficiency as a public health problem • In 1996, 49 th WHA reaffirms the goal of eliminating IDD as a major public health problem in all countries • In 2005, the 58 th WHA adopted a resolution (WHA 58. 24) committing WHO to report on the global situation of IDD every 3 years • In 2013, the 66 th WHA further recognized that USI remains the preferred strategy for the control of IDD ‒ • Countries should continue to recognize the importance of iodized salt for preventing IDD while working to reduce total salt intake In 2013, the 66 th WHA agreed on a voluntary global NCD target for a 30% relative reduction in the mean population intake of salt by 2025 (resolution 66. 10)
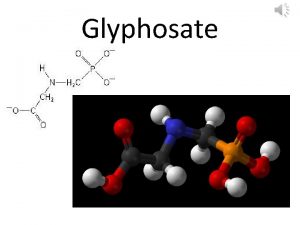
Salt as a vehicle fortification • Salt is an appropriate vehicle fortification with iodine ‒ Widely consumed by virtually all population groups in all countries ‒ In many countries, salt production is limited to a few centres, facilitating quality control ‒ The technological needs of salt iodization are well established and relatively inexpensive ‒ The addition of iodine to salt does not affect the taste or smell of the salt or foods containing iodized salt ‒ The concentration of iodine in salt can easily be adjusted to meet policies aimed at reducing the consumption of salt in order to prevent cardiovascular disease
WHO guidance • Salt iodization has been the preferred strategy for the control of iodine deficiency disorders • To provide 150 µg/day of iodine via iodized salt, iodine concentration in salt at the point of production should be within the range of 20 -40 mg of iodine per kg of salt (1996) ‒ Based on the assumptions that the average salt intake is 10 g/day • Updated guidance needed using procedures outlined in the WHO handbook for guideline development
Salt iodization review • Systematically reviewed the effectiveness and safety of iodized salt for the prevention of iodine deficiency disorders • Primary outcomes • ‒ ‒ ‒ ‒ ‒ Goitre* Cretinism* Mental development Cognitive function* Hypothyroidism* Hyperthyroidism* Secondary outcomes Urinary iodine excretion* Thyroid hormones Physical development Other adverse effects Aburto NJ, Abudou M, Candeias V, Wu T. Geneva: World Health Organization; 2014 (http: //apps. who. int/iris/bitstream/10665/148175/1/9789241508285_eng. pdf? ua=1)
Main findings • Populations receiving iodized salt: ‒ Reduced risk of goitre by 41 -82% o Risk of goitre reduced regardless of age group or concentration of iodine in salt (20 -40 ppm) ‒ Reduced odds of cretinism ‒ Improved cognitive function when exposed during gestation, infancy and early childhood o Increased intelligence quotient (IQ) by 8 -10 points o Decreased risk of inadequate IQ (IQ <70) by ~75% ‒ Increased intake of iodine o Increased urinary iodine excretion o Decreased risk of iodine insufficiency (UIC <100 ug/L) by 55 -60% Aburto NJ, Abudou M, Candeias V, Wu T. Geneva: World Health Organization; 2014.
Main findings • Potential adverse effects ‒ Hypothyroidism – no overall effect ‒ Hyperthyroidism o o Few events, results varied by study design Long-term studies suggest any increase in prevalence is temporary ‒ However, as with any intervention, potentially serious adverse effects may occur in some individuals with the introduction of salt iodization at the population level o Programmes should have a robust monitoring and evaluation system in place
Updated WHO guideline • All food-grade salt, used in household and food processing, should be fortified with iodine as a safe and effective strategy for the prevention and control of iodine deficiency disorders in populations living in stable and emergency settings (strong recommendation)
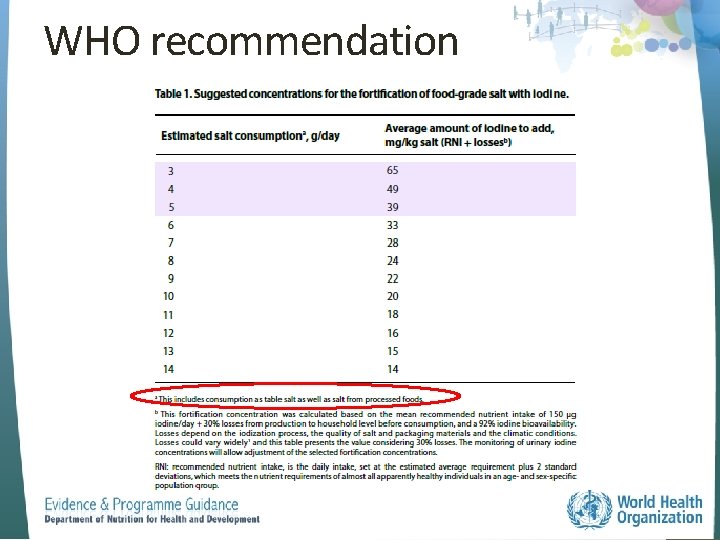
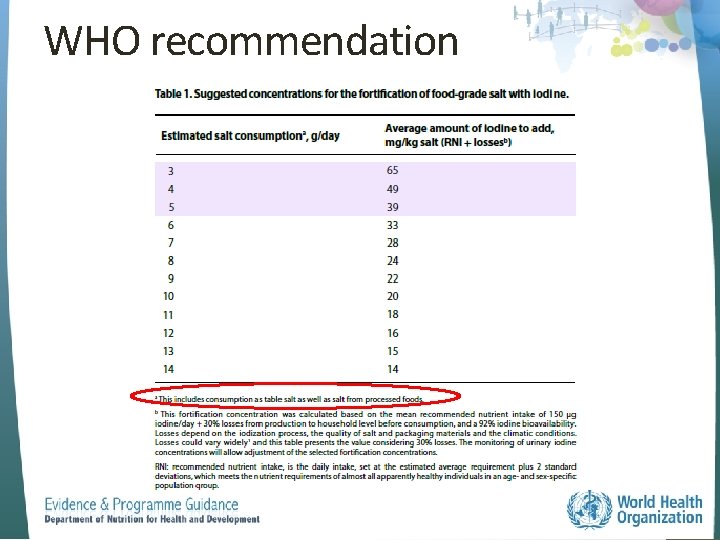
WHO recommendation
WHO recommendation • Iodization was calculated based on: ‒ Mean RNI of 150 μg iodine/day + ‒ 30% losses from production to household level before consumption ‒ 92% iodine bioavailability o • Losses depend on the iodization process, quality of salt and packaging materials, and climatic conditions. Losses could vary widely (30% assumed here). An estimated additional variability of ± 10% during iodization procedures could be considered at the production site for use in quality control and assurance procedures. This variability depends on the iodization methods used and quality assurance system in place. RNI = recommended nutrient intake
Remarks on recommendation • ‒ ‒ Policies for salt iodization and reduction of salt to <5 g/day are compatible, cost effective and of great public health benefit Iodization of salt should not justify promotion of salt intake National data on salt consumption must provide key guidance for the concentration of iodine in salt • Iodized salt should reach, and be used by, all members of the population after 1 year of age ‒ Infants and young children are assumed to be covered via breast milk or iodine-enriched infant formula milk when this is prescribed
Remarks on recommendation • Since pregnant women have a daily iodine requirement of 250 μg/day, other interventions such as iodine supplementation could be considered if iodine inadequacy is found. • Fortification of salt with iodine should be harmonized with other local or country programmes to ensure that iodine is delivered safely within the acceptable dosage range.
Remarks on recommendation • Clear legislation should also be established for food producers and distributors, especially where the main source of dietary salt is processed foods and meals consumed outside households. • Monitoring of food-grade salt quality is essential to ensure both efficacy and safety of the process of iodine fortification. ‒ Monitoring of UIE or UIC is useful to detect both deficiency and excessive intakes.
WHO guideline in e. LENA www. who. int/elena/titles/salt_iodization/en/
Reduction of salt intake • Salt is the main dietary source of sodium and a high intake of sodium has been associated with hypertension, cardiovascular disease and stroke • Decreasing sodium intake may reduce blood pressure and the risk of associated noncommunicable diseases • WHO currently recommends a reduction to <2 g/day sodium (5 g/day salt) in all adults • Adoption of the Global Monitoring Framework and Voluntary Global Targets for the Prevention and Control of NCDs, with a global target of a 30% relative reduction in mean population intake of salt/sodium by 2025
Salt reduction and salt iodization • WHO affirms that the policies on salt reduction and salt iodization are compatible • Monitoring of salt intake and salt iodization at the country level is needed to adjust salt iodization over time as necessary, depending on the observed salt intake in the population • There are opportunities to synergize both programmes
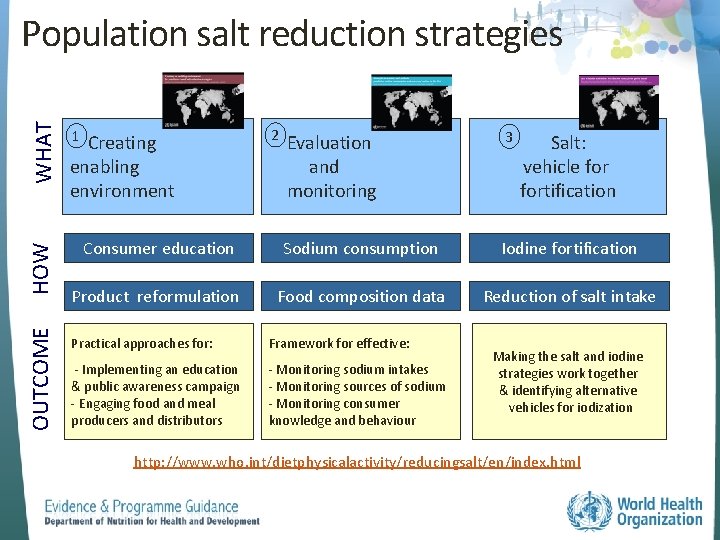
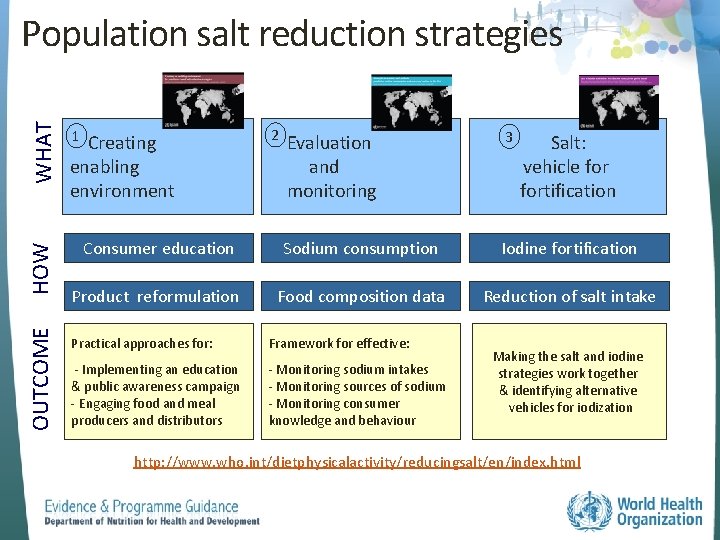
OUTCOME HOW WHAT Population salt reduction strategies 1 2 Evaluation and monitoring 3 Consumer education Sodium consumption Iodine fortification Product reformulation Food composition data Reduction of salt intake Creating enabling environment Practical approaches for: Framework for effective: - Implementing an education & public awareness campaign - Engaging food and meal producers and distributors - Monitoring sodium intakes - Monitoring sources of sodium - Monitoring consumer knowledge and behaviour Salt: vehicle fortification Making the salt and iodine strategies work together & identifying alternative vehicles for iodization http: //www. who. int/dietphysicalactivity/reducingsalt/en/index. html
Acknowledgements • The Evidence and Programme Guidance Unit receives financial resources from several external sources ‒ The Bill & Melinda Gates Foundation (2013 -2016) ‒ US Centers for Disease Control and Prevention (20142019) o National Center on Birth Defects and Developmental Disabilities o National Center for Chronic Disease Prevention and Health Promotion ‒ USAID (2014 -2016 ) ‒ The Micronutrient Initiative (2014 -2017) • Help keep WHO updated on your latest country data ‒ nutrition@who. int
 Non balanced occlusion
Non balanced occlusion Indirect guidance techniques
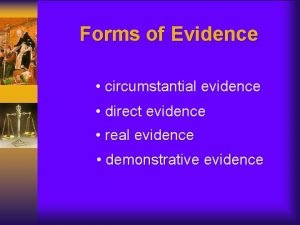
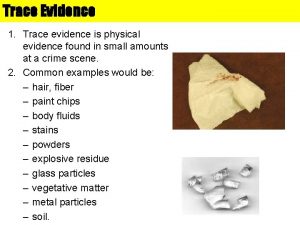
Indirect guidance techniques How can class evidence narrow a field of suspects
How can class evidence narrow a field of suspects Secondary sources
Secondary sources Primary evidence vs secondary evidence
Primary evidence vs secondary evidence Primary evidence vs secondary evidence
Primary evidence vs secondary evidence Primary evidence vs secondary evidence
Primary evidence vs secondary evidence Jobs vancouver
Jobs vancouver How can class evidence have probative value
How can class evidence have probative value Class vs individual evidence
Class vs individual evidence Class and individual evidence
Class and individual evidence Red herring fallacy
Red herring fallacy Kontinuitetshantering i praktiken
Kontinuitetshantering i praktiken Typiska drag för en novell
Typiska drag för en novell Tack för att ni lyssnade bild
Tack för att ni lyssnade bild Returpilarna
Returpilarna Varför kallas perioden 1918-1939 för mellankrigstiden
Varför kallas perioden 1918-1939 för mellankrigstiden En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Kassaregister ideell förening
Kassaregister ideell förening Tidbok
Tidbok