When Two Meds Are Better Than One Combination
When Two Meds Are Better Than One: Combination Medication Management for ADHD Oren Mason, MD Director, ATTENTION MD Assistant Professor of Family Medicine Michigan State U College of Human Medicine Grand Rapids, Michigan
Disclosures—Oren Mason MD • Speaker’s Bureau: Eli Lilly • Consultant: Eli Lilly • Royalties: Lulu Publishing
Learning Objectives • Summarize the current literature supporting combination therapy. • Recognized clinical cases in which monotherapy is suboptimal. • Utilize combination therapy to improve efficacy, duration and tolerability of ADHD therapy • Monitor patient response and safety when utilizing novel combination therapies. • Utilize rational combination for treating ADHD comorbid with depression, anxiety and mood disorder. ADHD, attention-deficit/hyperactivity disorder
Disclosure • Numerous examples of off-label usage of medications are presented. • The information in the presentation may not be construed as specific recommendations for the treatment of individual patients. • Clinical caution must be exercised with both onlabel and off-label prescription of medications.
ADHD Medication Limitations Side Effects Partial Efficacy Incomplete Duration of Effect Cost
Medication Limitations Side Effects Efficacy • Insomnia • Agitation, dysphoria • Anxiety • Loss of appetite, weight • Loss of personality, social “flatness” • Headache • Abdominal pain Duration Cost
Medication Limitations Side Effects Efficacy Duration Cost • Nathan is an active 11 yr old with combinedtype ADHD and ODD. • 54 mg OROS-MPH (0. 9 mg/kg/d) • Some symptoms improved: • Hyperactivity • Aggression • Some are still problems • Inattention in school • Impulsivity with playmates • Oppositionality with parents • 72 mg OROS-MPH (1. 2 mg/kg/d) • ADHD and ODD symptoms much better • Pulse 132 bpm • Falls asleep 11 pm - midnight
Medication Limitations Partial Efficacy Side Effects Duration Cost • Sarah is a shy 10 year old with inattentive ADHD and dyslexia. • Atomoxetine 40 mg (1. 4 mg/kg/d) • improved organization • completes morning routine and homework without support • reading proficiency and social function have improved. • School conference • reading specialist is pleased with her improved reading scores • but teacher sees distractibility in the classroom causing problems.
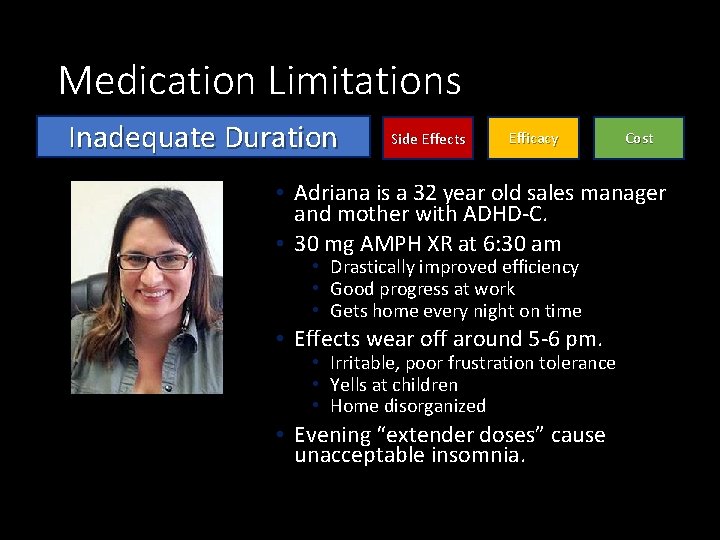
Medication Limitations Inadequate Duration Side Effects Efficacy Cost • Adriana is a 32 year old sales manager and mother with ADHD-C. • 30 mg AMPH XR at 6: 30 am • Drastically improved efficiency • Good progress at work • Gets home every night on time • Effects wear off around 5 -6 pm. • Irritable, poor frustration tolerance • Yells at children • Home disorganized • Evening “extender doses” cause unacceptable insomnia.

Medication Limitations Unacceptable Cost Side Effects Efficacy Duration • Josh is a 20 year old college junior with ADHD as well as a 290 pound defensive tackle on the football team. • 144 mg OROS-MPH. • (1. 1 mg/kg/d) • Good response – 65% symptom score reduction • Studies and time management are going well • Medication cost not affordable • His insurance covers only 72 mg/d • Josh pays $40 copay monthly AND • $350 monthly for uncovered amount
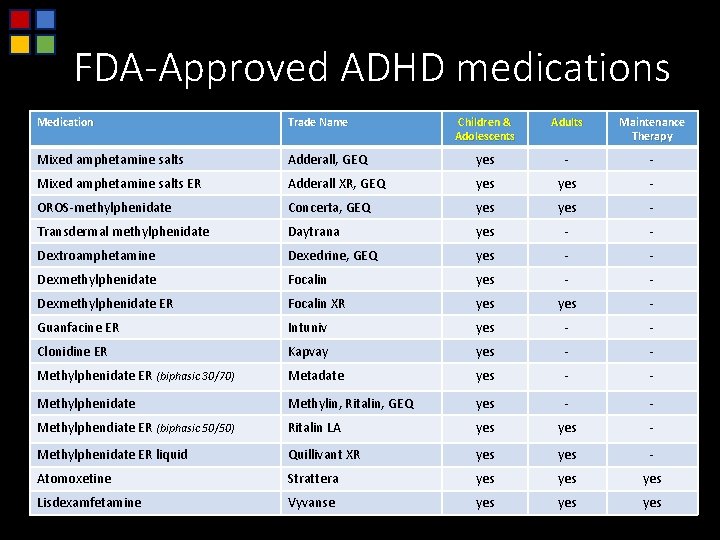
FDA-Approved ADHD medications Medication Trade Name Children & Adolescents Adults Maintenance Therapy Mixed amphetamine salts Adderall, GEQ yes - - Mixed amphetamine salts ER Adderall XR, GEQ yes - OROS-methylphenidate Concerta, GEQ yes - Transdermal methylphenidate Daytrana yes - - Dextroamphetamine Dexedrine, GEQ yes - - Dexmethylphenidate Focalin yes - - Dexmethylphenidate ER Focalin XR yes - Guanfacine ER Intuniv yes - - Clonidine ER Kapvay yes - - Methylphenidate ER (biphasic 30/70) Metadate yes - - Methylphenidate Methylin, Ritalin, GEQ yes - - Methylphendiate ER (biphasic 50/50) Ritalin LA yes - Methylphenidate ER liquid Quillivant XR yes - Atomoxetine Strattera yes yes Lisdexamfetamine Vyvanse yes yes
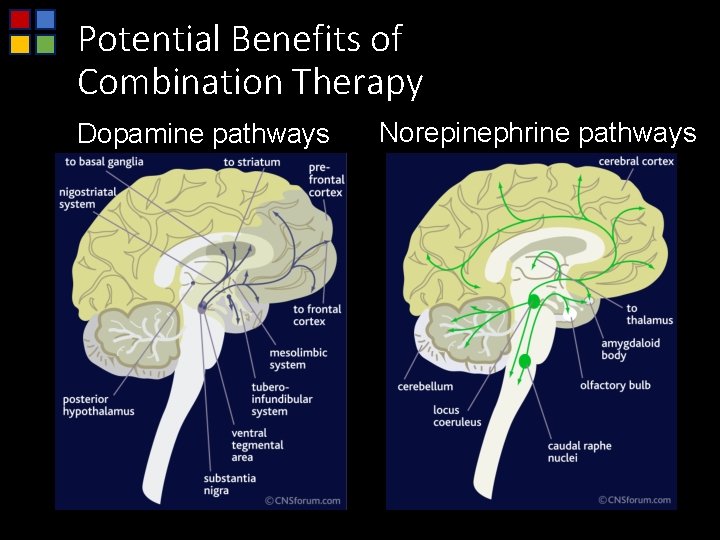
Potential Benefits of Combination Therapy Dopamine pathways Norepinephrine pathways
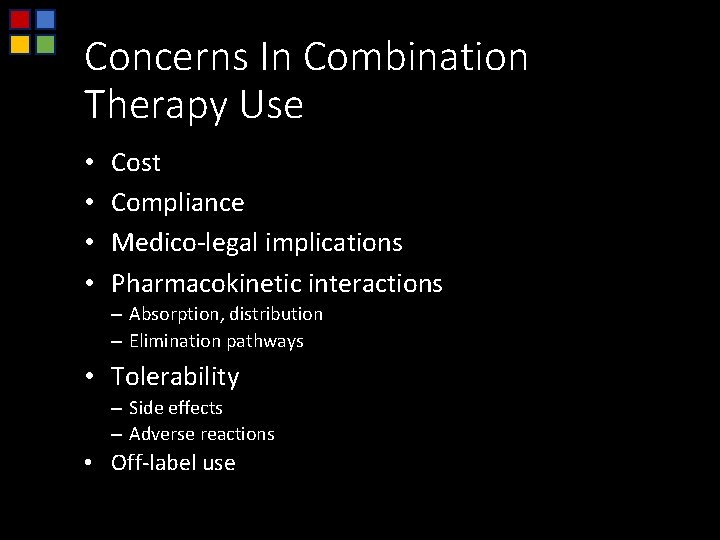
Concerns In Combination Therapy Use • • Cost Compliance Medico-legal implications Pharmacokinetic interactions – Absorption, distribution – Elimination pathways • Tolerability – Side effects – Adverse reactions • Off-label use
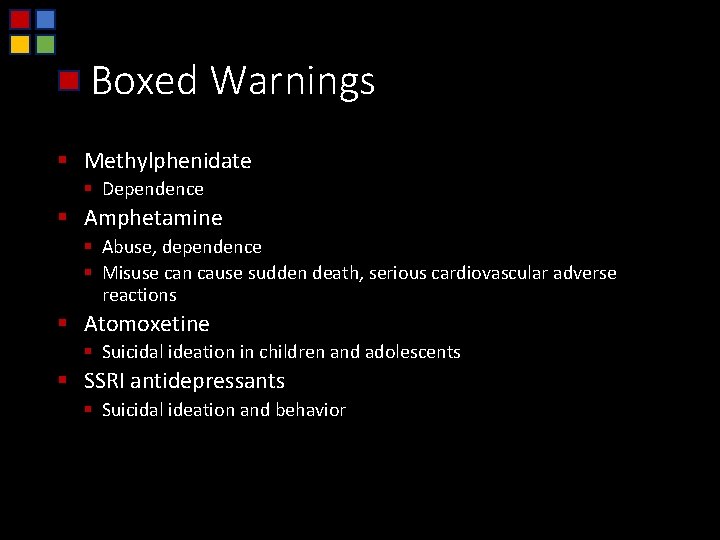
Boxed Warnings § Methylphenidate § Dependence § Amphetamine § Abuse, dependence § Misuse can cause sudden death, serious cardiovascular adverse reactions § Atomoxetine § Suicidal ideation in children and adolescents § SSRI antidepressants § Suicidal ideation and behavior
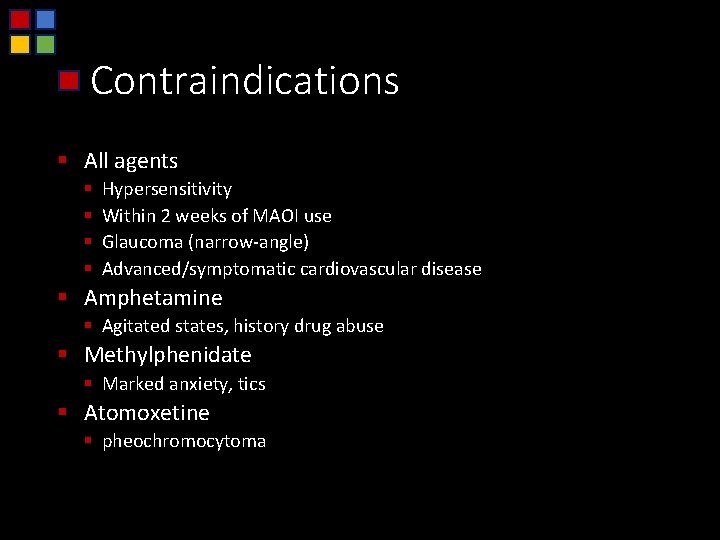
Contraindications § All agents § § Hypersensitivity Within 2 weeks of MAOI use Glaucoma (narrow-angle) Advanced/symptomatic cardiovascular disease § Amphetamine § Agitated states, history drug abuse § Methylphenidate § Marked anxiety, tics § Atomoxetine § pheochromocytoma
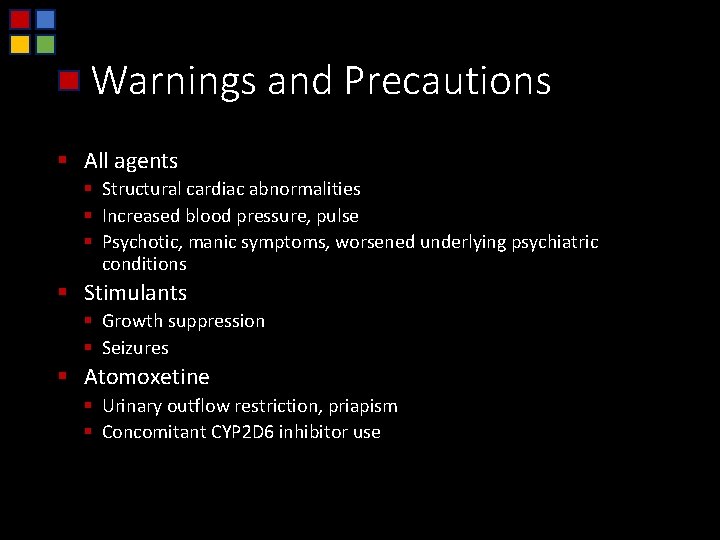
Warnings and Precautions § All agents § Structural cardiac abnormalities § Increased blood pressure, pulse § Psychotic, manic symptoms, worsened underlying psychiatric conditions § Stimulants § Growth suppression § Seizures § Atomoxetine § Urinary outflow restriction, priapism § Concomitant CYP 2 D 6 inhibitor use
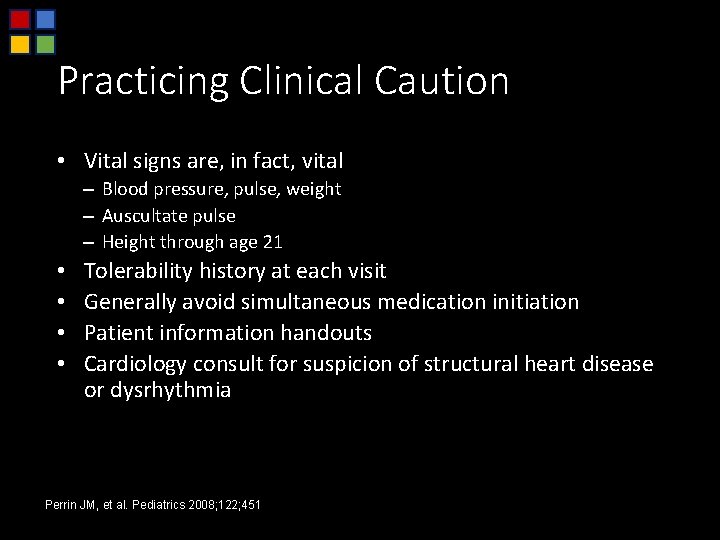
Practicing Clinical Caution • Vital signs are, in fact, vital – Blood pressure, pulse, weight – Auscultate pulse – Height through age 21 • • Tolerability history at each visit Generally avoid simultaneous medication initiation Patient information handouts Cardiology consult for suspicion of structural heart disease or dysrhythmia Perrin JM, et al. Pediatrics 2008; 122; 451
History of combination therapy Case Reports Published Studies

Case Reports Combination Therapy
Combination Therapy Case Report • 8 -year-old male, 50 mg MPH-IR divided tid-qid • Marked initial response • Tolerance developed at 6 months, dose effects ~ 2 hours • Further increases intolerable • ATMX 1. 2 mg/kg/d added • MPH-IR slowly down-titrated to 10 mg/d • ADHD-RS again measured 10 • Appetite and sleep issues no longer evident • Efforts to further reduce MPH dose resulted in significant return of baseline symptoms IR, immediate release Agarwal V, Sitholey P. J Can Acad Child Adolesc Psychiatry. 2008; 17(3): 160.
Combination Therapy Case Report • 11 -year-old male treated with MPH 20 mg/d • improved attention but mood and sleep worsened after 2 months • MPH 10 mg/d • resulted in return of inattention • ATMX monotherapy 40 mg/d • did not ameliorate inattention • MPH 10 mg/d added to ATMX 40 mg/d: • “ADHD symptomatology improved impressively” Niederhofer H. Psychiatr Danub. 2009; 21(3): 330.

Published Studies Combination Therapy
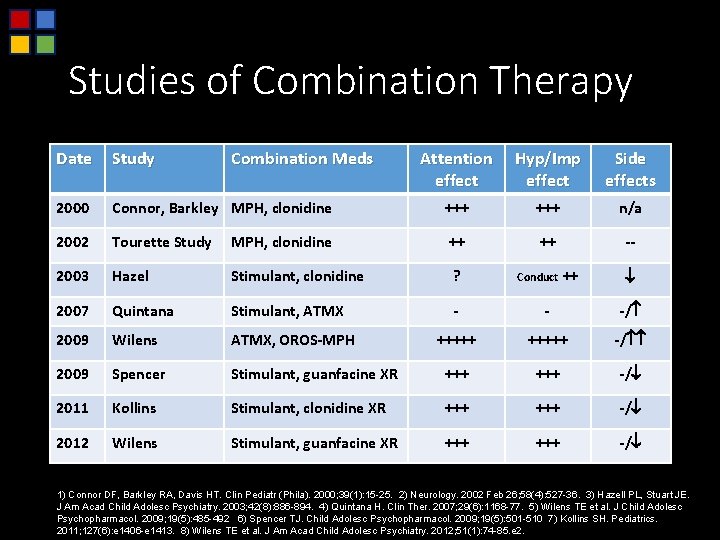
Studies of Combination Therapy Date Study 2000 Combination Meds Attention effect Hyp/Imp effect Side effects Connor, Barkley MPH, clonidine +++ n/a 2002 Tourette Study MPH, clonidine ++ ++ -- 2003 Hazel Stimulant, clonidine ? 2007 Quintana Stimulant, ATMX - - -/ 2009 Wilens ATMX, OROS-MPH +++++ -/ 2009 Spencer Stimulant, guanfacine XR +++ -/ 2011 Kollins Stimulant, clonidine XR +++ -/ 2012 Wilens Stimulant, guanfacine XR +++ -/ Conduct ++ 1) Connor DF, Barkley RA, Davis HT. Clin Pediatr (Phila). 2000; 39(1): 15 -25. 2) Neurology. 2002 Feb 26; 58(4): 527 -36. 3) Hazell PL, Stuart JE. J Am Acad Child Adolesc Psychiatry. 2003; 42(8): 886 -894. 4) Quintana H. Clin Ther. 2007; 29(6): 1168 -77. 5) Wilens TE et al. J Child Adolesc Psychopharmacol. 2009; 19(5): 485 -492 6) Spencer TJ. Child Adolesc Psychopharmacol. 2009; 19(5): 501 -510 7) Kollins SH. Pediatrics. 2011; 127(6): e 1406 -e 1413. 8) Wilens TE et al. J Am Acad Child Adolesc Psychiatry. 2012; 51(1): 74 -85. e 2.
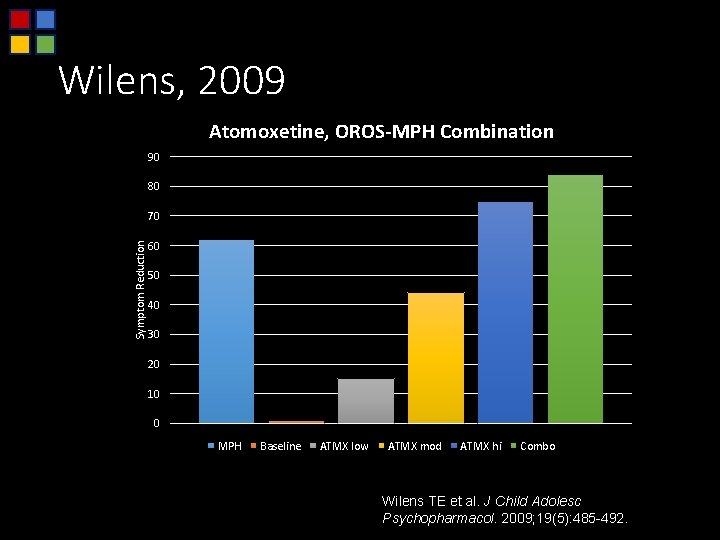
Wilens, 2009 Atomoxetine, OROS-MPH Combination 90 80 Symptom Reduction 70 60 50 40 30 20 10 0 MPH Baseline ATMX low ATMX mod ATMX hi Combo Wilens TE et al. J Child Adolesc Psychopharmacol. 2009; 19(5): 485 -492.
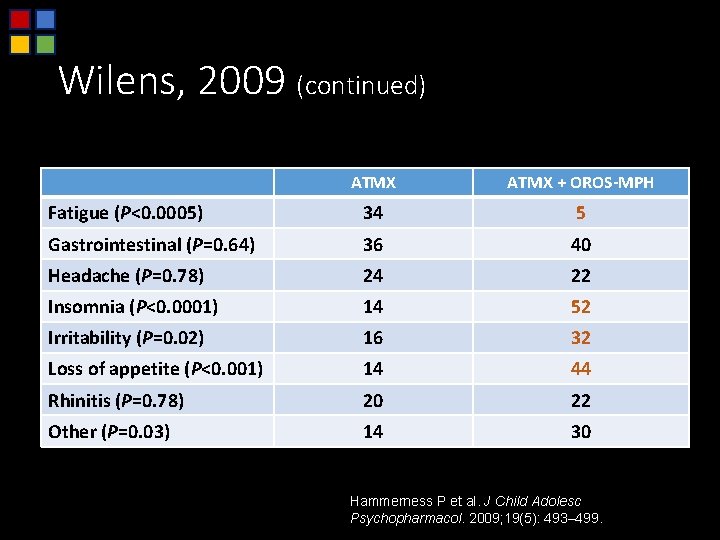
Wilens, 2009 (continued) Safety and Tolerability ATMX + OROS-MPH Fatigue (P<0. 0005) 34 5 Gastrointestinal (P=0. 64) 36 40 Headache (P=0. 78) 24 22 Insomnia (P<0. 0001) 14 52 Irritability (P=0. 02) 16 32 Loss of appetite (P<0. 001) 14 44 Rhinitis (P=0. 78) 20 22 Other (P=0. 03) 14 30 Hammerness P et al. J Child Adolesc Psychopharmacol. 2009; 19(5): 493– 499.

Clinical Monitoring of Combination Therapy Safeguard Patients Optimize Efficacy
Clinical Tools to Monitor Combination Therapy Vital Signs Structured Symptom Eval. Clinical History
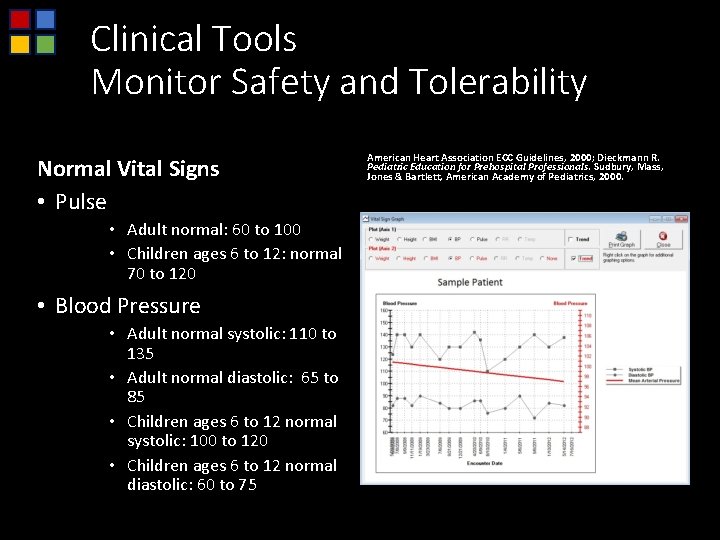
Clinical Tools Monitor Safety and Tolerability Normal Vital Signs • Pulse • Adult normal: 60 to 100 • Children ages 6 to 12: normal 70 to 120 • Blood Pressure • Adult normal systolic: 110 to 135 • Adult normal diastolic: 65 to 85 • Children ages 6 to 12 normal systolic: 100 to 120 • Children ages 6 to 12 normal diastolic: 60 to 75 American Heart Association ECC Guidelines, 2000; Dieckmann R. Pediatric Education for Prehospital Professionals. Sudbury, Mass, Jones & Bartlett, American Academy of Pediatrics, 2000.
Clinical Tools Monitor Safety and Efficacy Clinical History--Safety § Tolerability including intensity and time course § Compliance § Frequent updates of: § § Social history Substance use Screen for anxious, depressed, manic symptoms Sleep history Clinical History--Efficacy • Time course of symptom improvement • Residual symptoms and impairments • Progress in patient’s highest priority outcomes
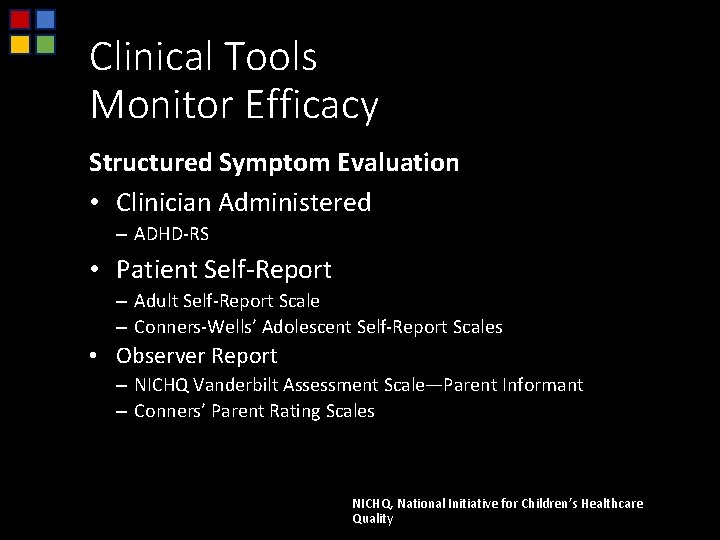
Clinical Tools Monitor Efficacy Structured Symptom Evaluation • Clinician Administered – ADHD-RS • Patient Self-Report – Adult Self-Report Scale – Conners-Wells’ Adolescent Self-Report Scales • Observer Report – NICHQ Vanderbilt Assessment Scale—Parent Informant – Conners’ Parent Rating Scales NICHQ, National Initiative for Children’s Healthcare Quality
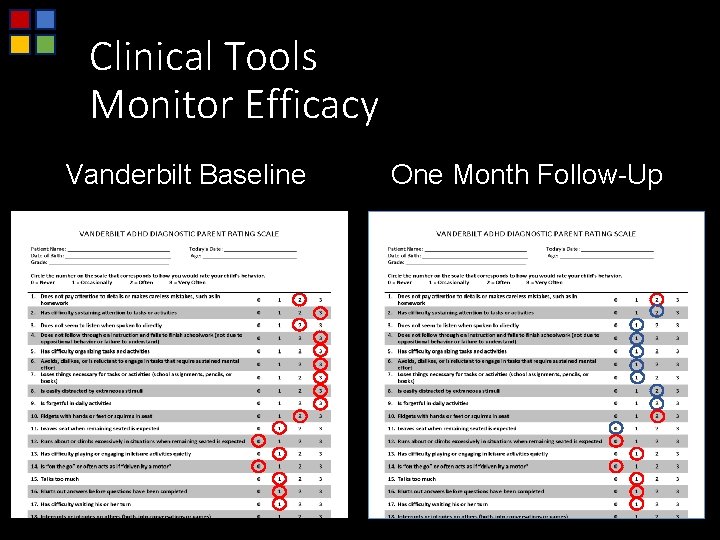
Clinical Tools Monitor Efficacy Vanderbilt Baseline One Month Follow-Up
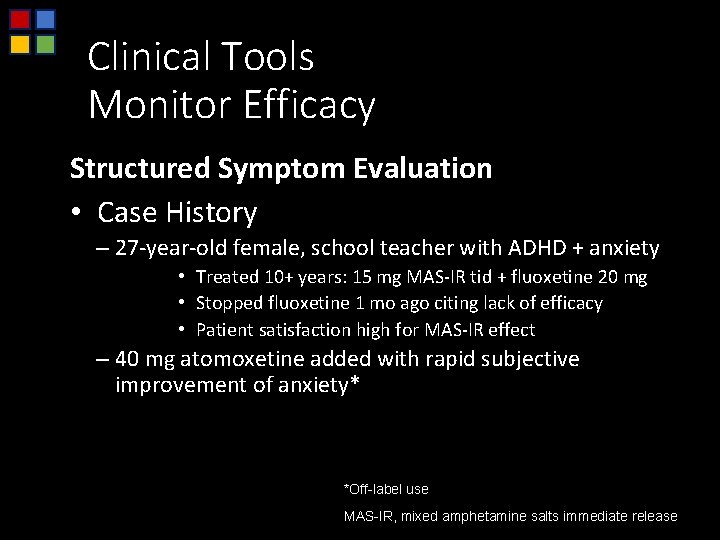
Clinical Tools Monitor Efficacy Structured Symptom Evaluation • Case History – 27 -year-old female, school teacher with ADHD + anxiety • Treated 10+ years: 15 mg MAS-IR tid + fluoxetine 20 mg • Stopped fluoxetine 1 mo ago citing lack of efficacy • Patient satisfaction high for MAS-IR effect – 40 mg atomoxetine added with rapid subjective improvement of anxiety* *Off-label use MAS-IR, mixed amphetamine salts immediate release
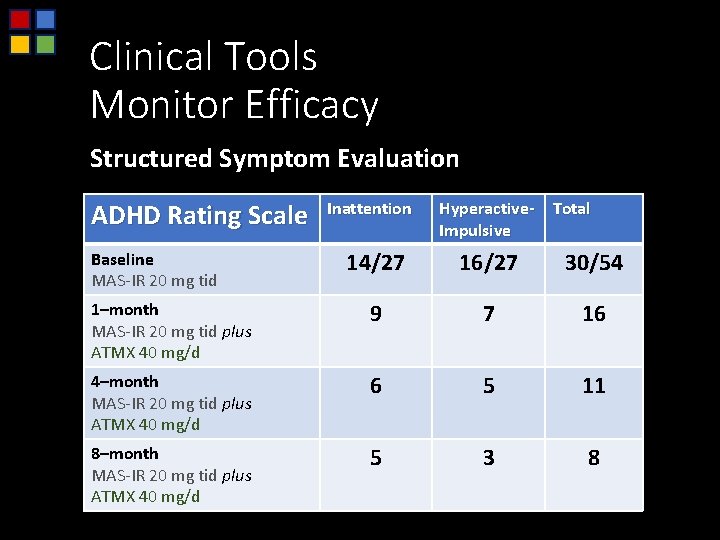
Clinical Tools Monitor Efficacy Structured Symptom Evaluation ADHD Rating Scale Inattention Hyperactive- Total Impulsive 14/27 16/27 30/54 1–month MAS-IR 20 mg tid plus ATMX 40 mg/d 9 7 16 4–month MAS-IR 20 mg tid plus ATMX 40 mg/d 6 5 11 8–month MAS-IR 20 mg tid plus ATMX 40 mg/d 5 3 8 Baseline MAS-IR 20 mg tid
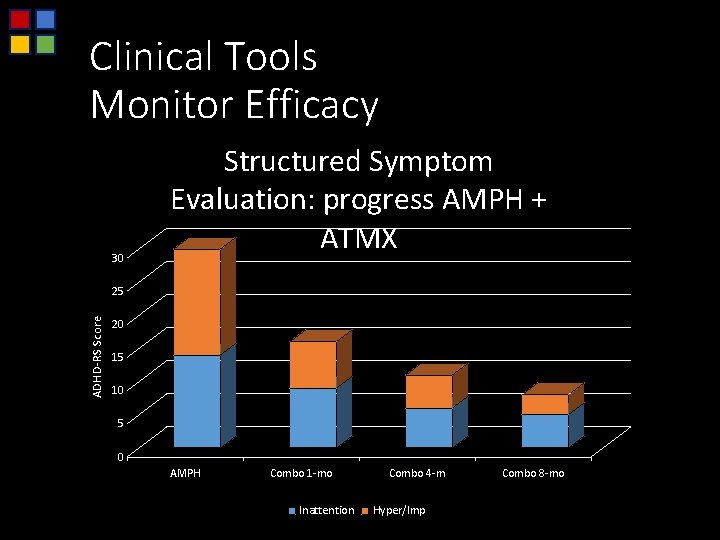
Clinical Tools Monitor Efficacy 30 Structured Symptom Evaluation: progress AMPH + ATMX ADHD-RS Score 25 20 15 10 5 0 AMPH Combo 1 -mo Inattention Combo 4 -m Hyper/Imp Combo 8 -mo
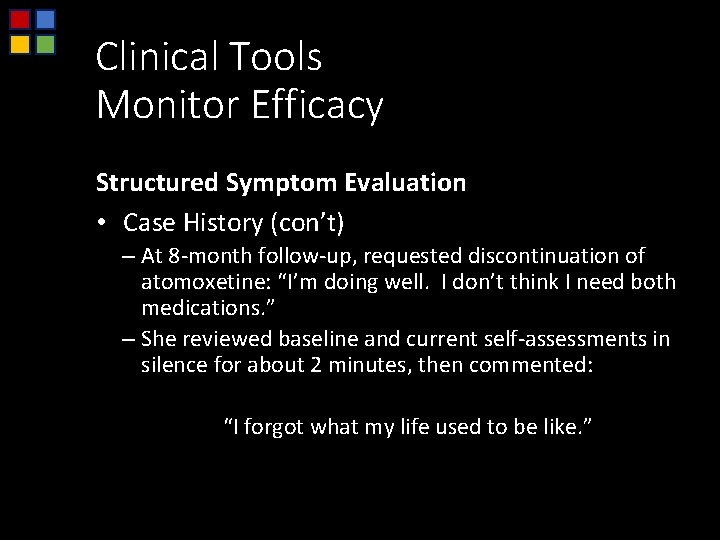
Clinical Tools Monitor Efficacy Structured Symptom Evaluation • Case History (con’t) – At 8 -month follow-up, requested discontinuation of atomoxetine: “I’m doing well. I don’t think I need both medications. ” – She reviewed baseline and current self-assessments in silence for about 2 minutes, then commented: “I forgot what my life used to be like. ”
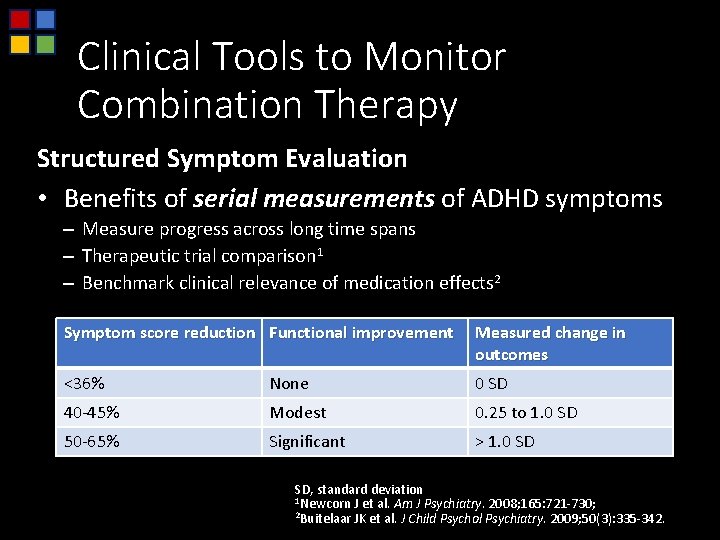
Clinical Tools to Monitor Combination Therapy Structured Symptom Evaluation • Benefits of serial measurements of ADHD symptoms – Measure progress across long time spans – Therapeutic trial comparison 1 – Benchmark clinical relevance of medication effects 2 Symptom score reduction Functional improvement Measured change in outcomes <36% None 0 SD 40 -45% Modest 0. 25 to 1. 0 SD 50 -65% Significant > 1. 0 SD SD, standard deviation 1 Newcorn J et al. Am J Psychiatry. 2008; 165: 721 -730; 2 Buitelaar JK et al. J Child Psychol Psychiatry. 2009; 50(3): 335 -342.

Prioritized Goals Of ADHD Medication Therapy First, do no harm Symptom Score Reduction > 50% 24 -hour Symptom Reduction No Impairing Symptoms No Residual (Clinical) Symptoms Functional Improvement
Examples Of Combination Therapy Case Histories
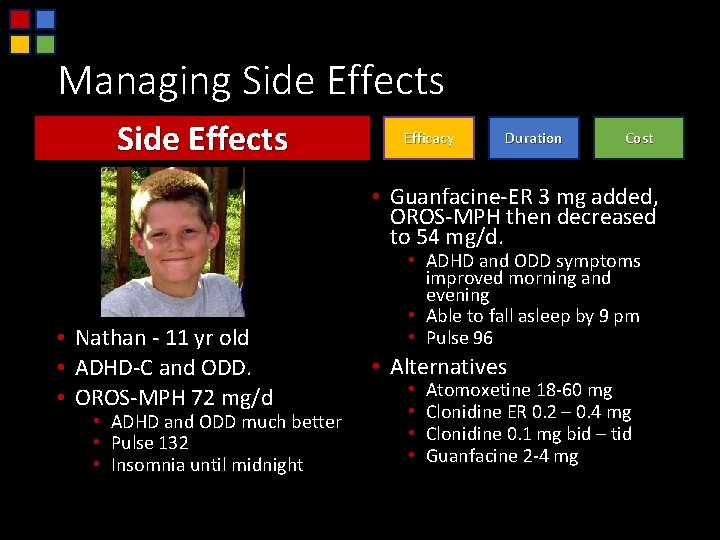
Managing Side Effects Efficacy Duration Cost • Guanfacine-ER 3 mg added, OROS-MPH then decreased to 54 mg/d. • Nathan - 11 yr old • ADHD-C and ODD. • OROS-MPH 72 mg/d • ADHD and ODD much better • Pulse 132 • Insomnia until midnight • ADHD and ODD symptoms improved morning and evening • Able to fall asleep by 9 pm • Pulse 96 • Alternatives • • Atomoxetine 18 -60 mg Clonidine ER 0. 2 – 0. 4 mg Clonidine 0. 1 mg bid – tid Guanfacine 2 -4 mg
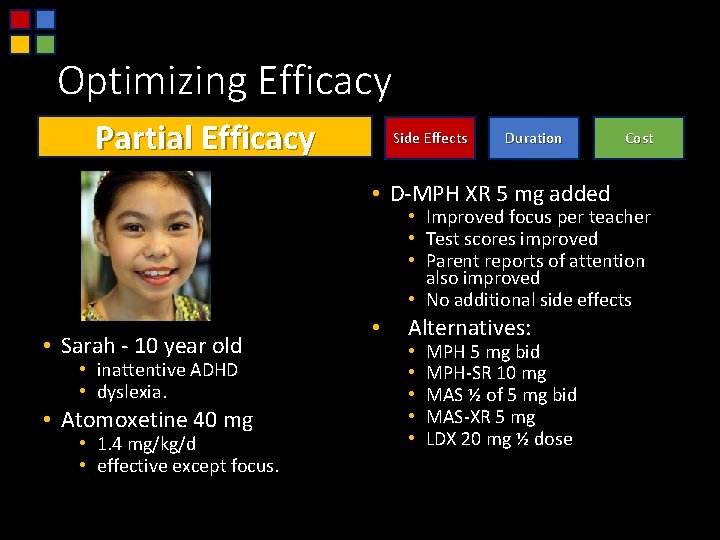
Optimizing Efficacy Partial Efficacy Side Effects Duration • D-MPH XR 5 mg added Cost • Improved focus per teacher • Test scores improved • Parent reports of attention also improved • No additional side effects • Sarah - 10 year old • inattentive ADHD • dyslexia. • Atomoxetine 40 mg • 1. 4 mg/kg/d • effective except focus. • Alternatives: • • • MPH 5 mg bid MPH-SR 10 mg MAS ½ of 5 mg bid MAS-XR 5 mg LDX 20 mg ½ dose
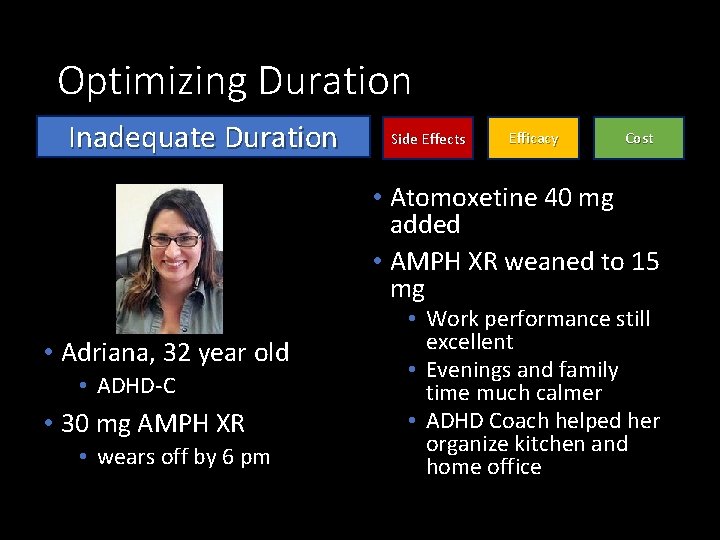
Optimizing Duration Inadequate Duration Side Effects Efficacy Cost • Atomoxetine 40 mg added • AMPH XR weaned to 15 mg • Adriana, 32 year old • ADHD-C • 30 mg AMPH XR • wears off by 6 pm • Work performance still excellent • Evenings and family time much calmer • ADHD Coach helped her organize kitchen and home office
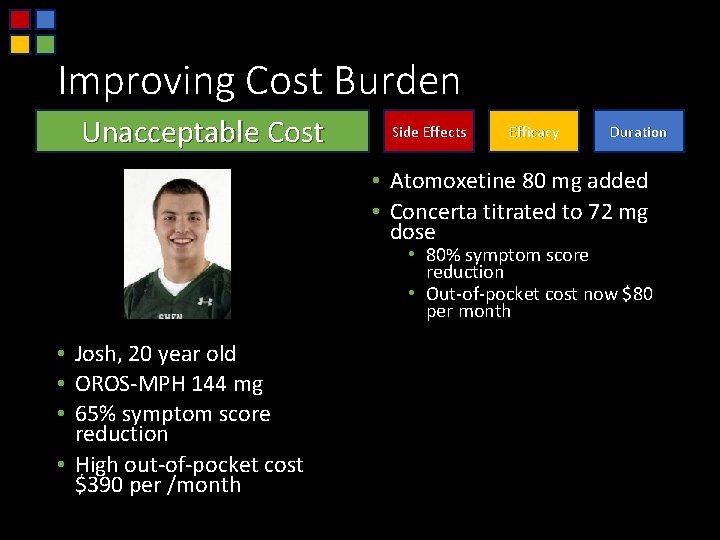
Improving Cost Burden Unacceptable Cost Side Effects Efficacy Duration • Atomoxetine 80 mg added • Concerta titrated to 72 mg dose • 80% symptom score reduction • Out-of-pocket cost now $80 per month • Josh, 20 year old • OROS-MPH 144 mg • 65% symptom score reduction • High out-of-pocket cost $390 per /month
Improving Cost Burden Unacceptable Cost Side Effects Efficacy Duration • This case may not be typical. • Many people will pay more, not less for combination therapy.

Combination Therapy Clinical Pearls Initial Agent • Start with “best fit” medication. • Aim for monotherapy success. • Limit initial agent to “highest tolerable dose”.
Combination Therapy Clinical Pearls Combination Agent • Initial target: ½ of usual dose • Titrate slowly to that target dose • Stimulant duration may be improved when added to nonstimulant • Unusually low dosages of second agent are sometimes very effective
Managing ADHD with Comorbid Conditions Anxiety, OCD, Panic Oppositional and Conduct Disorders Substance Use Disorder Depression, Bipolar
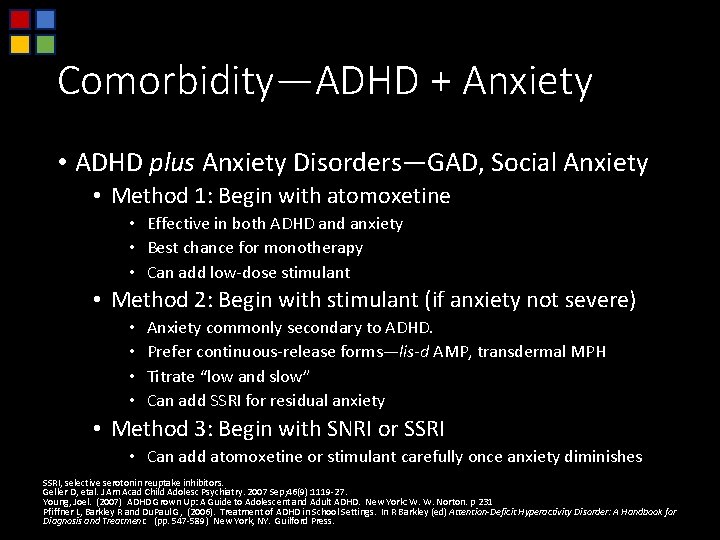
Comorbidity—ADHD + Anxiety • ADHD plus Anxiety Disorders—GAD, Social Anxiety • Method 1: Begin with atomoxetine • Effective in both ADHD and anxiety • Best chance for monotherapy • Can add low-dose stimulant • Method 2: Begin with stimulant (if anxiety not severe) • • Anxiety commonly secondary to ADHD. Prefer continuous-release forms—lis-d AMP, transdermal MPH Titrate “low and slow” Can add SSRI for residual anxiety • Method 3: Begin with SNRI or SSRI • Can add atomoxetine or stimulant carefully once anxiety diminishes SSRI, selective serotonin reuptake inhibitors. Geller D, etal. J Am Acad Child Adolesc Psychiatry. 2007 Sep; 46(9): 1119 -27. Young, Joel. (2007) ADHD Grown Up: A Guide to Adolescent and Adult ADHD. New York: W. W. Norton. p 231 Pfiffner L, Barkley R and Du. Paul G, (2006). Treatment of ADHD in School Settings. In R Barkley (ed) Attention-Deficit Hyperactivity Disorder: A Handbook for Diagnosis and Treatment. (pp. 547 -589) New York, NY. Guilford Press.
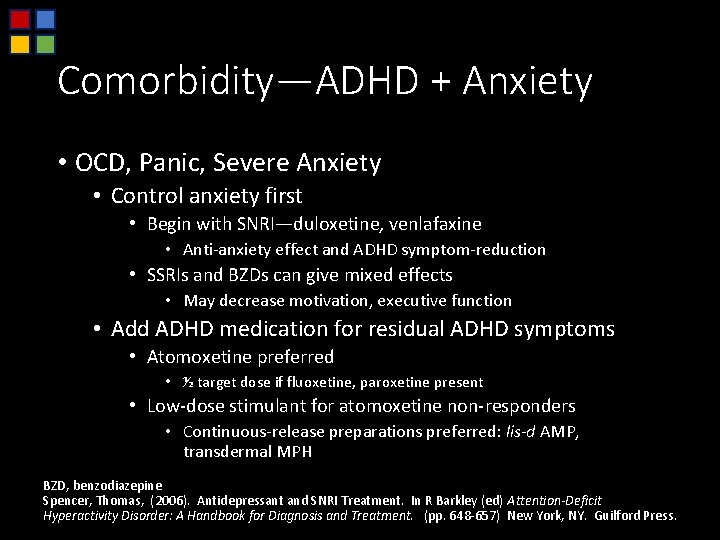
Comorbidity—ADHD + Anxiety • OCD, Panic, Severe Anxiety • Control anxiety first • Begin with SNRI—duloxetine, venlafaxine • Anti-anxiety effect and ADHD symptom-reduction • SSRIs and BZDs can give mixed effects • May decrease motivation, executive function • Add ADHD medication for residual ADHD symptoms • Atomoxetine preferred • ½ target dose if fluoxetine, paroxetine present • Low-dose stimulant for atomoxetine non-responders • Continuous-release preparations preferred: lis-d AMP, transdermal MPH BZD, benzodiazepine Spencer, Thomas, (2006). Antidepressant and SNRI Treatment. In R Barkley (ed) Attention-Deficit Hyperactivity Disorder: A Handbook for Diagnosis and Treatment. (pp. 648 -657) New York, NY. Guilford Press.
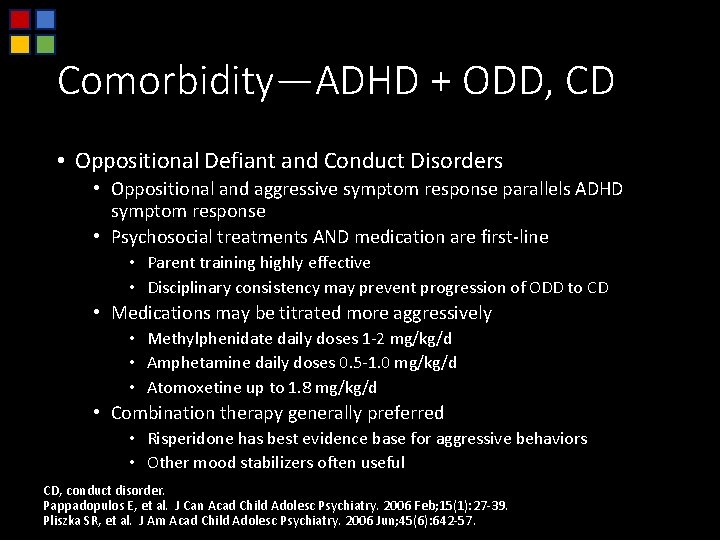
Comorbidity—ADHD + ODD, CD • Oppositional Defiant and Conduct Disorders • Oppositional and aggressive symptom response parallels ADHD symptom response • Psychosocial treatments AND medication are first-line • Parent training highly effective • Disciplinary consistency may prevent progression of ODD to CD • Medications may be titrated more aggressively • Methylphenidate daily doses 1 -2 mg/kg/d • Amphetamine daily doses 0. 5 -1. 0 mg/kg/d • Atomoxetine up to 1. 8 mg/kg/d • Combination therapy generally preferred • Risperidone has best evidence base for aggressive behaviors • Other mood stabilizers often useful CD, conduct disorder. Pappadopulos E, et al. J Can Acad Child Adolesc Psychiatry. 2006 Feb; 15(1): 27 -39. Pliszka SR, et al. J Am Acad Child Adolesc Psychiatry. 2006 Jun; 45(6): 642 -57.
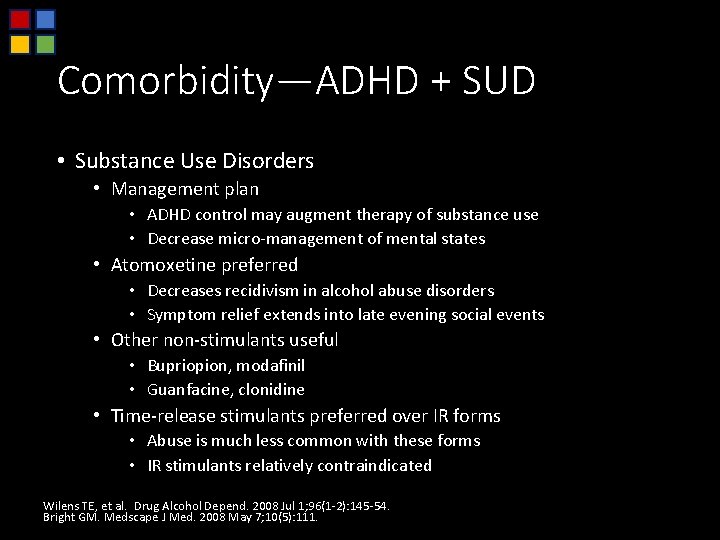
Comorbidity—ADHD + SUD • Substance Use Disorders • Management plan • ADHD control may augment therapy of substance use • Decrease micro-management of mental states • Atomoxetine preferred • Decreases recidivism in alcohol abuse disorders • Symptom relief extends into late evening social events • Other non-stimulants useful • Bupriopion, modafinil • Guanfacine, clonidine • Time-release stimulants preferred over IR forms • Abuse is much less common with these forms • IR stimulants relatively contraindicated Wilens TE, et al. Drug Alcohol Depend. 2008 Jul 1; 96(1 -2): 145 -54. Bright GM. Medscape J Med. 2008 May 7; 10(5): 111.
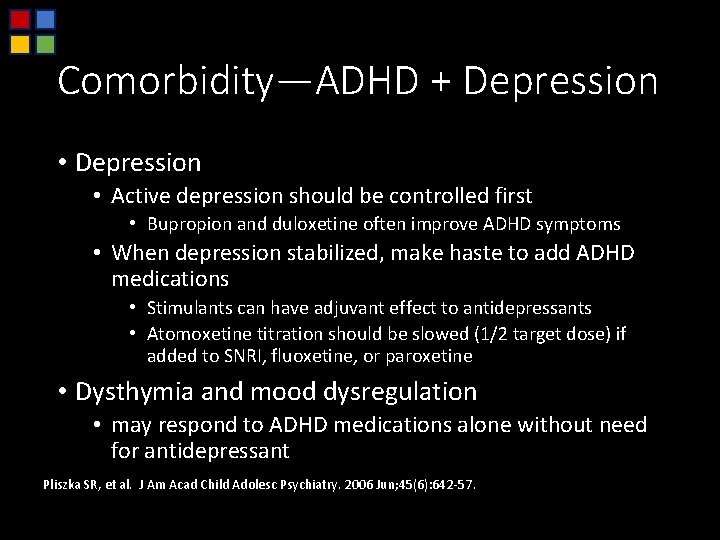
Comorbidity—ADHD + Depression • Depression • Active depression should be controlled first • Bupropion and duloxetine often improve ADHD symptoms • When depression stabilized, make haste to add ADHD medications • Stimulants can have adjuvant effect to antidepressants • Atomoxetine titration should be slowed (1/2 target dose) if added to SNRI, fluoxetine, or paroxetine • Dysthymia and mood dysregulation • may respond to ADHD medications alone without need for antidepressant Pliszka SR, et al. J Am Acad Child Adolesc Psychiatry. 2006 Jun; 45(6): 642 -57.
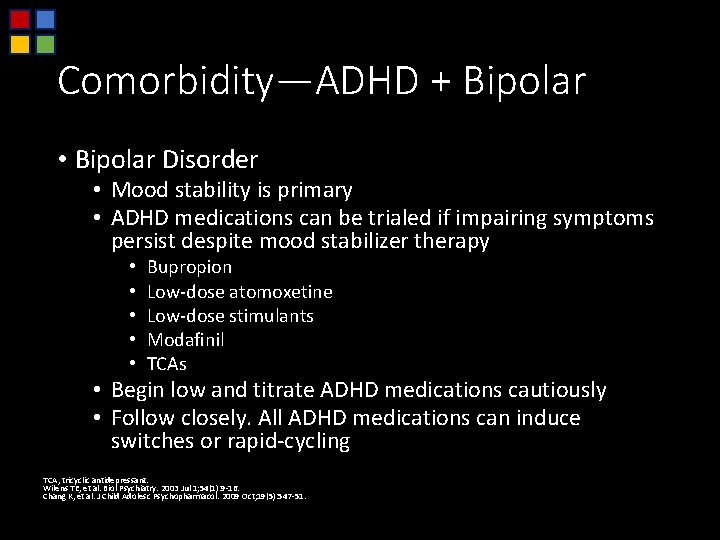
Comorbidity—ADHD + Bipolar • Bipolar Disorder • Mood stability is primary • ADHD medications can be trialed if impairing symptoms persist despite mood stabilizer therapy • • • Bupropion Low-dose atomoxetine Low-dose stimulants Modafinil TCAs • Begin low and titrate ADHD medications cautiously • Follow closely. All ADHD medications can induce switches or rapid-cycling TCA, tricyclic antidepressant. Wilens TE, et al. Biol Psychiatry. 2003 Jul 1; 54(1): 9 -16. Chang K, et al. J Child Adolesc Psychopharmacol. 2009 Oct; 19(5): 547 -51.
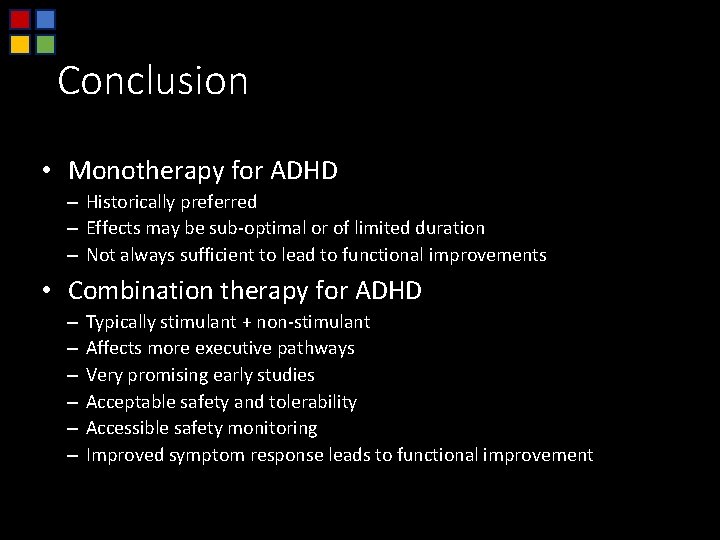
Conclusion • Monotherapy for ADHD – Historically preferred – Effects may be sub-optimal or of limited duration – Not always sufficient to lead to functional improvements • Combination therapy for ADHD – – – Typically stimulant + non-stimulant Affects more executive pathways Very promising early studies Acceptable safety and tolerability Accessible safety monitoring Improved symptom response leads to functional improvement
When Two Meds Are Better Than One: Combination Medication Management for ADHD Questions?
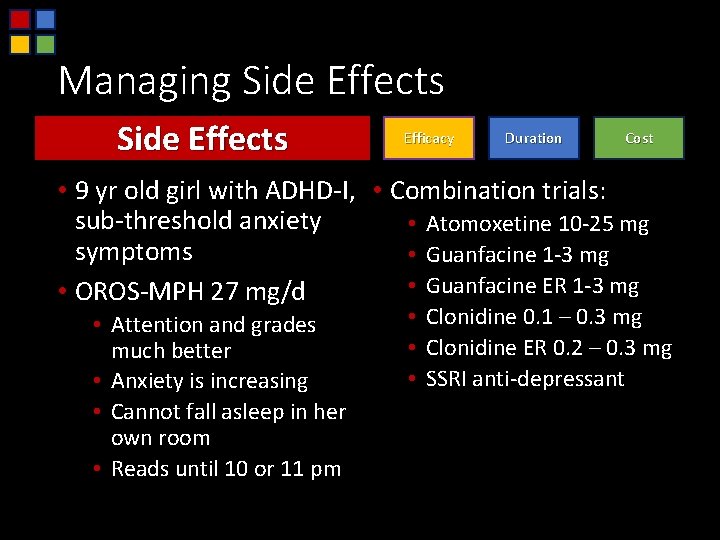
Managing Side Effects Efficacy Duration Cost • 9 yr old girl with ADHD-I, • Combination trials: sub-threshold anxiety • Atomoxetine 10 -25 mg symptoms • Guanfacine 1 -3 mg • Guanfacine ER 1 -3 mg • OROS-MPH 27 mg/d • Attention and grades much better • Anxiety is increasing • Cannot fall asleep in her own room • Reads until 10 or 11 pm • Clonidine 0. 1 – 0. 3 mg • Clonidine ER 0. 2 – 0. 3 mg • SSRI anti-depressant
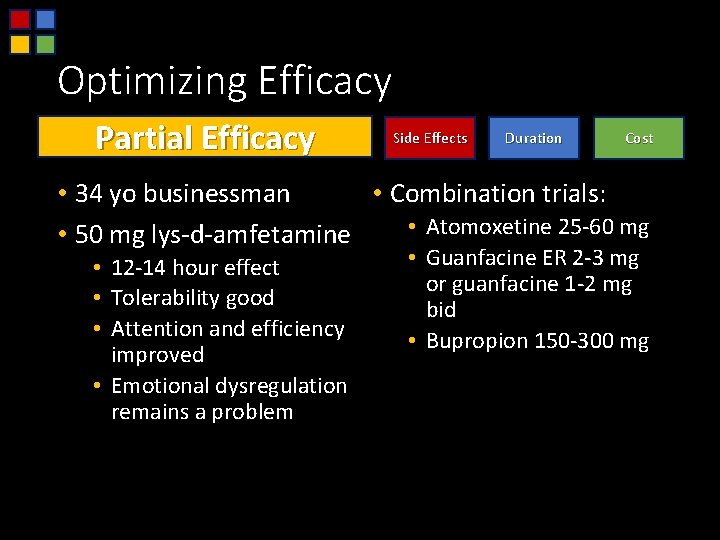
Optimizing Efficacy Partial Efficacy Side Effects Duration Cost • 34 yo businessman • Combination trials: • Atomoxetine 25 -60 mg • 50 mg lys-d-amfetamine • 12 -14 hour effect • Tolerability good • Attention and efficiency improved • Emotional dysregulation remains a problem • Guanfacine ER 2 -3 mg or guanfacine 1 -2 mg bid • Bupropion 150 -300 mg
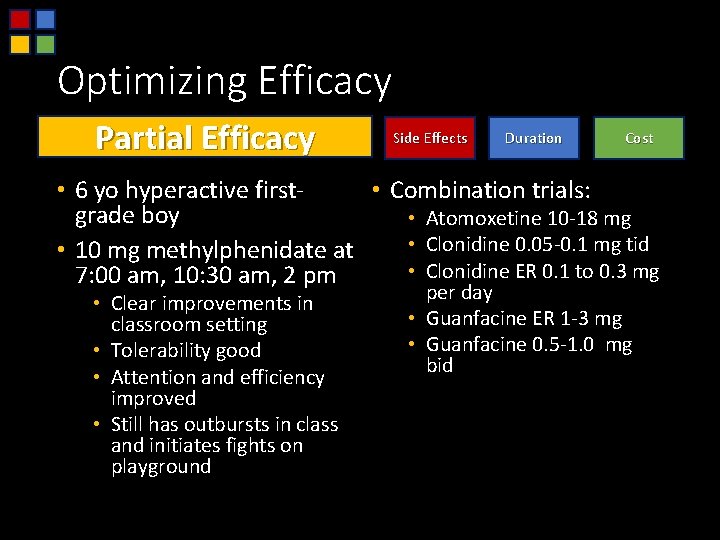
Optimizing Efficacy Partial Efficacy Side Effects Duration Cost • 6 yo hyperactive first • Combination trials: grade boy • Atomoxetine 10 -18 mg • Clonidine 0. 05 -0. 1 mg tid • 10 mg methylphenidate at • Clonidine ER 0. 1 to 0. 3 mg 7: 00 am, 10: 30 am, 2 pm • Clear improvements in classroom setting • Tolerability good • Attention and efficiency improved • Still has outbursts in class and initiates fights on playground per day • Guanfacine ER 1 -3 mg • Guanfacine 0. 5 -1. 0 mg bid
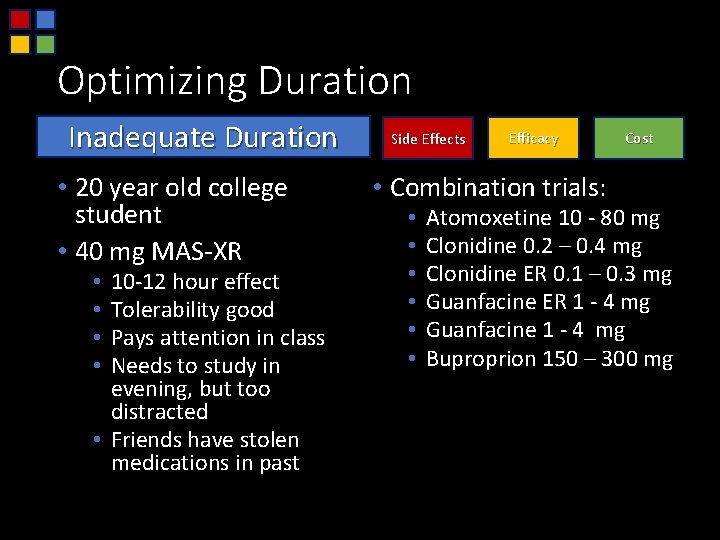
Optimizing Duration Inadequate Duration • 20 year old college student • 40 mg MAS-XR 10 -12 hour effect Tolerability good Pays attention in class Needs to study in evening, but too distracted • Friends have stolen medications in past • • Side Effects Efficacy • Combination trials: • • • Cost Atomoxetine 10 - 80 mg Clonidine 0. 2 – 0. 4 mg Clonidine ER 0. 1 – 0. 3 mg Guanfacine ER 1 - 4 mg Guanfacine 1 - 4 mg Buproprion 150 – 300 mg
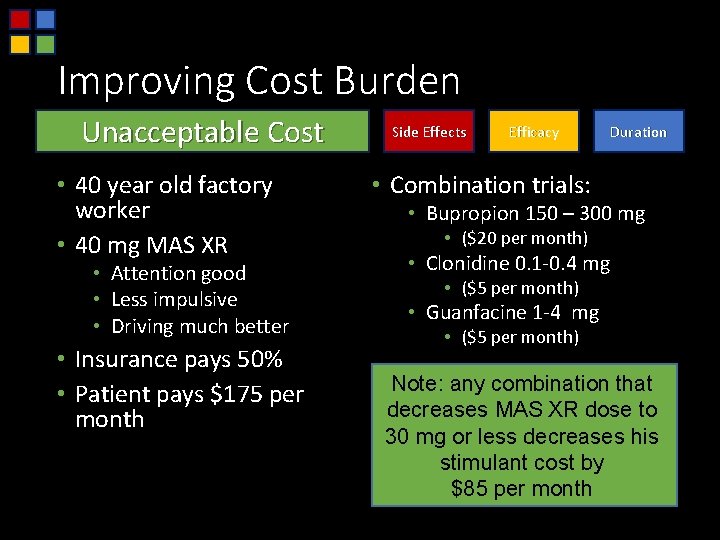
Improving Cost Burden Unacceptable Cost • 40 year old factory worker • 40 mg MAS XR • Attention good • Less impulsive • Driving much better • Insurance pays 50% • Patient pays $175 per month Side Effects Efficacy Duration • Combination trials: • Bupropion 150 – 300 mg • ($20 per month) • Clonidine 0. 1 -0. 4 mg • ($5 per month) • Guanfacine 1 -4 mg • ($5 per month) Note: any combination that decreases MAS XR dose to 30 mg or less decreases his stimulant cost by $85 per month
- Slides: 59